Professional Documents
Culture Documents
Pediatric Sample Exam
Uploaded by
Rho Vince Caño MalagueñoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pediatric Sample Exam
Uploaded by
Rho Vince Caño MalagueñoCopyright:
Available Formats
1. Which of the following would be inappropriate when administering chemotherapy to a child? a.
Monitoring the child for both general and specific adverse effects b. Observing the child for 10 minutes to note for signs of anaphylaxis c. Administering medication through a free-flowing intravenous line d. Assessing for signs of infusion infiltration and irritation 2. Which of the following is the best method for performing a physical examination on a toddler a. From head to toe b. Distally to proximally c. From abdomen to toes, the to head d. From least to most intrusive 3. Which of the following organisms is responsible for the development of rheumatic fever? a. Streptococcal pneumonia b. Haemophilus influenza c. Group A -hemolytic streptococcus d. Staphylococcus aureus 4. Which of the following is most likely associated with a cerebrovascular accident (CVA) resulting from congenital heart disease? a. Polycythemia b. Cardiomyopathy c. Endocarditis d. Low blood pressure 5. How does the nurse appropriately administer mycostatin suspension in an infant? a. Have the infant drink water, and then administer mycostatin in a syringe b. Place mycostatin on the nipple of the feeding bottle and have the infant suck it c. Mix mycostatin with formula d. Swab mycostatin on the affected areas 6. A mother tells the nurse that she is very worried because her 2-year old child does not finish his meals. What should the nurse advise the mother? a. make the child seat with the family in the dining room until he finishes his meal b. provide quiet environment for the child before meals c. do not give snacks to the child before meals d. put the child on a chair and feed him 7. The nurse is assessing a newborn who had undergone vaginal delivery. Which of the following findings is least likely to be observed in a normal newborn? a. uneven head shape b. respirations are irregular, abdominal, 30-60 bpm c. (+) moro reflex d. heart rate is 80 bpm 8. Which of the following situations increase risk of lead poisoning in children? a. playing in the park with heavy traffic and with many vehicles passing by b. playing sand in the park c. playing plastic balls with other children d. playing with stuffed toys at home 9. An inborn error of metabolism that causes premature destruction of RBC? a. G6PD
b. Hemocystinuria c. Phenylketonuria d. Celiac Disease 10. Which of the following blood study results would the nurse expect as most likely when caring for the child with iron deficiency anemia? a. Increased hemoglobin b. Normal hematocrit c. Decreased mean corpuscular volume (MCV) d. Normal total iron-binding capacity (TIBC) 11. The nurse answers a call bell and finds a frightened mother whose child, the patient, is having a seizure. Which of these actions should the nurse take? a. The nurse should insert a padded tongue blade in the patients mouth to prevent the child from swallowing or choking on his tongue. b. The nurse should help the mother restrain the child to prevent him from injuring himself. c. The nurse should call the operator to page for seizure assistance. d. The nurse should clear the area and position the client safely. 12. At the community center, the nurse leads an adolescent health information group, which often expands into other areas of discussion. She knows that these youths are trying to find out who they are, and discussion often focuses on which directions they want to take in school and life, as well as peer relationships. According to Erikson, this stage is known as: a. identity vs. role confusion. b. adolescent rebellion. c. career experimentation. d. relationship testing 13. The nurse is assessing a 9-month-old boy for a well-baby check up. Which of the following observations would be of most concern? a. The baby cannot say mama when he wants his mother. b. The mother has not given him finger foods. c. The child does not sit unsupported. d. The baby cries whenever the mother goes out. 14. Cheska, the mother of an 11-month-old girl, KC, is in the clinic for her daughters immunizations. She expresses concern to the nurse that Shannon cannot yet walk. The nurse correctly replies that, according to the Denver Developmental Screen, the median age for walking is: a. 12 months. b. 15 months. c. 10 months. d. 14 months. 15. Sally Kent., age 13, has had a lumbar puncture to examine the CSF to determine if bacterial infection exists. The best position to keep her in after the procedure is: a. prone for two hours to prevent aspiration, should she vomit. b. semi-fowlers so she can watch TV for five hours and be entertained. c. supine for several hours, to prevent headache. d. on her right sides to encourage return of CSF
16. Bucks traction with a 10 lb. weight is securing a patients leg while she is waiting for surgery to repair a hip fracture. It is important to check circulation- sensation-movement: a. every shift. b. every day. c. every 4 hours. d. every 15 minutes. 17. Carol Smith is using bronchodilators for asthma. The side effects of these drugs that you need to monitor this patient for include: a. tachycardia, nausea, vomiting, heart palpitations, inability to sleep, restlessness, and seizures. b. tachycardia, headache, dyspnea, temp . 101 F, and wheezing. c. blurred vision, tachycardia, hypertension, headache, insomnia, and oliguria. d. restlessness, insomnia, blurred vision, hypertension, chest pain, and muscle weakness. 18. The adolescent patient has symptoms of meningitis: nuchal rigidity, fever, vomiting, and lethargy. The nurse knows to prepare for the following test: a. blood culture. b. throat and ear culture. c. CAT scan. d. lumbar puncture. 19. The nurse is drawing blood from the diabetic patient for a glycosolated hemoglobin test. She explains to the woman that the test is used to determine: a. the highest glucose level in the past week. b. her insulin level. c. glucose levels over the past several months. d. her usual fasting glucose level. 20. The twelve-year-old boy has fractured his arm because of a fall from his bike. After the injury has been casted, the nurse knows it is most important to perform all of the following assessments on the area distal to the injury except: a. capillary refill. b. radial and ulnar pulse. c. finger movement d. skin integrity
1. B. When administering chemotherapy, the nurse should observe for an anaphylactic reaction for 20 minutes and stop the medication if one is suspected. Chemotherapy is associated with both general and specific adverse effects, therefore close monitoring for them is important. 2. D. When examining a toddler or any small child, the best way to perform the exam is from least to most intrusive. Starting at the head or abdomen is intrusive and should be avoided. Proceeding from distal to proximal is inappropriate at any age. 3. C. Rheumatic fever results as a delayed reaction to inadequately treated group A -hemolytic streptococcal infection.
4. A. The child with congenital heart disease develops polycythemia resulting from an inadequate mechanism to compensate for decreased oxygen saturation 5. D. Mycostatin suspension is given as swab. Never mix medications with food and formula. 6. C. If the child is hungry he/she more likely would finish his meals. Therefore, the mother should be advised not to give snacks to the child. The child is a busy toddler. He/she will not able to keep still for a long time. 7. D. Normal heart rate of the newborn is 120 to 160 bpm. Choices A, B, and C are normal assessment findings (uneven head shape is molding). 8. A. Lead poisoning may be caused by inhalation of dusk and smoke from leaded gas. It may also be caused by lead-based paint, soil, water (especially from plumbings of old houses). 9. A. Glucose-6-phosphate dehydrogenase deficiency (G6PD) is an X-linked recessive hereditary disease characterised by abnormally low levels of glucose-6-phosphate dehydrogenase (abbreviated G6PD or G6PDH), a metabolic enzyme involved in the pentose phosphate pathway, especially important in red blood cell metabolism. 10. C. For the child with iron deficiency anemia, the blood study results most likely would reveal decreased mean corpuscular volume (MCV) which demonstrates microcytic anemia, decreased hemoglobin, decreased hematocrit and elevated total iron binding capacity. 11. D. The primary role of the nurse when a patient has a seizure is to protect the patient from harming him or herself. 12. A. During this period, which lasts up to the age of 18-21 years, the individual develops a sense of self. Peers have a major big influence over behavior, and the major decision is to determine a vocational goal. 13. C. Over 90% percent of babies can sit unsupported by nine months. Most babies cannot say mama in the sense that it refers to their mother at this time. 14. A. By 12 months, 50 percent of children can walk well. 15. C. Lying flat keeps the patient from having a spinal headache. Increasing the fluid intake will assist in replenishing the lost fluid during this time. 16. C. The patient can lose vascular status without the nurse being aware if left for more than 4 hours, yet checks should not be so frequent that the patient becomes anxious. Vital signs are generally checked q4h, at which time the CSM checks can easily be performed. 17. A. Bronchodilators can produce the side effects listed in answer choice (A) for a short time after the patient begins using them.
18. D. Meningitis is an infection of the meninges, the outer membrane of the brain. Since it is surrounded by cerebrospinal fluid, a lumbar puncture will help to identify the organism involved. 19. C. The glycosolated hemoglobin test measures glucose levels for the previous 3 to 4 months. 20. D. Capillary refill, pulses, and skin temperature and color are indicative of intact circulation and absence of compartment syndrome. Skin integrity is less important.
You might also like
- Pedia 1Document4 pagesPedia 1Aijem Ryan100% (2)
- Blueprints QA Pediatrics For Step 3 1Document59 pagesBlueprints QA Pediatrics For Step 3 1Moataz Trabeh100% (1)
- E1 Fall 20Document10 pagesE1 Fall 20Alexander BarbechoNo ratings yet
- BluePrint 5th QuestionsDocument25 pagesBluePrint 5th QuestionsAbuFreihNo ratings yet
- PEDIADocument15 pagesPEDIAEdith Cabrera Cabigas - Sabalboro0% (1)
- Ped A Internship 1517300917 PDF 2Document13 pagesPed A Internship 1517300917 PDF 2dariasuslowaNo ratings yet
- All Pediatrics 2Document200 pagesAll Pediatrics 2niemand daNo ratings yet
- 4 5839111053702598026Document7 pages4 5839111053702598026خلدون سليمNo ratings yet
- (PAED) End-Posting Examination Questions (R3G1)Document16 pages(PAED) End-Posting Examination Questions (R3G1)loxNo ratings yet
- B33 - Paeds PDFDocument5 pagesB33 - Paeds PDFEthan KhooNo ratings yet
- Transposition of The Great ArteriesDocument23 pagesTransposition of The Great Arterieswaseem mohammedNo ratings yet
- MCQ5FULL (Watermarked) PDFDocument164 pagesMCQ5FULL (Watermarked) PDFAbuMajedNo ratings yet
- Non Non-Surgical Selection August 2021Document19 pagesNon Non-Surgical Selection August 2021Majd HosamNo ratings yet
- PEDIA DOCUMENT REVIEWDocument157 pagesPEDIA DOCUMENT REVIEWBea Y. Bas-ong100% (1)
- Peds MCQDocument395 pagesPeds MCQSmart NemoNo ratings yet
- Part 1-2023 (1st Version)Document19 pagesPart 1-2023 (1st Version)Waleed SofiNo ratings yet
- Soal MCQDocument39 pagesSoal MCQRonald Allan Valle SantosNo ratings yet
- PEDIA QUIZ CARDIORESPI and NEPHRODocument5 pagesPEDIA QUIZ CARDIORESPI and NEPHROAlessa Mikkah BaltazarNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Pediatrics Objective Type Questions and Answers - All Medical Questions and AnswersDocument4 pagesPediatrics Objective Type Questions and Answers - All Medical Questions and AnswersAbdul Ghaffar AbdullahNo ratings yet
- Aiims Neet-Pg 2017 Pediatrics Mcqs 91-100Document4 pagesAiims Neet-Pg 2017 Pediatrics Mcqs 91-100DrHassan Ahmed Shaikh100% (1)
- Name: - Date: - Date of Rotation: - Score: - Pediatrics Shifting ExamDocument5 pagesName: - Date: - Date of Rotation: - Score: - Pediatrics Shifting ExamKristine Seredrica100% (1)
- MCQ GitDocument15 pagesMCQ Gitpriya009100% (1)
- 2005 FRACP Written Examination Paediatrics & ChildDocument30 pages2005 FRACP Written Examination Paediatrics & ChildMedicEdNo ratings yet
- Pediatric Homework 2Document16 pagesPediatric Homework 2turner_marsha0% (1)
- Paeds MCQs Part 1Document34 pagesPaeds MCQs Part 1SsNo ratings yet
- MCQ4FULLDocument139 pagesMCQ4FULLBruta Brutal100% (2)
- Pedes McqsDocument16 pagesPedes McqsSyeda Aroosa Abbas Naqvi100% (1)
- Filename: AMC PEDIATRICS 2005 To 2009 PDFDocument38 pagesFilename: AMC PEDIATRICS 2005 To 2009 PDFZahid QamarNo ratings yet
- Bawasig Pediatric ExamDocument20 pagesBawasig Pediatric Examخلدون سليمNo ratings yet
- اذكرونا بدعوة Pediatric Theory Final ExamDocument23 pagesاذكرونا بدعوة Pediatric Theory Final ExamSarwar Sarkawt100% (1)
- Paediatrics MCQsDocument5 pagesPaediatrics MCQsbalarajuuk100% (1)
- Pediatrics Case Studies and Management GuidelinesDocument103 pagesPediatrics Case Studies and Management GuidelinesJulius Matthew LuzanaNo ratings yet
- Paediatric Question BankDocument27 pagesPaediatric Question BankBashiru SelemaniNo ratings yet
- MCQ Congenital Malformation of The LungsDocument3 pagesMCQ Congenital Malformation of The LungsAmrut Lovesmusic100% (1)
- First Part Exam - Feb 2020Document16 pagesFirst Part Exam - Feb 2020hassan mohamedNo ratings yet
- Musawi 17Document22 pagesMusawi 17Full MarksNo ratings yet
- Pediatric Nursing Exam Review: Growth, Development and Common ConditionsDocument21 pagesPediatric Nursing Exam Review: Growth, Development and Common ConditionsChristianmel JavierNo ratings yet
- 5th Year 112 PediatricsDocument12 pages5th Year 112 PediatricsAmjad A. Amir100% (2)
- Self-Assessment Questions, Group 6Document20 pagesSelf-Assessment Questions, Group 6naveenkovalNo ratings yet
- PEDIATRICSDocument51 pagesPEDIATRICSJoanne BlancoNo ratings yet
- Pediatric G.I Disorders FinalDocument53 pagesPediatric G.I Disorders FinalRashid Hussain0% (1)
- Pediatrics BookDocument53 pagesPediatrics BookMobin Ur Rehman Khan100% (1)
- Pediatrics Problem Solving QsDocument32 pagesPediatrics Problem Solving QsabozinaNo ratings yet
- Newborn MCQDocument58 pagesNewborn MCQعبدالرحمن بشير100% (2)
- Downloadfile 2Document8 pagesDownloadfile 2Michael SilvaNo ratings yet
- BXX - Pediatrics PDocument57 pagesBXX - Pediatrics PJason Steel100% (1)
- MK Paeds BazookaDocument118 pagesMK Paeds BazookaChipasha Bwalya100% (1)
- Pediatric 5th year 2017-محلولDocument27 pagesPediatric 5th year 2017-محلولmotasem alsharifNo ratings yet
- Growth and Development QuestionsDocument12 pagesGrowth and Development QuestionsPamela Castillo100% (1)
- 2016.07.18 Pediatrics PREVENTIVE PEDIATRIC HEALTH CARE PDFDocument115 pages2016.07.18 Pediatrics PREVENTIVE PEDIATRIC HEALTH CARE PDFRjDNo ratings yet
- Khalid Alfaki PedDocument21 pagesKhalid Alfaki PedAli HusseinNo ratings yet
- Pedia+smiley Block7Document7 pagesPedia+smiley Block7tej0331No ratings yet
- Integrated Management of Childhood Illness AssessmentDocument2 pagesIntegrated Management of Childhood Illness AssessmentRamon Carlo AlmiranezNo ratings yet
- MCQ3FULLDocument153 pagesMCQ3FULLtheintrov100% (4)
- Mock Exam 5 23 21Document4 pagesMock Exam 5 23 21Anne Lorraine BringasNo ratings yet
- Pedia FinalDocument37 pagesPedia FinalVince CabahugNo ratings yet
- PRC - ICF - Compilations 2009-2016Document18 pagesPRC - ICF - Compilations 2009-2016Jonas Marvin AnaqueNo ratings yet
- QuestionsDocument9 pagesQuestionsDennis Dane AngelesNo ratings yet
- ASTHMA TreatmentDocument27 pagesASTHMA TreatmentRho Vince Caño Malagueño0% (1)
- QuestDocument1 pageQuestRho Vince Caño MalagueñoNo ratings yet
- Operating Room StandardsDocument28 pagesOperating Room StandardsRho Vince Caño MalagueñoNo ratings yet
- Imci NTG 2016 New RV - ScribdDocument32 pagesImci NTG 2016 New RV - ScribdRho Vince Caño MalagueñoNo ratings yet
- Cranial Epidural AbscessDocument31 pagesCranial Epidural AbscessRho Vince Caño MalagueñoNo ratings yet
- Imci NTG 2016 New RV - Student's OpyDocument33 pagesImci NTG 2016 New RV - Student's OpyRho Vince Caño MalagueñoNo ratings yet
- Electron Transport ChainDocument25 pagesElectron Transport ChainRho Vince Caño MalagueñoNo ratings yet
- TonsillectomyDocument27 pagesTonsillectomyRho Vince Caño MalagueñoNo ratings yet
- The Bradyarrhythmias: Disorders of The Atrioventricular NodeDocument34 pagesThe Bradyarrhythmias: Disorders of The Atrioventricular NodeRho Vince Caño MalagueñoNo ratings yet
- Republic of the Philippines passes anti-sexual harassment lawDocument3 pagesRepublic of the Philippines passes anti-sexual harassment lawErika Jane Madriago PurificacionNo ratings yet
- Neurologic Nursing ReviewDocument2 pagesNeurologic Nursing ReviewRho Vince Caño MalagueñoNo ratings yet
- ThalamusDocument30 pagesThalamusRho Vince Caño Malagueño100% (1)
- 10 Medicinal Plants Approved by The Department of HealthDocument5 pages10 Medicinal Plants Approved by The Department of HealthAnilour MalaguenoNo ratings yet
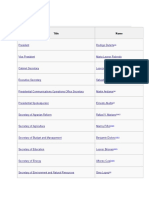
- Cabinet: Title NameDocument5 pagesCabinet: Title NameRho Vince Caño MalagueñoNo ratings yet
- Human SexualityDocument45 pagesHuman SexualityRho Vince Caño MalagueñoNo ratings yet
- Chapter 1Document1 pageChapter 1Rho Vince MalagueñoNo ratings yet
- Post Partum CareDocument23 pagesPost Partum CareRho Vince Caño MalagueñoNo ratings yet
- Conceptual FrameworkDocument1 pageConceptual FrameworkRho Vince MalagueñoNo ratings yet
- Post Partum CareDocument23 pagesPost Partum CareRho Vince Caño MalagueñoNo ratings yet
- Labor and Delivery Signs and StagesDocument17 pagesLabor and Delivery Signs and StagesRho Vince Caño MalagueñoNo ratings yet
- Primary Health Care Post Test QuestionsDocument9 pagesPrimary Health Care Post Test QuestionsRho Vince Caño MalagueñoNo ratings yet
- Buntis Congress - Prenatal CareDocument26 pagesBuntis Congress - Prenatal CareRho Vince Caño MalagueñoNo ratings yet
- Subj - and Verb AgreementDocument2 pagesSubj - and Verb AgreementRho Vince Caño MalagueñoNo ratings yet
- Reading As A Physiological ProcessDocument2 pagesReading As A Physiological ProcessRho Vince Caño Malagueño89% (9)
- Schwann CellsDocument3 pagesSchwann CellsRho Vince Caño MalagueñoNo ratings yet
- Arrowroot Powder vs. Cornstarch: Why Arrowroot Powder Is A Better ChoiceDocument53 pagesArrowroot Powder vs. Cornstarch: Why Arrowroot Powder Is A Better ChoiceRho Vince Caño MalagueñoNo ratings yet
- Darwinz Table of Specification in English IVDocument4 pagesDarwinz Table of Specification in English IVRho Vince Caño MalagueñoNo ratings yet
- SAT II Physics Formula SheetDocument10 pagesSAT II Physics Formula Sheetalex100% (1)
- Arrow of GodDocument24 pagesArrow of GodRho Vince Caño Malagueño100% (1)
- Renal Colic and Joint DeformitiesDocument19 pagesRenal Colic and Joint DeformitiesAhmad Syahmi YZ100% (1)
- Nebosh: Management of Health and Safety Unit Ig1Document5 pagesNebosh: Management of Health and Safety Unit Ig1Muhammad Talha0% (1)
- Material Safety Data Sheet: Section 01: Product and Company IdentificationDocument9 pagesMaterial Safety Data Sheet: Section 01: Product and Company IdentificationMaya SeptianaNo ratings yet
- Hashimoto ThyroiditisDocument6 pagesHashimoto Thyroiditismananginsiang100% (1)
- Maxicare Plus BenefitsDocument10 pagesMaxicare Plus BenefitsMithiVillarmeaNo ratings yet
- 6610 Assignment 4Document19 pages6610 Assignment 4gyanendraNo ratings yet
- LRT (Light Rapid Transit) Pulo Gadung Accident Report 1. Description 1.1 Chronology of AccidentDocument4 pagesLRT (Light Rapid Transit) Pulo Gadung Accident Report 1. Description 1.1 Chronology of AccidentYogi GuntaraNo ratings yet
- Health, Safety and Environmental Policies and Procedures ManualDocument64 pagesHealth, Safety and Environmental Policies and Procedures ManualBenaoumeur FertasNo ratings yet
- Safety Officer Resume - 6+ Years HSE ExperienceDocument3 pagesSafety Officer Resume - 6+ Years HSE ExperienceMuhammad Zeeshan Ahmed100% (1)
- Surgical Nursing Brunner 2016Document74 pagesSurgical Nursing Brunner 2016Faisol Kabir100% (1)
- Epidemiology Terminology GuideDocument5 pagesEpidemiology Terminology GuideBiratNagar100% (2)
- Progestin Only ContraceptionDocument4 pagesProgestin Only ContraceptionTareq SawanNo ratings yet
- Gastroenterology - Pancreatitis PDFDocument2 pagesGastroenterology - Pancreatitis PDFMonica J Ortiz PereiraNo ratings yet
- Monitoring Tool For Sped ADocument3 pagesMonitoring Tool For Sped ARica Claire SerqueñaNo ratings yet
- Chitoglucan New OverviewDocument6 pagesChitoglucan New OverviewmjmorcelliNo ratings yet
- Drug StudyDocument3 pagesDrug StudyMelanie Moises JavierNo ratings yet
- Bronchial Asthma & Cardiac AsthmaDocument7 pagesBronchial Asthma & Cardiac AsthmaAbraham Chiu100% (1)
- Practice Questions 1 - YoungDocument12 pagesPractice Questions 1 - Youngejyoung928100% (1)
- Balantidium ColiDocument7 pagesBalantidium ColiOmar GhoneimNo ratings yet
- Case Presentation OF Acute Tonsillitis: Nueva Ecija University of Science andDocument38 pagesCase Presentation OF Acute Tonsillitis: Nueva Ecija University of Science andBeverly DatuNo ratings yet
- Forceps DeliveryDocument22 pagesForceps DeliveryN. Siva100% (1)
- Florian1995, Mental HealthDocument9 pagesFlorian1995, Mental Healthade ubaidahNo ratings yet
- CARDOS NAUSEA FDAR-formatDocument3 pagesCARDOS NAUSEA FDAR-formatGabrielle CardosNo ratings yet
- Maternity and Newborn MedicationDocument34 pagesMaternity and Newborn MedicationNicholas ClaytonNo ratings yet
- METHODS AND STRATEGIES IN TEACHING MAPEH MODULE 1 - BajadoDocument40 pagesMETHODS AND STRATEGIES IN TEACHING MAPEH MODULE 1 - Bajadoacademic coordinatorNo ratings yet
- Merriam-Webster Dictionary: NaturalDocument8 pagesMerriam-Webster Dictionary: NaturalRAJA PAARVAI PoovanathanNo ratings yet
- BP6 15depression PDFDocument75 pagesBP6 15depression PDFada ramosNo ratings yet
- History Taking TemplateDocument6 pagesHistory Taking TemplateNooredin JomaaNo ratings yet
- Epithelioid Hemangioendothelioma of The Superior Vena - 2022 - Archivos de BroncDocument1 pageEpithelioid Hemangioendothelioma of The Superior Vena - 2022 - Archivos de Broncguidance mtisiNo ratings yet
- Basic Malaria Microscopy - Part 1 Learner's Guide, 2nd Edition, WHO, 2010Document87 pagesBasic Malaria Microscopy - Part 1 Learner's Guide, 2nd Edition, WHO, 2010Joey MarcNo ratings yet