Professional Documents
Culture Documents
J 1365-277X 2011 01189 X
Uploaded by
SunardiasihOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
J 1365-277X 2011 01189 X
Uploaded by
SunardiasihCopyright:
Available Formats
Journal of Human Nutrition and Dietetics
RESEARCH PAPER
Simple nutritional intervention in patients with advanced cancers of the gastrointestinal tract, non-small cell lung cancers or mesothelioma and weight loss receiving chemotherapy: a randomised controlled trial
C. Baldwin,* A. Spiro,* C. McGough,* A. R. Norman, A. Gillbanks,* K. Thomas, D. Cunningham,* M. OBrien* & H. J. N. Andreyev*
*Department of Medicine Royal Marsden Hospital, London and Sutton, UK Diabetes and Nutritional Sciences Division, School of Medicine, Kings College London, London, UK Department of Computing, Royal Marsden Hospital, London and Sutton, UK
Keywords cancer, chemotherapy, dietary advice, oral nutritional supplement, quality of life, survival, weight loss. Correspondence J. Andreyev, The GI Unit, Department of Medicine, Royal Marsden Hospital, Fulham Road, London SW3 6JJ, UK. Tel.: +44 (0) 207 811 8216 Fax: +44 (0) 207 811 8107 E-mail: j@andreyev.demon.co.uk doi:10.1111/j.1365-277X.2011.01189.x
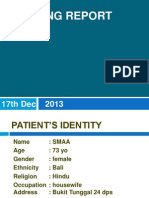
Abstract Background: Weight loss in patients with cancer is common and associated with a poorer survival and quality of life. Benets from nutritional interventions are unclear. The present study assessed the effect of dietary advice and/or oral nutritional supplements on survival, nutritional endpoints and quality of life in patients with weight loss receiving palliative chemotherapy for gastrointestinal and non-small cell lung cancers or mesothelioma. Methods: Participants were randomly assigned to receive no intervention, dietary advice, a nutritional supplement or dietary advice plus supplement before the start of chemotherapy. Patients were followed for 1 year. Survival, nutritional status and quality of life were assessed. Results: In total, 256 men and 102 women (median age, 66 years; range 24 88 years) with gastrointestinal (n = 277) and lung (n = 81) cancers were recruited. Median (range) follow-up was 6 (049) months. One-year survival was 38.6% (95% condence interval 33.343.9). No differences in survival, weight or quality of life between groups were seen. Patients surviving beyond 26 weeks experienced signicant weight gain from baseline to 12 weeks, although this was independent of nutritional intervention. Conclusions: Simple nutritional interventions did not improve clinical or nutritional outcomes or quality of life. Weight gain predicted a longer survival but occurred independently of nutritional intervention. (non-small cell) cancers or mesothelioma who have lost weight are a reduced response to chemotherapy and the fact that patients experience increased toxicity from treatment, as a result of which a smaller total amount of chemotherapy can be given (Andreyev et al., 1998) (Ross et al., 2004). This provides a rationale to investigate whether improving the nutritional status of patients might lead to improved clinical outcomes. Weight loss in patients with cancer may be managed by dietetic interventions, which aim to increase oral nutritional intake. These interventions include nutritional counselling to increase food intake, modication of the
431
Introduction Adequately powered, randomised, controlled clinical trials are lacking to inform current international guidelines for the nutritional management of patients with cancer (Arends et al., 2006). Patients with cancer frequently have weight loss at the time of diagnosis and, in patients receiving palliative chemotherapy, weight loss predicts a signicantly shorter survival and poorer quality of life (DeWys et al., 1980). Amongst the known reasons for poorer outcomes in patients with cancers of the gastrointestinal tract, lung
2011 The Authors Journal of Human Nutrition and Dietetics 2011 The British Dietetic Association Ltd. 2011 J Hum Nutr Diet, 24, pp. 431440
Oral nutritional interventions in cancer and weight loss
C. Baldwin et al.
energy density of meals and the prescription of oral nutritional supplements. Oral nutritional supplements are available on prescription and, theoretically, are easy to use. In the UK, the cost of prescribed nutritional supplements is well in excess of 100 million per annum and studies of patient usage of prescribed supplements have highlighted potential problems with compliance (Fearon et al., 2003). An alternative to the prescription of expensive nutritional supplements is to help patients modify their normal food intake. Manipulation of food intake has potential advantages in that it may offer greater variety, be better tailored to individual needs and, if effective, may reduce healthcare costs. The small number of studies that have examined the efcacy of the dietary management of weight loss in cancer have suggested that oral nutritional interventions result in an increase in energy and nutrient intake and may be associated with benets to quality of life in some groups (Arnold & Richter, 1989; Ravasco et al., 2005a,b; Isenring et al., 2007), although they have consistently failed to demonstrate an impact on clinical and functional outcomes. However, all the studies of simple nutritional interventions reported to date have been signicantly underpowered to demonstrate whether they alter clinical outcomes (Brown, 2002; Arends et al., 2006; Elia et al., 2006). Despite this, it has been argued that simple nutritional interventions may be futile in the management of weight loss in patients with cancer who are receiving chemotherapy (Koretz et al., 2007) and that efforts should be focused on the use of agents that modulate the inammatory processes associated with cachexia (Skipworth & Fearon, 2007; Fearon, 2008). In the absence of adequately powered studies assessing the impact of simple nutritional interventions on important clinical endpoints such as survival, quality of life or nutritional status in patients with advanced cancer receiving palliative chemotherapy, this large randomised trial aimed to determine whether such simple interventions are useful. Materials and methods Study design This prospective, randomised, controlled trial was approved by research and development and ethics committees for all participating centres. It was also reviewed and adopted into the portfolio of the National Cancer Research Network, UK. All enrolled patients provided their written informed consent before randomisation. Subjects Adults with histologically proven, metastatic or locally advanced tumours of the gastrointestinal tract
432
(oesophagus, stomach, pancreas, liver and biliary tract, colon and rectum), non-small cell lung (NSCL) cancer or mesothelioma were eligible for recruitment if they had lost any weight in the 3 months before presentation, had agreed to undergo palliative chemotherapy and were t for chemotherapy according to standard local criteria. Patients were not eligible if they were unable, or unwilling, to provide informed consent to randomisation, had a clinical condition precluding oral nutrition, were unable to tolerate milk or it was considered that they should receive immediate enteral or parenteral nutrition. Interventions Participating patients were randomly allocated to one of four groups: Group 1 received no dietary intervention. Group 2 received advice to increase food intake by an additional 2510 kJ (600 kcal) per day, which is the amount recommended to achieve weight gain (Todorovic & Micklewright, 2004). Consistency of advice was maintained by providing a booklet, which set out a selection of commonly used snack foods, drinks and desserts in portion sizes each providing 628 kJ (150 kcal). Participants were asked to select four items daily from the booklet, in addition to their usual food intake, and were guided to consider suitable choices. Group 3 received one sachet of nutritional supplement [either ScandiShake (SHS International, Liverpool, UK) or Calshake (Fresenius-Kabi, Runcorn, UK)] per day, which provided 2460 kJ (588 kcal), when prepared in 240 mL of fullcream milk. Patients were provided with a selection of both supplements and with assorted avours at the time of randomisation and could choose which product to take, according to preference. Patients were guided to t the supplements into their existing meal pattern. In addition, this group received a daily multivitamin and mineral supplement, either a capsule (Forceval; Unigreg, Morden, UK), tablet or effervescent formulation (Supradyn; Roche, Welwyn, UK), according to preference. Group 4 received advice to increase food intake by 250 kJ (600 kcal) per day and one sachet of the nutritional supplements and vitamin preparations as given to groups 2, 3 and 4. All patients were assessed, recruited and followed up by trained, trial dietitians. Advice given to patients in the three intervention groups was supported by written information and they were followed-up at subsequent outpatient appointments and via weekly telephone calls for 6 weeks. Encouragement was given to continue with the intervention and patients were encouraged to discuss any problems that they experienced. No dietary information was given during the telephone calls to participants in the no dietary intervention group.
2011 The Authors Journal of Human Nutrition and Dietetics 2011 The British Dietetic Association Ltd. 2011 J Hum Nutr Diet, 24, pp. 431440
C. Baldwin et al.
Oral nutritional interventions in cancer and weight loss
The primary endpoint of the study was mortality. The secondary endpoints were change in nutritional status, energy intake and quality of life. Timing of intervention and assessments The initial randomisation and intervention took place as early as possible before the start of chemotherapy. The trial intervention period was for 6 weeks only. After 6 weeks, participants were allowed to continue with their nutritional intervention(s), if desired, but did not continue to receive regular weekly encouragement. Patients were followed for 1 year after randomisation or until death. Data were collected at baseline, 6 weeks (end of the intervention period) and at 3, 6 and 12 months after randomisation. These data included: height, weight, handgrip strength and quality of life data, using questionnaires from the European Organisation for Research and Treatment of Cancer (EORTC-C30) (Aaronson et al., 1993) and Functional Assessment of Cancer Therapy (FAACT) (Cella et al., 1993) (baseline, 6 weeks and 26 weeks only) and performance status (World Health Organization). The date of death was recorded. Compliance with dietary interventions and change in energy intake was assessed in patients with gastrointestinal cancers recruited at the Royal Marsden Hospital (n = 236) using 3-day food diaries. Patients were shown how to complete their diaries at the same time as they were given patient information sheets about the study, and they were asked to complete the diary before their next appointment if they decided to participate in this trial. All patients randomised to receive a supplement were also asked to complete a diary of volume of supplement usage daily for 6 weeks. For assessment purposes, foods recorded descriptively in the 3-day diaries were converted to weights using standard portions. Dietary data were analysed using dietplan5 (Foresteld Software Ltd, Horsham, UK). Randomisation Randomisation was performed by the independent randomisation ofce of the Institute of Cancer Research, after stratifying patients according to the two known prognostic factors for gastrointestinal cancer: disease site and performance status. Eligibility was checked by the independent study monitor and randomisation was performed using random permuted blocks. Group allocation was concealed from both the investigator and patient until consent to enter the trial had been obtained. Study personnel were not blinded to treatment group.
Statistical analysis Where data were normally distributed, the appropriate parametric test was used. Data on continuous variables, such as weight, handgrip strength and energy intake results, were analysed using appropriate tests including, analysis of variance, two-sample t-tests or the Mann Whitney U-test depending on the distribution of the data collected. A Friedman test was used to compare mean weight at each time point. Two-by-two factorial analysis was used to compare groups receiving dietary advice with groups receiving no dietary advice and groups receiving nutritional supplements with no nutritional supplement. Overall survival was derived using the product-limit method of KaplanMeier, which allowed patients lost to follow-up (censored observations) to be included in the analysis. The log-rank test was used to evaluate differences in survival curves. Cox multivariate analysis was used to examine survival differences between comparison groups (supplement versus no supplement and dietary advice versus no dietary advice) after correcting for known prognostic factors. The results are reported as hazard ratios. Power calculation The primary outcome measure was survival at 1 year. When the trial was conceived, recent results from a large patient dataset from our unit has shown that patients with advanced tumours of the gastrointestinal tract (all sites), presenting for treatment with no weight loss have a 1-year survival rate of 50%, whereas patients who have lost weight at presentation have a 1-year survival rate of 30% (Andreyev et al., 1998). To detect an increase in 1-year survival of 10% in those patients who had lost weight, it was calculated that, if a total of 660 patients were randomised, the study had at least 80% statistical power, with an alpha of 0.05 (two-sided test), to detect a difference between either of the two arms of the stratications (i.e. supplement versus no supplement and dietary advice versus no dietary advice). Data monitoring/patient safety The protocol stipulated that an independent data monitoring committee would review the data after 200 patients had been randomised, and at additional time-points subsequently specied by the committee. Results From 2002 to 2004, patients with gastrointestinal malignancy were recruited from a single centre. Subsequently,
433
2011 The Authors Journal of Human Nutrition and Dietetics 2011 The British Dietetic Association Ltd. 2011 J Hum Nutr Diet, 24, pp. 431440
Oral nutritional interventions in cancer and weight loss
C. Baldwin et al.
the trial was extended to patients with NSCL cancer and mesothelioma. After 2005, four additional UK centres (Maidstone, Guilford, Coventry, Birmingham) and one Australian centre (Melbourne) became involved. The trial was stopped prematurely in 2006 on the advice of the independent data monitoring committee. At that point, 358 patients (256 men and 102 women) had been randomised. The groups were well balanced for all baseline characteristics (Table 1). The median followup was 189 days (6 months) with a range of 01485 days (049 months). Fourteen patients had no follow-up and a further four patients had <1 month follow-up as a result of early death or withdrawal from the trial (Fig. 1). Nutritional intervention and survival Overall 1-year survival was 38.6% [95% condence interval (CI) 33.343.9]. There were no signicant differences in overall survival between any of the groups (Fig. 2 and Table 2).
Patients with a performance status of two or more had signicantly poorer survival than patients with performance status 0 or 1 (21.4% (95% CI 12.931.3) (PS2) versus 43.0% (95% CI 35.651.0) (PS1) and 65.5 (95% CI 42.681) (PS0) respectively). Patients with colorectal tumours had signicantly better 1-year survival (55.8%; 95% CI 46.965.5) than patients with oesophago-gastric and pancreatic (29.6%; 95% CI 22.237.4) or lung tumours (32.3%; 95% CI 21.643.5). No differences in survival were detected from nutritional intervention within these sub groups. Nutritional intervention and quality of life Data on quality of life were collected using two questionnaires (EORTC-C30 and FAACT) at baseline, and at 6 and 26 weeks. A small number of the whole range of questions from each questionnaire were not completed by patients. Therefore, data were available from the EORTCC30 questionnaire from 302310 patients at baseline, 213233 patients at 6 weeks and 118129 patients at
Table 1 Baseline characteristics of patients recruited to the trial of nutritional intervention for weight loss in cancer Subdivided according to intervention Nutritional supplement alone (Group 3) 86 (24%) 66.5 (3888) 64 (25%) 22 (22%) 17 (24%) 18 (25%) 3 (30%) 27 (24%) 19 (23.5%) 1 (14%) 1 (25%) 7 (30.5%) 39 (21%) 21 (26.25%) 1 (25%) Dietary advice + nutritional supplement (Group 4) 86 (24%) 68 (4286) 57 (22%) 29 (28%) 18 (25%) 20 (28%) 0 27 (24%) 18 (22%) 2 (29%) 1 (25%) 7 (30.5%) 48 (26%) 17 (21.25%) 0
Total
No intervention (Group 1)
Dietary advice alone (Group 2) 90 (25%) 66 (2484) 66 (26%) 24 (24%) 19 (27%) 16 (22%) 3 (30%) 30 (26%) 19 (23.5%) 1 (14%) 2 (50%) 4 (17%) 50 (27%) 17 (21.25%) 2 (50%)
Number 358 96 (27%) Age (years) Median 66.8 65.5 (range) (2488) (3385) Gender Male 256 69 (27%) Female 102 27 (26%) Site of primary tumour Oesophago-gastric 71 17 (24%) Pancreas 72 18 (25%) Liver and biliary 10 4 (40%) Colorectal 113 29 (26%) Lung 81 25 (31%) Unknown primary 7 3 (43%) Other 4 0 Performance status (World Health Organization) 0 23 5 (22%) 1 184 47 (26%) 2 80 25 (31.25%) 3 4 1 (25%) Unavailable 67 Centre Royal Marsden Hospital 299 76 (25%) Guildford 27 11 (41%) Maidstone 18 5 (28%) Melbourne 10 2 (20%) Birmingham 3 2 (67%) Walsgrave 1 0
78 (26%) 5 (18%) 4 (22%) 3 (30%) 0 0
75 (25%) 3 (11%) 3 (17%) 3 (30%) 1 (33%) 1 (100%)
70 (24%) 8 (30%) 6 (33%) 2 (20%) 0 0
434
2011 The Authors Journal of Human Nutrition and Dietetics 2011 The British Dietetic Association Ltd. 2011 J Hum Nutr Diet, 24, pp. 431440
C. Baldwin et al.
Oral nutritional interventions in cancer and weight loss
Figure 1 Consort owchart of participant progression through a randomised controlled trial of nutritional intervention in the management of advanced cancer. RMH, Royal Marsden Hospital.
26 weeks. Data were available from the FAACT questionnaire on 308313 patients at baseline, 229237 patients at 6 weeks and 132 patients at 26 weeks. Changes in each parameter of quality of life from baseline to 6 and 26 weeks were not signicantly different between the groups receiving dietary advice compared to no dietary advice, as well as oral nutritional supplements compared to no oral nutritional supplements, for any parameter (data not shown). Nutritional intervention and nutritional status Weight loss at trial entry varied across the whole group (range 1.135.0%). The mean (SD) weight loss for patients with gastrointestinal tumours was
11.2% (6.4%) and 9.8% (6.0%) for lung cancer patients. The mean weight changes from baseline to 6 weeks and baseline to 26 weeks were small and there were no statistically signicant differences between groups (Table 3). The mean weight change at 52 weeks for all surviving patients varied in the range 1.364.78 kg according to intervention group (Table 3). Patients randomised to receive dietary advice compared to no dietary advice were signicantly heavier at 1 year (P = 0.04), although the numbers involved (n = 68) are small and this nding should be interpreted with caution. There was no signicant difference in weight at 1 year between those receiving a nutritional supplement compared to those not receiving supplements. No signicant difference was found when
435
2011 The Authors Journal of Human Nutrition and Dietetics 2011 The British Dietetic Association Ltd. 2011 J Hum Nutr Diet, 24, pp. 431440
Oral nutritional interventions in cancer and weight loss
C. Baldwin et al.
Figure 2 Percentage survival according to group allocation.
were interrogated according to whether patients did or did not survive beyond 26 weeks. Comparison of mean weight change data for survivors with nonsurvivors from baseline to 6 weeks revealed no signicant differences between groups (P = 0.434) (Fig. 3), although a trend towards less weight loss in patients who survived beyond 26 weeks was seen. Mean weight change from baseline to 12 weeks was greater in survivors beyond 26 weeks (P = 0.002) (Fig. 3) [mean (SD) weight change from baseline to 12 weeks in survivors 0.58 (2.47) kg and nonsurvivors )0.66 (3.76) kg]. This nding was independent of group allocation, suggesting that weight gain is primarily associated with survival and not nutritional intervention and thus, possibly, is a surrogate marker of tumour response to chemotherapy. Hand grip strength Data on handgrip strength were only collected for patients treated at the Royal Marsden Hospital (n = 282). The mean changes at all time-points were small and there were no signicant differences between groups (data not shown). Compliance with nutritional interventions Food diaries were given to 236 patients, of whom only 60 (25%) completed one at baseline and 40 (17%) completed one at more than one time-point. The reasons for noncompletion of a second food diary were deterioration in health or premature death. Analysis of these was considered futile in view of the sample size. Diaries of supplement intake were returned by 62 (41%) of 150 patients. Recorded compliance with the prescribed quantity of supplement fell after the rst week of study. In the rst week, 31% of patients reported taking all of the prescribed supplement and ve patients 8% reported being
Table 2 One-year survival rate subdivided by intervention group Group No advice Dietary advice No nutritional supplement Nutritional supplement No intervention Any intervention (advice and/or supplement) Hazard ratio adjusted (95% condence interval) 1.00 0.840 (0.6531.08) 1.00 1.016 (0.7911.306) 1.00 0.977 (0.7331.302)
this analysis was repeated including all patients missing at 1 year (intention-to-treat analysis), assuming zero change since the last available measurement. Factors predicting weight gain Mean weight at each time-point according to group allocation and site of primary tumour did not differ between groups, although the SDs were wide. Therefore, mean weight change from baseline to 6 weeks and to 12 weeks
Table 3 Mean weight (kg) and weight change from baseline to 6 and 26 weeks, in a randomised controlled trial of nutritional intervention for weight loss in cancer, subdivided by intervention group Mean (SD) change (kg): as treated 6 weeks )0.20 (3.5) (n = 132) )0.43 (3.6) (n = 141) 0.07 (3.7) (n = 127) )0.66 (3.5) (n = 146) 26 weeks 0.41 (6.0) (n = 115) 0.11 (6.1) (n = 122) 0.58 (6.1) (n = 113) )0.04 (6.0) (n = 124) 52 weeks 4.78 (5.0)* (n = 31) 1.36 (7.5)* (n = 37) 3.41 (5.8) (n = 38) 2.30 (8.1) (n = 30) Mean (SD) change (kg): intention-to-treat analysis 6 weeks )0.16 (3.1) )0.36 (3.3) 0.06 (3.3) )0.55 (3.2) 26 weeks 0.06 (5.2) (n = 167) )0.16 (5.3) (n = 168) 0.22 (5.3) (n = 159) )0.29 (5.2) (n = 176) 52 weeks 0.12 (5.3) )0.29 (5.9) 0.21 (5.4) )0.35 (5.8)
Intervention Dietary advice No dietary advice Nutritional supplement No nutritional supplement
Mean (SD) weight (kg) at baseline 70.3 (13.0) (n = 167) 70.0 (13.4) (n = 168) 69.4 (13.3) (n = 159) 70.8 (13.2) (n = 176)
*Statistically signicant difference between dietary advice and no dietary advice at 52 weeks (P = 0.04).
2011 The Authors Journal of Human Nutrition and Dietetics 2011 The British Dietetic Association Ltd. 2011 J Hum Nutr Diet, 24, pp. 431440
436
C. Baldwin et al.
Oral nutritional interventions in cancer and weight loss
Figure 3 The magnitude of weight change from (a) baseline to 6 weeks and (b) baseline to 12 weeks according to survival. 95% CI, 95% condence interval.
unable to take any supplement. The number of patients able to take the full prescription decreased to 19% by week 6 and the number of patients being unable to take any supplement increased six-fold, to 48% by week 6. Discussion The primary endpoint of this randomised controlled trial was to assess whether a simple, very modest nutritional intervention in patients with weight loss receiving palliative chemotherapy improves survival. The trial was stopped early by the independent data monitoring committee because no benet was seen after randomisation of 358 patients. Of the secondary endpoints examined, the study demonstrated that oral nutritional interventions based on dietary advice or supplements had no effect on nutritional status or quality of life. There are no previously published studies of simple nutritional interventions for the management of weight loss in patients receiving palliative chemotherapy that have been powered to examine clinical endpoints. However, the limited data that do exist (Brown, 2002) have suggested that nutritional intervention probably does not improve clinical endpoints or the quality of life in patients receiving chemotherapy. The ndings of the present study are in agreement with this conclusion. The effects of nutritional intervention in these previous small studies on weight change were variable. In the present study, we have shown that weight gain was associated with an improved survival, although this effect was independent of nutritional intervention and the site of disease, suggesting that weight gain may be a marker of treatment success rather than a positive effect of nutritional intervention. The inability to detect any clinical benet in the present study may have been a result of the choice of
intervention. The supplements used in the present study were chosen after an earlier randomised and blinded evaluation of a variety of supplements and were clearly the preferred choice (Rahemtulla et al., 2005). Despite this and the very limited nature of the dietary prescription requested of participants, fewer than 50% of patients complied in the rst week and this number declined to 19% by 6 weeks. A systematic review of dietary advice and nutritional supplements in the management of weight loss has demonstrated benets to weight gain, with interventions providing as little as an additional 11.25 kJ (250300 calories) per day (Baldwin & Weekes, 2008). Our ndings suggest that patients struggled to comply with a modest increase in nutritional intake for 6 weeks. Failure of the patients to take the intervention mean that it is difcult to draw conclusions about the efcacy of nutritional interventions in this population and highlight difculties inherent in studying the effects of nutritional interventions in this group. The supplements options were milk-based. Lactose intolerance during 5-uouracil-based chemotherapy has been reported in a proportion of patients (Parnes et al., 1994). It is possible that this contributed to decreasing compliance over time, although it is very unlikely to have inuenced compliance in the early weeks of treatment. The interventions were supported by regular contact with the trial dietitian for the rst 6 weeks. After this time, patients were free to continue with interventions but received less intensive support, which may have accounted for the failure to nd clinical benets. There is insufcient information to determine the optimal length of intervention. The majority of dietetic interventions in a trial setting are given for 3 months or less (Baldwin & Weekes, 2008), and it is unknown whether this represents a reasonable goal in clinical practice. However, the poor compliance recorded by those prescribed supplements
437
2011 The Authors Journal of Human Nutrition and Dietetics 2011 The British Dietetic Association Ltd. 2011 J Hum Nutr Diet, 24, pp. 431440
Oral nutritional interventions in cancer and weight loss
C. Baldwin et al.
(albeit obtained from approximately half the cohort only) strongly suggests that continuing this intervention for longer would not have produced additional benet. It is not possible to determine whether persevering longer with the food options to increase energy intake, carefully tailored to usual habits and food preferences, would have been benecial because so few patients in the study group completed food diaries. There is no gold standard for the assessment of compliance with dietary interventions. A variety of methods used in other studies, including prescription charts for hospital patients (Lawson et al., 2000), supplement consumption records (Fearon et al., 2003) and counting of cans or packs on home visits and wards (Bruce et al., 2003; Gosney, 2003), are all known to be inaccurate. In the present study, it was difcult to retrieve supplement diaries from patients after 6 weeks. Information on why patients were unwilling or unable to comply with the prescription was not collected. Studies of compliance with nutritional regimens have concentrated on whether patients are compliant or not (Lawson et al., 2000; Bruce et al., 2003; Gosney, 2003), rather than exploring the factors inuencing this. The present study had some limitations. It was stopped on the advice of an independent data monitoring committee prematurely. The original power calculation was based on the likelihood of nding an improvement in survival at 1 year increasing from 30% to 40%, which would equate to a hazard ratio of 0.76. The study had 80% power to detect this change. After randomisation of 358 patients, post hoc calculation (conditional power) requested by the data monitoring committee demonstrated that there was only a 6% probability for groups receiving nutritional supplements, and a 1% probability for groups receiving dietary advice, of observing a signicant treatment effect, if the trial had been continued to full accrual, assuming that the projected true hazard ratio was 0.76. At the time the trial was stopped, only half of the predicted number of deaths had occurred. The present study was initially powered using outcomes in 1500 consecutive patients with gastrointestinal cancers treated in our unit over the previous 10 years (Andreyev et al., 1998). The overall survival of patients in the study had improved above the levels used in the power calculation and reects improvements in the management of gastrointestinal and lung cancers. Independent data suggest that outcomes in our patient cohort are not simply a statistical aberration because they do not differ from those in other cohorts (Katopodis et al., 2004). The present study was opened to patients with lung cancer after 18 months to address difculties with recruitment. Patients with lung cancer have a different disease
438
from patients with gastrointestinal cancer and it is possible that the inclusion of patients with lung cancer may have inuenced the ndings of the study. The addition of patients with NSCL cancer and mesothelioma was considered to be reasonable in view of a study that showed almost identical outcomes in these patients with and without weight loss to the gastrointestinal patients (Ross et al., 2004). Other possible confounding factors are the possibility that patients obtained nutritional information from alternative sources to the study dietitian. Additionally, the trial dietitians were not blinded to treatment group. These are major methodological issues relating to the conduct of randomised controlled trials of dietetic interventions (Baldwin et al., 2008) and issues relating to this have been reported in previous trials (Lundholm et al., 2004). This may have inuenced assessment of the subjective outcomes. Third, the EORTC-C30 was one of the questionnaires used to assess quality of life. This questionnaire has been developed and validated for use in patients with cancer, although it is possible that this questionnaire is too generic, such that important quality of life issues specic to individual disease sites might have been missed. We attempted to capture the food-related aspects of quality of life by using FAACT, a quality of life questionnaire focusing on nutritional issues associated with weight loss, although this did not detect differences between groups. In the absence of a questionnaire designed to measure the impact of nutrition on quality of life, it remains a difcult relationship to investigate (Barr & Schumacher, 2003). The present study represents the largest, randomised controlled trial of nutritional intervention in patients with cancer and weight loss receiving palliative chemotherapy performed to date. The study failed to demonstrate that signicant improvements in clinical, nutritional and quality of life end-points could be achieved with simple nutritional interventions. Acknowledgments We would like to thank Jacqui Oates for her help with obtaining and recording data collected in the study and for maintaining all the trial paperwork. We also thank everyone in the GI Trials Unit for the support given to the study. We are very grateful to those who collaborated in recruiting patients at other centres. They include: St Lukes, Guildford: Dr Marianne Illsley, Tanya Klopper, Dr Gary Middleton and Dr Clare Topham; Maidstone Oncology centre: Carol Drabble, Dr Mark Hill and Dr Justin Waters; Austin Hospital, Heidelberg, Australia: Leonie Pearce, Olive Schmid and Dr Neil Tebbutt; Birmingham Heartlands: Dr Joyce Thompson and Fiona
2011 The Authors Journal of Human Nutrition and Dietetics 2011 The British Dietetic Association Ltd. 2011 J Hum Nutr Diet, 24, pp. 431440
C. Baldwin et al.
Oral nutritional interventions in cancer and weight loss
Underwood; Coventry: Dr Caroline Humber, Gordon ONeil, Mrs J Travis and Dr Sharmila Sothi. We are also very grateful to the members of the independent data monitoring committee who spent a great deal of unpaid time reviewing the data on two separate occasions. They include: Dr Roger Ahern, Professor Marinos Elia and Dr Kevin Harrington. We thank Peter Milligan, Kings College London for additional statistical input. Approval: This study was approved by the R&D and Ethics Committees of all the participating centres. Registration with clinical trials register: ISRCTN86266498. Conict of interest, source of funding and authorship Nutritional supplements and vitamin supplements used in this study were provided free by Nutricia Clinical Care (Trowbridge, UK), Fresenius Kabi Ltd (Runcorn, UK), Unigreg Ltd (Morden, UK) and Roche Products Ltd (Welwyn Garden City, UK). This study was funded by grants from The Henry Smith Charity and The Special Trustees of the Chelsea & Westminster Hospital, London. We acknowledge NHS funding to the NIHR Biomedical Research Centre. CB helped design the study, recruited many of the patients, helped with the analysis and wrote many of the drafts of this manuscript. AS recruited all the lung cancer patients and helped with the writing of the drafts. CMcG recruited and followed up many of the patients for the study. ARN designed and powered the study and analysed all the data for the interim analyses. AG was the data manager who handled all the data generated by the study, entered it into the trial data base and coordinated all the multiple site permissions. KT performed all the statistical data analysis at the end of the study. DC was involved in the conceptual design of the study, facilitated the recruitment of patients to the trial and funded the data manager for this trial. MOB was involved in the conceptual design of the study and facilitated the recruitment of patients to the trial. HJNA conceived and wrote the study protocol, contributed and edited all drafts of this manuscript, funded the additional funds required to pay all the research dietitians and is the guarantor for this study. All authors have critically reviewed the manuscript and approved the nal version submitted for publication. References
Aaronson, N.K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N.J., Filiberti, A., Flechtner, H., Fleishman, S.B., de Haes, J.C.J.M., Kaasa, S., Klee, M., Osoba, D., Razavi, D., Rofe, P.B., Schraub, S., Sneeuw, K., Sullivan, M. & Takeda, F. (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-
life instrument for use in international clinical trials in oncology. J. Natl Cancer Inst. 85, 365376. Andreyev, H.J.N., Norman, A.R., Oates, J. & Cunningham, D. (1998) Why do patients with weight loss have a worse outcome when undergoing chemotherapy for gastrointestinal malignancies? Eur. J. Cancer 34, 503509. Arends, J., Bodoky, G., Bozzetti, F., Fearon, K., Muscaritoli, M., Selga, G., van Bokhorst-de van der Schueren, M.A., von Meyenfeldt, M., Zurcher, G., Fietkau, R., Aulbert, E., Frick, B., Holm, M., Kneba, M., Mestrom, H.J. & Zander, A. (2006) ESPEN Guidelines on Enteral Nutrition: non-surgical oncology. Clin. Nutr. 25, 245259. Arnold, C. & Richter, M.P. (1989) The effect of oral nutritional supplements on head and neck cancer. Int. J. Radiat. Oncol. Biol. Phys. 16, 15951599. Baldwin, C. & Weekes, C.E. (2008) Dietary advice for illnessrelated malnutrition in adults. Cochrane Database Syst. Rev., CD002008. Baldwin, C., Weekes, C.E. & Campbell, K.L. (2008) Measuring the effectiveness of dietetic interventions in nutritional support. J. Hum. Nutr. Diet. 21, 303305. Barr, J.T. & Schumacher, G.E. (2003) The need for a nutrition-related quality-of-life measure. J. Am. Diet. Assoc. 103, 177180. Brown, J.K. (2002) A systematic review of the evidence on symptom management of cancer-related anorexia and cachexia. Oncol. Nurs. Forum 29, 517532. Bruce, D., Laurance, I., McGuiness, M., Ridley, M. & Goldswain, P. (2003) Nutritional supplements after hip fracture: poor compliance limits effectiveness. Clin. Nutr. 22, 497500. Cella, D.F., Tulsky, D.S., Gray, G., Saraan, B., Linn, E., Bonomi, A., Silberman, M., Yellen, S.B., Winicour, P. & Brannon, J. (1993) The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J. Clin. Oncol. 11, 570579. DeWys, W.D., Begg, C., Lavin, P.T., Band, P.R., Bennett, J.M., Bertino, J.R., Cohen, M.H., Douglass, H.O.J., Engstrom, P.F., Ezdinli, E.Z., Horton, J., Johnson, G.J., Moertel, C.G., Oken, M.M., Perlia, C., Rosenbaum, C., Silverstein, M.N., Skeel, R.T., Sponzo, R.W. & Tormey, D.C. (1980) Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am. J. Med. 69, 491497. Elia, M., Van Bokhorst-de van der Schueren, M.A., Garvey, J., Goedhart, A., Lundholm, K., Nitenberg, G. & Stratton, R.J. (2006) Enteral (oral or tube administration) nutritional support and eicosapentaenoic acid in patients with cancer: a systematic review. Int. J. Oncol. 28, 523. Fearon, K.C. (2008) Cancer cachexia: developing multimodal therapy for a multidimensional problem. Eur. J. Cancer 44, 11241132. Fearon, K.C., Von Meyenfeldt, M.F., Moses, A.G., Van Geenen, R., Roy, A., Gouma, D.J., Giacosa, A., Van Gossum, A., Bauer, J., Barber, M.D., Aaronson, N.K., Voss, A.C. &
2011 The Authors Journal of Human Nutrition and Dietetics 2011 The British Dietetic Association Ltd. 2011 J Hum Nutr Diet, 24, pp. 431440
439
Oral nutritional interventions in cancer and weight loss
C. Baldwin et al.
Tisdale, M.J. (2003) Effect of a protein and energy dense N-3 fatty acid enriched oral supplement on loss of weight and lean tissue in cancer cachexia: a randomised double blind trial. Gut 52, 14791486. Gosney, M. (2003) Are we wasting our money on food supplements in elder care wards? J. Adv. Nurs. 43, 275280. Isenring, E.A., Bauer, J.D. & Capra, S. (2007) Nutrition support using the American Dietetic Association medical nutrition therapy protocol for radiation oncology patients improves dietary intake compared with standard practice. J. Am. Diet. Assoc. 107, 404412. Katopodis, O., Ross, P., Norman, A.R., Oates, J. & Cunningham, D. (2004) Sixty-day all-cause mortality rates in patients treated for gastrointestinal cancers, in randomised trials, at the Royal Marsden Hospital. Eur. J. Cancer 40, 22302236. Koretz, R.L., Avenell, A., Lipman, T.O., Braunschweig, C.L. & Milne, A.C. (2007) Does enteral nutrition affect clinical outcome? A systematic review of the randomized trials Am. J. Gastroenterol. 102, 412429. Lawson, R.M., Doshi, M.K., Ingoe, L.E., Colligan, J.M., Barton, J.R. & Cobden, I. (2000) Compliance of orthopaedic patients with postoperative oral nutritional supplementation. Clin. Nutr. 19, 171175. Lundholm, K., Daneryd, P., Bosaeus, I., Korner, U. & Lindholm, E. (2004) Palliative nutritional intervention in addition to cyclooxygenase and erythropoietin treatment
for patients with malignant disease: effects on survival, metabolism, and function. Cancer 100, 19671977. Parnes, H.L., Fung, E. & Schiffer, C.A. (1994) Chemotherapyinduced lactose intolerance in adults. Cancer 74, 16291633. Rahemtulla, Z., Baldwin, C., Spiro, A., McGough, C., Norman, A.R., Frost, G., Cunningham, D. & Andreyev, H.J.N. (2005) The palatability of milk-based and non-milk-based nutritional supplements in gastrointestinal cancer and the effect of chemotherapy. Clin. Nutr. 24, 10291037. Ravasco, P., Monteiro-Grillo, I., Marques Vidal, P. & Camilo, M.E. (2005a) Impact of nutrition on outcome: a prospective randomized controlled trial in patients with head and neck cancer undergoing radiotherapy. Head Neck 27, 659668. Ravasco, P., Monteiro-Grillo, I., Vidal, P.M. & Camilo, M.E. (2005b) Dietary counseling improves patient outcomes: a prospective, randomized, controlled trial in colorectal cancer patients undergoing radiotherapy. J. Clin. Oncol. 23, 1431 1438. Ross, P.J., Ashley, S., Norton, A., Priest, K., Waters, J.S., Eisen, T., Smith, I.E. & OBrien, M.E. (2004) Do patients with weight loss have a worse outcome when undergoing chemotherapy for lung cancers? Br. J. Cancer 90, 19051911. Skipworth, R.J. & Fearon, K.C. (2007) The scientic rationale for optimizing nutritional support in cancer. Eur. J. Gastroenterol. Hepatol. 19, 371377. Todorovic, V. & Micklewright, A. (2004) Pocket Guide to Clinical Nutrition. Nottingham: PEN Group Publications.
440
2011 The Authors Journal of Human Nutrition and Dietetics 2011 The British Dietetic Association Ltd. 2011 J Hum Nutr Diet, 24, pp. 431440
You might also like
- Nasophar CA 980121Document25 pagesNasophar CA 980121Andrés VillaseñorNo ratings yet
- CJC 31 04 185Document12 pagesCJC 31 04 185Azan Al RasyidNo ratings yet
- Nasopharyngeal Carcinoma in Children and Young AdultsDocument9 pagesNasopharyngeal Carcinoma in Children and Young AdultsSunardiasihNo ratings yet
- 516 Full PDFDocument7 pages516 Full PDFSunardiasihNo ratings yet
- 6841 11598 1 SMDocument7 pages6841 11598 1 SMSunardiasihNo ratings yet
- 00 09 01 PDFDocument5 pages00 09 01 PDFSunardiasihNo ratings yet
- Incidence of Bronchiolitis in Breast Fed Infants Below 2 Years of AgeDocument5 pagesIncidence of Bronchiolitis in Breast Fed Infants Below 2 Years of AgeSunardiasihNo ratings yet
- Oc33 PDFDocument60 pagesOc33 PDFSunardiasihNo ratings yet
- Pediatrics 2006 Chantry 425-32-2Document11 pagesPediatrics 2006 Chantry 425-32-2SunardiasihNo ratings yet
- Fluid and Electrolytes ManagmentDocument13 pagesFluid and Electrolytes ManagmentSunardiasih100% (1)
- IndianJRadiolImaging192135-1650431 043504 PDFDocument11 pagesIndianJRadiolImaging192135-1650431 043504 PDFSunardiasihNo ratings yet
- IndianJRadiolImaging192135-1650431 043504 PDFDocument11 pagesIndianJRadiolImaging192135-1650431 043504 PDFSunardiasihNo ratings yet
- CBD CKDDocument23 pagesCBD CKDSunardiasihNo ratings yet
- ATS GuidelinesDocument46 pagesATS Guidelinesapi-3847280100% (1)
- CHT Hfa Boys Z 2 5Document1 pageCHT Hfa Boys Z 2 5Sunu RachmatNo ratings yet
- Nutrition Journal: Nutrition Support in Cancer Patients: A Brief Review and Suggestion For Standard Indications CriteriaDocument5 pagesNutrition Journal: Nutrition Support in Cancer Patients: A Brief Review and Suggestion For Standard Indications CriteriaSunardiasihNo ratings yet
- Protap MataDocument40 pagesProtap MataSunardiasihNo ratings yet
- Nutritional Management of Gastrointestinal Malignancies: Invited CommunicationDocument3 pagesNutritional Management of Gastrointestinal Malignancies: Invited CommunicationSunardiasihNo ratings yet
- Practical Gastro Mar 04Document9 pagesPractical Gastro Mar 04SunardiasihNo ratings yet
- Nutrition Journal: Nutrition Support in Cancer Patients: A Brief Review and Suggestion For Standard Indications CriteriaDocument5 pagesNutrition Journal: Nutrition Support in Cancer Patients: A Brief Review and Suggestion For Standard Indications CriteriaSunardiasihNo ratings yet
- The Balinese Tradmed PPT 2003Document44 pagesThe Balinese Tradmed PPT 2003SunardiasihNo ratings yet
- MORNING REPORT CASEDocument22 pagesMORNING REPORT CASESunardiasihNo ratings yet
- BMI, Physical Activity, and Diet Role in Colorectal Cancer Recurrence and SurvivalDocument21 pagesBMI, Physical Activity, and Diet Role in Colorectal Cancer Recurrence and SurvivalSunardiasihNo ratings yet
- 1475 2891 3 19Document21 pages1475 2891 3 19SunardiasihNo ratings yet
- Nutrition Journal: Nutrition Support in Cancer Patients: A Brief Review and Suggestion For Standard Indications CriteriaDocument5 pagesNutrition Journal: Nutrition Support in Cancer Patients: A Brief Review and Suggestion For Standard Indications CriteriaSunardiasihNo ratings yet
- Nutritional Management of Gastrointestinal Malignancies: Invited CommunicationDocument3 pagesNutritional Management of Gastrointestinal Malignancies: Invited CommunicationSunardiasihNo ratings yet
- BMI, Physical Activity, and Diet Role in Colorectal Cancer Recurrence and SurvivalDocument21 pagesBMI, Physical Activity, and Diet Role in Colorectal Cancer Recurrence and SurvivalSunardiasihNo ratings yet
- 1475 2891 12 118Document8 pages1475 2891 12 118SunardiasihNo ratings yet
- 1475 2891 11 27Document18 pages1475 2891 11 27SunardiasihNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- McGill Nutrition Guide Page8 Homemade Food SupplementsDocument31 pagesMcGill Nutrition Guide Page8 Homemade Food Supplementsapi-3714923100% (1)
- B7-H3 Expression in Gastric CancerDocument6 pagesB7-H3 Expression in Gastric CancerIvoBarrosNo ratings yet
- TMP 9 CE9Document7 pagesTMP 9 CE9FrontiersNo ratings yet
- Pharmacology 2 NotesDocument21 pagesPharmacology 2 Notesgnikap_deleonNo ratings yet
- Potential Growth Inhibitory Effect of Maitake D-Fraction On Canine Cancer CellsDocument9 pagesPotential Growth Inhibitory Effect of Maitake D-Fraction On Canine Cancer Cellsclaudio vasquesNo ratings yet
- Claudio Lucarelli CV-2018Document5 pagesClaudio Lucarelli CV-2018ignacioillanesNo ratings yet
- Daftar Obat Sitostatika Yang Penyimpanan Dan Pemberiannya Terlindung Dari Cahaya PDFDocument1 pageDaftar Obat Sitostatika Yang Penyimpanan Dan Pemberiannya Terlindung Dari Cahaya PDFAyahe YumnaNo ratings yet
- Toward A Cancer Drug of Fungal OriginDocument31 pagesToward A Cancer Drug of Fungal OrigininsaNo ratings yet
- ''Pharmacology ExamDocument44 pages''Pharmacology Examsean blaze100% (4)
- Sfda Approved Drug Mar2021Document9 pagesSfda Approved Drug Mar2021iyad.alsabiNo ratings yet
- Chemotherapy Cooling Cap Instructions: Arctic Heat Pty LTD., Queensland, AustraliaDocument4 pagesChemotherapy Cooling Cap Instructions: Arctic Heat Pty LTD., Queensland, AustraliaMohamed SouidiNo ratings yet
- Basic Principles in Surgical Oncology - Blake CadyDocument19 pagesBasic Principles in Surgical Oncology - Blake CadypathoTM0% (1)
- The Big Four by Rolf GordonDocument40 pagesThe Big Four by Rolf GordonArcanistNo ratings yet
- Breast Cancer TreatmentDocument13 pagesBreast Cancer TreatmentRissa AlmiraNo ratings yet
- Precision Medicine in Cancers and Non-Communicable DiseasesDocument343 pagesPrecision Medicine in Cancers and Non-Communicable DiseasesBenaia João NHAMITAMBONo ratings yet
- ADC Skan Occupational SafetyDocument6 pagesADC Skan Occupational SafetyjmittalNo ratings yet
- Cancer Chemotherapy - A Critical Analysis of Its 60 Years of HistoryDocument19 pagesCancer Chemotherapy - A Critical Analysis of Its 60 Years of HistoryCarlaValongoNo ratings yet
- Hyperleukocytosis and Leukostasis in Hematologic MalignanciesDocument9 pagesHyperleukocytosis and Leukostasis in Hematologic Malignanciessoclose1200No ratings yet
- Ccs Sample QuestionsDocument20 pagesCcs Sample Questionscarrie0875% (44)
- Oncologic NursingDocument16 pagesOncologic NursingDharline Abbygale Garvida AgullanaNo ratings yet
- M.D. Anderson Cancer Center International Patient FormsDocument6 pagesM.D. Anderson Cancer Center International Patient FormsNasib KaurNo ratings yet
- Handbook of Systemic Treatments For Cancer - 8th EditionDocument186 pagesHandbook of Systemic Treatments For Cancer - 8th EditionLaurențiu Acostioaei67% (3)
- Case PresentationDocument24 pagesCase Presentationnaega hoshii'hhNo ratings yet
- Baking Soda and Maple SyrupDocument6 pagesBaking Soda and Maple SyrupTorentSpy100% (1)
- GastricDocument6 pagesGastricapi-282129282No ratings yet
- Cancer Cells vs Normal CellsDocument2 pagesCancer Cells vs Normal CellsAryan JaiswalNo ratings yet
- 1 - AntineoplasticsDocument171 pages1 - AntineoplasticsMelika SadrolashrafiNo ratings yet
- Daniel PompaDocument16 pagesDaniel PompaK Mehmet ŞensoyNo ratings yet
- Once-Censored Cancer CuresDocument65 pagesOnce-Censored Cancer CuresJeremy Perez100% (5)
- Antiproliferative Properties of Lavatera - 5.31 - UGCDocument3 pagesAntiproliferative Properties of Lavatera - 5.31 - UGCMudasir MirNo ratings yet