Professional Documents
Culture Documents
What You Need To Know About Thyroid Disorders in Pregnancy: Dowden Health Media
Uploaded by
najmulOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
What You Need To Know About Thyroid Disorders in Pregnancy: Dowden Health Media
Uploaded by
najmulCopyright:
Available Formats
What you need to know about thyroid disorders in pregnancy
Managing overt disorders is straightforward, but even subclinical disease warrants heightened scrutiny
ntil recently, thyroid dysfunction was thought to have little influence on pregnancy as long as it was treated, and management was straightforward. That was before case control studies in prominent journals suggested an association between even subclinical hypothyroidism and impaired neonatal neurodevelopment.14 The risk associated with hyperthyroidism in pregnancy is less clear. Currently, it is believed to cause no adverse effects; the low thyroid-stimulating hormone (TSH) resolves in most women within 4 to 12 weeks. As for the nonpregnant state, there is no agreement between the American College of Physicians and its British counterpart as to whether isolated, subclinical hyperthyroidism leads to morbidity or mortality, although some investigators have found an excess risk of atrial fibrillation and possibly increased bone loss in postmenopausal women. Treatment of hyperthyroidism in nonpregnant women is recommended only if low TSH persists after 4 to 12 weeks and the level is less than 0.1 mIU/L.5 This article discusses the detection and management of thyroid disease in pregnancy, concentrating on 2 representative cases. (See TABLE 1, page 28, for a list of the full spectrum of thyroid disorders.)
Meena Khandelwal, MD
Associate Professor, Department of Obstetrics and Gynecology, Division of MaternalFetal Medicine, Cooper University Hospital, University of Medicine and Dentistry of New Jersey, Camden, NJ The author reports no financial relationships relevant to this article.
CASE 1 History of Graves disease
S.H., 32, is 6 weeks pregnant with her rst child. She has a history of Graves disease, and underwent radioactive iodine treatment 10 years ago. She then became hypothyroid and has been on levothyroxine replacement for the past 9 years. She visits her endocrinologist annually and reports good control on 125 g daily of oral levothyroxine sodium. How should her pregnancy be managed?
D u l t a h n yrig r perso p o C Fo
ea y H n e nl owd se o
ed M h lt
ia
IN THIS ARTICLE
Signs and symptoms of thyroid dysfunction
Page 31
When the mother has a history of Graves disease, regardless of her current thyroid state, 1% to 5% of newborns develop hyperthyroidism due to transplacental passage of thyroid-stimulating immunoglobulins (TSI). Fetal or neonatal hyperthyroidism is associated with fetal tachycardia (heart rate >160 bpm), poor growth, goiter, craniosynostosis, and advanced bone age. Therefore, fetal growth and heart rate should be monitored throughout pregnancy in these women. Investigators have published monograms on fetal thyroid measurement,6 and even argued that Doppler ultrasonography can differentiate between fetal hypo- and hyperthyroidism caused by drugs or disease processes.7 However, measurement of TSI levels (poor predictive value) and ultrasonography for fetal goiter (low yield) are controversial.
CONTINUED
Consequences of untreated dysfunction
Page 32
Screening recommendations
Page 38
w w w. o bg m a nagem ent .com
May
2007
OBG MANAGEMENT
27
For mass reproduction, content licensing and permissions contact Dowden Health Media.
Thyroid disorders in pregnancy
TABLE 1
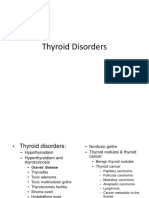
The spectrum of thyroid disorders is wide
Hypothyroidism Hashimotos or subacute thyroiditis Subclinical hypothyroidism Subclinical hypothyroxemia Postpartum thyroiditis Secondary hypothyroidism Hypothalamic dysfunction Radioactive iodine therapy Thyroidectomy Iodine deficiency TSH receptor resistance/mutation Hyperthyroidism Graves disease Subclinical hyperthyroidism Thyroid storm Secondary hyperthyroidism TSH-producing pituitary adenoma Toxic multinodular goiter Toxic adenoma Subacute thyroiditis Metastatic follicular thyroid cancer Iodine excess Factitious/iatrogenic Thyroid hormone resistance syndrome Struma ovarii Gestational trophoblastic neoplasia Hyperemesis gravidarum
TSH level, if no reading is available from the past 3 months. If baseline TSH is less than 2.5 mIU/L, the dosage increase is probably adequate. If the TSH exceeds 2.5 mIU/L, however, I would ask the patient to take 1 extra pill (125 g) on 2 days of the week (>30% dosage increase) and measure TSH again 4 to 6 weeks later (thyroxine takes 5 weeks to equilibrate after a change in dosage). Once the dosage has been adequately adjusted, I would monitor TSH every 6 to 8 weeks until delivery. At that time, the dosage should be reduced to the prepregnancy level, with TSH measured again in 4 to 6 weeks to confirm that the dosage is adequate. Levothyroxine absorption is hampered by ferrous sulfate, aluminum hydroxide antacids, proton-pump inhibitors, and cholestyramine. Levothyroxine should be ingested at least 4 hours before or after the prenatal vitamin. The metabolism of levothyroxine is altered by phenytoin, carbamazepine, and rifampin.
FAST TRACK
Levothyroxine should be ingested at least 4 hours before or after the prenatal vitamin
Subclinical hypothyroidism can progress to overt disease The majority of women with hypothyroidism are asymptomatic, with only 20% to 30% having any complaints, usually Another important consideration: nonspecific (TABLE 2, page 31). Women The requirement for thyroxine hor- with 1 or 2 symptoms are no more likely mone increases by approximately 30% to have abnormal thyroid function tests in women on thyroid supplementation than are asymptomatic women. during pregnancy.8 This has been demOvert hypothyroidism is primarily onstrated in more than 9 studies, with diagnosed with laboratory testsspecifiathyrotic women experiencing greater cally, low free thyroxine (FT4) or free triincreases than women with autoimmune iodothyronine (FT3), or both, resulting in hypothyroidism.9 The need for thyroxine elevated TSH levels. increases as early as 5 weeks gestation If untreated, overt hypothyroidism and plateaus by 16 weeks. is associated with significant morbidity Because hypothyroxemia or hypo- in both the nonpregnant and pregnant thyroidism (clinical or subclinical) may states (TABLE 3, page 32). Levothyroxine be associated with adverse neurodevel- is easily administered and well tolerated, opment in the newborn, I recommend with no to few adverse effects with apincreasing the dosage of levothyroxine propriate follow-up.10 In women with subclinical hypothyat the first encounter with this patient to 150 g/day (<25% dosage increase). roidism, only 1 of the thyroid function I also suggest measuring the baseline tests is elevatedeither elevated TSH
OBG MANAGEMENT May 2007
28
Thyroid disorders in pregnancy
with normal free thyroid hormone levels (mild thyroid failure) or normal TSH with low FT4 levels (hypothyroxemia). Most cases of mild thyroid failure are thought to be related to thyroid dysfunction, whereas hypothyroxemia is usually associated with a deficiency of iodine. Subclinical hypothyroidism can occur in women with a history of thyroid disease, after surgery or radioactive iodine therapy for toxic goiter, or as the result of an inadequate dosage of thyroid medication. It can also occur in women with no history of thyroid dysfunction, detected in routine testing in women with no symptoms or with nonspecific complaints that could be related to thyroid disease. Experts agree that women with secondary subclinical disease should be treated to achieve a euthyroid state because approximately 5% per year will develop overt disease. Considerable controversy clouds management of women with primary subclinical hypothyroidism. Subclinical hypothyroidism is more common among white women (~67%) than among black women. Subclinical hyperthyroidism is more elusive Overt hyperthyroidism can be detected through symptom-based screening (TABLE 2). Subclinical hyperthyroidism is defined as low TSH with normal thyroid hormone levels. The pituitary appears to be more sensitive to the presence of thyroid hormones than to their absence. Subclinical hyperthyroidism is most common in black women and smokers. Approximately 50% of women with subclinical disease will have normal TSH levels several weeks to 1 year later. Because subclinical hyperthyroidism can occur in up to 20% of women on thyroid replacement therapy, the dosage should be adjusted to achieve a euthyroid state.
TABLE 2
Know these signs and symptoms of thyroid dysfunction
HYPOTHYROIDISM HYPERTHYROIDISM
Fatigue Constipation Somnolence Cold intolerance Hair loss Depression Decreased libido Menstrual irregularities Weight gain despite poor appetite Dry skin Deafness Hoarseness Paresthesia Carpal tunnel syndrome Periorbital puffiness Slow cerebration or movement Slowing ankle jerk Goiter
Resting tremors Hyperdefecation Insomnia Heat intolerance Diaphoresis Nervousness Palpitations
Weight loss
Warm, moist skin Ophthalmopathy Sinus tachycardia
Hyperreflexia Thyromegaly
FAST TRACK
CASE 2 Diabetes, with a family history of hypothyroidism
M.H., 30, is 12 weeks pregnant with her second child and reports a 12-year history of diabetes. Before she became pregnant, she was taking insulin, with HbA1C = 8.5%. Her history includes a mother with hypothyroidism. How should she be managed?
Approximately 5% of women with secondary subclinical hypothyroidism develop overt disease each year
Besides the obvious need for good diabetes control, this case merits screening for thyroid dysfunction, as the patient has 2 risk factors (TABLE 4, page 37). One prominent controversy of the 21st century is whether all pregnant women should undergo routine screening for hypothyroidism. The controMay 2007 OBG MANAGEMENT
w w w. o bg m a nagem ent .com
31
Thyroid disorders in pregnancy
TABLE 3
Consequences of untreated thyroid dysfunction are signicant
HYPOTHYROIDISM HYPERTHYROIDISM
nant or planning to conceive should be based on many factors, most notably whether treatment prevents impaired neonatal neurodevelopment and preterm delivery. A mothers elevated TSH level can have lasting effects in the child Haddow and colleagues1 measured the IQ of 47 children, ages 7 to 9 years, whose mothers had had an elevated serum TSH concentration in the second trimester, 15 children whose mothers had high serum TSH values in combination with low thyroxine levels in the second trimester, and 124 children whose mothers had normal TSH values. None of these children had hypothyroidism at birth. The children of the women with an elevated TSH concentration had lower IQs. Interestingly, the group with hypothyroxemia was not evaluated at the time, and the mean FT4 level was low in the entire group, suggesting overt hypothyroidism rather than subclinical disease. In a study from the Netherlands, Pop and associates2 found impaired psychomotor function in 22 infants (age 10 months) whose mothers had had FT4 below the 10th percentile at 12 weeks of gestation, compared with 194 infants whose mothers had normal readings. When these children were reevaluated at 2 years, no neurodevelopmental delay was found in the infants whose mothers had a spontaneously increased free thyroxine level after the first trimester. There is much speculation about precisely when thyroid hormone is critical for fetal brain development. The study by Pop and associates2 would suggest it is important after the first trimester. That study also recommends exogenous thyroxine for FT4 values below 0.96 ng/mL (12 pmol/L). In Italy, Vermiglio and coworkers11 conducted behavioral and neuropsychological testing in 27 children at ages 18 to 36 months and again at 8 to 10
Nonpregnant state Hyperlipidemia Atherosclerosis Osteoporosis Neuropsychiatric disorders Neuropsychiatric disorders with or without dementia/Alzheimers disease Reduced functional status and quality of life Atrial fibrillation Congestive heart failure
Reduced functional status and quality of life Pregnancy Spontaneous abortion Preterm delivery <32 weeks Low birth weight Perinatal morbidity and mortality Preeclampsia/ gestational hypertension Anovulation Cesarean delivery Postpartum hemorrhage Placental abruption Nonreassuring fetal heart rate tracing Impaired neurodevelopment Subclinical disease Risk factor for overt disease
Spontaneous abortion Preterm labor Low birth weight Stillbirth Preeclampsia
Risk factor for overt disease
versy extends to screening all women of childbearing age.
$64,000 question: Should all women be screened?
Screening would involve testing thyroid function in women with no history and few or no signs and symptoms of thyroid dysfunction. Such screening could be population-based (using special methods to recruit, contact, and follow patients) or case-finding (performed on patients who present for unrelated reasons). The decision to screen a woman who is preg32
OBG MANAGEMENT May 2007
Thyroid disorders in pregnancy
How common?
Anterior pituitary Thyroid levels in blood too high: TSH secretion in pituitary decreases
+ TSH TSH
Thyroid gland
Thyroid levels in blood too low: TSH secretion in pituitary increases
Thyroid disorders affect approximately 5% of the general population, two thirds of them women.17 Subclinical hypothyroidism occurs in an additional 4.3%, and subclinical hyperthyroidism in 0.7%. In pregnancy, subclinical disease is present in 3.6% of women; overt hypothyroidism, in 2.5%; and overt hyperthyroidism, in 0.2%. In addition, thyroid disease affects 5% to 9% of postpartum women.14
years. Mothers of 16 of these children were from a moderately iodine-deficient area (group A), and the mothers of 11 children were from a marginally iodinesufficient area and were monitored with thyroid function tests in the first trimester (group B). Attention-deficit and hyperactivity disorders were more prevalent in group A. Two studies published in 2006 also suggest that maternal free thyroxine levels in the first trimester of pregnancy correlate with impaired neonatal behavior at 3 months, and impaired mental development at ages 6, 9, and 12 months.3,4
34
OBG MANAGEMENT May 2007
No consensus on whom to test or what test is best There is no clear agreement about which population should be targeted for screening or what test to use. Most medical societies do not recommend routine screening, including the American College of Obstetricians and Gynecologists, which recommends TSH testing only in women with a history of thyroid disease and in women with symptoms (but does not specify which symptoms or how many symptoms warrant testing). A majority of organizations agree that all high-risk women should be tested when pregnancy is planned or as soon as pregnancy is confirmed (TABLE 5, page 38). Proponents of routine screening argue that it may limit health risks to children and save money in the long run, and they point out that thyroid disease is easy to treat with pills. Opponents note that no cost-benefit analysis has been performed, the benefits of treating mild disease are unclear, and screening a large population could be a significant expense ($40100 per person) and would necessitate a lifelong commitment to daily medication in asymptomatic patients. As a diagnostic test, the TSH immunoassay has 98% sensitivity and 92% specificity, and the current third-generation test lacks biases between methods and does not require method-specific reference ranges. However, it has low predictive value as a screening test (725%), possibly because of multiple confounding variables (TABLE 6, page 41). Despite being the gold standard, it can lead to falsely positive results. As for the value of FT4 alone as a screening test, we lack sufficient data on its utility. Another problem is that equilibrium dialysis, the most accurate and reliable laboratory method to measure FT4, is too technically complex and expensive for routine use. The most widely used 2-step radioimmunoassay is automated, but different methods are used by different commercial laboratories, cutoffs vary for every laboratory, and
Rob Flewell
Thyroid disorders in pregnancy
TABLE 4
Risk factors for hypothyroidism include other autoimmune disorders
Family history of thyroid disease More than 3 symptoms History of postpartum thyroid disease Type 1 diabetes mellitus Recurrent spontaneous abortions Unexplained intrauterine fetal demise Other autoimmune disorders Vitiligo Addisons disease Pernicious anemia Multiple sclerosis Rheumatoid arthritis Sjgrens disease
the results are sensitive to abnormal binding-protein states such as pregnancy in a method-specific manner. Tandem mass spectrometry is as reliable as equilibrium dialysis, but is not yet readily available.12 Another consideration: The physiologic changes in pregnancy render the cutoffs for the nongravid state inapplicable. TSH is lower in pregnancy, whereas the FT4 level is probably slightly increased or unchanged (TT4 is 1.5 times the prepregnancy value). The normal reference values in each trimester of pregnancy from iodine-sufficient, autoimmune thyroid antibodynegative women are becoming available for TSH,12 as are nomograms that adjust for fetal number and gestational age.13 The measurement of FT4 still needs to be standardized across laboratories (method-specific, trimester-specific, and, possibly, population-specific reference ranges) for pregnancy.
the TSH level is less than 0.1 mIU/L: High-risk women: postmenopausal or over age 60 Low-risk women with cardiac disease, low bone density, or nodular thyroid disease. If the TSH level is between 0.1 and 0.5 mIU/L, treatment is recommended for high-risk women with cardiac disease, low bone density, or nodular thyroid disease. Subclinical hypothyroidism with a TSH level of 4.5 to 10 mIU/L need not be treated even in an elderly woman or a patient with a high antibody titer. Treatment of any woman is beneficial when the TSH level exceeds 10 mIU/L because it can ease symptoms, reduce low-density lipoprotein cholesterol, and prevent progression to overt disease. However, treatment may not lower morbidity and mortality and carries a roughly 20% risk of causing subclinical hyperthyroidism. It also involves a lifelong commitment to daily medication. How to treat subclinical hypothyroidism in pregnancy It is clear that overt hypothyroidism warrants treatment in both the pregnant and nonpregnant states, but the management of subclinical disease remains controversial. No trials have assessed the benefits of thyroid hormone replacement on the neuropsychological development of the newborn. Expert opinion suggests that women be treated if they are planning a pregnancy, are already pregnant, or have high TSH or low FT4. Until we have more data, pregnant women and those planning a pregnancy should be treated with levothyroxine (starting at 2 g/kg/day) if they are found to have elevated TSH or low FT4. Two studies will answer questions about effects in pregnancy The Controlled Antenatal Thyroid Screening (CATS) study will be completed in 2009, and the National Institute of Child Health and Human Development MaMay 2007 OBG MANAGEMENT
FAST TRACK
Treat gravidas and women planning to conceive with levothyroxine (starting at 2 g/kg/day) if they have an elevated TSH or low FT4
How to manage subclinical thyroid disorders
In the nonpregnant state, subclinical hyperthyroidism should be treated in the following groups if the abnormal thyroid levels persist beyond 4 to 12 weeks and
w w w. o bg m a nagem ent .com
37
Thyroid disorders in pregnancy
TABLE 5
Comparison of screening recommendations highlights lack of consensus (and, in pregnancy, the absence of guidance)
YEAR ORGANIZATION NONPREGNANT STATE PREGNANCY
1994
American Association of Clinical Endocrinologists (AACE) American Academy of Family Physicians American College of Physicians
Periodic assessment via thyroid function tests in older women
No recommendation
1998
Office screening of women >50 years of age Measure TSH every 5 years in women age 35 and older (probably men also) Measure TSH every 5 years in women age 65 and older
No recommendation
2000
American Thyroid Association (ATA)
No recommendation
2002
American College of Obstetricians and Gynecologists Institute of Medicine
No screening recommended
2003
Screening is not cost-effective in No recommendation Medicare population Routine screening of children and adults is not recommended No population-based screening, but aggressive case finding in women at high risk and those over age 60 No recommendation
2004
United States Preventive Services Task Force AACE, ATA, the Endocrine Society Consensus Group
2004
Do not support routine testing; recommend aggressive case finding and screening pregnant women at high risk
FAST TRACK
Postpartum thyroid dysfunction affects 5% to 9% of women and usually involves psychiatric symptoms
ternalFetal Medicine Units (NICHDMFMU) study will conclude in 2014. The CATS study screened 22,000 pregnant women in the United Kingdom before 16 weeks gestation. Half these women were treated with levothyroxine in pregnancy if they had a TSH measurement above the 97.5th percentile or FT4 below the 2.5th percentile, and half had their blood samples stored and tested only after delivery.14 Cutoff values were derived from previously obtained antenatal sera from well-dated pregnancies, and were adjusted after every 2,000 to 3,000 samples. The CATS study was conducted in an iodine-sufficient area with a median urinary iodine excretion of 100 g/L (range: 11240 g/L). Each group contained 400 women with subclinical hypothyroidism (52% had low FT4, 45% had high TSH, and 3% had both). Antithyroid peroxidase antibodies were
OBG MANAGEMENT May 2007
present in 50% of women with elevated TSH but in only 10% of women with low FT4. Neuropsychological development in their children is being tested at 3 years of age. The NICHD-MFMU study plans to screen 110,000 women at 14 centers over 2 years, and will randomize roughly 1,000 women to thyroxine treatment or placebo. They plan to assess intellectual development of the infants yearly for 5 years, and test the mothers for postpartum thyroid dysfunction and follow them at 1 and 5 years to detect the rate of progression to overt hypothyroidism.
Postpartum dysfunction can be transient or permanent
Postpartum thyroid dysfunction (PPTD) is an autoimmune disorder that occurs at 13 to 19 weeks postpartum, affects 1 in 12
38
Thyroid disorders in pregnancy
women worldwide, and is usually associated with psychiatric symptomatology.15 PPTD also is strongly associated with antithyroid peroxidase antibodies (TPOAbs).16 Premawardhana and colleagues found that 10% of women are TPOAbs-positive in the first trimester; of these, 50% develop PPTD. Of the women with PPTD, 20% to 30% develop permanent hypothyroidism, and an additional 30% to 40% develop it by 7 years. In contrast, only 5% of women without PPTD progress to overt disease by 7 years. These findings have generated considerable controversy about routine screening for PPTD. Proponents argue that PPTD is highly prevalent, linked to considerable morbidity, is easily diagnosed with relatively inexpensive tests, and is easy to treat effectively. Critics note the lack of consensus on the best screening test (thyroid function test versus TPOAbs), optimal timing of screening (early pregnancy or postpartum), and lack of high-quality, prospective cost-benefit analyses. The NICHD-MFMU hopes to resolve these controversies.
References
1. Haddow JE, Palomaki GE, Allan WC, et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child [see comment]. N Engl J Med. 1999;341:549555. 2. Pop VJ, Kuijpens JL, van Baar AL, et al. Low maternal free thyroxine concentrations during early pregnancy are associated with impaired psychomotor development in infancy [see comment]. Clin Endocrinol. 1999;50:149155. 3. Kasatkina EP, Samsonova LN, Ivakhnenko VN, et al. Gestational hypothyroxinemia and cognitive function in offspring. Neurosci Behav Physiol. 2006;36:619624. 4. Kooistra L, Crawford S, van Baar AL, Brouwers EP, Pop VJ. Neonatal effects of maternal hypothyroxinemia during early pregnancy. Pediatrics. 2006;117:161167. 5. Surks MI, Ortiz E, Daniels GH, et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management [see comment]. JAMA. 2004;291:228238. 6. Ranzini AC, Ananth CV, Smulian JC, Kung M, Limbachia A, Vintzileos AM. Ultrasonography of the fetal thyroid: nomograms based on biparietal diameter and gestational age. J Ultrasound Med. 2001;20:613-7. 7. Polak M, Le Gac I, Vuillard E, et al. Fetal and neonatal thyroid function in relation to maternal Graves disease. Best Practice & Research Clin Endocrinol Metab. 2004;18:289-302.
TABLE 6
What makes a TSH measurement falsely high or low?
ELEVATED TSH LOW TSH
Recovery from nonthyroidal illness Late evening TSH surge Assay variability Adrenal insufficiency Drugs: metoclopramide, amiodarone, cholecystographic dye (sodium ipodate)
Euthyroid sick syndrome Recovery from normal pregnancy
Drugs: glucocorticoids, dopamine
8. Alexander EK, Marqusee E, Lawrence J, Jarolim P, Fischer GA, Larsen PR. Timing and magnitude of increases in levothyroxine requirements during pregnancy in women with hypothyroidism [see comment]. N Engl J Med. 2004;351:241249. 9. Mandel SJ, Spencer CA, Hollowell JG. Are detection and treatment of thyroid insufficiency in pregnancy feasible? Thyroid. 2005;15:4453. 10. Negro R, Formoso G, Mangieri T, Pezzarossa A, Dazzi D, Hassan H. Levothyroxine treatment in euthyroid pregnant women with autoimmune thyroid disease: effects on obstetrical complications [see comment]. J Clin Endocrinol Metab. 2006;91:25872591. 11. Vermiglio F, Lo Presti VP, Moleti M, et al. Attention deficit and hyperactivity disorders in the offspring of mothers exposed to mild-moderate iodine deficiency: a possible novel iodine deficiency disorder in developed countries. J Clin Endocrinol Metab. 2004;89:60546060. 12. Soldin OP, Tractenberg RE, Hollowell JG, Jonklaas J, Janicic N, Soldin SJ. Trimester-specific changes in maternal thyroid hormone, thyrotropin, and thyroglobulin concentrations during gestation: trends and associations across trimesters in iodine sufficiency. Thyroid. 2004;14:10841090. 13. Dashe JS, Casey BM, Wells CE, et al. Thyroid-stimulating hormone in singleton and twin pregnancy: importance of gestational age-specific reference ranges. Obstet Gynecol. 2005;106:753757. 14. Lazarus JH, Premawardhana LDKE. Screening for thyroid disease in pregnancy. J Clin Pathol. 2005;58:449 452. 15. Nicholson WK, Robinson KA, Smallridge RC, Ladenson PW, Powe NR. Prevalence of postpartum thyroid dysfunction: a quantitative review. Thyroid. 2006;16:573582. 16. Premawardhana LDKE, Parkes AB, John R, Harris B, Lazarus JH. Thyroid peroxidase antibodies in early pregnancy: utility for prediction of postpartum thyroid dysfunction and implications for screening. Thyroid. 2004;14:610615. 17. Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III) [see comment]. J Clin Endocrinol Metab. 2002;87:489499.
FAST TRACK
A late evening TSH surge can cause a falsely elevated TSH measurement
w w w. o bg m a nagem ent .com
May
2007
OBG MANAGEMENT
41
You might also like
- 13Document5 pages13najmulNo ratings yet
- Comparison Between Visual Inspection of Cervix and Cytology Based Screening Procedures in BangladeshDocument5 pagesComparison Between Visual Inspection of Cervix and Cytology Based Screening Procedures in BangladeshnajmulNo ratings yet
- 16Document49 pages16najmulNo ratings yet
- Comparison Between Visual Inspection of Cervix and Cytology Based Screening Procedures in BangladeshDocument5 pagesComparison Between Visual Inspection of Cervix and Cytology Based Screening Procedures in BangladeshnajmulNo ratings yet
- 11Document4 pages11najmulNo ratings yet
- 9Document7 pages9najmulNo ratings yet
- 12Document8 pages12najmulNo ratings yet
- 2Document7 pages2najmulNo ratings yet
- Dissertation Psychosocial Effects of Cervical CancerDocument69 pagesDissertation Psychosocial Effects of Cervical CancernajmulNo ratings yet
- 7Document6 pages7najmulNo ratings yet
- Case in Ovarian CystsDocument4 pagesCase in Ovarian CystsAde Gustina SiahaanNo ratings yet
- Malignant Transformation in An Ovarian Mature Cystic Teratoma: A Case ReportDocument4 pagesMalignant Transformation in An Ovarian Mature Cystic Teratoma: A Case ReportnajmulNo ratings yet
- 8Document6 pages8najmulNo ratings yet
- 3Document7 pages3najmulNo ratings yet
- Kanker OvariumDocument4 pagesKanker OvariumRizna SaidNo ratings yet
- ProfileDocument3 pagesProfilenajmulNo ratings yet
- SynopsisDocument15 pagesSynopsisnajmulNo ratings yet
- Retailing, Clothing and Textiles Production in Australia: Sally WellerDocument18 pagesRetailing, Clothing and Textiles Production in Australia: Sally WellerMallesh MalluNo ratings yet
- How To Start An Export/Import BusinessDocument18 pagesHow To Start An Export/Import Businesscontactway1No ratings yet
- 951 44 5752 8Document114 pages951 44 5752 8najmulNo ratings yet
- Centre For Continuing Education (Cce)Document2 pagesCentre For Continuing Education (Cce)najmulNo ratings yet
- 4Document6 pages4najmulNo ratings yet
- Umi Umd 3091Document120 pagesUmi Umd 3091najmulNo ratings yet
- Nottingham MBA Scholarship Application Form 2014/15Document2 pagesNottingham MBA Scholarship Application Form 2014/15najmulNo ratings yet
- StuDocument17 pagesStunajmulNo ratings yet
- CIMA Syllabus PDFDocument80 pagesCIMA Syllabus PDFMuhammad AshrafNo ratings yet
- Kamau GraceDocument44 pagesKamau GracenajmulNo ratings yet
- 1113-19 CM University Brochure - FA3 - LRDocument20 pages1113-19 CM University Brochure - FA3 - LRnajmulNo ratings yet
- AttachmentDocument2 pagesAttachmentnajmulNo ratings yet
- Part 01 (A)Document12 pagesPart 01 (A)najmulNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- S1 2013 280476 BibliographyDocument4 pagesS1 2013 280476 BibliographyrizkaNo ratings yet
- The Technique: of ThyroidectomyDocument5 pagesThe Technique: of Thyroidectomyعمر كمالNo ratings yet
- Dr. Kunta Setiaji (ThyroidNodule) MDocument18 pagesDr. Kunta Setiaji (ThyroidNodule) MRachman UsmanNo ratings yet
- Struma Nodosa 2Document10 pagesStruma Nodosa 2dewi rositaNo ratings yet
- Thyroid Benign TumorDocument30 pagesThyroid Benign TumormackieccNo ratings yet
- SK2 Pertemuan 2Document61 pagesSK2 Pertemuan 2andistinoorfitryNo ratings yet
- Guideline For Hyperthyroidism ManagementDocument9 pagesGuideline For Hyperthyroidism ManagementSyaimee Annisa AzzahraNo ratings yet
- Thyrotoxicosis and Graves DiseaseDocument25 pagesThyrotoxicosis and Graves DiseaseMeekel SusikuNo ratings yet
- Subacute Thyroiditis PDFDocument102 pagesSubacute Thyroiditis PDFIoana BodescuNo ratings yet
- Thyroid Disorders: Hyperthyroidism HypothyroidismDocument66 pagesThyroid Disorders: Hyperthyroidism HypothyroidismGabz GabbyNo ratings yet
- Endocrine DisordersDocument28 pagesEndocrine DisordersRhitzle Ann50% (2)
- 09-2013 UTpt EndoDocument44 pages09-2013 UTpt Endomina0% (1)
- Pharmacotherapy of Thyroid DisordersDocument6 pagesPharmacotherapy of Thyroid DisordersShaden -No ratings yet
- Thyroid ReportDocument105 pagesThyroid ReportAARVNo ratings yet
- MCQ ThyroidDocument6 pagesMCQ ThyroidFaridOrahaNo ratings yet
- Acog Practice Bulletin TiroidesDocument10 pagesAcog Practice Bulletin TiroidesMerpi Alvarez Goris100% (1)
- NM Brosura ENG RED OldDocument29 pagesNM Brosura ENG RED OldDacan MiticNo ratings yet
- Hyperthyroidism: Div. Endokrin-Metabolisme Dan Diabetes. Dep Ilmu Penyakit Dalam FK USU / RSUP HAM MedanDocument46 pagesHyperthyroidism: Div. Endokrin-Metabolisme Dan Diabetes. Dep Ilmu Penyakit Dalam FK USU / RSUP HAM MedanDaniel IvanNo ratings yet
- Thyroid Gland Clinical Chemistry 2 (Laboratory) : LessonDocument4 pagesThyroid Gland Clinical Chemistry 2 (Laboratory) : LessonCherry Ann ColechaNo ratings yet
- 2013 ENDOCRINE PHARMACOLOGY Word Notes PDFDocument52 pages2013 ENDOCRINE PHARMACOLOGY Word Notes PDFNicole Opao100% (4)
- Thyroid Disorder NCPDocument9 pagesThyroid Disorder NCPKen RegalaNo ratings yet
- Nursing Management of A Patient With: HyperthyroidismDocument31 pagesNursing Management of A Patient With: Hyperthyroidismember parkNo ratings yet
- Ata Hyperthyroidism BrochureDocument3 pagesAta Hyperthyroidism BrochureKumalaAudiKusumaNo ratings yet
- ThyrotoxicosisDocument15 pagesThyrotoxicosischrysandre100% (1)
- Thyroid Disease: Dr. Gusti Hariyadi Maulana, MSC, SPPD-KGH Internist-NephrologistDocument30 pagesThyroid Disease: Dr. Gusti Hariyadi Maulana, MSC, SPPD-KGH Internist-NephrologistNurul HikmaNo ratings yet
- HyperthyroidismDocument59 pagesHyperthyroidismjoanna73% (11)
- Autoimmune DiseasesDocument4 pagesAutoimmune DiseasesMahak JandwaniNo ratings yet
- Herbal Formulation Considerations For Autoimmune DisordersDocument26 pagesHerbal Formulation Considerations For Autoimmune Disordershitesh mendirattaNo ratings yet
- Anthroposophy Autoimmune - Diseases PDFDocument30 pagesAnthroposophy Autoimmune - Diseases PDFpenfo100% (1)
- Chirurgia TiroideiDocument15 pagesChirurgia TiroideiAna CotomanNo ratings yet