Professional Documents
Culture Documents
26 3 Movahed
Uploaded by
balab2311Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
26 3 Movahed
Uploaded by
balab2311Copyright:
Available Formats
Application of cranial bone grafts for reconstruction of maxillofacial deformities
Reza Movahed, DMD, Lecio P. Pinto, DDS, PhD, Carlos Morales-Ryan, DDS, MSD, Will R. Allen, DDS, and Larry M. Wolford, DMD
This retrospective study evaluated outcomes with the use of calvarial bone grafts (CBGs) in maxillofacial reconstruction as well as donor and recipient site complications. The records of 50 consecutive patients from a private practice were reviewed; there were 34 women and 16 men, with an average age of 32.4 years (range 16 to 66 years). Among the 50 patients, CBGs were placed in 63 sites: the ramus (10), nasal dorsum (14), maxilla/alveolar ridge (12), glenoid fossa/temporal bone (14), mandibular body/symphysis (3), and orbitozygomatic complex (10). The longest follow-up averaged 22.4 months (range 12 to 48 months). An outer-table CBG harvest technique was utilized. All subjects were evaluated for infection, dehiscence, loss of graft, and any other complications. Three complications occurred (5%) at the recipient sites. Two grafts became infected requiring removal, and one nasal dorsal graft was mobile but remained in position. At 50 donor sites, 2 complications (4%) occurred, resulting in dural tears in two patients that were immediately repaired with no untoward consequence. In conclusion, CBGs are an effective bone source for maxillofacial reconstruction with low donor and recipient site complications.
utogenous bone grafts are the gold standard for reconstruction of maxillofacial defects. Autogenous bone becomes osseointegrated and vascularized at its site of implantation, which decreases the chances of infection, displacement, and foreign body reaction compared with alloplastic implants. The drawbacks are the harvest time, donor site morbidity, graft resorption, modeling changes, and harvest volume limitations (1). The clinician has to choose the site of bone harvest wisely, taking into account the nature of the reconstruction and volume requirements. Autogenous bone can be harvested from multiple sites, including the calvarium, tibia, anterior ileum, posterior ileum, rib, sternoclavicle, zygoma, mandible, and so forth. The use of calvarial bone grafts (CBGs) was rst reported in 1670, when Van Meekren reconstructed a Russian soldiers calvarial defect utilizing a CBG from a dog (2). Other early contributors were Konig (3) and Muller (4) in 1890, reporting on human CBGs for the correction of posttraumatic craniomaxillofacial defects. In the 1980s, Tessier popularized the technique as an aid in the correction of craniofacial deformities (5). Pensler and McCarthy (6) published a study on the
252
thickness and specic anatomy of the calvarium for safe and predictable harvesting. CBGs have been utilized in reconstruction of the mandible (7), maxilla (8, 9), orbital oor (10, 11), orbital roof (12), malar region (13), and as a strut for nasal reconstruction (14). In craniofacial surgery, the CBG can be used to reconstruct advancement gaps resulting from Lefort I, II, and III procedures. Outer-table CBGs can be taken from the parietal region of the skull, posterior to the coronal suture, where the skull is the thickest. CBGs can usually be harvested with minimal morbidity at the donor site, with a scar hidden in the hair-bearing region. The geometry and convexity of the CBG makes it suitable for most maxillofacial reconstructions. Due to its cortical nature, the CBG can be rigidly xated, providing a stable platform for revascularization and osseointegration. In maxillofacial reconstruction, the proximity of the CBG donor site to the surgical site avoids the need for a second distant surgical eld, but may preclude simultaneous bone graft harvest and recipient site preparation. Postoperative complications are few, and recovery is relatively painless. The donor site defect of the outer table can be reconstructed with a bone cement that solidies with endothermic reaction. The graft should not be harvested in the midline because of the risk of injuring the sagittal sinus. METHODS This retrospective study consisted of 50 consecutive patients (34 women and 16 men), treated from 1996 to 2010 by a single private practice, in whom only cranial bone grafts were used to reconstruct maxillofacial defects (Figures 12). This study was exempt from institutional review board approval. Records were reviewed, including operative reports, discharge summaries, progress notes, radiographs, and photographs. Subjects were excluded from the study if they had less than 12 months of follow up or inadequate records. All subjects underwent bone harvesting and grafting by the same surgeon (Wolford). The outer-table CBG harvest technique
From the Department of Oral and Maxillofacial Surgery, Baylor College of Dentistry, Texas A&M University System Health Science Center, and Baylor University Medical Center at Dallas. Corresponding author: Larry Wolford, DMD, 3409 Worth Street, Suite 400, Dallas, TX 75246 (e-mail: lwolford@swbell.net). Proc (Bayl Univ Med Cent) 2013;26(3):252255
Figure 1. Loss of left maxillary alveolar ridge secondary to trauma, reconstructed with layered calvarial bone grafts.
Figure 3. Surgical approach for harvesting of calvarial bone grafts.
The evaluation consisted of the clinical description of any complication at the donor or recipient site during the procedure, immediately after surgery, and at longest followup. The healing and integration of grafts were evaluated clinically and radiographically. RESULTS Fifty patients with 63 grafted areas were evaluated. The distribution of grafted areas is shown in the Table. The six grafted areas Figure 2. Reconstruction of right ramus and temporomandibular joint with calvarial bone grafts and TMJ included mandibular body/symphysis, ramus, Concepts prosthesis (previously Techmedica Inc, Camarillo, CA), following removal of Vitek total joint nasal dorsum, maxilla/alveolar ridge, glenoid prosthesis (Vitek Inc, Houston, TX), containing Proplast/Teflon that destroyed the ramus. One calvarial fossa, and orbitozygomatic complex. Patients bone graft was attached to the prosthesis to replace the lateral cortical bone, and the second piece was average age was 32.4 years (range 16 to placed on the medial side of the ramus to replace the medial cortex. 66 years), and the longest follow-up averaged 22.4 months (range 12 to 48 months). was utilized in all patients, and the volume of the bone was harThe percentage of complications associated with the revested according to the recipient site defect. The harvest of the cipient sites was calculated from the total number of grafted CBG was performed following completion of the recipient site anatomical locations, while the percentage of complications preparation. The initial incision was made 2 cm posterior to the associated with the donor site was calculated using the total hair line and 2 cm lateral to the midline. The incision was made in number of patients, since there was a single donor site per paa curvilinear fashion, superior to the temporalis muscle attachment tient. At the recipient sites, three complications were noted (Figure 3). Using a #10 scalpel, the incision was carried down to the (4.8%). In one case of a maxillary ridge augmentation with cranium. Raney clips were placed at the edges of the incision. Minisimultaneous osseointegrated dental implants, the graft was lost mal use of Bovie cautery and minimized harvest time decreased secondary to infection. The second patient had facial congenital damage to the hair follicles. The bone to be harvested was outlined inltrating lipomatosis and received a unilateral orbitozygousing a 701 burr, to correlate to the amount of bone necessary for matic reconstruction with a CBG, following extensive resection the recipient site. The site of harvest was usually 2 cm lateral to the of the tumor, which involved the orbit, zygoma, and associated sagittal and squamoparietal sutures. The unicortical osteotomies soft tissue. There was partial loss of the graft secondary to inof outer cortex bone to be harvested were connected. The inferior fection, related to the poorly vascularized recipient bed. In the or superior edge of the donor site was beveled using a pineapple third case a nasal dorsal reconstruction graft became mobile, burr in order to access the diplo, deep to the outer cortex. Using a failing to integrate and fuse to the nasal bony structure, but it combination of slightly curved and straight osteotomies, the bone remained in place 3 years after surgery. The rest of the grafts grafts were dislodged from the diplo. The bone was kept in saline healed uneventfully and at the radiographic evaluation appeared and placed on ice for preservation. Hemostasis was achieved. The to demonstrate adequate integration between the graft and the Raney clips were removed, and the incision was closed in a single host bone at long-term follow-up. layer using a 2.0 or 3.0 Prolene suture. A compression dressing At the donor sites, two complications were identied (4.0%). was placed for prevention of hematoma. Sutures were removed A dural tear occurred on a 16-year-old patient who had only 7 to 10 days after surgery. one cortical plate of the parietal bone. The tear was primarily
July 2013 Application of cranial bone grafts for reconstruction of maxillofacial deformities 253
Table. Distribution of grafts and outcome
Reconstruction area Mandibular ramus Nasal dorsum Maxilla/alveolar ridge Glenoid fossa/ temporal bone Mandible Orbitozygomatic complex Total Number of grafts 10 14 12 14 3 10 63 Complications at recipient site None 1 mobile graft, in proper anatomical position 1 infection; graft loss None None 1 infection; partial graft loss 3/63 sites (4.8%) Complications at donor site 2 dural tears; repaired None None None None
low. The outer-table CBG harvest technique is a time-consuming procedure compared with use of alloplastic and tissue-engineered materials. In comparison to bone grafts obtained from other anatomical sites, CBGs benet the operator with one eld of surgical access, eliminating the preparation of a distant second site. The reported complication rates are low. This bone grafting procedure is an eective technique for reconstruction of maxillofacial defects.
1.
repaired. In the second patient the dura tear was also closed primarily. Both patients healed uneventfully. DISCUSSION CBGs are used for a multitude of maxillofacial reconstructions, with low complication rates (15). The literature has reported clinical observation of minimal to no resorption of the CBG at short-term follow-up (16, 17). The reconstruction, although technique sensitive in its adaptation to the recipient site, is safer and more cost-eective than alloplastic grafting (1820). CBGs can be considered the material of choice for maxillofacial reconstruction due to their histocompatibility, anatomofunction, and mechanical properties (21). Additionally, CBGs are fresh live tissue that will revascularize and osseointegrate to adjacent bone, having a low rate of infection (22). Although CBGs require time for harvest, unlike alloplastic graft materials, the disadvantages associated with CBGs are few. When large bone grafts are harvested, the donor defect can be reconstructed with synthetic substitutes, which have been reported to result in infections and inammatory reactions (23). The chance of dural tear exists with outer-table CBG harvesting if the inner table is penetrated (24). In harvesting outer CBGs, the possible complications are intracerebral hematoma, subarachnoid hemorrhage, and cerebrospinal uid leaks (25), none of which were encountered in this study. Additionally, the volume of graft to be harvested could be a limiting factor for large defects requiring reconstruction (24). Removal of the outer table where the residual defect is inadequately lled can result in a cosmetic defect in the skull. Although no controlled human studies have measured the exact rate of resorption and retained volume of CBGs, the clinical studies support stable outcomes (2628). DeLuca et al reported an animal study, where the CBGs had a volume retention rate of 85.1%, and recommended CBGs as the gold standard for craniofacial reconstruction (29). In our retrospective study, the complication rates at the donor site (4.0%) and the recipient site (4.8%) were relatively
254
Rogers GF, Greene AK. Autogenous bone graft: basic science and clinical implications. J Craniofac Surg 2012;23(1):323327. 2. Papel ID, ed. Facial Plastic and Reconstructive Sur2/50 subjects (4.0%) gery, 3rd ed. New York: Thieme, 2009. 3. Konig F. Der knocherne Ersatz grosser Schadeldefekte. Zentralbl Chir 1890;17:65. 4. Muller W. Zur Frage der temporaren Schadelresektion an Stelle der Trepanation. Zentralbl Chir 1890;17:65. 5. Tessier P. Autogenous bone grafts taken from the calvarium for facial and cranial applications. Clin Plast Surg 1982;9(4):531538. 6. Pensler J, McCarthy JG. The calvarial donor site: an anatomic study in cadavers. Plast Reconstr Surg 1985;75(5):648651. 7. Tet S, Vinci R, Zara S, Zizzari V, Cataldi A, Mastrangelo F, Mortellaro C, Gherlone E. Atrophic jaw reconstruction by means of calvarial bone graft: long-term results. J Craniofac Surg 2010;21(4): 11471152. 8. Pereira CC, Gealh WC, Martins MM, Homsi N, Garcia IR Jr. Utilization of surgical trepan for the obtainment of calvarial autogenous bone graft in maxillary reconstructions. J Oral Implantol 2011;37(3):347351. 9. Ferri J, Lauwers L, Jeblaoui Y, Genay A, Raoul G. Le Fort I osteotomy and calvarial bone grafting for dental implants. Rev Stomatol Chir Maxillofac 2010;111(2):6367. 10. Ilankovan V, Jackson IT. Experience in the use of calvarian bone grafts in orbital oor reconstruction. Br J Oral Maxillofac Surg 1992;30(2):92 96. 11. Zunz E, Blanc O, Leibovitch I. Traumatic orbital oor fractures: repair with autogenous bone grafts in a tertiary trauma center. J Oral Maxillofac Surg 2012;70(3):584592. 12. Penfold CN, Lang D, Evans BT. The management of orbital roof fractures. Br J Oral Maxillofac Surg 1992;30(2):97103. 13. Tatum SA, Kellman RM. Cranial bone grafting in maxillofacial trauma and reconstruction. Facial Plast Surg 1998;14(1):117129. 14. Cheney ML, Gliklich RE. The use of calvarial bone in nasal reconstruction. Arch Otolaryngol Head Neck Surg 1995;121(6):643648. 15. Smolka W, Eggensperger N, Kollar A, Iizuka T. Midfacial reconstruction using calvarial split bone grafts. Arch Otolaryngol Head Neck Surg 2005;131(2):131136. 16. Gruss JS, Mackinnon SE, Kassel EE, Cooper PW. The role of primary bone grafting in complex craniomaxillofacial trauma. Plast Reconstr Surg 1985;75(1):1724. 17. Powell NB, Riley RW. Facial contouring with outer-table calvarial bone. A 4-year experience. Arch Otolaryngol Head Neck Surg 1989;115(12):1454 1458. 18. Agrawal A, Dulani R, Mahadevan A, Vagaha SJ, Vagha J, Shankar SK. Primary Ewings sarcoma of the frontal bone with intracranial extension. J Cancer Res Ther 2009;5(3):208209. 19. Agrawal A, Rao KS, Krishnamoorthy B, Shetty RB, Anand M, Jain H. Single stage craniofacial reconstruction for fronto-nasal encephalocele and hypertelorism in an adult. Singapore Med J 2007;48(8):e215e219. 20. Hayward RD. Cranioplasty: dont forget the patients own bone is cheaper than titanium. Br J Neurosurg 1999;13(5):490491.
None
Baylor University Medical Center Proceedings
Volume 26, Number 3
21. Artico M, Ferrante L, Pastore FS, Ramundo EO, Cantarelli D, Scopelliti D, Iannetti G. Bone autografting of the calvaria and craniofacial skeleton: historical background, surgical results in a series of 15 patients, and review of the literature. Surg Neurol 2003;60(1):7179. 22. Aikgz B, Ozcan OE, Erbengi A, Bertan V, Ruacan S, Aikgz HG. Histopathologic and microdensitometric analysis of craniotomy bone aps preserved between abdominal fat and muscle. Surg Neurol 1986;26(6):557561. 23. Simpson D, Robson A. Recurrent subarachnoid bleeding in association with dural substitute. Report of three cases. J Neurosurg 1984;60(2):408409. 24. Earley MJ, Green MF, Milling MA. A critical appraisal of the use of free aps in primary reconstruction of combined scalp and calvarial cancer defects. Br J Plast Surg 1990;43(3):283289.
25. Lin SJ, Hanasono MM, Skoracki RJ. Scalp and calvarial reconstruction. Semin Plast Surg 2008;22(4):281293. 26. Hunter D, Baker S, Sobol SM. Split calvarial grafts in maxillofacial reconstruction. Otolaryngol Head Neck Surg 1990;102(4):345350. 27. Frodel JL. Calvarial bone graft harvest in children. Otolaryngol Head Neck Surg 1999;121(1):7881. 28. Brusati R, Biglioli F, Mortini P, Raaini M, Goisis M. Reconstruction of the orbital walls in surgery of the skull base for benign neoplasms. Int J Oral Maxillofac Surg 2000;29(5):325330. 29. DeLuca L, Raszewski R, Tresser N, Guyuron B. The fate of preserved autogenous bone graft. Plast Reconstr Surg 1997;99(5):13241328.
July 2013
Application of cranial bone grafts for reconstruction of maxillofacial deformities
255
You might also like
- Greek and Latin Root Words MasterDocument7 pagesGreek and Latin Root Words Masterdoug_hewinsNo ratings yet
- Diagnosis and Treatment of Worker-Related Musculoskeletal Disorders of The Upper Extremity OmbroDocument705 pagesDiagnosis and Treatment of Worker-Related Musculoskeletal Disorders of The Upper Extremity OmbroDouglas GarciaNo ratings yet
- Three-Dimensional Vertical Alveolar Ridge Augmentation in The Posterior Maxilla: A 10-Year Clinical StudyDocument10 pagesThree-Dimensional Vertical Alveolar Ridge Augmentation in The Posterior Maxilla: A 10-Year Clinical StudyFabian Sanabria100% (1)
- CT Scanning Techniques and ApplicationsDocument358 pagesCT Scanning Techniques and Applicationsbalab2311No ratings yet
- Mandibular Bone Block Harvesting From The Retromolar Region: A 10-Year Prospective Clinical StudyDocument10 pagesMandibular Bone Block Harvesting From The Retromolar Region: A 10-Year Prospective Clinical StudyFerenc NagyNo ratings yet
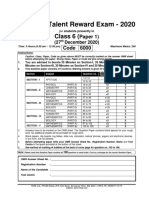
- Fiitjee: Talent Reward Exam - 2020Document25 pagesFiitjee: Talent Reward Exam - 2020Imtesalur Rahman100% (1)
- Anesthesia Consent FormDocument2 pagesAnesthesia Consent Formbalab2311No ratings yet
- Disability Book ReflectionDocument7 pagesDisability Book ReflectionLauren HolcombNo ratings yet
- PPM Informed Consent in Anesthesia WITH FORMSDocument10 pagesPPM Informed Consent in Anesthesia WITH FORMSbalab2311No ratings yet
- Drug Study NursingDocument27 pagesDrug Study Nursingbilliam123No ratings yet
- Zygomatic Implants PDFDocument18 pagesZygomatic Implants PDFgirl33No ratings yet
- Aps 39 345Document9 pagesAps 39 345isabelNo ratings yet
- Midfacial Reconstruction Using Calvarial Split Bone GraftsDocument6 pagesMidfacial Reconstruction Using Calvarial Split Bone Graftsbalab2311No ratings yet
- Cortical Mandibular Bone Blocks Grafts and Piezoelectric Surgery in Complex Anterior Maxillary Alveolar Defects A Case Report and Literature ReviewDocument6 pagesCortical Mandibular Bone Blocks Grafts and Piezoelectric Surgery in Complex Anterior Maxillary Alveolar Defects A Case Report and Literature ReviewAthenaeum Scientific PublishersNo ratings yet
- Brief Resume of Intended WorkDocument7 pagesBrief Resume of Intended WorkNavin ChandarNo ratings yet
- Microsaw and Piezosurgery in Harvesting Mandibular Bone Blocks From The Retromolar Region: A Randomized Split-Mouth Prospective Clinical TrialDocument8 pagesMicrosaw and Piezosurgery in Harvesting Mandibular Bone Blocks From The Retromolar Region: A Randomized Split-Mouth Prospective Clinical TrialdivyaNo ratings yet
- Novel Surgical Technique For Clavicle Graft HarvestDocument5 pagesNovel Surgical Technique For Clavicle Graft Harvestsanchaita kohliNo ratings yet
- Ijcem 0001148Document10 pagesIjcem 0001148Сава БојићNo ratings yet
- MandibulaDocument4 pagesMandibulaMohamed MukhrizNo ratings yet
- Double Barrel Fibula FlapDocument9 pagesDouble Barrel Fibula FlapAlvaro RivCalleNo ratings yet
- Jips 15 131Document5 pagesJips 15 131Nadeem khanNo ratings yet
- Ma 2021Document6 pagesMa 2021bigben9262No ratings yet
- Fotos OclusalesDocument6 pagesFotos OclusalesMarco Antonio García LunaNo ratings yet
- International Journal of Health Sciences and ResearchDocument6 pagesInternational Journal of Health Sciences and ResearchDentist HereNo ratings yet
- Osteoplastic Reconstruction of Severely Resorbed Maxilla by Stack Plasty: Combining Sinus Augmentation With Lateral and Vertical Onlay Bone GraftingDocument5 pagesOsteoplastic Reconstruction of Severely Resorbed Maxilla by Stack Plasty: Combining Sinus Augmentation With Lateral and Vertical Onlay Bone GraftingAnonymous Qt31LLO1lNo ratings yet
- Cleft PalateDocument4 pagesCleft PalateShoaib A. KaziNo ratings yet
- Onlay Bone Graft Augmentation For Refined Correction of Coronal SynostosisDocument9 pagesOnlay Bone Graft Augmentation For Refined Correction of Coronal Synostosisbalab2311No ratings yet
- Cantilever Bone Graft Nose RestorationDocument5 pagesCantilever Bone Graft Nose RestorationMENGANO8593No ratings yet
- Materials: A Modified Ridge Splitting Technique Using Autogenous Bone Blocks-A Case SeriesDocument10 pagesMaterials: A Modified Ridge Splitting Technique Using Autogenous Bone Blocks-A Case SeriesLouis HutahaeanNo ratings yet
- Pi Is 1010518215004084Document8 pagesPi Is 1010518215004084Ceza CezaaNo ratings yet
- Mandibular Reconstruction With Lateral Tibial Bone Graft: An Excellent Option For Oral and Maxillofacial SurgeryDocument7 pagesMandibular Reconstruction With Lateral Tibial Bone Graft: An Excellent Option For Oral and Maxillofacial SurgeryDwifitri MaretaNo ratings yet
- Catastrophic Talar Bone Loss From High Velocity Trauma Treated With Structural Tricorticate Fibula Autograft Compression Frame and Midfoot Distraction ArthroplastyDocument9 pagesCatastrophic Talar Bone Loss From High Velocity Trauma Treated With Structural Tricorticate Fibula Autograft Compression Frame and Midfoot Distraction ArthroplastyAthenaeum Scientific PublishersNo ratings yet
- DF W ReconDocument11 pagesDF W ReconPraveen RavishankaranNo ratings yet
- Algun DiaDocument6 pagesAlgun DiaMarco Antonio García LunaNo ratings yet
- Fuchs 2005Document5 pagesFuchs 2005BudhiNo ratings yet
- Strategies in Reconstruction of The Atrophic MaxillaDocument19 pagesStrategies in Reconstruction of The Atrophic MaxillaEmil CorreaNo ratings yet
- Free Flaps MaxillaDocument7 pagesFree Flaps MaxillaFahad QiamNo ratings yet
- Article 004Document14 pagesArticle 004MedstudNo ratings yet
- Clinical Study: A Liquid Membrane As A Barrier Membrane For Guided Bone RegenerationDocument6 pagesClinical Study: A Liquid Membrane As A Barrier Membrane For Guided Bone RegenerationStanislav ȘuiuNo ratings yet
- Ramus Onlay Bone Graft For Maxillary Alveolar Ridge Augmentation-A Case ReportDocument9 pagesRamus Onlay Bone Graft For Maxillary Alveolar Ridge Augmentation-A Case ReportIJAR JOURNALNo ratings yet
- He 2019Document10 pagesHe 2019Rashif AkmalNo ratings yet
- 37886153Document22 pages37886153Zilbran BerontaxNo ratings yet
- BibliographyDocument6 pagesBibliographysuryaNo ratings yet
- Osteochondral Multiple Autograft Transfer (OMAT) For The Treatment of Cartilage Defects in The Knee JointDocument4 pagesOsteochondral Multiple Autograft Transfer (OMAT) For The Treatment of Cartilage Defects in The Knee JointAnil SoodNo ratings yet
- Distraction Osteogenesis EbookDocument27 pagesDistraction Osteogenesis EbookSundeep SharmaNo ratings yet
- Tranmucosal FixationDocument4 pagesTranmucosal Fixationlippincott2011No ratings yet
- Non-Vascularized Auto Bone Grafting in Segmental Defect of Mandible in Treatment of Benign TumorDocument5 pagesNon-Vascularized Auto Bone Grafting in Segmental Defect of Mandible in Treatment of Benign TumorRajan KarmakarNo ratings yet
- Cantarella2018 DisyunciónDocument9 pagesCantarella2018 DisyunciónFernando Ruiz BorsiniNo ratings yet
- Mandibular Reconstruction With Tissue EngineeringDocument5 pagesMandibular Reconstruction With Tissue EngineeringtamisatnamNo ratings yet
- Articulo ProtodonciaDocument5 pagesArticulo ProtodonciaMilton David Rios SerratoNo ratings yet
- Biomed 2Document5 pagesBiomed 2Olesea CutitaruNo ratings yet
- Chitsazi 2017 AAADocument6 pagesChitsazi 2017 AAAJavi ChavezNo ratings yet
- Evaluation of Marginal Alveolar Bone in The Anterior Mandible With Pretreatment and Posttreatment Computed Tomography in Nonextraction PatientsDocument10 pagesEvaluation of Marginal Alveolar Bone in The Anterior Mandible With Pretreatment and Posttreatment Computed Tomography in Nonextraction PatientsSoe San KyawNo ratings yet
- Costochondral GraftsDocument5 pagesCostochondral Graftssmartdoc36100% (1)
- Congenital Pseudoarthrosis of The Clavicle A Rare CaseDocument5 pagesCongenital Pseudoarthrosis of The Clavicle A Rare CaseInternational Medical PublisherNo ratings yet
- Alveolar Ridge Augmentation by Distraction OsteogenesisDocument8 pagesAlveolar Ridge Augmentation by Distraction OsteogenesisCarlos Santiago VivenzaNo ratings yet
- Continuing Education 1: Horizontal Alveolar Ridge Augmentation: The Importance of Space MaintenanceDocument11 pagesContinuing Education 1: Horizontal Alveolar Ridge Augmentation: The Importance of Space MaintenanceJuan Jose Sosa BerganzaNo ratings yet
- Fuhrmann 2002Document6 pagesFuhrmann 2002DentalErNo ratings yet
- Case Report: Rehabilitation of Posterior Maxilla With Zygomatic and Dental Implant After Tumor Resection: A Case ReportDocument6 pagesCase Report: Rehabilitation of Posterior Maxilla With Zygomatic and Dental Implant After Tumor Resection: A Case ReportManjulika TysgiNo ratings yet
- Artigo Bad SplitDocument6 pagesArtigo Bad SplitCarolinaNo ratings yet
- Schlund 2019Document3 pagesSchlund 2019mesescuNo ratings yet
- Repair Processes of Experimental Root Fractures in Rat Molars Examined by Histopathological Techniques and 3D Micro-CT ImagingDocument8 pagesRepair Processes of Experimental Root Fractures in Rat Molars Examined by Histopathological Techniques and 3D Micro-CT ImagingAhmad Ulil AlbabNo ratings yet
- Anehosur Et Al 2020 Concepts and Challenges in The Surgical Management of Edentulous Mandible Fractures A Case SeriesDocument7 pagesAnehosur Et Al 2020 Concepts and Challenges in The Surgical Management of Edentulous Mandible Fractures A Case SeriesHenry Adhy SantosoNo ratings yet
- Raffaini Bioss CollagenDocument7 pagesRaffaini Bioss CollagenÂngelo Rosso LlantadaNo ratings yet
- Recurrent Giant Cell Tumour of Distal Tibia: Case Report and Review of The LiteratureDocument4 pagesRecurrent Giant Cell Tumour of Distal Tibia: Case Report and Review of The LiteratureAMBS ABMS JMAANo ratings yet
- Huang 2018Document6 pagesHuang 2018zj7n2rhtb4No ratings yet
- ArtículoDocument8 pagesArtículoCatalina PetrelNo ratings yet
- Orthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFrom EverandOrthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFederico BrugnamiNo ratings yet
- Building Blocks Issue 7 26 1Document10 pagesBuilding Blocks Issue 7 26 1balab2311No ratings yet
- Azhaar TopicDocument4 pagesAzhaar Topicbalab2311No ratings yet
- IndianJAnaesth542116-1332734 034207Document5 pagesIndianJAnaesth542116-1332734 034207balab2311No ratings yet
- Craniosynostosis & Craniofacial Surgery: A Parent's GuideDocument16 pagesCraniosynostosis & Craniofacial Surgery: A Parent's Guidebalab2311No ratings yet
- Super StuccoDocument2 pagesSuper Stuccobalab2311No ratings yet
- Particularities in The Surgical Technique of Calvaria GraftDocument6 pagesParticularities in The Surgical Technique of Calvaria Graftbalab2311No ratings yet
- Onlay Bone Graft Augmentation For Refined Correction of Coronal SynostosisDocument9 pagesOnlay Bone Graft Augmentation For Refined Correction of Coronal Synostosisbalab2311No ratings yet
- Brushbond TI Flexicoat PDFDocument3 pagesBrushbond TI Flexicoat PDFbalab2311No ratings yet
- Crackers Price ListDocument4 pagesCrackers Price Listbalab2311No ratings yet
- A Short History of The Thyroid Gland PDFDocument4 pagesA Short History of The Thyroid Gland PDFsmartjohnsmith10No ratings yet
- Lecture On PHYSIOLOGY of Cerebellum by Dr. RoomiDocument42 pagesLecture On PHYSIOLOGY of Cerebellum by Dr. RoomiMudassar Roomi100% (2)
- Spec Hells Handlers MC Florida Chapter Book 2 Lilly Atlas All ChapterDocument67 pagesSpec Hells Handlers MC Florida Chapter Book 2 Lilly Atlas All Chapteralonzo.cramer529100% (4)
- Oral Mucosal Ulceration - A Clinician's Guide To Diagnosis and TreatmentDocument9 pagesOral Mucosal Ulceration - A Clinician's Guide To Diagnosis and TreatmentAnonymous pvuOXZNo ratings yet
- Secdocument - 61download Breast Pathology 2Nd Edition David J Dabbs Full ChapterDocument67 pagesSecdocument - 61download Breast Pathology 2Nd Edition David J Dabbs Full Chapterjulia.swanson282100% (5)
- Is Diet Important in Bipolar Disorder?Document13 pagesIs Diet Important in Bipolar Disorder?Giovane de PaulaNo ratings yet
- Costipation CorrectionDocument21 pagesCostipation CorrectionTim CostaNo ratings yet
- FJVKDocument2 pagesFJVKMutia RahayuNo ratings yet
- A Comparison Study of Whole Genome Sequencing (WGS) in Clinical SettingDocument3 pagesA Comparison Study of Whole Genome Sequencing (WGS) in Clinical SettingSteven4654No ratings yet
- Atlas of The Global Egg IndustryDocument36 pagesAtlas of The Global Egg IndustryJNo ratings yet
- 06 Msds Ripoxy R-802 ExDocument9 pages06 Msds Ripoxy R-802 ExAnto Maryadi100% (1)
- Module Opthalmology Corneal Ulcer: Group 7 Wulan-Fadzely-Arif Amri-Safuan Arif-Nadiah-Insyira-Fatimah-Andi AbsharinaDocument19 pagesModule Opthalmology Corneal Ulcer: Group 7 Wulan-Fadzely-Arif Amri-Safuan Arif-Nadiah-Insyira-Fatimah-Andi Absharinaarifamri92No ratings yet
- PG Syllabus - PLANT PATHOLOGYDocument18 pagesPG Syllabus - PLANT PATHOLOGYAnitharaj AlaguvelNo ratings yet
- I. Choose The Correct Answer: Do at ClassDocument9 pagesI. Choose The Correct Answer: Do at ClassNishali SamNo ratings yet
- Jurnal DematitisDocument11 pagesJurnal DematitisRana NurfadillahNo ratings yet
- Multi Focal Choroid It Is FinalDocument23 pagesMulti Focal Choroid It Is FinalDiaconescu AlexNo ratings yet
- Dengue QuizDocument10 pagesDengue QuizAfifah SelamatNo ratings yet
- Bams 1st Year Kriya Sharir Pranavaha Srota 02 05 2020Document12 pagesBams 1st Year Kriya Sharir Pranavaha Srota 02 05 2020Shravan KumarNo ratings yet
- Abdominal Organ - Vermiform AppendixDocument3 pagesAbdominal Organ - Vermiform AppendixayooniaNo ratings yet
- Patricia Nicole Y.Cruz 2BSA-4 Module 2: Lesson 1-Assignment #1Document4 pagesPatricia Nicole Y.Cruz 2BSA-4 Module 2: Lesson 1-Assignment #1Patricia CruzNo ratings yet
- FCR Capsula Xl2 Brochure 01Document3 pagesFCR Capsula Xl2 Brochure 01Zhandra50% (2)
- At The Crossroads of Lipid Metabolism and InflammationDocument7 pagesAt The Crossroads of Lipid Metabolism and InflammationChow Sing SingNo ratings yet
- Dwnload Full Nutrition Exercise and Behavior An Integrated Approach To Weight Management 3rd Edition Summerfield Solutions Manual PDFDocument36 pagesDwnload Full Nutrition Exercise and Behavior An Integrated Approach To Weight Management 3rd Edition Summerfield Solutions Manual PDFbokcardera100% (12)
- Department of Anthropology Plagues and People (ANTH 2240, A01/CRN18650)Document13 pagesDepartment of Anthropology Plagues and People (ANTH 2240, A01/CRN18650)jakejnfhfbNo ratings yet
- Dgca Module 09 Part 01Document11 pagesDgca Module 09 Part 01RAVI SHUKLANo ratings yet