Professional Documents
Culture Documents
NCP Impaired Physical Mobility
Uploaded by
Rene John FranciscoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP Impaired Physical Mobility
Uploaded by
Rene John FranciscoCopyright:
Available Formats
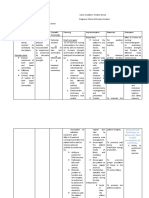
Cues Subjective: Ang hirap ng may ganito (traction).
Bawal kumilos, hindi man lang ako makapunta sa banyo para maligo. Hinihintay ko pa na may bisita ako para lang makapaglinis ng sarili ko verbalized by the client. Objective: Client is on modified bucks extension traction. Client is on semifowlers position. Client had fracture on the proximal 3rd of his left femur due to gunshot. Client had three gunshots on his abdomen with mainly his duodenum and jejunum as well as in his right leg. Provisional Diagnosis: Hypovolemic shock 2 to multiple GSW Measurement: Red Blood Cells
Nursing Diagnosis Impaired Physical Mobility related to musculoskeletal impairment possibly evidenced by inability to move purposefully within the physical environment, imposed restriction.
Analysis Impaired Physical Mobility Limitation in independent, purposeful physical movement of the body or of one or more extremities. (Nurses Pocket Guide-Diagnoses, Prioritized Interventions, and Rationales by Marilynn E. Doenges, Mary Frances Moorhouse, Alice C. Murr p.457) Alteration in mobility may be a temporary or more permanent problem. Most disease and rehabilitative states involve some degree of immobility (e.g., as seen in strokes, leg fracture, trauma, morbid obesity, and multiple sclerosis). With the longer life expectancy for most Americans, the incidence of disease and disability continues to grow. And with shorter hospital stays, patients are being transferred to rehabilitation
Planning Goals: After 8 hours of nursing intervention, the client will be able to verbalize understanding of situation and individual treatment regimen and safety measures independently. Objectives: After 1 hour of nursing intervention, the client will be able to: 1. To identify at least five out of eight causative/contributing factors
Intervention
Rationale
Evaluation The goal was met.
Determine diagnosis that contributes to immobility
These conditions can cause physiological and psychological problems that can seriously impact physical, social, and economic well-being. Identifies potential impairments and determines type of interventions needed to provide for clients safety To determine presence of characteristics of clients unique impairment and to guide choice of interventions Identified mobility as the most important functional ability that determines the degree of independence and healthcare needs among older persons.2 While aging per se does not cause impaired mobility, several
Met. The client was able to identify five out of eight causative/contributing factors.
Note factors affecting current situation and potential time involved.
Assess clients developmental level, motor skills, ease and capability of movement, posture and gait. Note older clients general health status
3.77 x 10^12/L Normal Findings: (Males) 5.5-6.5 x10^12/L Hemoglobin 11.80 g/dL Normal Findings: (Males) 14-16 g/dL Hematocrit 0.33 L/L Normal Findings: (Males) 0.42-0.52 L/L Lymphocytes 0.21 Normal Findings: 0.25-0.35 Eosinophils 0.01 Normal Findings 0.03-0.05
facilities or sent home for physical therapy in the home environment. Mobility is also related to body changes from aging. Loss of muscle mass, reduction in muscle strength and function, stiffer and less mobile joints, and gait changes affecting balance can significantly compromise the mobility of elderly patients. Mobility is paramount if elderly patients are to maintain any independent living. Restricted movement affects the performance of most activities of daily living (ADLs). Elderly patients are also at increased risk for the complications of immobility. Nursing goals are to maintain functional ability, prevent additional impairment of physical activity, and ensure a safe environment. (Nursing Care Plans: Nursing Diagnosis and Intervention by Gulanick, Myers,
predisposing factors in addition to age-related changes can lead to immobility Evaluate for presence/degree of pain, listening to clients description about manner in which pain limits mobility. Ascertain clients perception of activity/exercise needs and impact of current situation. Identify cultural beliefs and expectations affecting recovery/response to long-term limitations. Assess nutritional status and clients report of energy level. To determine needed interventions for pain management
Helps to determine clients expectations/beliefs related to activity and potential long-term effect of current immobility. Also identifies barriers that may be addressed
Deficiencies in nutrients and water, electrolytes and minerals can negatively affect energy and activity tolerance. Client may be restricting activity because of weakness/debilitation, actual injury during a fall, or from psychological distress that can persist after a fall. Identifies strengths and deficits impaired physical mobility and may provide information regarding potential for recovery Impairments related to age, chronic or acute disease condition, trauma, Met. The client was able to report three out of five of his functional ability.
Determine history of falls and relatedness to current situation.
2. To report three out of five of his functional ability
Determine degree of immobility in relation to 04 scale, noting muscle strength and tone, joint mobility, cardiovascular status, balance, and endurance. Determine degree of perceptual/cognitive impairment and ability to follow directions
Klop, Galanes, Gradishar and Puzas) Observe movement when client is unaware of observation Note emotional/behavioral responses to problems of immobility
surgery, or medications require alternative interventions or changes in plan of care. To note any incongruence with reports of abilities. Can negatively affect selfconcept and self-esteem, autonomy, and independence. Feelings of frustration and powerlessness may impede attainment of goals. Social, occupational, and relationship roles can change, leading to isolation, depression, and economic consequences Studies have shown that as much as 5.5% of muscle strength can be lost each day of rest and immobility.5 Other complications include changes in circulation and impairments of organ function affecting the whole person To maximize potential for mobility and optimal function. May be necessary when client is using avoidance or controlling behavior, or is not aware of own abilities due to anxiety/fear. To enhance circulation to Met. The client was able to explain at least five of the optimal level of function and measures on how to prevent complications.
Determine presence of complications related to immobility
3. To explain at least five of the optimal level of function and measures on how to prevent complications.
Assist with treatment of underlying condition(s) Discuss discrepancies in movement with client aware and unaware of observation and methods for dealing with identified problems. Assist/have client reposition self
on a regular schedule as dictated by individual situation Review/encourage use of proper body mechanics Demonstrate/assist with use of side rails, overhead trapeze, roller pads, hydraulic lifts/chairs Support affected body parts/joints using pillows/rolls, foot supports/shoes, gel pads, etc., Provide/recommend egg-crate, alternating air-pressure, or water mattress. Use padding and positioning devices
tissues, reduce risk of tissue ischemia. To prevent injury to client and caregiver For position changes/transfers. Instruct in safe use of walker/cane for ambulation. To maintain position of function and reduce risk of pressure ulcers. Reduces tissue pressure and aids in maximizing cellular perfusion to prevent dermal injury. To prevent stress on tissues and reduce potential for disuse complications. Reduces sensory deprivation, enhances selfconcept and sense of independence, and improves body strength and function. To reduce fatigue.
Encourage clients participation in self-care activities, physical/occupational therapies as well as diversional/recreational activities. Provide client with ample time to perform mobility-related tasks. Schedule activities with adequate rest periods during the day Avoid routinely assisting or doing for client those activities that client can do for self. Identify/encourage energyconserving techniques for
Caregivers can contribute to impaired mobility by being overprotective or helping too much. Limits fatigue, maximizing
ADLs. Note change in strength to do more or less self-care
participation. To promote psychological and physical benefits of self-care and to adjust level of assistance as indicated. To permit maximal effort/involvement in activity. To reduce pressure on sensitive areas and to prevent development of problems with skin integrity. Promotes well-being and maximizes energy production. Enhances commitment to plan, optimizing outcomes. Multiple options provide client choices and variety May need instruction and to give return demonstration May need referral for support and community services to provide care, supervision, companionship, respite services, nutritional and ADL assistance, adaptive devices or changes to living environment, financial assistance, etc Met. The client was able to discuss four out of five of wellness program.
Administer medications before activity as needed for pain relief Perform/encourage regular skin examination and care
Encourage adequate intake of fluids/nutritious foods Encourage clients/SOs involvement in decision making as much as possible Discuss safe ways that client can exercise 4. To discuss four out of five of wellness program. Assist client/SO to learn safety measures as individually indicated. Involve client and SO(s) in care, assisting them to learn ways of managing problems of immobility, especially when impairment is expected to be long-term.
Demonstrate use of standing aids and mobility devices and have client/careprovider demostrate knowledge about/safe use of device. Identify appropriate resources for obtaining and maintaining appliances/ equipment.
Safe use of mobility aids promotes clients independence and enhances quality of life and safety for client and caregiver (Nurses Pocket GuideDiagnoses, Prioritized Interventions, and Rationales by Marilynn E. Doenges, Mary Frances Moorhouse, Alice C. Murr p.458-461)
You might also like
- NCP For Impaired Physical MobilityDocument1 pageNCP For Impaired Physical Mobilityitzme_andreaNo ratings yet
- Impaired Physical MobilityDocument1 pageImpaired Physical Mobilityrozj0781% (21)
- Impaired Physical MobilityDocument1 pageImpaired Physical Mobilitykyaw100% (1)
- NCP-Impaired Physical MobilityDocument3 pagesNCP-Impaired Physical MobilityRene John FranciscoNo ratings yet
- Improving Physical Mobility Through Nursing InterventionsDocument2 pagesImproving Physical Mobility Through Nursing InterventionsPrincess Averin Navarro50% (2)
- NCP Cva Impaired Physical MobilityDocument2 pagesNCP Cva Impaired Physical MobilityMaricar Azolae MascualNo ratings yet
- Impaired Physical MobilityDocument3 pagesImpaired Physical Mobilityvidagurl0% (1)
- NCP of Impaired MobilityDocument3 pagesNCP of Impaired MobilityHazel Cabrera0% (1)
- Impaired Physical Mobility. NCPDocument1 pageImpaired Physical Mobility. NCPwguino100% (3)
- NCP Impaired Physical MobilityDocument2 pagesNCP Impaired Physical MobilityKate Charnhattasin63% (8)
- NCP Impaired Physical Mobility-2Document4 pagesNCP Impaired Physical Mobility-2ejoanbNo ratings yet
- Nursing Care for Impaired Physical MobilityDocument3 pagesNursing Care for Impaired Physical MobilityMeljonesDaan100% (1)
- NCP For Impaired Skin IntegrityDocument3 pagesNCP For Impaired Skin IntegrityAemz Alacasnap Ainegud100% (1)
- NCP Impaired Physical MobilityDocument2 pagesNCP Impaired Physical MobilityDante Sales67% (6)
- NCP-Self Care DeficitDocument2 pagesNCP-Self Care DeficitJon Eric G. Co100% (2)
- NCP-Impaired Physical MobilityDocument3 pagesNCP-Impaired Physical MobilityradarsoulNo ratings yet
- Nursing Care Plan (ImpairedphyssicalDocument5 pagesNursing Care Plan (ImpairedphyssicalkuroroexileNo ratings yet
- Impaired Bed MobilityDocument2 pagesImpaired Bed MobilityMary Louisse LastimadoNo ratings yet
- Nursing Cues for Pain ManagementDocument8 pagesNursing Cues for Pain ManagementAi RouNo ratings yet
- Improve knee mobility with exercise and medicationDocument1 pageImprove knee mobility with exercise and medicationMaria Chrislyn Marcos Genorga100% (1)
- Mobility Nursing Diagnosis GuideDocument3 pagesMobility Nursing Diagnosis GuideYan ReyesNo ratings yet
- Impaired Physical Mobility Related To Application of Traction or Cast As Evidenced by AssessmentDocument13 pagesImpaired Physical Mobility Related To Application of Traction or Cast As Evidenced by AssessmentJaylord VerazonNo ratings yet
- NCP FractureDocument3 pagesNCP FractureDino V EscalonaNo ratings yet
- NCP - BedriddenDocument4 pagesNCP - Bedriddenadelaigner_racho589475% (4)
- Impaired mobility assessmentDocument2 pagesImpaired mobility assessmentVhin Lim100% (2)
- NCP For Impaired Physical MobilityDocument2 pagesNCP For Impaired Physical MobilityFielMendoza0% (1)
- Impaired Physical Mobility RT Neuromuscular Skeletal Impairment.Document3 pagesImpaired Physical Mobility RT Neuromuscular Skeletal Impairment.Abegail Abaygar100% (2)
- Self Care Deficit BahtingDocument1 pageSelf Care Deficit BahtingNaj SoliveresNo ratings yet
- Impaired Physical MobilityDocument8 pagesImpaired Physical MobilityKM78% (9)
- Mpaired Physical Mobility (Amputation) : Nursing Care PlanDocument3 pagesMpaired Physical Mobility (Amputation) : Nursing Care PlanTheSweetpea5010% (2)
- Nursing Care Plan - Impaired Physical MobilityDocument2 pagesNursing Care Plan - Impaired Physical MobilitySusan Croce57% (7)
- NCP About Fluid IntakeDocument5 pagesNCP About Fluid IntakeWild Rose100% (1)
- Gouty Arthritis-NcpDocument2 pagesGouty Arthritis-NcpJohn D100% (2)
- NCP-Impaired Physical Mobility - E+ ImbalanceDocument3 pagesNCP-Impaired Physical Mobility - E+ ImbalanceRene John FranciscoNo ratings yet
- Impaired Skin IntegrityDocument1 pageImpaired Skin IntegrityHanya Bint PotawanNo ratings yet
- NCP Impaired Physical MobilityDocument2 pagesNCP Impaired Physical MobilityKristine Young0% (1)
- Impaired Physical MobilityDocument3 pagesImpaired Physical MobilityCharmaine ChuaNo ratings yet
- Impaired Physical Mobility Related To Pain and DiscomfortDocument2 pagesImpaired Physical Mobility Related To Pain and DiscomfortRis NapolisNo ratings yet
- Impaired Physical Mobility CholecystectomyDocument2 pagesImpaired Physical Mobility CholecystectomyPrincess Danica Purcia100% (1)
- College of Health Sciences Nursing Care Plan for Fractured FemurDocument5 pagesCollege of Health Sciences Nursing Care Plan for Fractured FemurMae CeaesarNo ratings yet
- Spinal Cord Injury NCPDocument2 pagesSpinal Cord Injury NCPEmmanuelRodriguez100% (1)
- Nursing Diagnosis Fatigue Liver Cancer Care PlanDocument2 pagesNursing Diagnosis Fatigue Liver Cancer Care PlanPC NNo ratings yet
- NCP-Impaired Skin IntegrityDocument2 pagesNCP-Impaired Skin IntegrityRI NA100% (1)
- NCP CVA Impaired Physical Mobility 1Document2 pagesNCP CVA Impaired Physical Mobility 1Frency Anne Causo Pascual100% (1)
- NCP-Impaired Physical MobilityDocument6 pagesNCP-Impaired Physical MobilityRowell Zaragoza91% (11)
- IMPAIRED PHYSICAL MOBILITY RT Neuromuscular Involvement (Right Sided Paresthesia Aeb Inability To Purposefully Move Body Parts.Document2 pagesIMPAIRED PHYSICAL MOBILITY RT Neuromuscular Involvement (Right Sided Paresthesia Aeb Inability To Purposefully Move Body Parts.Senyorita KHaye67% (3)
- Nursing Care Plan: Cues and Data Nursing Diagnosis Analysis Goal and Objectives Interventions Rationale EvaluationDocument3 pagesNursing Care Plan: Cues and Data Nursing Diagnosis Analysis Goal and Objectives Interventions Rationale EvaluationPaul Cubacub100% (1)
- NCP Delayed Wound RecoveryDocument5 pagesNCP Delayed Wound RecoveryDarkCeades100% (2)
- XIII. NCP Risk For FallsDocument1 pageXIII. NCP Risk For FallsMartin T Manuel100% (2)
- Body Weakness NCPDocument1 pageBody Weakness NCPArnold Christian QuilonNo ratings yet
- Nursing DiagnosisvfsdsDocument2 pagesNursing DiagnosisvfsdsPrincess Gutierrez Rosita100% (1)
- NCP - Risk For Impaired Skin Integrity R/T Dry Skin and Behaviors That May Lead To Skin Integrity Impairment AEB Scratching of ScabsDocument1 pageNCP - Risk For Impaired Skin Integrity R/T Dry Skin and Behaviors That May Lead To Skin Integrity Impairment AEB Scratching of ScabsCarl Elexer Cuyugan Ano100% (4)
- NCP Bed MobilityDocument1 pageNCP Bed MobilityDiana Laura Lei100% (2)
- Impaired Physical MobilityDocument11 pagesImpaired Physical MobilityAgronaSlaughter100% (1)
- NCP - Impaired Tissue IntegrityDocument3 pagesNCP - Impaired Tissue IntegrityRene John FranciscoNo ratings yet
- NCM104b BSN220 Mobility NursingDocument9 pagesNCM104b BSN220 Mobility NursingChristian Apelo SerquillosNo ratings yet
- Nursing Care Plan: West Visayas State University College of NursingDocument4 pagesNursing Care Plan: West Visayas State University College of NursingLizaEllaga100% (1)
- NUR403 Assiginment 2Document8 pagesNUR403 Assiginment 2KwanNingYuNo ratings yet
- Geriatric Nursing Care Plan for Failure to ThriveDocument15 pagesGeriatric Nursing Care Plan for Failure to ThriveYongNo ratings yet
- Assessing SLE Patient with Rash, Alopecia and Joint PainDocument13 pagesAssessing SLE Patient with Rash, Alopecia and Joint PainMary Mae Bercacio Buella100% (3)
- Genexpert TestDocument2 pagesGenexpert TestRene John FranciscoNo ratings yet
- Surgical InstrumentsDocument8 pagesSurgical InstrumentsSharmaine Simon91% (11)
- Bloom's TaxonomyDocument26 pagesBloom's TaxonomyRene John FranciscoNo ratings yet
- Surgical Instrumentation - R. ILADODocument54 pagesSurgical Instrumentation - R. ILADOrhenier_ilado100% (1)
- MSPPP 12913337842396 Phpapp01Document26 pagesMSPPP 12913337842396 Phpapp01RI NANo ratings yet
- Gifts of the Holy Spirit ExplainedDocument4 pagesGifts of the Holy Spirit ExplainedMauricio Rojas ValdiviaNo ratings yet
- Basic Surgical InstrumentsDocument37 pagesBasic Surgical Instrumentsapi-2658787991% (33)
- Stress ManagementDocument17 pagesStress Managementanon_469843072No ratings yet
- Potassium ChlorideDocument2 pagesPotassium ChlorideRene John FranciscoNo ratings yet
- Scientific Death of JesusDocument7 pagesScientific Death of JesusRene John FranciscoNo ratings yet
- Slides Surgical Instruments Update 1.7Document43 pagesSlides Surgical Instruments Update 1.7Paul Christian P. Santos, RN100% (32)
- Drug Study for Psychosis and Bipolar DisorderDocument4 pagesDrug Study for Psychosis and Bipolar DisorderJowel Cruz De LeonNo ratings yet
- Facts of The RealityDocument11 pagesFacts of The RealityRene John FranciscoNo ratings yet
- OR EquipmentsDocument8 pagesOR EquipmentsRene John FranciscoNo ratings yet
- Basic Delivery Set (Nullipara)Document1 pageBasic Delivery Set (Nullipara)Rene John FranciscoNo ratings yet
- Naloxone, MorphineDocument7 pagesNaloxone, MorphineRene John FranciscoNo ratings yet
- Dressing For Job Interview and ResignationDocument7 pagesDressing For Job Interview and ResignationRene John FranciscoNo ratings yet
- Drug Study For Paracetamol, Omeprazole and Vitamin B ComplexDocument3 pagesDrug Study For Paracetamol, Omeprazole and Vitamin B ComplexMichelle Manibale R.N100% (4)
- Drug Study - MirceraDocument2 pagesDrug Study - MirceraRene John FranciscoNo ratings yet
- Drug Study - Paracetamol Ambroxol, Ascorbic Acid, CefuroximeDocument4 pagesDrug Study - Paracetamol Ambroxol, Ascorbic Acid, Cefuroximeapi-3701489100% (12)
- Omeprazole and Polynerv (B1,6,12)Document3 pagesOmeprazole and Polynerv (B1,6,12)Rene John Francisco100% (1)
- Drug Study (Combivent)Document2 pagesDrug Study (Combivent)Rene John Francisco100% (3)
- Chapter 45 - Drugs For HypertensionDocument14 pagesChapter 45 - Drugs For Hypertensiondlneisha61100% (1)
- NCP-Impaired Physical Mobility - E+ ImbalanceDocument3 pagesNCP-Impaired Physical Mobility - E+ ImbalanceRene John FranciscoNo ratings yet
- Omeprazole and Polynerv (B1,6,12)Document3 pagesOmeprazole and Polynerv (B1,6,12)Rene John Francisco100% (1)
- ErythromycinDocument6 pagesErythromycinapi-3797941100% (1)
- Drug Study On Emergency DrugsDocument14 pagesDrug Study On Emergency DrugsRene John FranciscoNo ratings yet
- Drug Study (Budesonide)Document1 pageDrug Study (Budesonide)Rene John Francisco33% (3)
- Drug Study (Seretide)Document1 pageDrug Study (Seretide)Rene John Francisco100% (1)
- Diazepam, Lanoxin, Hemostan, NaprexDocument6 pagesDiazepam, Lanoxin, Hemostan, NaprexRene John Francisco100% (1)
- Instructions For Treatment and Use of Insecticide-Treated Mosquito NetsDocument51 pagesInstructions For Treatment and Use of Insecticide-Treated Mosquito NetsMaxwell WrightNo ratings yet
- Alywn Cosgrove Real World Fat Loss PDFDocument75 pagesAlywn Cosgrove Real World Fat Loss PDFJM Gym Manticao100% (1)
- BDMS Trauma Algorithm Version 2.0Document32 pagesBDMS Trauma Algorithm Version 2.0Aungkhena Noomnim100% (2)
- Hemodialysis Prescription and TreatmentDocument12 pagesHemodialysis Prescription and TreatmentkidneymastersNo ratings yet
- PSMDocument62 pagesPSMzamijakaNo ratings yet
- Factors Influencing Health Status (FIHS) : Rating GuidelinesDocument3 pagesFactors Influencing Health Status (FIHS) : Rating GuidelinesAyan Kumar GhoshNo ratings yet
- The Effect of Piezoelectric and Magnetostrictive Scaling DevicesDocument38 pagesThe Effect of Piezoelectric and Magnetostrictive Scaling Devicesnotaden1849No ratings yet
- Kesesuaian StokDocument2 pagesKesesuaian StokResky OktavianiNo ratings yet
- The Relevance of Root Canal Isthmuses in Endodontic RehabilitationDocument13 pagesThe Relevance of Root Canal Isthmuses in Endodontic RehabilitationVictorNo ratings yet
- Comm 602 Assignment 1Document4 pagesComm 602 Assignment 1hamiltjw2No ratings yet
- Dream New Dreams by Jai Pausch - Reading Group GuideDocument9 pagesDream New Dreams by Jai Pausch - Reading Group GuideCrown Publishing GroupNo ratings yet
- Krav Maga To Empower KidsDocument7 pagesKrav Maga To Empower KidshectorhugoarNo ratings yet
- Micronutrient Deficiency Among FilipinosDocument20 pagesMicronutrient Deficiency Among FilipinosAlnyssa Cornell100% (1)
- Asbmt: BK Virus Disease After Allogeneic Stem Cell Transplantation: A Cohort AnalysisDocument7 pagesAsbmt: BK Virus Disease After Allogeneic Stem Cell Transplantation: A Cohort Analysiscalixto hernandezNo ratings yet
- Masonry QuizDocument12 pagesMasonry QuizJoanne Jose Castro0% (1)
- Get ShreddedDocument17 pagesGet ShreddedSlevin_KNo ratings yet
- Incident Report PortfolioDocument2 pagesIncident Report Portfolioapi-397923551No ratings yet
- Flora-Focus® Lactobacillus Reuteri LR-G100 200billionDocument2 pagesFlora-Focus® Lactobacillus Reuteri LR-G100 200billionUmar AliNo ratings yet
- Individual Development FactorsDocument9 pagesIndividual Development Factorshanani_leeNo ratings yet
- Tai Chi Qigong TrainerDocument11 pagesTai Chi Qigong Trainerskycall28No ratings yet
- Hse Pja BtsguideDocument2 pagesHse Pja BtsguideMohamed Ismail ShehabNo ratings yet
- Building The Future - Children and The Sustainable Development Goals in Rich CountriesDocument60 pagesBuilding The Future - Children and The Sustainable Development Goals in Rich CountriesStuff Newsroom100% (1)
- Controlled and Novel Drug DeliveryDocument23 pagesControlled and Novel Drug Deliverynews information0% (1)
- Group Dynamics, Kidnapping, Abduction, Fraternities & GangsDocument18 pagesGroup Dynamics, Kidnapping, Abduction, Fraternities & GangsThe UseNo ratings yet
- Malmstrom Et Al - 1999 - Oral Montelukast, Inhaled Beclomethasone, and Placebo For Chronic AsthmaDocument10 pagesMalmstrom Et Al - 1999 - Oral Montelukast, Inhaled Beclomethasone, and Placebo For Chronic AsthmaRutvik ShahNo ratings yet
- Briovent VentilatorDocument10 pagesBriovent VentilatorPurchase DepartmentNo ratings yet
- Thrombosis and EmbolismDocument39 pagesThrombosis and Embolismilva100% (1)
- SW 103 2nd Topic PDFDocument12 pagesSW 103 2nd Topic PDFMarielle BringasNo ratings yet
- 2011 Fyi Report DocumentDocument110 pages2011 Fyi Report DocumentSmart Horizons Lifetime Training SolutionsNo ratings yet
- Symposium BullyingDocument28 pagesSymposium BullyingJackielyn CatallaNo ratings yet