Professional Documents
Culture Documents
UKPDS
Uploaded by
Richard S. RoxasCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
UKPDS
Uploaded by
Richard S. RoxasCopyright:
Available Formats
The UK Prospective Diabetes Study (UKPDS): clinical and therapeutic implications for type 2 diabetes
Paromita King,1 Ian Peacock1 & Richard Donnelly1,2
1
Jenny ONeill Diabetes Centre, Derbyshire Royal Inrmary, Derby and Division of Vascular Medicine, School of Medical and Surgical Sciences, University of Nottingham, UK
Keywords: antihypertensives, diabetic complications, glycaemic control, oral hypoglycaemic agents, type 2 diabetes, UKPDS
The burden of type 2 diabetes
Diabetes was rst recognized 3500 years ago by the Ancient Egyptians. One of the rst clinical descriptions was by Aretaeus, who practised in Cappadocia around 120 AD. He wrote that the condition was fortunately rare, but short will be the life of the man in whom the disease is fully developed [1]. In modern society, the rst statement is far from true. The incidence of diabetes has doubled every 20 years since 1945 [2]. In 1994 the world wide prevalence of type 2 (non-insulin dependent) diabetes was 99 million (1.8% of the population); by 2010 it is estimated that this gure will rise to 215 million (3.8%) [3]. The second statement is as true today as it was almost 2000 years ago. In the West, 44% of patients with type 2 diabetes die within 10 years of diagnosis [4], mostly from macrovascular disease; the incidence of and mortality from cardiovascular disease are 23 times greater than in the general population [5]. As the majority of patients develop complications, which are present in up to 50% even at the time of diagnosis [6], type 2 diabetes imposes a signicant burden on health services, as well as on the individuals who suer from this progressive and incurable disease. Currently the 2% of the UK population with diabetes consume 5% of the health service budget; by comparison the 12% with arthritis consume just 1.9% [7]. With the increasing prevalence of the condition, these gures will escalate. Prevention would be the ideal solution, but is currently a remote prospect. In the meantime any way of signicantly reducing the burden of diabetes-related complications will have a major impact on patient well-being and on cost eectiveness of management.
incidence of vascular complications. On the contrary, the pioneering study of the 1960s, the University Group Diabetes Program (UGDP) [8], suggested that treatment with tolbutamide might be harmful. The study was designed to assess the impact of blood glucose lowering therapies on complications, with patients being randomly allocated to placebo, tolbutamide, phenformin, or insulin. The study was stopped after 8 years because of an increase in cardiovascular deaths in those receiving tolbutamide. However, for many years the design and conduct of the UGDP were subject to erce debate which was never satisfactorily resolved; uncertainty continued about treatment and glycaemic targets for type 2 diabetes. The Diabetes Control and Complications Trial (DCCT), published in 1993 [9], showed that intensive glycaemic control (i.e. keeping blood glucose as near to normal as possible) reduces the incidence and progression of microvascular complications (retinopathy, nephropathy and neuropathy) in type 1 diabetes. Whether the same holds true in type 2 diabetes remained uncertain. Intensive treatment often results in hyperinsulinaemia, with weight gain and an increase in hypoglycaemia [9], both of which have theoretical adverse eects on macrovascular disease, the major life threatening complication of type 2 diabetes. Patients with type 2 diabetes frequently have other risk factors for macrovascular disease, such as hypertension and hyperlipidaemia, the former having a prevalence of 40%-60% [10, 11]. Antihypertensive therapy reduces the risk of both cardiovascular and cerebrovascular disease in the general population [12], but to what extent these ndings apply to type 2 diabetes was again not clear. The United Kingdom Prospective Diabetes Study (UKPDS) was conceived to explore these uncertainties and provide clearer guidelines for the management of type 2 diabetes.
The benets of treatment?
Until the early 1990s, there was no evidence that our management of diabetes had any benecial impact on the
Correspondence: Dr I. Peacock, Derbyshire Royal Inrmary, London Road, Derby, DE1 2QY, UK. Received 15 March 1999, accepted 24 August 1999.
Design of the UKPDS (Figures 13)
The UKPDS was set up in the late 1970s, by Dr Robert Turner and colleagues in Oxford. Over 7600 subjects at 23 centres across the UK were considered for inclusion; 5102 took part. It was the largest and longest study ever
643
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
P. King et al.
does improved blood glucose control reduce the incidence of complications? do different treatments have specific advantages or disadvantages?
Figure 1 UKPDSthe principal questions.
Hypertension in Diabetes Study does tight control of blood pressure have an impact on complications? do atenolol or captopril have specific advantages or disadvantages? glycaemic control using combination treatment (Glucose study 2) acarbose quality of life cost-effectiveness many incidental scientific, epidemiological and clinical studies
Figure 2 UKPDSembedded studies.
undertaken in diabetes; median follow-up was 10 years. As well as attempting to resolve unanswered clinical issues, the study generated a huge epidemiological database, comprising over 20 million data items. The primary aim was to determine the eect of intensive glycaemic control on the incidence of complications; the secondary aim was to assess whether there were dierences between treatments (Figure 1). Protocol amendments were made to add topics not originally included. These strengthened the study by broadening its scope, but at the cost of complicating the treatment allocation, conduct and analysis of the study. Numerous substudies were embedded (Figure 2), the most notable being the Hypertension in Diabetes Study. Over 30 papers have been published from the UKPDS database, and many more are in preparation or planned.
Key points (Figure 4) Glucose control studies [13, 14]
Subjects were randomized to receive conventional or intensive therapy. In the former, the intention was to keep patients aymptomatic, with a fasting plasma glucose 1 less than 15 mmol l ; in the latter, the target fasting 1 glucose was 6 mmol l . When diet failed to achieve these targets, subjects were randomized to sulphonylureas, insulin or metformin, the latter in obese patients only. When single treatments failed, combinations were used. The results were primarily expressed in terms of aggregate end points: any diabetes related end point,
644
which included both microvascular and macrovascular events, and diabetes related death. Twenty-one single end points were also dened. The emphasis on aggregate end-points allowed the study outcomes to be presented in a clinically meaningful way, i.e. overall risk. Their use also reduced the number of treatment comparisons, thus minimizing the chances of false-positive results, but had the disadvantage of concealing the magnitude of eects on individual end points. Intensive glucose control signicantly reduced any diabetes-related end point, but had no eect on mortality. The predominant eect of tighter control was a reduction of microvascular disease by a quarter, largely due to a reduction in laser photocoagulation. There was also a trend, just short of statistical signicance, towards a reduction in macrovascular disease. No threshold was seen, i.e. any improvement in glycaemic control is benecial. These ndings are similar to those of the DCCT and a more recent study in Japanese patients with type 2 diabetes, in whom 6 years intensive therapy with insulin reduced the incidence of microvascular complications [15]. That the reduced occurrence of myocardial infarction was not signicant may be due to type 2 statistical error. The study was set up to detect a 15% dierence in events over the 10 years study period, and a larger number of macrovascular than microvascular events occurred, but the separation of HbA1c between intensive and conventionally treated groups was disappointingly low: 0.9% (half that in the DCCT). Had the separation of HbA1c between groups been greater, a signicant eect of intensive control on macrovascular disease might have been demonstrated. The secondary aim of the study was to compare the eects of dierent treatments for diabetes, since some have theoretical advantages and disadvantages. For example, sulphonylureas close myocardial ATP-sensitive potassium channels, which could impair ischaemia induced vasodilatation [16], perhaps explaining the results of the UGDP. In addition, some studies have suggested that hyperinsulinaemic states are atherogenic [17], and the increased incidence of hypoglycaemia with intensive control with insulin could theoretically precipitate a cerebrovascular or cardiovascular event. The UKPDS showed no dierence in outcome between treatments, which is at rst sight reassuring, but the study was powered to assess the eects of intensive therapy in general and it is unclear whether there is adequate power in this subgroup analysis. In addition, actual therapy often diered from allocated treatment, especially as patients required additional treatment over time. The results of this aspect of the study should therefore be interpreted with caution. The results of metformin treatment are the most controversial [14]. Metformin use was associated with fewer aggregate end-points (including overall mortality)
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
Therapeutic implications of the UKPDS
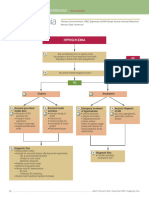
Newly diagnosed diabetes Fasting plasma glucose >6mmoll1 Prudent diet for 34 months
>6mmoll1 6mmoll
1
Diet satisfactory
>6 and 15mmoll1
>15mmoll1
Main randomization
Primary diet failure randomization
if becomes >6mmoll1
Conventional policy target <15mmoll1
Intensive policy target <6mmoll1
Diet only
Figure 3 Design of UKPDS.
Sulphonylurea
Insulin
Metformin (obese patients only)
intensive glucose control, using existing treatments, improved microvascular morbidity, but not mortality insulin and sulphonylureas were similarly effective metformin was advantageous in the obese intensive blood pressure control was more beneficial, improving morbidity (both micro- and macrovascular), and mortality ideal targets: HbAlc < 7%, BP < 140/80 mmHg any reduction was beneficial
An unexpected nding was that the addition of metformin to sulphonylureas (in both obese and nonobese patients) was associated with increased mortality. The numbers involved in this subgroup analysis were very small, with few deaths (26 vs 14 in the group treated with sulphonylureas alone) and no dierence in the incidence of heart attacks or strokes between the groups, only in the proportion who died. Furthermore, the mortality in the group treated by sulphonylureas alone was unexpectedly low. The authors therefore concluded that this anomalous result was likely to be have been due to chance.
Figure 4 Key points.
Hypertension in Diabetes Study [18, 19]
in obese patients. However the number of patients allocated to metformin was less than 10% of all those randomised. The ndings could also be interpreted as indicating that insulin and sulphonylureas are equally harmful in the obese, possibly as a consequence of hyperinsulinaemia.
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
One thousand one hundred and forty-eight patients took part. Half the participants were allocated to tight control (target blood pressure less than 150/85 mm Hg ) and were randomised to either atenolol or captopril, with other agents added as necessary. The remainder were allocated to less tight control (target blood pressure less
645
P. King et al.
than 180/105 mm Hg); in these patients, drugs other than b-adrenoceptor blockers and ACE inhibitors were used. Mean blood pressure was 144/82 mm Hg in the tight control group, compared with 154/87 mm Hg in the less tight control group. One-third of patients allocated to tight control required three more drugs in the attempt to achieve the target blood pressure. Tight control of blood pressure reduced both diabetesrelated morbidity and mortality. Unlike glycaemic control, there was a signicant eect on macrovascular as well as microvascular complications, with strokes and heart failure reduced by a half. Myocardial infarction was reduced by a fth, but this was not statistically signicant. As in the glucose control study, no threshold for risk was seen in the hypertension study. These are very impressive results, establishing that blood pressure control is at least as important as glycaemic control, if not more so, in the prevention of complications in type 2 diabetes. In the last 2 years, the results of several other studies of hypertension which have included patients with diabetes have been published. These also demonstrated a reduction in macrovascular risk, including myocardial infarction [20, 21]. A variety of agents was used, but blood pressure dierences between treatment and control groups were comparable with the UKPDS, and protective eects were observed despite shorter periods of follow up (25 years). Thus there is no doubt of the signicance of blood pressure control in type 2 diabetes, but there remains the question whether particular drugs have advantages or disadvantages. The UKPDS compared captopril and atenolol, both drugs having theoretical benets. In the general population with hypertension, b-adrenoceptor blockers reduce macrovascular events and are specically cardioprotective, reducing sudden death and further myocardial events in those with prior myocardial infarction[22]. ACE inhibitors improve survival in patients with heart failure [23, 24]; in type 1 diabetes, they reduce the progression of nephropathy [25, 26] and possibly retinopathy [27], but whether ACE inhibitors have specic advantages over other antihypertensive agents in type 2 diabetes is not yet agreed. Recently the ABCD trial showed a reduction in myocardial infarction in diabetic hypertensive subjects treated with an ACE inhibitor compared with a calcium channel blocker [28], but it was not clear whether the ACE inhibitor was especially benecial or the calcium channel blocker relatively harmful, particularly as the groups were inadequately matched for concomitant medication. The UKPDS found that captopril and atenolol were equally eective as antihypertensive agents, in preventing macrovascular complications and in reducing the progression of retinopathy and albuminuria. The ACE inhibitor was however, better tolerated. These results are again reassuring at rst sight, but, as with the
646
glucose control study, type 2 errors cannot be excluded; there was a trend in favour of the atenolol treated group.
Therapeutic implications, study limitations and outstanding questions (Figures 57)
The UKPDS demonstrated that any improvement in glycaemic control and blood pressure reduces diabetesrelated complications. In trials such as this, patients are selected both by investigators and by themselves. The observation that UKPDS patients had a lower mortality than the general population with type 2 diabetes may be a reection of this. What was achievable and acceptable to a trial population cannot be necessarily translated to everyone with type 2 diabetes. This must be remembered when applying the results of the study to clinical practice. There is no doubt that aggressive management of blood pressure is important, particularly in reducing macrovascular disease, the main cause of morbidity and mortality in these patients. A target blood pressure of less than 140/80 is suggested by the authors. The fact that benets are achieved within 2 or 3 years means that all patients should be treated irrespective of age. Clearly, achieving this goal will require aggressive follow up ( patients in the UKPDS were seen 3 monthly), and this may not be acceptable to all patients. With one third requiring 3 or more agents to maintain target blood pressures, compliance will certainly be a problem in some. Whether intensive glycaemic control should be routinely introduced in type 2 diabetes is more controversial.
limited separation between conventional and intensive glucose groups (patient compliance?) insufficient statistical power for subgroup analyses
Figure 5 Limitations of the study.
how worthwhile are the benefits achieved? can targets be achieved in routine practice? benefit of increasing insulin dose? benefit of insulin/tablet combinations place of aspirin, statins, anti-oxidants, etc.
Figure 6 Outstanding questions.
treatment with several drugs will often be necessary increased resources will be needed to realize benefits of better control treatment is cost effective, when benefits are taken into account screening programmes should be considered
Figure 7 Therapeutic implications.
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
Therapeutic implications of the UKPDS
Despite achieving statistical signicance, the absolute risk reduction from intensive glycaemic control is small, with a reduction of 5 events over 10 years compared with 16 for blood pressure (Table 1). Furthermore, the benets of glucose reduction did not accrue for several years, unlike intensive blood pressure control. Intensive glycaemic control, particularly with insulin, also leads to morbidity from hypoglycaemia and weight gain. Thus, unlike blood pressure control, intensive glycaemic control is not suitable for all patients, particularly the elderly, or those with existing severe complications. The small absolute risk reduction also needs to be compared with the possible eects of other risk factor interventions, e.g. treatment with aspirin, lipid lowering drugs or antioxidants. Despite these limitations, the UKPDS provides evidence and quantitative guidelines for those in whom intensive control is achievable. The study also assessed eects of intensive treatment on quality of life; no adverse eect was apparent. One scale demonstrated that poor quality of life is related to complications rather than the treatments given [unpublished]. This is reassuring in implementing the results of the study, though the results may not apply equally to an unselected population. One aspect of management inadequately addressed by the study is the optimal combination of drugs to be used either for glucose or blood pressure control. Dierent agents seemed equally eective, but the possibility of type 2 errors in these subgroup analyses cannot be excluded, as already discussed. To date, the eectiveness of insulin and oral hypoglycaemic agent combinations is not known, although there are unpublished data from the study on the combination of insulin and sulphonylureas. Data on possible dose-dependent eects of insulin, and the combination of insulin and metformin are lacking. For now, until further information is available, clinical practice should be based on achieving glucose and blood pressure reduction by whatever means best suits an individual patient. In the study, patients were reviewed 3 monthly, rather than 612 monthly as in routine clinical practice, which has considerable resource implications. The reduction in blood pressure [29] and glucose [unpublished] achieved were relatively cheap, 48 and 22 per patient per year,
Table 1 Absolute risk.
Number of events Intensive Conventional Glucose control Blood pressure control 41 51 46 67
respectively, when the benets were discounted. These gures are valuable ammunition in the battle to improve services for patients. With 50% of patients presenting with complications, the issue of screening should also be addressed. The UKPDS provides management guidelines for selected patients, but leaves many questions unanswered. The advantages of good care have been more clearly dened than ever before, but the huge gulf between the benets achieved in the study and the many frustrations of everyday practice remains. In most centres, there are large numbers of patients with poor control of both blood glucose and blood pressure. Type 2 diabetes must at least be taken more seriously.
References
1 Reed JA. Aretaeus, the Cappadocian. Diabetes 1954; 3: 419421. 2 Barnett T. Epidemiology, complications and costs of diabetes mellitus. In The insulin treatment of diabetes: a practical guide, ed. Tony Barnett, London, E-map healthcare: 69, 1998. 3 McCarty D, Zimnet P. Diabetes 19942010: global estimates and projections. Leverkusen, Bayer.: 146, 1994. 4 Panzam G. Mortality and survival in type II (non-insulin dependent) diabetes mellitus. Diabetologia 1987; 30: 123131. 5 Garcia MJ, McNamara PM, Gordon T, Kannell WB. Morbidity and mortality in diabetics in the Framingham population. Sixteen year follow-up study. Diabetes 1974; 23: 105111. 6 UK Prospective Diabetes Study (UKPDS) Group. UK prospective diabetes study VIII. study design, progress and performance. Diabetologia 1991; 34: 877890. 7 Leese B. Economic evaluations of Type II diabetes. In The social and cost implications of Type II diabetes, ed Bengt Jo nsson H, Krans MJ, PharmacoEconomics 8(Suppl, 1995; 1 ): 2327. 8 University Group Diabetes Programme. A study on the eects of hypoglycaemic agents on vascular complications in patients with adult-onset diabetes. Diabetes 1976; 25: 11291153. 9 The Diabetes Control and Complications Trial Research Group. The eect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329: 977986. 10 Hypertension in Diabetes Study Group HDS. 1. Prevalence of hypertension in newly presenting type 2 diabetic patients and the association with risk factors for cardio-vascular and diabetic complications. J Hypertens 1993; 11: 309317. 11 Prescott-Clarke P, Primatesa P. Health Survey for England 1995 London HMSO, 1997. 12 Collins R, Macmahon S. Blood pressure, antihypertensive drug treatment and the risks of stroke and coronary heart disease. Br Med J 1994; 50: 272298. 13 UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin
*NNT 20 (95% CI 10500) 6 (310)
*number needed to treat for 10 years to prevent 1 event.
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
647
P. King et al.
14
15
16
17
18
19
20
21
compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998; 352: 837853. UK Prospective Diabetes Study (UKPDS) Group. Eect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998; 352: 854865. Ohkubo Y, Kishikawa H, Araki E, et al. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin dependent diabetes mellitus: a randomised prospective 6-year study. Diabet Res Clin Pract 1995; 28: 103117. Ashford ML, Bond CT, Blair TA, Adelman JP. Cloning and functional expression of a rat heart K-ATP channel. Nature 1994; 370: 456459. Stout RW. Insulin and atherosclerosis. In Diabetes and Atherosclerosis, ed Stout RW, Dordrecht, The Netherlands. Kluwer Academic publishers., 1992: 165201. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. Br Med J 1998; 317: 703713. UK Prospective Diabetes Study Group. Ecacy of atenolol and captopril in reducing risk of macrovascular and microvasvular complications in type 2 diabetes: UKPDS 39. Br Med J 1998; 317: 713720. Curb JD, Pressel SL, Cutler JA, et al. Eect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic hypertension in the Elderly Program Cooperative Resaerch Group. JAMA 1996; 276: 18861892. Hansson L, Zanchetti A, Carruthers SG, et al. for the HOT Study Group. Eects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet 1998; 351: 17551762.
22
23
24
25
26
27
28
29
Yusef S, Peto R, Lewis J, Collins R, Sleight P. Betablockade during and after myocardial infarction; an overview of the randomised trials. Progr Cardiovascular Dis 1997; 30: 335371. CONSENSUS Trial Study Group. Eects of enalapril on mortality in severe congestive heart failure. New Eng J Med 1987; 316: 14291435. SOLVD Investigators. Eect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. New Eng J Med 1992; 327: 685691. Bjo rck S, Mulec H, Johnsen SA, Norden G, Aurell M. Renal protective eects in diabetic nephropathy. Br Med J 1992; 304: 339343. Lewis EJ, Hunsicker LG, Bain RP, Rhode RD. for the Colloborative Study Group. The eect of angiotensinconverting enzyme inhibition on diabetic nephropathy. New Engl J Med 1993; 329: 14561462. Chaturvedi N, Sjolie AK, Stevenson JM, et al. Eect of lisinopril on progression of retinopathy in normotensive people with type 1 diabetes. The EUCLID Study Group. EURODIAB Controlled Trial of Lisinopril in InsulinDependent Diabetes Mellitus. Lancet 1998; 351: 2831. Estacio RO, Schrier RW. Antihypertensive therapy in type 2 diabetes: implications of the Appropriate Blood pressure Control in Diabetes (ABCD) trial. Am J Cardiol 1998; 82: 9R14R. UK Prospective Diabetes Study Group. Cost eectiveness analysis of improved blood pressure control in hypertensive patients with type 2 diabetes: UKPDS 40. Br Med J 1998; 317: 720726.
Note added in proof
We wish to pay tribute to Robert Turner whose recent untimely death is such a tragedy.
648
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Critical+appraisal+RCT Su+May+LiewDocument34 pagesCritical+appraisal+RCT Su+May+LiewRichard S. RoxasNo ratings yet
- Evidence-Based Medicine: The Basics: Will Olmstadt, MS, MPHDocument14 pagesEvidence-Based Medicine: The Basics: Will Olmstadt, MS, MPHRichard S. RoxasNo ratings yet
- EDICDocument13 pagesEDICRichard S. RoxasNo ratings yet
- Management of Hyperglycemia in Type 2 Diabetes A Patient-Centered ApproachDocument16 pagesManagement of Hyperglycemia in Type 2 Diabetes A Patient-Centered ApproachThawatchai NakkaratniyomNo ratings yet
- 14 1 1 Blood ConsumptionDocument3 pages14 1 1 Blood ConsumptionRichard S. RoxasNo ratings yet
- AccordDocument2 pagesAccordRichard S. RoxasNo ratings yet
- 35.5 Inches LengthDocument1 page35.5 Inches LengthRichard S. RoxasNo ratings yet
- CancerDocument8 pagesCancerRichard S. RoxasNo ratings yet
- Things Needed2Document1 pageThings Needed2Richard S. RoxasNo ratings yet
- Villi: RD THDocument2 pagesVilli: RD THRichard S. RoxasNo ratings yet
- AdvanceDocument5 pagesAdvanceRichard S. RoxasNo ratings yet
- DM Update 2012Document64 pagesDM Update 2012Richard S. RoxasNo ratings yet
- CGM Week 2: Interstitial Fluid & Insulin PumpsDocument3 pagesCGM Week 2: Interstitial Fluid & Insulin PumpsRichard S. RoxasNo ratings yet
- Week 1 Diabetes Pathophysiology and Glycemic ControlDocument10 pagesWeek 1 Diabetes Pathophysiology and Glycemic ControlRichard S. RoxasNo ratings yet
- Week 3: Vaccines RECOMBINANT DNA: Viral Subunit SummaryDocument3 pagesWeek 3: Vaccines RECOMBINANT DNA: Viral Subunit SummaryRichard S. RoxasNo ratings yet
- Week 1: Vaccines History of Vaccines: POLIO VACCINE: 1930'sDocument2 pagesWeek 1: Vaccines History of Vaccines: POLIO VACCINE: 1930'sRichard S. RoxasNo ratings yet
- Virology SyllabusDocument6 pagesVirology SyllabusRichard S. RoxasNo ratings yet
- NOVEMBER 16, 2013 12:00 PM-3:00 PM SVB Room 503: Week 1: Methods of ResearchDocument2 pagesNOVEMBER 16, 2013 12:00 PM-3:00 PM SVB Room 503: Week 1: Methods of ResearchRichard S. RoxasNo ratings yet
- Disaster Preparedness SyllabusDocument7 pagesDisaster Preparedness SyllabusRichard S. RoxasNo ratings yet
- Excitation CouplingDocument3 pagesExcitation CouplingRichard S. RoxasNo ratings yet
- Schedule of Activities 1st Sem '08-'09Document7 pagesSchedule of Activities 1st Sem '08-'09Richard S. RoxasNo ratings yet
- Medical-Surgical Nursing ReviewDocument90 pagesMedical-Surgical Nursing Reviewɹǝʍdןnos99% (312)
- FertilizationDocument3 pagesFertilizationRichard S. RoxasNo ratings yet
- Ob Concept RMRDocument86 pagesOb Concept RMRRichard S. RoxasNo ratings yet
- Ob 1Document61 pagesOb 1Richard S. RoxasNo ratings yet
- The Nursing Process and Client TeachingDocument15 pagesThe Nursing Process and Client TeachingRichard S. RoxasNo ratings yet
- OB Sked Midterm 2008-09Document2 pagesOB Sked Midterm 2008-09Richard S. RoxasNo ratings yet
- Pharmacology Case StudyDocument4 pagesPharmacology Case StudyRichard S. RoxasNo ratings yet
- Easy QuestionsDocument8 pagesEasy QuestionsRichard S. RoxasNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Diabetes MellitusDocument75 pagesDiabetes MellitusIndika KarunamuniNo ratings yet
- Diabetes GestacionalDocument3 pagesDiabetes GestacionalCeiila GonzálezNo ratings yet
- Diabetes Mellitus PowerpointDocument18 pagesDiabetes Mellitus PowerpointZach Woodrow0% (1)
- epid15,+07.+Marisa+Gita+Putri Inggris 256+sd+264Document9 pagesepid15,+07.+Marisa+Gita+Putri Inggris 256+sd+264Selmitha SariNo ratings yet
- Riska Amelia, A. Mushawwir Taiyeb, Irma Suryani IdrisDocument11 pagesRiska Amelia, A. Mushawwir Taiyeb, Irma Suryani IdrisÈkä Sêtýä PrätämäNo ratings yet
- Evaluasi ElektrolitDocument3 pagesEvaluasi ElektrolitMonica Ariestha ToewehNo ratings yet
- Toronto Notes Nephrology 2015 8Document1 pageToronto Notes Nephrology 2015 8JUSASBNo ratings yet
- Canine and Feline Endocrinology and Reproduction PARTE DIABETEDocument44 pagesCanine and Feline Endocrinology and Reproduction PARTE DIABETEmarparolaNo ratings yet
- HypoglycemiaDocument113 pagesHypoglycemiamadelleinetNo ratings yet
- Boys Centile ChartDocument1 pageBoys Centile ChartElma AprilliaNo ratings yet
- Hubungan Perilaku Diet Dengan Kadar Gula Darah Pada Penderita Diabetes Melitus Tipe Ii (Di Desa Jogomerto Kecamatan Tanjung Anom)Document9 pagesHubungan Perilaku Diet Dengan Kadar Gula Darah Pada Penderita Diabetes Melitus Tipe Ii (Di Desa Jogomerto Kecamatan Tanjung Anom)Rafael SebastianNo ratings yet
- Asia - Pan - Management of Prediabetes and Type 2 DiabetesDocument19 pagesAsia - Pan - Management of Prediabetes and Type 2 DiabetesputrakartonoNo ratings yet
- Nursing Care Plan for Diabetes MellitusDocument3 pagesNursing Care Plan for Diabetes Mellitusinagasi83% (12)
- Lect.10 Acromegaly, Gigantism and OthersDocument10 pagesLect.10 Acromegaly, Gigantism and OthersShubhamNo ratings yet
- Anidem Hw1Document2 pagesAnidem Hw1John Cromwell A. MedinaNo ratings yet
- SF8 TemplateDocument6 pagesSF8 TemplateMITZHE MAMINONo ratings yet
- Thyroidism Patient Survey ResultsDocument90 pagesThyroidism Patient Survey ResultsBvayNo ratings yet
- Exemplar - Hypoglycemia: If Blood Glucose Levels Continue To Drop.Document1 pageExemplar - Hypoglycemia: If Blood Glucose Levels Continue To Drop.Mary GiuntiniNo ratings yet
- Thyroid DisorderDocument20 pagesThyroid DisorderNadun MethwadaneNo ratings yet
- Diabetes Basics: Signs and SymptomsDocument5 pagesDiabetes Basics: Signs and Symptomsindigopussycat2No ratings yet
- Causes of Metabolic AcidosisDocument10 pagesCauses of Metabolic AcidosisKimberly Anne SP PadillaNo ratings yet
- Lab Report Sample BloodDocument5 pagesLab Report Sample BloodgjvpandiyanNo ratings yet
- GDMDocument12 pagesGDMJennicaNo ratings yet
- Hypoglycemia - Schermerhorn, ThomasDocument2 pagesHypoglycemia - Schermerhorn, ThomasJuanMartínezNo ratings yet
- Pituitary Tumor & AcromegalyDocument32 pagesPituitary Tumor & Acromegalysam840720No ratings yet
- Endocrine Pathophysiology Nursing Notes - Part 2Document10 pagesEndocrine Pathophysiology Nursing Notes - Part 2grad_nurse_2015100% (1)
- Endocrine Nursing ReviewDocument38 pagesEndocrine Nursing ReviewAmiel Francisco Reyes100% (2)
- DMG Diagnosis and ManagementDocument6 pagesDMG Diagnosis and ManagementCésar MonjarásNo ratings yet
- USMLE Step 2 Lesson on Thyroid DiseaseDocument4 pagesUSMLE Step 2 Lesson on Thyroid DiseaseMavra zNo ratings yet
- Interpretation: S03 - FPSC DILSHAD COLONY (C004263143) J-50 Dilshad Colony, DelhiDocument6 pagesInterpretation: S03 - FPSC DILSHAD COLONY (C004263143) J-50 Dilshad Colony, DelhiAll VIDEOS TechNo ratings yet