Professional Documents
Culture Documents
Chronic Kidney Disease
Uploaded by
Roseben SomidoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chronic Kidney Disease
Uploaded by
Roseben SomidoCopyright:
Available Formats
PERPETUAL HELP COLLEGE OF MANILA
COLLEGE OF NURSING
A PARTIAL REQUIREMENT FOR NCM 204
CASE STUDY ON CHRONIC KIDNEY DISEASE
Submitted to : Mrs. May Flores-Lugay Submitted by: Lucky Bryan S. Abala
CHRONIC KIDNEY DISEASE
Definition Chronic kidney disease (CKD), also known as chronic renal disease, is a progressive loss in renal function over a period of months or years. The symptoms of worsening kidney function are unspecific, and might include feeling generally unwell and experiencing a reduced appetite. Often, chronic kidney disease is diagnosed as a result of screening of people known to be at risk of kidney problems, such as those with high blood pressure or diabetes and those with a blood relative with chronic kidney disease. Chronic kidney disease may also be identified when it leads to one of its recognized complications, such as cardiovascular disease, anemia or pericarditis.[1] Chronic kidney disease is identified by a blood test for creatinine. Higher levels of creatinine indicate a falling glomerular filtration rate and as a result a decreased capability of the kidneys to excrete waste products. Creatinine levels may be normal in the early stages of CKD, and the condition is discovered if urinalysis (testing of a urine sample) shows that the kidney is allowing the loss of protein or red blood cells into the urine. To fully investigate the underlying cause of kidney damage, various forms of medical imaging, blood tests and often renal biopsy (removing a small sample of kidney tissue) are employed to find out if there is a reversible cause for the kidney malfunction.[1] Recent professional guidelines classify the severity of chronic kidney disease in five stages, with stage 1 being the mildest and usually causing few symptoms and stage 5 being a severe illness with poor life expectancy if untreated. Stage 5 CKD is also called established chronic kidney disease and is synonymous with the now outdated terms endstage renal disease (ESRD), chronic kidney failure (CKF) or chronic renal failure (CRF).[1] There is no specific treatment unequivocally shown to slow the worsening of chronic kidney disease. If there is an underlying cause to CKD, such as vasculitis, this may be treated directly with treatments aimed to slow the damage. In more advanced stages, treatments may be required for anemia and bone disease. Severe CKD requires one of the forms of renal replacement therapy; this may be a form of dialysis, but ideally constitutes a kidney transplant Introduction Chronic Kidney Disease (CKD) is a rapidly growing health problem. Estimates are that 11% of the U.S population or 19.2 million people have CKD. The centers for disease control and prevention in Atlanta has recently established a chronic kidney disease program to enhanced surveillance and prevention programs for CKD at the federal and state levels. The many diseases described in this chapter can lead to CKD, and the etiology will differ by disease. Recognition of the type of kidney disease and etiology may be useful to prevent or slow progression of the disease.
Patient Profile: Name: Ms. E. E Age: 41 Sex: Female Address: Manila Chief complaint: difficulty of breathing Admitting diagnosis: Chronic Kidney disease 2 chronic glomerulonephritis Patient health history: Patient experienced difficulty of breathing 2 years and 3 months ago, while she was working abroad. She worked as OFW at South Korea and she verbalized that while working she was a light drinker and she stay up late in the evening. Family health history: The patient verbalized that she and her family also have a history of hypertension.
Anatomy and Physiology
The human kidney anatomy is well equipped to perform all its crucial functions. The following kidney diagram represents the structure of a kidney... sliced vertically.
KIDNEY DIAGRAM
KIDNEY ANATOMY The kidneys are dark-red, bean-shaped organs. One side of the kidney bulges outward (convex) and the other side is indented (concave). There is a cavity attached to the indented side of the kidney, called the Renal Pelvis... which extends into the ureter. Each Kidney is enclosed in a transparent membrane called the renal capsule... which helps to protect them against infections and trauma. The kidney is divided into two main areas... a light outer area called the renal cortex, and a darker inner area called the renal medulla. Within the medulla there are 8 or more cone-shaped sections known as renal pyramids. The areas between the pyramids are called renal columns. Kidney Anatomy and Excretion The most basic structures of the kidneys are nephrons. Inside each kidney there are about one million of these microscopic structures. They are responsible for filtering the blood... removing waste products. The renal artery delivers blood to the kidneys each day. Over 180 liters (50 gallons) of blood pass through the kidneys every day. When this blood enters the kidneys it is filtered and returned to the heart via the renal vein. The process of separating wastes from the body's fluids and eliminating them is known as excretion. The body has four organ systems that are responsible for excretion. The urinary system is one of the main organ systems responsible for excretion. It excretes a broad variety of metabolic wastes, toxins, drugs, hormones, salts, hydrogen irons and water. The kidneys are the main organs of the urinary system. The kidneys are full of blood vessels. Blood vessels are integral to efficient kidney function. Every function of the kidney involves blood, therefore, it requires a lot of blood vessels to facilitate these functions. Together, the two kidneys contain about 160 km of blood vessels.
KIDNEY LOCATION The normal kidney location is towards the back of the abdominal cavity, just above the waist. If you put your hands on your hips, your kidneys are located just about where your thumbs are. One kidney is normally located just below the liver, on the right side of the abdomen and the other is just below the spleen on the left side. In rare cases, however, one or both kidneys may be located much lower in the abdomen. This is not necessarily a problem except probably in the case of pregnancy. As the fetus begins to develop in the womb this could sometimes place pressure on the kidney which is located in the lower abdomen.
NORMAL KIDNEY SIZE
The normal kidney size of an adult human is about 10 to 13 cm (4 to 5 inches) long and about 5 to 7.5 cm (2 to 3 inches) wide. It is approximately the size of a conventional computer mouse. A kidney weighs approximately 150 grams. Kidneys weigh about 0.5 percent of total body weight.
The human kidney anatomy, though relatively simple, enables it to perform extremely complex but essential functions. If any area of the kidney is damaged or becomes diseased, this could significantly affect its ability to perform these functions. The function of the kidney is primarily to rid the body of toxins, but this is not the only function of the kidney. The kidney plays a crucial role in keeping the blood clean and regulating the amount of fluid in the body. It has a unique anatomy and is equipped to efficiently discharge its functions. Most humans are born with two kidneys, although one kidney is capable of performing the normal functions of both kidneys. In rare cases a person may be born with one kidney or may lose a kidney through injury, disease or surgery (for example when a person donates a kidney). Amazingly, such people are still able to lead normal lives, without any adverse effects to their health.
The function of the kidney is primarily to rid the body of toxins, but this is not the only function of the kidney. The kidney plays a crucial role in keeping the blood clean and regulating the amount of fluid in the body. It has a unique anatomy and is equipped to efficiently discharge its functions. Most humans are born with two kidneys, although one kidney is capable of performing the normal functions of both kidneys. In rare cases a person may be born with one kidney or may lose a kidney through injury, disease or surgery (for example when a person donates a kidney). Amazingly, such people are still able to lead normal lives, without any adverse effects to their health. Key Kidney Functions If you asked anyone what is the function of the kidney, they might respond by saying that it produces urine. They will, of course, be correct but this is not the only kidney function. While this is one of the major functions of the kidney, this remarkable organ does a lot more. You might be amazed to discover just how extensive is the role of the kidney, as it pertains to maintaining overall human health. The main function of the kidney is the removal of toxic waste products from the blood. Chief among these waste products are urea and uric acid. If too many of these waste products are allowed to accumulate in the blood stream, this will result in life threatening illnesses. Fortunately, these two deadly substances are easily expelled from the body by the kidneys... through the process of excretion. Excretion is a process which continuously cleans the blood... keeping it free of unwanted and dangerous substances. This very important job is performed by microscopic structures in the kidneys called nephrons. The kidneys are in fact the main organs of the urinary system... responsible for removing waste substances from the body, in the form of urine. Regulating the amount of water and salt in the blood is another important function of the kidney. As you may know, the body is made up primarily of water. Water is indeed necessary for many of the body's biological functions. Too much water, however, could dilute the blood... negatively affecting the environment in which the cells operate. Let's suppose that you drink a lot of water quickly. The water is absorbed from your gut into the bloodstream, and it has the effect of diluting the blood. The diluted blood reaches the kidney, which takes excess water out of it and passes it into the urine. Salt is dealt with in the same way. If you had a salty meal the salt is absorbed into your blood. When the salty blood reaches the kidney the salt is removed from it and passed into the urine. This is an extremely important function of the kidney. The relative amount of water and salt in the blood give the blood a particular concentration. By regulating the amount of salt and water in the blood, the kidneys ensure that the concentration and volume of the blood stays more or less the same all the time.
Another crucial function of the kidney is to regulate blood-pressure. They secrete an enzyme called renin, which activates hormonal mechanisms that controls blood pressure and electrolyte balance. When, for instance, blood-pressure begins to fall, the kidneys release the enzyme renin. This enzyme converts blood protein into a hormone called angiotensin. Angiotensin then induces the adrenal gland to release another hormone called aldosterone. This hormone causes sodium and water to be reabsorbed into the blood, thereby increasing blood-volume and blood-pressure. The response of the kidneys to aldosterone helps to regulate the level of salt in the blood.
Etiology and risk factors The increasing incidence of CKD partially reflects increased obesity-related hypertension and diabetes Mellitus in sedentary, well-nourished populations. Since cardiovascular disease and Diabetes mellitus are frequently co-morbid conditions associated with CKD, aggressive treatment of the disease and risk factors can slow progression of the illness and limit morbidity and mortality. The National Kidney Foundation (NKF) Kidney DISEASE Outcome Quality initiative (K/DOQI) defined CKD as kidney damage with a glomerular filtration rate (GFR) <60 ML/MINUTE/1.73 M2 for more than 3 months. The NKF (Developed a classification system for the stages of CKD. Traditionally, the classification of the type of kidney disease has been focused on pathology and etiology. The K/DOQI classification system focuses on the GFR, but it remains important to diagnose the cause of CKD.
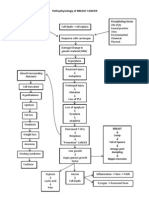
Pathophysiology There are many diseases that cause CKD; each has its own pathophysiology. However, there are common mechanisms for disease progression. Pathologic features include fibrosis, loss of renal cells, and infiltration of renal tissue by monocytes and macrophages. Proteinuria, hypoxia, and excessive angiotensin II production all contribute to the pathophysiology. In an attempt to maintain GFR, the glomerulus hyper filtrates; this results in endothelial injury. Proteinuria results from increased glomerular permeability and increased capillary pressure. Hypoxia also contributes to disease progression. Angiotensin II increases glomerular hypertension, which further damages the kidney. Clinical Manifestations The clinical manifestations of CKD are highly variable. Many people with CKD have few if any complaints. In sage 1, clients usually have normal blood pressure, no laboratory test abnormalities, and no clinical manifestations. Clients in stage 2 are generally asymptomatic, but mat develop hypertension, and laboratory test abnormalities exist. In stage 3, clients are still usually asymptomatic but laboratory values suggest abnormalities in several organ systems, and hypertension is frequently present. By stage
4, clients begin to experience clinical manifestations associated with CKD such as fatigue and poor appetite. At stage 5, full-blown clinical manifestations of end-stage renal disease (ESRD) are evident. Proteinuria is one of the strongest predictors of progression of CKD. As the GFR declines, clients may show not only proteinuria but also hypertension, a wide range of lab abnormalities, and manifestation resulting from disorders in other organs. These disorders include anemia, metabolic acidosis, dyslipidemia, bone disease, protein-energy malnutrition, and neuropathy.
Stages of Chronic Kidney Disease
STAGE DESCRIPTION Kidney damage with normal glomerular filtration rate Kidney damage with mild decrease in GFR Moderate decrease in GFR Severe decrease in GFR Kidney failure Other Terms used At risk GFR (ml/min/1.73m2) >90
Chronic renal insufficiency (CRI) CRI, chonic renal failure (CRF) CRF
60_89
30-59
3 4
15-29
Ed-stage renal disease (ESRD)
<15
National KIDNEY Foundation Classification of Chronic Kidney Disease
Stage --
Severity At increased risk
GFR Ml/min 60
Kiney damage damage: normal or Increase GFR Kidney damge: Mild GFR
90
Progression (Chronic kidney disease risk factors present ) None apparent
Symptoms None
None
60-89
3 Moderate GFR
30-59
Increasing PTH Early bone disease Erythropoietin deficiency anemia
Subtle
Mild
Severe:
GFR
15-29
End-stage kidney disease; Kidney failure
<15
Increased triglycerides Metabolic acidosis Hyperkalemia Salt/water retention uremia
Moderate
Severe
Adapted from National Kidney Foundation, Clinical practice Guide Guidelines for Chronic Kidney Disease: Evaluation, classification, stratification: dentition and classification of stages of chronic kidney disease, 2002; Available at http://www.kidney.org/professionals/kdoqi/guidelines_ckd/p4_class_g1.htm
Factors Representing Progression of Chronic Renal Failure Factor Proteinuria Creatinine and urea clearance Sodium and water balance Phosphate and calcium balance Characteristics
Glomerular hyper filtration of protein contributes to tubular interstitial injury by accumulating in the interstitial space and promoting inflammation and progressive fibrosis. In chronic renal failure, the GFR falls and the plasma creatinine concentration increases by a reciprocal amount; because there is no regulatory adjustment for creatinine , plasma levels continue to rise and serve as an index of changing glomerular function. As GFR declines, urea clearance increases, (NOTE: Urea is both filtered and reabsorbed and varies with the state of hydration. In chronic renal failure, sodium load delivered to nephrons exceed normal, so excretion must increased, thus less is reabsorbed. Obligatory loss occurs, leading to sodium deficits and volume depletion. As GFR is reduced, ability to concentrate and dilute urine diminishes. Changes in acid-base balance affect phosphate and calcium balance. The major disorders associated with chronic renal failure are reduced renal phosphate excretion, decreased renal synthesis of 1, 25(OH)2 Vitamin D3, and hypocalcemia. Hypocalcemia leads to secondary hyperparathyroidism, GFR falls, and progressive hyperphoshatemia, hypocalcemia, and dissolution of bone result. Because of anemia that accompanies chronic renal failure, lethargy, dizziness, and low hematocrit are common. In chronic renal failure, tubular secretion of potassium increases until oliguria develops. Use of potassium- sparring diuretics also may precipitate elevated serum potassium levels. As disease progresses, total body potassium levels can rise to life-threatening levels and dialysis is required. In early renal insufficiency, acid excretion and bicarbonate reabsorption are increase to maintain normal pH. Metabolic acidosis begins when GFR Reaches 30% to 40%. Metabolic acidosis and hyperkalemia may be severe enough to require dialysis when end-stage renal failure develops. Chronic hyperlipidemia may induce glomerular and tubolointerstitial injury, contributing to the progression of chronic renal disease.
Hematocrit Potassium balance Acid-base balance
Dyslipidemia
Laboratory test: Result Cholesterol Creatinine Glucose (FBS) Triglycerides Uric acid (BUA) Urea nitrogen (BUN) Sodium (Na) Potassium (K) Chloride(Cl) 210.6 mg/dl 14.5 mg/dl 82.mg/dl 145 mg/dl 11.8 mg/dl 91.7 mg/dl 139.4 mg/dl 4.63 mg/dl 104.5 mg/dl Normal value 0-200 0.5-1.2 74-106 0-200 91.7 6-20 135-145 3.4-4.0 92-102 Interpretation
Serology Test Anti- HCV Patient count 0.018 Cut off value 0.140 Result Non reactive
hemoglobin Hematocrit RBC WBC Neutrophils Lymphocytes Monocytes Eosinophil Platelet count
Result 129.2 .38 4.1 7.4 .65 .33 .01 .01 Adeq.
Normal values Female: 120 -160 g/l 0.37 0.47 4.0-5.5 x 10 g/l 5-10x10 g/l 0.50-0.66 0.20-0.40 0.02-0.06 0.01-0.03 150-400 x10 g/l
Interpretation
Test name HBSAg-11 Anti-HBS
Cut-off value 1.00 10.00
Patients count 0.36 2.00
result negative negative
MEDICAL MANAGEMENT: Ideal outcomes of medical management include the following: controlling blood pressure (BP) to below 130/80 mmHg managing blood glucose level to maintain HbA1c Below 7% managing hyperlipidemia with diet and cholesterol-lowering drugs(usually statins) Managing and treating emerging manifestations of renal failure including anemia, hyperphosphatemia and hyperparathyroidism, hyperkalemia, and metabolic acidosis. Preparing clients for renal replacement therapy when necessary
Reduce blood pressure Hypertension in CKD increases the risk of loss of kidney function. The lower the BP, the lower the risk of cardiovascular disease. At blood pressures above 115/75 mmHg, the risk of cardiovascular mortality doubles for each increase of 20 mmHg Systolic and 10 mm Hg diastolic BP. Clinical practice guidelines suggest that systolic BP should be maintained below 130 mmHg and diastolic BP below 80 mm Hg in people with less than 1 g proteinuria/day <125/75 mmHg in people with >1 g of proteinuria/day. Reduce serum lipids Cardiovascular mortality is elevated among people with CKD. For this reason,low-fat diets and administration of cholesterol-lowering medications, particularly statins, are indicated. The NKF recommends maintaining LDL<100mg/dl, non-HDL <130 mg/dl, and tiglycerides <500 mg/dl. Hyperlipidemia should be managed aggressively to reduce the risk of atherosclerotic cardiovascular disease.
Controlling phosphorus intake Elevations in the levels of serum phosphorus, calcium-phosphorus product, and parathyroid hormone substantially increase the risk of death. The NKF recommends that serum phosphorus level be maintained between 2.7 and 4.6 mg/dl for those with stage 3 or 4 CKD, dietary phosphorus intake should be limited, and phosphorus binders started of necessary.
Nursing management of the medical client Assessment: for any client with CKD, take a comprehensive history that includes medications and diet currently prescribed. Check blood pressure. Monitor urine studies including micro albumin and albumin levels as well as blood creatinine level, GFR, red blood cell count, and levels of electrolytes, glucose and lipids for changes suggesting increasing renal failure. Physical assessment findings that suggest progressing renal failure may include fatigue, peripheral edema, shortness of breath, adventitious lung sounds, heart murmurs or gallops, bruising, memory loss, GI disturbances, impaired wound healing, and increased infections. Control blood glucose level- dietary management, exercise, anti diabetic agents, and insulin therapy are essential aspects of managing blood glucose. Encourage smoking Cessation- Smoking cessation assistance is another important area for prevention of risk factors. The mechanisms of the effect of smoking on kidney disease progression are unclear, but studies have shown an association between smoking and decreasing renal function, smoking increases the risk of developing type 2 diabetes mellitus and micro albuminuria, and furthering progression of diabetic nephropathy. Smoking was related to the development of kidney disease in a longitudinal study of 2585 people with no previous history of kidney disease with a mean follow-up of 18.5 years, there are many nursing strategies to facilitate smoking cessation, but this is a difficult addiction to overcome and repeated and varied interventions may be necessary.
You might also like
- Chronic Kidney Disease Case PresDocument32 pagesChronic Kidney Disease Case Presnnaesor_1091No ratings yet
- Chronic Kidney Disease Case PresentationDocument14 pagesChronic Kidney Disease Case Presentationnnaesor_109150% (2)
- Chronic Kidney DiseaseDocument33 pagesChronic Kidney DiseasesexiiimammaNo ratings yet
- Case Study #3 Renal 1. LabDocument9 pagesCase Study #3 Renal 1. Labapi-207971474No ratings yet
- Case Study CKD DM Type 2Document7 pagesCase Study CKD DM Type 2Brian Cornel0% (3)
- Chronic Kidney DiseaseDocument9 pagesChronic Kidney Diseaseluvgrace100% (1)
- Case Study On Chronic Kidney DiseaseDocument101 pagesCase Study On Chronic Kidney DiseaseZNEROL100% (6)
- Chronic Kidney Disease CompilationDocument33 pagesChronic Kidney Disease CompilationGwen Stefanie Lagrimas ValloyasNo ratings yet
- Case Study On Chronic Kidney Disease Probably To Secondary HypertensionDocument18 pagesCase Study On Chronic Kidney Disease Probably To Secondary Hypertensionkyeria77% (26)
- CaseStudy ChronicRenalFailureDocument29 pagesCaseStudy ChronicRenalFailureCarlcedrick ManlapusNo ratings yet
- Pathophysio CRF RevisedDocument2 pagesPathophysio CRF Revisedroseanne18No ratings yet
- Chronic Kidney Disease Case StudyDocument52 pagesChronic Kidney Disease Case StudyGi100% (1)
- ESRD CaseDocument51 pagesESRD Casepjerry100% (1)
- Case Analysis FinalDocument29 pagesCase Analysis FinalVeyNo ratings yet
- Case Study 10 Renal FailureDocument19 pagesCase Study 10 Renal FailureAriadne Cordelette100% (2)
- CKD (F&e)Document110 pagesCKD (F&e)Al-nazer Azer Al100% (1)
- ESRD Secondary To Diabetic Nephropathy CASE STUDYDocument42 pagesESRD Secondary To Diabetic Nephropathy CASE STUDYRalph Pelegrino75% (4)
- Chronic Kidney Disease Stage 5Document21 pagesChronic Kidney Disease Stage 5Kristine Anne Soriano100% (1)
- Diabetic Neuropathy and Chronic Kidney DiseaseDocument62 pagesDiabetic Neuropathy and Chronic Kidney DiseaseMae Navidas DigdiganNo ratings yet
- Chronic Renal FailureDocument37 pagesChronic Renal Failuredorkiebaby100% (10)
- Case Study 18 CKDDocument7 pagesCase Study 18 CKDapi-301049551No ratings yet
- ESRD Secondary To Diabetic Nephropathy CASE STUDY Docx 2Document42 pagesESRD Secondary To Diabetic Nephropathy CASE STUDY Docx 2Eyerusalem100% (1)
- A Case Study On Chronic Renal DiseaseDocument17 pagesA Case Study On Chronic Renal Diseasematucojulio100% (1)
- Case Study 18Document4 pagesCase Study 18api-271284613No ratings yet
- Nephrotic SyndromeDocument35 pagesNephrotic SyndromesudhaNo ratings yet
- Acute Glomerulonephritis 42-mDocument27 pagesAcute Glomerulonephritis 42-mcbanguisNo ratings yet
- Case Study - Chronic Kidney Disease Treated With DialysisDocument7 pagesCase Study - Chronic Kidney Disease Treated With Dialysisapi-387604918100% (1)
- Acute Renal Failure Case StudyDocument18 pagesAcute Renal Failure Case Studymanjeet3680% (5)
- CKD PresentationDocument51 pagesCKD PresentationBasneyatPragyanNo ratings yet
- HNF 42 Case StudyDocument25 pagesHNF 42 Case StudyDana SablanNo ratings yet
- Chronic Kidney DiseaseDocument49 pagesChronic Kidney Diseasesarguss1471% (7)
- ESRD Case Study on Diabetic NephropathyDocument19 pagesESRD Case Study on Diabetic Nephropathylenecarglbn100% (1)
- ESRD Causes and StagesDocument63 pagesESRD Causes and StagesGregory LitangNo ratings yet
- Individual Case Study Acute GlomerulonephritisDocument26 pagesIndividual Case Study Acute GlomerulonephritisMonique ReyesNo ratings yet
- Chronic Kidney DiseaseDocument11 pagesChronic Kidney Diseasenaly23No ratings yet
- Case+Study Chronic Renal FailureDocument38 pagesCase+Study Chronic Renal Failurelynsweet100% (12)
- Hypertension Pathophysiology and Treatment PDFDocument6 pagesHypertension Pathophysiology and Treatment PDFBella TogasNo ratings yet
- CKD Case StudyDocument24 pagesCKD Case Studyapi-384366795No ratings yet
- A Case Study-FinalDocument45 pagesA Case Study-FinalJáylord OsorioNo ratings yet
- FINAL PPT of Grand Case Presentation About CKDDocument66 pagesFINAL PPT of Grand Case Presentation About CKDmaria erika94% (16)
- Individual Case Study Acute GlomerulonephritisDocument26 pagesIndividual Case Study Acute GlomerulonephritisBatrisyia HalimsNo ratings yet
- End Stage Renal Disease Case StudyDocument8 pagesEnd Stage Renal Disease Case StudyNikko Dela CruzNo ratings yet
- Chronic Renal FailureDocument3 pagesChronic Renal FailureAura Salve Ildefonso AllasNo ratings yet
- Acute Renal FailureDocument59 pagesAcute Renal Failurepaul_v_44440% (1)
- Case Study - Acute Glomerulonephritis Sample Case Study Report For PCL Level by Amrit BanstolaDocument15 pagesCase Study - Acute Glomerulonephritis Sample Case Study Report For PCL Level by Amrit BanstolaAmrit Banstola100% (5)
- Case StudyDocument37 pagesCase StudyAnonymous t78m8ku100% (1)
- CKD Case StudyDocument27 pagesCKD Case StudyMary Rose Vito100% (1)
- Age Greater Than 60 Y/o Hereditary Precipitating Factors: Hypertension Increase Protein and Fat IntakeDocument3 pagesAge Greater Than 60 Y/o Hereditary Precipitating Factors: Hypertension Increase Protein and Fat Intakenursing concept mapsNo ratings yet
- HyponatremiaDocument44 pagesHyponatremiaALi TaLib ShukurNo ratings yet
- Chronic Kidney Disease OverviewDocument12 pagesChronic Kidney Disease OverviewHalles Beverlyn Crisostomo GeraldeNo ratings yet
- Kidney Transplant in Delhi, Kidney Stone Treatment in DelhiDocument3 pagesKidney Transplant in Delhi, Kidney Stone Treatment in DelhiDr. Anant KumarNo ratings yet
- Mr. R.E.B. - CKDDocument61 pagesMr. R.E.B. - CKDChristy Rose AgrisNo ratings yet
- Managing KidneyDocument4 pagesManaging KidneyPalaNo ratings yet
- Introduction To Urinary System:-: Antilithiatic Activity of Ethanolic Extract of Dried Leaves of Fragaria Vesca Linn."Document41 pagesIntroduction To Urinary System:-: Antilithiatic Activity of Ethanolic Extract of Dried Leaves of Fragaria Vesca Linn."Rohit PatilNo ratings yet
- DR. SEBI KIDNEY FAILURE SOLUTION: Dialysis-Free Living. A Natural Approach to Treating and Preventing Chronic Kidney Disease (2022 Guide for Beginners)From EverandDR. SEBI KIDNEY FAILURE SOLUTION: Dialysis-Free Living. A Natural Approach to Treating and Preventing Chronic Kidney Disease (2022 Guide for Beginners)Rating: 5 out of 5 stars5/5 (2)
- KidneyDocument3 pagesKidneyAngelicaNo ratings yet
- Easy Renal Diet Cookbook: Ultimate Guide To Manage Kidney DiseaseFrom EverandEasy Renal Diet Cookbook: Ultimate Guide To Manage Kidney DiseaseNo ratings yet
- Spectrum September KidneyDocument29 pagesSpectrum September KidneyParth LandeNo ratings yet
- Your Amazing KidneysDocument13 pagesYour Amazing KidneysjerinthomasrajanNo ratings yet
- Funda Q and ADocument4 pagesFunda Q and ARoseben SomidoNo ratings yet
- nLE rEVIEWER 2Document1 pagenLE rEVIEWER 2Roseben SomidoNo ratings yet
- PhynetoinDocument3 pagesPhynetoinRoseben SomidoNo ratings yet
- Drug Study - Paracetamol Ambroxol, Ascorbic Acid, CefuroximeDocument4 pagesDrug Study - Paracetamol Ambroxol, Ascorbic Acid, Cefuroximeapi-3701489100% (12)
- Medical Terminology Element DefinitionsDocument6 pagesMedical Terminology Element DefinitionsRoseben SomidoNo ratings yet
- Ferrous SulfateDocument2 pagesFerrous SulfateRoseben SomidoNo ratings yet
- Funda Q and ADocument4 pagesFunda Q and ARoseben SomidoNo ratings yet
- NLE Reviewer Q and ADocument11 pagesNLE Reviewer Q and ARoseben Somido100% (1)
- DKADocument5 pagesDKARoseben SomidoNo ratings yet
- Baptism of JesusDocument3 pagesBaptism of JesusRoseben SomidoNo ratings yet
- MethergineDocument2 pagesMethergineRoseben SomidoNo ratings yet
- Vitamin CDocument3 pagesVitamin CRoseben SomidoNo ratings yet
- Drug StudyDocument14 pagesDrug Studysyd1975% (8)
- Lyrica Generic vs Brand Name GuideDocument3 pagesLyrica Generic vs Brand Name GuideRoseben Somido100% (1)
- DKADocument5 pagesDKARoseben SomidoNo ratings yet
- Medical Terminology Element DefinitionsDocument6 pagesMedical Terminology Element DefinitionsRoseben SomidoNo ratings yet
- NCP - Disturbed Body ImageDocument3 pagesNCP - Disturbed Body ImageRoseben Somido100% (1)
- Angiography Research SummaryDocument8 pagesAngiography Research SummaryRoseben SomidoNo ratings yet
- Impaired Physical MobilityDocument2 pagesImpaired Physical MobilityRoseben SomidoNo ratings yet
- NCP ConstipationDocument2 pagesNCP ConstipationRoseben Somido100% (1)
- NCP Hypertension 2Document3 pagesNCP Hypertension 2Roseben Somido50% (2)
- Altered Cerebral PerfusionDocument3 pagesAltered Cerebral PerfusionRoseben SomidoNo ratings yet
- School Age ChildDocument26 pagesSchool Age ChildRoseben SomidoNo ratings yet
- Roseben R. Somido: PATIENT: Mitra Michelle, 8 Years Old CASE: Enteric FeverDocument2 pagesRoseben R. Somido: PATIENT: Mitra Michelle, 8 Years Old CASE: Enteric FeverRoseben SomidoNo ratings yet
- Vulvitis Diagnosis and Treatment GuideDocument22 pagesVulvitis Diagnosis and Treatment GuideRoseben Somido75% (4)
- Wound DebridementDocument3 pagesWound DebridementRoseben SomidoNo ratings yet
- Roseben R. Somido: PATIENT: Delos Reyes, Lloyd: 2mos - Old CASE: Pneumonia SevereDocument2 pagesRoseben R. Somido: PATIENT: Delos Reyes, Lloyd: 2mos - Old CASE: Pneumonia SevereRoseben SomidoNo ratings yet
- Vulvitis Diagnosis and Treatment GuideDocument22 pagesVulvitis Diagnosis and Treatment GuideRoseben Somido75% (4)
- Pa Tho Physiology of Ectopic PregnancyDocument2 pagesPa Tho Physiology of Ectopic Pregnancythediaber60% (5)
- Preschooler: From 3-5 Years OldDocument44 pagesPreschooler: From 3-5 Years OldRoseben Somido100% (2)
- Platelet Rich Plasma in OrthopaedicsDocument269 pagesPlatelet Rich Plasma in OrthopaedicsBelinda Azhari SiswantoNo ratings yet
- In This Issue: Wound Infection and ColonisationDocument7 pagesIn This Issue: Wound Infection and ColonisationSeftiana WahyuniNo ratings yet
- Traumatic Brain Injury PresentationDocument14 pagesTraumatic Brain Injury Presentationapi-413607178No ratings yet
- Surya Namaskar ExplanationDocument17 pagesSurya Namaskar Explanationnaresh08No ratings yet
- STD X - Biology - Paper VI FinalDocument8 pagesSTD X - Biology - Paper VI FinalYashodhaNo ratings yet
- Human Motivation Edited2Document23 pagesHuman Motivation Edited2jingoNo ratings yet
- Diagram Human Heart Kel 1Document3 pagesDiagram Human Heart Kel 1Rahma SafitriNo ratings yet
- Tarot Study Journal TDM Rws Thoth SKTDocument378 pagesTarot Study Journal TDM Rws Thoth SKTBrigita NemetNo ratings yet
- Soal BiomolekulerDocument3 pagesSoal BiomolekuleralmasyifaNo ratings yet
- Pathophysiology of BREAST CANCERDocument1 pagePathophysiology of BREAST CANCERAlinor Abubacar100% (6)
- Clinical Manual of Otolaryngology Clear ScanDocument283 pagesClinical Manual of Otolaryngology Clear ScanAyman Yakout100% (4)
- School: San Agustin Elementary School Grade Level: Six Teacher: Jonalvin A. Ke Learning Area: Science Date: SEPTEMBER 5, 2018 (WEDNESDAY)Document3 pagesSchool: San Agustin Elementary School Grade Level: Six Teacher: Jonalvin A. Ke Learning Area: Science Date: SEPTEMBER 5, 2018 (WEDNESDAY)Jonalvin KENo ratings yet
- ECG Interpretation BookDocument57 pagesECG Interpretation BookLouis Plan100% (2)
- Chapter 41 - Thoracic Outlet Syndrome SynonymsDocument8 pagesChapter 41 - Thoracic Outlet Syndrome SynonymsPiero Massafra100% (1)
- Practical 14 PDFDocument3 pagesPractical 14 PDFSiddharth KumraNo ratings yet
- IGCSE Biology 2015 Paper 21Document20 pagesIGCSE Biology 2015 Paper 21VeronicaAndrianNo ratings yet
- Naziya & JignaDocument44 pagesNaziya & Jignakishan100% (1)
- BugSpeaks Sample ReportDocument27 pagesBugSpeaks Sample ReportAnonymous 76wOMTpNo ratings yet
- Oral Histology Quiz - Scientific Term (AmCoFam)Document22 pagesOral Histology Quiz - Scientific Term (AmCoFam)AmericanCornerFamily100% (5)
- MKFP Mat-Xs Clinical 16052012 enDocument8 pagesMKFP Mat-Xs Clinical 16052012 ensuharyantoNo ratings yet
- 1 Digestion and AbsorptionDocument12 pages1 Digestion and AbsorptionJared Dela cruzNo ratings yet
- Optimizing Ba and Iba Concentrations For Micro Propagation of Spineless Yucca Yucca Elephantipes IJERTV8IS010004Document5 pagesOptimizing Ba and Iba Concentrations For Micro Propagation of Spineless Yucca Yucca Elephantipes IJERTV8IS010004SHUBHAM JIBHAKATENo ratings yet
- Listening Skiill NotesDocument7 pagesListening Skiill Notesvivian nyariboNo ratings yet
- Ventilation Perfusion RatiosDocument22 pagesVentilation Perfusion Ratiosنمر نصارNo ratings yet
- Animal Kingdom (Phylum 1-7)Document4 pagesAnimal Kingdom (Phylum 1-7)AllenNo ratings yet
- Muscle Fiber Number in Biceps Brachii in Bodybuilders and Control SubjectsDocument5 pagesMuscle Fiber Number in Biceps Brachii in Bodybuilders and Control SubjectswaelNo ratings yet
- Homeopathy For AsthmaDocument12 pagesHomeopathy For AsthmasksmilyinNo ratings yet
- Types of Plant HormonesDocument6 pagesTypes of Plant HormonesKarren ReyesNo ratings yet
- Cysteine, Methionine, ProlineDocument3 pagesCysteine, Methionine, ProlineRio BurlazaNo ratings yet
- Pathophysiology of Clinical Benign Prostatic Hyperplasia: SciencedirectDocument6 pagesPathophysiology of Clinical Benign Prostatic Hyperplasia: SciencedirectMuhammad Fuad MahfudNo ratings yet