Professional Documents
Culture Documents
An Epidemiologic Study of Index and Family Infectious Mononucleosis and Adult Hodgkin'S Disease (HD) : Evidence For A Specific Association With Ebv HD in Young Adults
Uploaded by
Mihailo Majk ŽikićOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
An Epidemiologic Study of Index and Family Infectious Mononucleosis and Adult Hodgkin'S Disease (HD) : Evidence For A Specific Association With Ebv HD in Young Adults
Uploaded by
Mihailo Majk ŽikićCopyright:
Available Formats
Int. J. Cancer: 107, 298 302 (2003) 2003 Wiley-Liss, Inc.
Publication of the International Union Against Cancer
AN EPIDEMIOLOGIC STUDY OF INDEX AND FAMILY INFECTIOUS MONONUCLEOSIS AND ADULT HODGKINS DISEASE (HD): EVIDENCE FOR A SPECIFIC ASSOCIATION WITH EBVVE HD IN YOUNG ADULTS
Freda E. ALEXANDER1*, Davia J. LAWRENCE2, June FREELAND3, Andrew S. KRAJEWSKI4, Brian ANGUS5, G. Malcolm TAYLOR6 and Ruth F. JARRETT3 1 Department of Community Health, Public Health Sciences, University of Edinburgh, Medical School, Teviot Place, Edinburgh, UK 2 Clinical Trials and Statistics Unit, Institute of Cancer Research, Sutton, Surrey, UK 3 Leukaemia Research Fund Virus Centre, Department of Veterinary Pathology, University of Glasgow, Glasgow, UK 4 Department of Pathology, Northampton General Hospital NHS Trust, Northampton, UK 5 Department of Pathology, University of Newcastle on Tyne, UK 6 Immunogenetics Laboratory, University of Manchester, St Marys Hospital, Manchester, UK
Infectious mononucleosis (IM) is an established risk factor for Hodgkins disease (HD). A substantial minority (33%) of cases of HD have Epstein-Barr virus (EBV) DNA within the malignant cells (are EBVve). It is unclear whether risk after IM applies specically to EBVve HD. We report the results of a population-based case-control study of HD in adults (n 408 cases of classical HD, 513 controls) aged 16 74 years; the case series included 113 EBVve and 243 EBV-ve HD. Analyses compared total HD, EBVve HD and EBV-ve HD with the controls and EBVve HD with EBV-ve HD cases using, mainly, logistic regression. Regression analyses were adjusted for gender, age-group and socioeconomic status, and were performed for the whole age range and separately for young (< 35 years) and old adults (> 35 years); formal tests of effect modication by age were included. For the young adults, reported IM in index or relative was strongly and signicantly associated with EBVve HD when compared to controls (odds ratio [OR] 2.94, 95% condence interval [CI]: 1.08 7.98 and OR 5.22, 95% CI: 2.1512.68, respectively). These results may be interpreted as indications that late rst exposure to EBV increases risk of HD, especially in young adults; this applies primarily to EBVve HD. 2003 Wiley-Liss, Inc. Key words: Epstein-Barr virus; Hodgkins disease; epidemiology; risk factor
Abundant epidemiologic evidence supports the hypothesis that Hodgkins disease (HD) aetiology differs for cases diagnosed in the young adult peak and diagnosed in older people (aged 50).1 Under the late host-response model,2 HD in the young adult peak arises as a sequel to relatively late rst infection with a common infectious agenta similar pattern to that seen for infectious mononucleosis (IM) in relation to the Epstein-Barr virus (EBV). Large cohort studies3,4 have demonstrated that HD risk is increased around 3-fold in the followup of subjects with IM compared to the general population. This could indicate that EBV is causally implicated in HD or, alternatively, that IM is a marker of a type of lifestyle that predisposes to late rst exposure to many infectious agents. A direct link seemed probable when EBV viral DNA was identied within the HD tumour cells.5,6 It is now established that EBV is associated with a substantial minority (referred to here as EBVve) of cases of HD, and IARC has recently classied EBV as a probable human carcinogen in relation to HD.7 Subsequent research has indicated the complexity of the association between EBV and HD. For example, the proportion of cases that are EBVve is markedly lower in the young adult peak (16 34 years) than for HD in children or older people.8 Because the late host-response model applies to the young adult peak, this suggests that EBV is not the elusive agent involved in that model, if indeed there is just 1 agent. One key question is whether IM is associated specically with EBVve HD or, alternatively, associated as strongly with the cases
that lack EBV (the EBV-ve cases) that constitute the majority of cases in the young adult peak. Very few studies have looked at epidemiologic risk factors for HD with cases classied as EBVve or EBV-ve. Only 2 studies have collected personal data to address this question: a US case-series that compared EBVve and EBV-ve HD and included cases aged 16 55 years at diagnosis,9 and a UK case-control study10,11 that was restricted to subjects aged 16 24 years and analysed as both a case-series and case-control study. These 2 studies generated results that are potentially inconsistent, and suggest different answers to the key question. Sleckman et al.9 found no evidence that a history of IM conveyed specic risk for EBVve compared to EBV-ve HD. In contrast, Alexander et al.10,11 reported evidence that increased risk after IM was specic to EBVve HD, although there was also a small excess risk of EBV-ve HD after IM. These 2 results are consistent only if the age at diagnosis of HD becomes critical to the association of IM with subsequent HD. The study of Alexander and colleagues also found that family history of IM was a signicant risk factor for EBVve HD in the age range 16 24 years.12 Most affected relatives were siblings, and this was interpreted as further evidence that relatively late and recent exposure to EBV increased risk of EBVve HD in young adults; alternative interpretations involving confounding social factors and inherited susceptibility to EBV are also available. We now report the results of a population based case-control study (SNEHD: Scotland and Newcastle Epidemiological Study of Hodgkins Disease) for which all newly diagnosed adult cases of HD in a dened geographic area of Scotland and Northern England were eligible. We aimed, rst, to test the hypothesis that index history of IM, family history of IM or the 2 combined conveys both a small general risk of HD and a larger, specic risk of EBVve HD. Second, we aimed to test the modied hypothesis under which the specic risk of EBVve HD was conned to young adults. It is only this second hypothesis that is compatible
Grant sponsor: Kay Kendall Leukaemia Fund; Grant sponsor:LRF Specialist Programme Grant. *Correspondence to: Department of Community Health, Public Health Sciences, University of Edinburgh Medical School, Teviot Place, Edinburgh EH89AC, UK. Fax: 44-131-556-6793. E-mail: freda.alexander@ed.ac.uk Received 14 May 2002; Revised 21 October 2002, 9 December 2002; Accepted 11 December 2002 DOI 10.1002/ijc.11156
INFECTIOUS MONONUCLEOSIS AND ADULT HD
299
with the published work of both Sleckman et al.9 and Alexander et al.10,11 We restricted our analysis to classical HD because lymphocyte predominance HD is now considered a separate disease entity with a distinct aetiology.13
MATERIAL AND METHODS
Subjects Eligible cases were all people aged 16 74 years diagnosed with HD while resident in Scotland (excluding the Western Isles and Dumfries and Galloway) and the Northern Region of England from January 1, 1993 to July 31, 1997. Controls were randomly selected from computerised regional primary care lists (regions were Family Health Service Authorities (FHSAs) in England and Health Boards in Scotland). Control numbers were selected so that cases and controls would have similar frequencies by age group (16 24, 2534, . . . 6574), sex and region. An additional eligibility criterion imposed on cases and controls was that they must have been born in the UK. Cases were identied in the rst instance from the ongoing lymphoma registration system already in place for the study area: the Scotland and Newcastle Lymphoma Group.14 Annual cross checks with the relevant cancer registries (Scottish Cancer registry, Northern region cancer registry) provided a second source of cases. Provided that their treating consultants gave consent, cases were then approached by letter. The approach letter provided full information about our study and enabled subjects to give informed consent. When a patient died before being approached or before interview, the general practitioner (GP) was asked to give the name of a close relative and consent to approach the relative. Relatives who gave informed consent then provided proxy interviews. Controls were approached by letter in a similar way after receipt of consent to approach from their GP. When we failed to recruit a selected control we replaced this control with a second (or later) choice randomly selected from patients of the same age and sex on the list of the GP practice of the rst control. This process was intended to retain to some extent the socioeconomic status of the area of residence of our rst choice controls. Each case was given as a reference date the date of histologic diagnosis. Each control was allocated a reference date that was designed to have a similar relationship with date of interview as date of diagnosis for cases: random numbers were used to generate a year (19931997) with the month and day being that of the subjects birthday. Interview data Trained interviewers conducted face-to-face interviews, normally in subjects homes, to complete our study questionnaire. This questionnaire elicited personal medical history of a number of conditions relevant to our study hypotheses, including IM (glandular fever). Events were only included in the analyses if they occurred before the reference date. A list of rst-degree family members was also obtained, together with forenames and dates of birth/death. Respondents were asked whether they were aware of a previous diagnosis of a similar list of medical conditions for each of these relatives. This second list also contained IM. No particular emphasis was placed on IM but it is possible that responding cases were aware of a potential link between IM and HD. In response to the question, Have you previously had glandular fever?, respondents could answer yes, denitely, yes, suspected or no. Those answering yes were then asked if the diagnosis was conrmed by analysis of a blood sample. In the analyses reported here in detail, we have taken as prior IM an episode of illness that began before the diagnosis of HD and was described as yes, denitely or yes, suspected, but analyses were replicated with alternative denitions. Because the prodromal symptoms of HD can resemble IM, we also performed analyses in which illness occurring within the year before the reference date was excluded.
Family history of IM (in a rst-degree relative) was, mainly, analysed as a dichotomy: yes or no. However, we also attempted to introduce an improved measure that incorporated adjustment for number of relatives at risk. Specically, we calculated a weighted sum over available relatives based on their ages at reference date (weights of 0.06 for 0 4 years, 0.35 for 514 years and 1 for all others). The choice of weights was taken from an independent source.15 Family risk was then the number of affected rst-degree relatives divided by this weighted sum of relatives. Where we reported the affected relative (parent, sibling, child) and more than 1 relative was affected, we took the relationship from the relative whose IM occurred closest in time to the reference date. Similarly, the time gap from IM in a relative to the reference date was calculated as the shortest of the available times. We did not have detailed information on whether these family members were living together at the times when the relatives had IM, nor whether they met frequently. Nevertheless, we included an additional exposure variable index and/or family IM as a yes/no dichotomy. This is meaningful only if index and family IM are interpreted as indicators of a similar underlying biologic process: most probably, infection by EBV, but also, possibly, inherited susceptibility to EBV and, if the affected relative is a sibling, lifestyle conducive to late rst exposure to EBV. Socioeconomic status classication for eligible cases and controls was taken from the Carstairs index or depcat16 of the small census area in which they lived. Laboratory methods Parafn-embedded biopsy material and, if possible, immunohistochemically-stained sections were retrieved along with the relevant reports. Where satisfactory staining was not available, immunohistochemic staining was performed using the following panel of monoclonal antibodies: CD45, CD20, CD3, CD15, CD30 and EMA using a standard ABC peroxidase method (Vector Laboratories, Peterborough, UK) and a Dako Techmate automated stainer (Dako Ltd., Cambridgeshire, UK). Histopathologic review was carried out by B.A. and A.S.K., and if the review diagnosis differed from the original diagnosis or the diagnosis was considered problematic, the case was referred for discussion before reaching a diagnosis. Cases were classied according to the Revised European-American Lymphoma (REAL) classication,13 and those diagnosed as lymphocyte predominant were excluded from the statistical analysis. EBV status was determined by performing EBV EBER in situ hybridisation on sections of parafnembedded material using a commercially available probe (Vector Laboratories) and hybridization kit (Dako Ltd). In cases in which signicant numbers of bystander cells appeared to be staining on the EBER analysis, LMP-1 immunohistochemistry was also performed using the CS1-4 monoclonal antibodies (Dako Ltd.) and an ABC kit (Vectastain, Vector Laboratories). Cases were designated EBVve if Reed-Sternberg cells and variants stained positively in either of these assays. Statistical methods Except where nonparametric methods are specically indicated, all analyses were based on unconditional logistic regression.17 Four comparisons were systematically conducted: 1. 2. 3. 4. HD compared to controls EBVve HD compared to controls EBV-ve HD compared to controls EBVve HD compared to EBV-ve HD (the case-series analysis)
These comparisons yielded estimates of risk, expressed as odds ratios (OR) accompanied by 95% condence intervals (CI). An OR 1 indicates that the exposure is associated with the rst of the pair (e.g., with HD). All analyses were adjusted for gender and depcat in the regression modelling; analyses were further adjusted
300
ALEXANDER ET AL.
by age (16 34, 35 49, 50) except when data were restricted to young adults. Formal homogeneity tests of specicity of associations to the young adults tested the effect of adding a term for exposure only in young adults to a model that included the main affect of the exposure, age group, gender and depcat. The statistical packages SPSS and EGRET were used for the statistical analyses.
RESULTS
Altogether, 78% of eligible cases were recruited, but only 46% of our rst choice controls were recruited. Recruitment of rst choice controls was lowest for the youngest (16 24 years at reference date) and oldest (6574 at reference date) subjects (38% and 40%, respectively). In the youngest age group, male recruitment was much lower than female (21% compared to 28%), but it was higher in the oldest age group (43% and 36%, respectively). Control recruitment was strongly associated with deprivation of area of residence, with 61% of those living in areas with depcat 1 (most afuent) but just 36% of those with depcat 7 (most deprived) recruited. Case recruitment decreased with age over 55 years (around 80% for all age groups under 55, 68% for 55 64 and 60% for 6574). In general, case recruitment was slightly higher in females (80%) than males (75%). The numbers of interviewed subjects (cases of classical HD and controls) available for analyses are shown in Table I by age group and status. This excludes 54 interviewed cases of HD whose disease was classied as lymphocyte predominance HD. Analyses of case subgroups compared to controls by reported prior IM (Table II) showed several statistically signicant results, including those for total HD, which were of similar magnitude at all ages and in young adults and older people separately. EBVve HD was strongly and signicantly associated with index IM in young adults; while this association was also evident when the whole age range was analysed, it was of smaller magnitude and not statistically signicant in the older people alone. In contrast, the associations for EBV-ve HD were of similar magnitude across the age range, although only statistically signicant when all ages were combined. In the case-series analysis (EBVve and EBV-ve cases compared), the OR for young adults is modestly elevated, but this failed to approach statistical signicance; the OR for older people is close to unity. When similar analyses were conducted for family IM, statistically signicant associations were conned to the young adults, and were most marked in EBVve cases compared to the controls (Table II). Although the association remained statistically significant when total HD was compared to the controls, the case-series analysis indicated a specic association with EBVve cases. The homogeneity test demonstrated the statistical signicance of the differences between young adults and older people. Similar results were found when reports of IM within the year before reference date were excluded. We repeated these analyses with alternative denitions of index IM (taking those who reported merely suspicion of IM as no IM, and also taking suspicious but unconrmed IM as missing data). Both of these alternative denitions gave very similar results to those we report here. Exclusion
TABLE I NUMBERS OF SUBJECTS AVAILABLE FOR ANALYSIS Status Age range 35 3549 50 & over All adults
of cases for whom interviews had been conducted with surrogates (8 EBVve and 5 EBV-ve, of whom 1 was positive for index IM and 3 for family IM) made only marginal differences to the ORs. Times from index IM to reference date were compared using the Mann-Whitney test; those for EBVve cases were shorter than those for controls and EBV-ve cases (p 0.16 and 0.075, respectively). The relationship between index case and family member and the time between familial IM and reference date were examined for subjects reporting family IM. For the young adults, the majority (75%) of affected relatives were siblings, compared to 35% for older people, for whom 51% of affected relatives were children (p 0.001, Pearsons chi-square). The time gap between illness in a relative and reference date was shorter for the young ( 35) than older adults ( 35) (p 0.006, Mann-Whitney test). There was no evidence that these intervals were shorter for EBVve compared to EBV-ve cases, but when these cases were combined, the time gaps were shorter than for the controls (p 0.046, Mann-Whitney test). Finally, we restricted analyses of the time gaps to sibling IM; intervals were shortest for EBVve cases and longest for controls (p 0.09, Kruskal-Wallis test), and the differences for the EBVve and EBV-ve cases taken together and compared to the controls achieved statistical signicance (p 0.03, Mann-Whitney test). An alternative analysis of family IM took numbers of family members at risk into account. When risk in family members (now taken as a continuous variable) was analysed by the Mann-Whitney test, signicantly higher risk was found for EBVve HD compared to controls (p 0.001), total HD compared to controls (p 0.007) and EBVve HD compared to EBV-ve HD (p 0.016), but the excess for EBV-ve HD compared to controls was of borderline statistical signicance (p 0.09). A small number of subjects reported positively for both index and family IM (n 8 EBVve HD, n 3 EBV-ve HD and n 5 controls). Despite the small numbers, we conducted a multivariate analysis for the young adults with an extension of the previous models that included (i) terms for both index and family IM simultaneously and (ii) a further term for their interaction. There was no evidence of statistical interaction (all p-values 0.3); the adjusted analyses reduced, in general, the ORs reported in Table II but conrmed the importance of prior IM (both in index and relative) in relation to HD, especially when EBVve. For example, adjusted ORs for EBVve HD compared to controls were 2.50 (95% CI: 0.877.22, p 0.09) for index IM and 4.89 (95% CI: 1.98 12.07, p 0.001) for family IM. When index and/or family IM were taken together as a single exposure variable (Table III, all ORs for comparisons of case subgroups with the controls showed signicant elevations for the total age range and for the young adults. However, the magnitudes were larger for the young adults and for EBVve cases; the case-series analysis showed a signicant positive association with EBVve cases in the young adults. All ORs for older people were close to, or less than, unity. The formal test of homogeneity conrmed the age group differences.
DISCUSSION
EBVve classical HD EBVve classical HD Classical HD, EBV status not available Controls
44 145 17 235
21 49 15 117
48 49 20 161
113 243 52 513
This is the rst large case-control study of adult HD to have included EBV status of subjects, and the largest case-series comparison of epidemiologic variables for HD by EBV status. Our present study is also, we believe, the rst to report results restricted to classical HD and to have conducted histologic review that included immunohistochemistry. Smaller previous studies are a case-series comparison of 100 cases aged 18 55 years,9 a casecontrol study (n 103 cases) of 16- to 24-year-olds only10 and a case-series comparison based on the same subjects.11 These studies yielded potentially inconsistent results (see Introduction). SNEHD has potential methodologic problems: recall bias, selection bias, misclassication of prodromal HD as IM and lack of laboratory conrmation of IM diagnoses. We have noted that IM
INFECTIOUS MONONUCLEOSIS AND ADULT HD
TABLE II CLASSICAL HD, ASSOCIATIONS WITH REPORTED INDEX IM AND REPORTED FAMILY IM All adult ages1 Young adults (1634 yrs)2
301
Older persons (35 and older)3
Index prior IM4 HD vs. ctrl EBV vs. ctrl EBV vs. ctrl
EBV vs. EBV Family IM5 HD vs. ctrl EBV vs. ctrl EBV vs. ctrl EBV vs. EBV
OR (CI) p n1(%)n2(%) OR (CI) p n1(%)n2(%) OR (CI) p n1(%)n2 (%) OR (CI) p n1(%)n2(%) OR (CI) p n1(%)n2(%) OR (CI) p n1(%)n2(%) OR (CI) p n1(%)n2(%) OR (CI) p n1(%)n2(%)
2.48 (1.474.18) 0.001 43 (10.5%)/24 (4.7%) 2.59 (1.245.43) 0.016 12 (10.6%)/24 (4.7%) 2.11 (1.143.90) 0.019 22 (9.1%)/24 (4.7%) 1.37 (0.632.98) 0.43 12 (10.6%)/22 (9.1%) 1.23 (0.791.90) 0.36 44 (11.0%)/47 (9.3%) 1.81 (0.973.38) 0.07 16 (14.5%)/48 (9.5%) 1.24 (0.742.08) 0.43 26 (10.9%)/47 (9.3%) 1.65 (0.813.35) 0.18 16 (14.5%)/26 (10.9%)
2.61 (1.305.23) 0.005 27 (13.1%)/13 (5.6%) 2.94 (1.087.98) 0.045 7 (15.9%)/13 (5.5%) 1.88 (0.854.14) 0.12 14 (9.7%)/13 (5.6%) 1.76 (0.634.88) 0.29 7 (15.9%)/14 (9.7%) 2.43 (1.234.78) 0.018 27 (13.3%)/14 (6.0%) 5.22 (2.1512.68) 0.001 11 (25.0%)/15 (6.4%) 1.84 (0.853.96) 0.12 15 (10.6%)/14 (6.0%) 3.35 (1.338.44) 0.012 11 (25.0%)/15 (10.6%)
2.28 (1.025.10) 0.042 16 (7.9%)/11 (4.0%) 2.17 (0.716.66) 0.19 5 (7.2%)/11 (4.0%) 2.47 (0.936.55) 0.08 8 (8.2%)/11 (4.0%) 0.98 (0.293.27) 0.97 5 (7.2%)/8 (8.2%) 0.67 (0.361.26) 0.21 17 (8.6%)/33 (12.2%) 0.67 (0.241.82) 0.41 5 (7.6%)/33 (12.2%) 0.83 (0.391.76) 0.62 11 (11.5%)/33 (12.2%) 0.63 (0.202.00) 0.42 5 (7.6%)/11 (11.5%)
1 Adjusted for gender, deprivation of area of residence and age group (16 34, 35 49, older).2Adjusted for gender and deprivation of area of residence.3Adjusted for gender, deprivation of area of residence and age group (35 49, older).4Homogeneity test by age at diagnosis: all p values exceeded 0.4.5Homogeneity best by age at diagnosis: p 0.005 (HD vs. ctrl), 0.002 (EBVve HD vs. crtrl), 0.1 (EBVve HD vs.ctrl), 0.04 (EBVve HD vs. EBVve HD).
TABLE III CLASSICAL HD, ASSOCIATION WITH REPORTED IM IN INDEX AND/OR FAMILY MEMBER (COMBINED EXPOSURE VARIABLE) All adult ages1 Young adults (1634yrs)2 Older persons (35 and older)3
HD vs. ctrl EBV vs. ctrl EBV vs. ctrl EBV vs. EBV
OR (CI) p n1(%)/n2(%)4 OR (CI) p n1(%)/n2 (%) OR (CI) p n1(%)/n2(%) OR (CI) p n1(%)/n2(%)
1.68 (1.172.41) 0.005 79 (19.8%)/66 (13.1%) 2.03 (1.193.46) 0.012 24 (21.8%)/67 (13.3%) 1.60 (1.042.44) 0.03 45 (18.9%)/66 (13.1%) 1.43 (0.792.60) 0.24 24 (21.8%)/45 (18.9%)
2.47 (1.474.15) 0.001 49 (24.1%)/27 (11.6%) 3.85 (1.818.19) 0.001 15 (34.1%/28 (12.0%) 1.90 (1.053.41) 0.031 28 (19.7%)/27 (11.6%) 2.46 (1.115.49) 0.03 15 (34.1%)/28 (19.7%)
1.11 (0.661.88) 0.69 30 (15.2%)/39 (14.4%) 1.08 (0.482.39) 0.86 9 (13.6%)/39 (14.4%) 1.25 (0.652.39) 0.50 17 (17.7%)/39 (14.4%) 0.73 (0.291.85) 0.51 9 (13.6%)/17 (17.7%)
1 Adjusted for gender, deprivation of area of residence and age group (16 34, 35 49, older); homogeneity test for age at diagnosis; p 0.03 (HD vs. ctrl), 0.02 (EBVve HD vs. ctrl), 0.3 (EBVve HD vs. ctrl), 0.07 (EBVve HD vs. EBVve HD).2Adjusted for gender and deprivation of area of residence.3Adjusted for gender, deprivation of area of residence and age group (35 49, older).4Numbers and percentages ve in 1st group/in 2nd group.
was not highlighted in the questionnaire in any way; however, cases may have become aware outside our study that a relationship between IM and HD is an important area of scientic research. Selection bias is certainly present, in that recruitment of our rst choice controls was strongly associated with the socioeconomic status of their area of residence. We tried to prevent inuence on our case-control comparisons in 2 ways: rst, by replacing controls with second and later choices from the same GP (hence, broadly, the same area of residence) and second, by adjusting all logistic regression analyses by depcat. Neither of these succeeded in removing the effects of socioeconomic status imbalance in our controls.18 It is possible, therefore, that our case-control comparisons for total HD may have been inuenced by recall bias and selection bias. However, cases had no knowledge of the EBV status of their tumour. The same set of controls were used in all case-control comparisons; neither recall nor selection bias could have inuenced differences between EBVve and EBV-ve HD
when compared to controls or when compared to each other in the case-series analysis. Lack of laboratory conrmation of IM should have led to nondifferential misclassication bias and, hence, biased our reported ORs towards the null. Differential misclassication can only arise if prodromal HD was misclassied as IM in cases; this may have occurred for total IM but there is no reason to suggest that it applies preferentially to EBVve or EBV-ve cases. We attempted to overcome this problem by replicating our analyses with exclusion of subjects with IM diagnosed within 1 year of the reference date. We believe that differential misclassication may have inuenced our results for total HD but not for differences between EBVve and EBV-ve HD when compared to controls or when compared to each other in the case-series analysis. Despite the large size of the overall study, our numbers are relatively small within age-group categories. Nevertheless, we
302
ALEXANDER ET AL.
consider it essential to analyse young adults and older people separately because there is overwhelming evidence that the aetiologies are distinct (see Introduction). Our data conrm our hypothesis that index IM conveys, or is a marker for, increased risk of HD that applies outside the young adult peak and outside the EBVve subgroup of cases. The magnitude of the risk we report is between 2 and 3 and is consistent with the cohort studies estimate of a 3-fold increase. The highest OR we report is for EBVve cases in young adults compared to controls, and there is a suggestion in our data that there is a specic additional risk of EBVve HD in this age-group after IM. This conrms results reported from our previous case-control study.10 When IM in rst-degree blood relatives was analysed, we found evidence of increased risk of, specically, EBVve HD in young adults. Here, IM in rst-degree blood relatives is capable of 2 (not mutually exclusive) interpretations: it may indicate an inherited host response to EBV infection, and it may indicate likelihood of rst infection by EBV beyond early childhood either by direct infection from the affected relative or, in the case of siblings, a childhood lifestyle conducive to subsequent delayed infection by EBV. Although we collected extensive data on dates of birth of relatives and dates of IM in relatives. we do not know how frequently and when relatives actually met, and so our data cannot be unambiguously interpreted in terms of the second alternative. Nevertheless, the results we reportspecically: (i) the difference in relationship of relative by age at reference date (i.e., siblings predominating as affected relatives in our young adult subjects but not subsequently); (ii) age-group specicity; and (iii) the shorter time intervals from relative IM to reference date for casestaken together, point to family IM in young adults being a marker for late exposure of index subjects to EBV. In the belief that this is true, we considered the composite exposure variable (own and/or family IM) as an indicator of potential late rst exposure to EBV. Although this interpretation is open to question, the results provide consistency that increases their plausibility: rst, there is a general increase in risk of total HD across all ages and involving both EBVve and EBV-ve HD and second, there is a specic risk of EBVve HD in young adults. This is consistent with the previously published epidemiologic data for IM and HD by EBV status.9 11
The most important existing models for HD aetiology are the multiple aetiology model1 and the polio model.3 Under the multiple aetiology model, HD in children, young adults and older people has distinct aetiologies. Under the polio model, the same infectious agent contributes to the aetiology of HD in children and young adults but infection with the agent during childhood conveys much reduced risk of subsequent HD compared to infection as a young adult. This higher risk is embodied in the late hostresponse model,2 which also seeks to explain the young adult peak under the multiple aetiology model. The identication of EBVve and EBV-ve HD as 2 large subsets of total HD has led to debate as to whether either model has adequate complexity.19 It is clear that the polio model, with EBV as infectious agent, does not explain the epidemiology of all HD because most cases are not EBVve and some cases have never been infected by EBV (i.e., are seronegative [Gallagher et al., unpublished], lack EBV in PCR analyses of peripheral blood and have no cytotoxic T-cell responses to EBV [Khan et al., unpublished]). Our main conclusion after the present analyses is that the polio model is an attractive one for paediatric and young adult EBVve HD. We have clearly demonstrated that young adults who have, themselves, been exposed to EBV late and succumbed to IM, together with those whose relatives have done so, are at substantially increased risk of HD that (at least when relatives are included) is specically EBVve. The specicity of this risk attenuates with age and time. Separation of individual effects of age and time is almost impossible. Our data add nothing to knowledge of paediatric EBVve HD but there is a growing body of epidemiologic data indicating increased frequency in places where exposure to EBV is likely to occur early.6 In the UK, both residence in an area of low SES and South Asian ethnicity contribute independently to EBV positivity in pediatric HD.20 For EBV-ve HD, we provided evidence that IM conveys increased risk of subsequent HD. This is strongest in the young adult peak but persists beyond it. Although this evidence is less strong, we prefer to interpret it, provisionally and in accordance with the literature, as indicating a genuine increased risk consequent upon behaviour and lifestyle that predispose to late rst infection by EBV and also other common infectious agents. Our data provide no evidence that EBV, itself, is causally associated with EBV-ve HD but offer limited support for the late host-response model for EBV-ve HD in young adults.
REFERENCES
1.
MacMahon M. Epidemiology of Hodgkins disease. Cancer Res 1966; 26:1189. 2. Gutensohn N, Cole P. Childhood social-environment and Hodgkins disease. N Engl J Med 1981;304:135 40. 3. Gutensohn N, Cole P. Epidemiology of Hodgkins disease. Semin Oncol 1980;7:92102. 4. Hjalgrim H, Askling J, Sorensen P. Risk of Hodgkins disease and other cancers after infectious mononucleosis. J Natl Cancer Inst 2000;92:1522 8. 5. Pallesen G, Hamilton-Dutoit SJ, Rowe M, Young LS. Expression of Epstein-Barr virus latent gene products in tumour cells of Hodgkins disease. Lancet 1991;337:320 2. 6. Jarrett RF, Armstrong AA, Alexander FE. Epidemiology of EBV and Hodgkins lymphoma. Ann Oncol 1996;7:S510. 7. IARC. Proceedings of the IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Epstein-Barr virus and Kaposis sarcoma herpesvirus/human herpesvirus 8. Lyon, France, 1724 June 1997. IARC Monogr Eval Carcinog Risks Hum 1997;70:1 492. 8. Armstrong AA, Alexander FE, Cartwright RA, Angus B, Krajewski AS, Wright DH, Brown I, Lee F, Krane E, Jarrett RF. Epstein-Barr virus and Hodgkins disease: further evidence for the three disease hypothesis. Leukemia 1998;12:1272 6. 9. Sleckman BG, Mauch PM, Ambinder RF. Correlation between EBVstatus and risk factor prole in Hodgkins disease. Cancer Epidemiol Biomark Prev 1998;7:111721. 10. Alexander FE, Jarrett RF, Lawrence DJ, Armstrong AA, Freeland J, Gokhale DA, Kane E, Taylor GM, Wright DH, Cartwright RA. Risk factors for Hodgkins disease by Epstein-Barr virus (EBV) status: prior infection by EBV and other agents. Br J Cancer 2000;82:111721. 11. Alexander FE, Jarrett RF, Cartwright RA, Armstrong AA, Gokhale D, Kane E, Gray D, Lawrence DJ, Taylor GM. Epstein-Barr virus and
12. 13.
14. 15. 16. 17. 18. 19. 20.
HLA-DPB1-*0301 in young adult Hodgkins disease: evidence for inherited susceptibility to Epstein-Barr virus in cases that are EBVve. Cancer Epidemiol Biomark Prev 2001;10:7059. Lawrence DJ. The epidemiology of Hodgkins disease with special reference to EBV status. PhD Thesis, University of Edinburgh, Edinburgh, 1999. Harris NL, Jaffe ES, Stein H, Banks PM, Chan JKC, Cleary ML, Delsol G, Dewolfpeeters C, Falini B, Gatter KC, Grogan TM, Isaacson PG, et al. A revised European-American classication of lymphoid neoplasmsa proposal from the International Lymphoma Study Group. Blood 1994;84:136192. The PACE (population adjusted clinical epidemiology) strategy: a new approach to multi-centred clinical research. QJ Med 1997;90: 14751. Douglas AS, Brown T, Reid D. Infectious mononucleosis and Hodgkins disease - A similar seasonality. Leuk Lymph, 1996; 23: 323-331. Jarman B, Townsend P, Carstairs V. Deprivation indices. Br J Med 1991;303:523. Clayton D, Hills M. Statistical methods in epidemiology. New York: Oxford University Press, 1993. Law GR, Smith AG, Roman E, for the United Kingdom Childhood Cancer Study Investigators. The importance of full participation: lessons from a national case-control study. Br J Cancer 2002;86:35055. Jarrett RF. Viruses and Hodgkins lymphoma. Ann Oncology 2002; 13(Suppl 1):239. Flavell KJ, Biddulph JP, Powell JE, Parkes SE, Redfern D, Weinreb M, Nelson P, Mann JR, Young LS, Murray PG. South Asian ethnicity and material deprivation increase the risk of Epstein-Barr virus infection in childhood Hodgkins disease. Br J Cancer 2001;85:350 6.
You might also like
- Risk Factors for Developing LeprosyDocument8 pagesRisk Factors for Developing LeprosyAjie WitamaNo ratings yet
- Esclerosis ArtDocument13 pagesEsclerosis ArtKelly GómezNo ratings yet
- Journal Pone 0034866Document4 pagesJournal Pone 0034866Seki MuminovicNo ratings yet
- MS27x 17 PDFDocument9 pagesMS27x 17 PDFijasrjournalNo ratings yet
- Review Article: Pediatric Multiple Sclerosis: Current Concepts and Consensus DefinitionsDocument24 pagesReview Article: Pediatric Multiple Sclerosis: Current Concepts and Consensus DefinitionsKelly GómezNo ratings yet
- Low level viremia is associated with Serious Non-AIDS Events in People Living with HIVDocument20 pagesLow level viremia is associated with Serious Non-AIDS Events in People Living with HIVAbrahamKatimeNo ratings yet
- Herpes ZosterDocument8 pagesHerpes ZosterPramita SariNo ratings yet
- LSHTM Study Designs NOTES LSTHMDocument39 pagesLSHTM Study Designs NOTES LSTHMKELVIN MAYOMBONo ratings yet
- Risk Factor TuberculinDocument7 pagesRisk Factor TuberculinAnonymous oUg5v1p4zNo ratings yet
- Jurnal PVDocument8 pagesJurnal PVAndreas SudarmadiNo ratings yet
- Antimicrobial Therapy and Late Onset SepsisDocument10 pagesAntimicrobial Therapy and Late Onset SepsisKendy LópezNo ratings yet
- Risk Factors For Herpes Zoster Infection: A Meta-Analysis: Review ArticleDocument8 pagesRisk Factors For Herpes Zoster Infection: A Meta-Analysis: Review Articleyenny handayani sihiteNo ratings yet
- Endemic Kaposi Sarcoma in HIV-negativeDocument7 pagesEndemic Kaposi Sarcoma in HIV-negativeAriana AmarilesNo ratings yet
- Pediatrics 2012Document9 pagesPediatrics 2012Elin TaopanNo ratings yet
- Risk Factors For Tuberculosis InfectionDocument13 pagesRisk Factors For Tuberculosis InfectionIndahMayaSafitriNo ratings yet
- Population-Wide Analysis of Differences in Disease Progression Patterns in Men and WomenDocument14 pagesPopulation-Wide Analysis of Differences in Disease Progression Patterns in Men and WomenSagar SononeNo ratings yet
- Eating Disorders Epidemiology Incidence Prevalence Mortality RatesDocument9 pagesEating Disorders Epidemiology Incidence Prevalence Mortality RatesVictória NamurNo ratings yet
- Trend and Outcome of Sepsis in ChildrenDocument8 pagesTrend and Outcome of Sepsis in ChildrenGunduz AgaNo ratings yet
- Eclinicalmedicine: Victoria Peer, Naama Schwartz, Manfred S. GreenDocument10 pagesEclinicalmedicine: Victoria Peer, Naama Schwartz, Manfred S. GreenBryam Arango HuamanNo ratings yet
- Epidemiological Study of Clinical and Laboratory Profiles of Patients Woth ALL at DR SoetomoDocument5 pagesEpidemiological Study of Clinical and Laboratory Profiles of Patients Woth ALL at DR SoetomoJulia Intan Permata SariNo ratings yet
- Personality disorders and criminal behavior focus of psychiatric studyDocument1 pagePersonality disorders and criminal behavior focus of psychiatric studyAyu Ersya WindiraNo ratings yet
- Epi Descriptive Study DesignsDocument4 pagesEpi Descriptive Study DesignsAndrea BardalesNo ratings yet
- Captura de Pantalla 2024-01-23 A La(s) 11.26.43Document9 pagesCaptura de Pantalla 2024-01-23 A La(s) 11.26.43Dany MorBenNo ratings yet
- RAE - Articulo en InglesDocument3 pagesRAE - Articulo en InglesMaria Alejandra Suarez BaronNo ratings yet
- Kawasaki Disease: An Update: EpidemiologyDocument10 pagesKawasaki Disease: An Update: EpidemiologyEmma González de BaideNo ratings yet
- Review Article: The Risk Factors of Acquiring Severe Hand, Foot, and Mouth Disease: A Meta-AnalysisDocument13 pagesReview Article: The Risk Factors of Acquiring Severe Hand, Foot, and Mouth Disease: A Meta-AnalysisFan AccountNo ratings yet
- 17akinbolaji EtalDocument5 pages17akinbolaji EtaleditorijmrhsNo ratings yet
- Epidemiologic Study of Langerhans Cell Histiocytosis in Children.Document9 pagesEpidemiologic Study of Langerhans Cell Histiocytosis in Children.marioNo ratings yet
- Johne's Disease and Crohn's Disease, Report in BriefDocument2 pagesJohne's Disease and Crohn's Disease, Report in BriefNational Academies of Science, Engineering, and MedicineNo ratings yet
- Tropmed 86 698 PDFDocument5 pagesTropmed 86 698 PDFsandraldiraNo ratings yet
- International Journal of Pediatric Research Ijpr 9 112Document12 pagesInternational Journal of Pediatric Research Ijpr 9 112VsbshNo ratings yet
- Pediatrics 2013 Iwamoto E817 24Document10 pagesPediatrics 2013 Iwamoto E817 24phobicmdNo ratings yet
- Legionnaires' Disease Incidence and Risk Factors, New York, New York, USA, 2002-2011Document8 pagesLegionnaires' Disease Incidence and Risk Factors, New York, New York, USA, 2002-2011Stella ValenskaNo ratings yet
- Gittle R 2017Document4 pagesGittle R 2017Hari 'hardyboy' PurwantoNo ratings yet
- Journal of Rheumatology 2022 - Trajectory of Damage Accrual in SLE Based On Ethnicity and Socioeconomic FactorsDocument7 pagesJournal of Rheumatology 2022 - Trajectory of Damage Accrual in SLE Based On Ethnicity and Socioeconomic FactorsTengku Reza MaulanaNo ratings yet
- Travel-Associated Antimicrobial Drug-Resistant Nontyphoidal Salmonellae, 2004-2009Document9 pagesTravel-Associated Antimicrobial Drug-Resistant Nontyphoidal Salmonellae, 2004-2009Diandhara NuryadinNo ratings yet
- Community-Acquired Pneumonia Requiring Hospitalization Among U.S. ChildrenDocument11 pagesCommunity-Acquired Pneumonia Requiring Hospitalization Among U.S. ChildrenParasNo ratings yet
- Risk Factors For Childhood Leukemia: A Comprehensive Literature ReviewDocument37 pagesRisk Factors For Childhood Leukemia: A Comprehensive Literature Reviewmisbahhari_mdNo ratings yet
- Survival Analysis of Adult Tuberculosis Disease: Olurotimi Bankole Ajagbe, Zubair Kabair, Terry O'ConnorDocument10 pagesSurvival Analysis of Adult Tuberculosis Disease: Olurotimi Bankole Ajagbe, Zubair Kabair, Terry O'ConnorGetachew GemedaNo ratings yet
- Jurnal AlergiDocument10 pagesJurnal AlergiAbdurrahman HasanuddinNo ratings yet
- Early-Onset Basal Cell CarcinomaDocument11 pagesEarly-Onset Basal Cell CarcinomajxmackNo ratings yet
- Demographic Variations in HIV Testing History Among Emergency Department Patients: Implications For HIV Screening in US Emergency DepartmentsDocument7 pagesDemographic Variations in HIV Testing History Among Emergency Department Patients: Implications For HIV Screening in US Emergency DepartmentsAnyone ElseNo ratings yet
- Age-Related Differences in Hospitalization Rates, Clinical Presentation, and Outcomes Among Older Adults Hospitalized With Influenza-U.S. Influenza Hospitalization Surveillance NetworkDocument8 pagesAge-Related Differences in Hospitalization Rates, Clinical Presentation, and Outcomes Among Older Adults Hospitalized With Influenza-U.S. Influenza Hospitalization Surveillance NetworkTony RobertsNo ratings yet
- Nihms 1688237Document20 pagesNihms 1688237Mohammed KhalidNo ratings yet
- Diag BronchiolitisDocument2 pagesDiag BronchiolitisoussamamusNo ratings yet
- Baldwin 2016Document10 pagesBaldwin 2016Nahda Fini SNo ratings yet
- Autism, Inflammatory Bowel Disease, and MMR VaccineDocument1 pageAutism, Inflammatory Bowel Disease, and MMR VaccineSinn VolleNo ratings yet
- CISH and Susceptibility To Infectious Diseases: Original ArticleDocument10 pagesCISH and Susceptibility To Infectious Diseases: Original ArticlenovianastasiaNo ratings yet
- Do We Need A New Definition of Sepsis?: Intensive Care Medicine February 2015Document4 pagesDo We Need A New Definition of Sepsis?: Intensive Care Medicine February 2015Amirullah AbdiNo ratings yet
- Dengue Hemorrhagic Fever in Infants: A Study of Clinical and Cytokine ProfilesDocument12 pagesDengue Hemorrhagic Fever in Infants: A Study of Clinical and Cytokine ProfilesYono FabiandiNo ratings yet
- HCW Vs Adult Influenza IncidenceDocument9 pagesHCW Vs Adult Influenza Incidencereza_adrian_2No ratings yet
- Epidemiology and Genetics of Rheumatoid Arthritis: Supplement ReviewDocument8 pagesEpidemiology and Genetics of Rheumatoid Arthritis: Supplement ReviewdionysiaNo ratings yet
- Nutritional Status and Tuberculosis Risk in Adult and Pediatric Household ContactsDocument17 pagesNutritional Status and Tuberculosis Risk in Adult and Pediatric Household ContactshasmawihadriantiNo ratings yet
- Research Paper On Aids in AmericaDocument6 pagesResearch Paper On Aids in Americajssoulznd100% (1)
- Respiratory Syncytial Virus Infections in Children With Acute Myeloid Leukemia: A Report From The Children's Oncology GroupDocument3 pagesRespiratory Syncytial Virus Infections in Children With Acute Myeloid Leukemia: A Report From The Children's Oncology GrouperickmattosNo ratings yet
- 30 Scientific Studies Link Vaccines to AutismDocument23 pages30 Scientific Studies Link Vaccines to Autismazrulelias100% (5)
- Gender 22Document4 pagesGender 22andi tzamrah istiqani syamNo ratings yet
- Knowledge Attitudes and Testing Preferences For Herpes Simplex Virus Infections Among Undergraduate Students at A Large University in Los AngelesDocument7 pagesKnowledge Attitudes and Testing Preferences For Herpes Simplex Virus Infections Among Undergraduate Students at A Large University in Los AngelessesiaNo ratings yet
- International Journal of Infectious Diseases: A A B A A A A A A A A B ADocument9 pagesInternational Journal of Infectious Diseases: A A B A A A A A A A A B AzikryauliaNo ratings yet
- Managing Health in the Genomic Era: A Guide to Family Health History and Disease RiskFrom EverandManaging Health in the Genomic Era: A Guide to Family Health History and Disease RiskNo ratings yet
- What Did The Martyrs Die For?: Martyrs or Political Criminals?Document13 pagesWhat Did The Martyrs Die For?: Martyrs or Political Criminals?Mihailo Majk ŽikićNo ratings yet
- Learn English A Beginner S Guide For Esl Learners Swan JennaDocument117 pagesLearn English A Beginner S Guide For Esl Learners Swan Jennasofronelena100% (6)
- Creation Out of Nothing: King Lear IV, 4, 122-6Document7 pagesCreation Out of Nothing: King Lear IV, 4, 122-6Mihailo Majk ŽikićNo ratings yet
- Data Science and Big Data Computing - Frameworks and MethodologiesDocument332 pagesData Science and Big Data Computing - Frameworks and MethodologiesMihailo Majk Žikić89% (9)
- Roman Catholic Church of CorruptionDocument4 pagesRoman Catholic Church of CorruptionherbertheadNo ratings yet
- Writing Magazine - August 2016Document112 pagesWriting Magazine - August 2016Mihailo Majk ŽikićNo ratings yet
- Word 2010 Thesis FinalDocument13 pagesWord 2010 Thesis FinalMihailo Majk ŽikićNo ratings yet
- 2005 09798 012Document7 pages2005 09798 012Mihailo Majk ŽikićNo ratings yet
- Nursing Growth and Development - G and D General OverviewDocument15 pagesNursing Growth and Development - G and D General OverviewMihailo Majk ŽikićNo ratings yet
- Biodiversity LichensDocument7 pagesBiodiversity LichensMihailo Majk ŽikićNo ratings yet
- Monasteries and Churches On Aegina IslandDocument2 pagesMonasteries and Churches On Aegina IslandMihailo Majk ŽikićNo ratings yet
- Severe Defects in Absorptive Ion Transport in Distal Colons of Mice That Lack ClC-2 ChannelsDocument7 pagesSevere Defects in Absorptive Ion Transport in Distal Colons of Mice That Lack ClC-2 ChannelsMihailo Majk ŽikićNo ratings yet
- Rabit Distal Colon Epithelium - IIDocument4 pagesRabit Distal Colon Epithelium - IIMihailo Majk ŽikićNo ratings yet
- Bcl-2 Gene Promotes Haemopoietic Cell Survival and Co... (NatureDocument1 pageBcl-2 Gene Promotes Haemopoietic Cell Survival and Co... (NatureMihailo Majk ŽikićNo ratings yet
- Active Potassium Transport Across Guinea-Pig Dista... (J PhysiolDocument1 pageActive Potassium Transport Across Guinea-Pig Dista... (J PhysiolMihailo Majk ŽikićNo ratings yet
- 8 Tones PresentationDocument42 pages8 Tones PresentationMihailo Majk Žikić100% (1)
- NURE 212course SyllabusDocument11 pagesNURE 212course SyllabusMihailo Majk ŽikićNo ratings yet
- Erikson's 8 Stages of Psychosocial Development Summary ChartDocument1 pageErikson's 8 Stages of Psychosocial Development Summary ChartMihailo Majk ŽikićNo ratings yet
- 001Document48 pages001Mihailo Majk ŽikićNo ratings yet
- Basolateral K-CL Cotransporter Regulates Colonic Potassium Absorption in Potassium Depletion PDFDocument7 pagesBasolateral K-CL Cotransporter Regulates Colonic Potassium Absorption in Potassium Depletion PDFMihailo Majk ŽikićNo ratings yet
- Active Potassium Transport Across Guinea-Pig Distal Colon - Action of S - by Gerhard Rechkemmer, Et Al PDFDocument2 pagesActive Potassium Transport Across Guinea-Pig Distal Colon - Action of S - by Gerhard Rechkemmer, Et Al PDFMihailo Majk ŽikićNo ratings yet
- Biological and Medical PhysicsDocument21 pagesBiological and Medical PhysicsMihailo Majk ŽikićNo ratings yet
- Principles of Embryonic DevelopmentDocument29 pagesPrinciples of Embryonic DevelopmentMihailo Majk ŽikićNo ratings yet
- Impact of Dairy Subsidies in NepalDocument123 pagesImpact of Dairy Subsidies in NepalGaurav PradhanNo ratings yet
- Egg Pasteurization Manual 1969Document54 pagesEgg Pasteurization Manual 1969Tomas MuzzioNo ratings yet
- RESEARCH PROPOSAL-Final AfraaaazzzzzzzzzDocument13 pagesRESEARCH PROPOSAL-Final AfraaaazzzzzzzzzRizwan Abdul Maalik50% (2)
- The Motive Journal (3rd Edition)Document42 pagesThe Motive Journal (3rd Edition)Shubham Sharma0% (1)
- 432 HZ - Unearthing The Truth Behind Nature's FrequencyDocument6 pages432 HZ - Unearthing The Truth Behind Nature's FrequencyShiv KeskarNo ratings yet
- 3.SAFA AOCS 4th Ed Ce 2-66 1994Document6 pages3.SAFA AOCS 4th Ed Ce 2-66 1994Rofiyanti WibowoNo ratings yet
- SafewayDocument70 pagesSafewayhampshireiiiNo ratings yet
- Test Units and Accessories: Sinteso™Document22 pagesTest Units and Accessories: Sinteso™Imad QsnNo ratings yet
- Myofascial Release for Piriformis MyalgiaDocument14 pagesMyofascial Release for Piriformis MyalgiaApoorvNo ratings yet
- Research PaperDocument12 pagesResearch PapershreyanshNo ratings yet
- DSUSJRC01161350 Corail ST-Total Hip SystemDocument20 pagesDSUSJRC01161350 Corail ST-Total Hip SystemXeniaNo ratings yet
- 9 Oet Reading Summary 2.0-195-213Document19 pages9 Oet Reading Summary 2.0-195-213Vijayalakshmi Narayanaswami0% (1)
- Versidrain 150: Green RoofDocument2 pagesVersidrain 150: Green RoofMichael Tiu TorresNo ratings yet
- VentilationDocument92 pagesVentilationRobert Nixon100% (1)
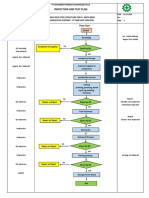
- Inspection and Test Plan: Flow Chart Start IncomingDocument1 pageInspection and Test Plan: Flow Chart Start IncomingSinden AyuNo ratings yet
- Rice Research: Open Access: Black Rice Cultivation and Forming Practices: Success Story of Indian FarmersDocument2 pagesRice Research: Open Access: Black Rice Cultivation and Forming Practices: Success Story of Indian Farmersapi-420356823No ratings yet
- Platinum Gazette 29 November 2013Document12 pagesPlatinum Gazette 29 November 2013Anonymous w8NEyXNo ratings yet
- Refresher 2 (Pipe)Document12 pagesRefresher 2 (Pipe)Kira YagamiNo ratings yet
- Final TLE9 Nail Care9 Q1 Module 3Document20 pagesFinal TLE9 Nail Care9 Q1 Module 3Ma. Andrea LagmanNo ratings yet
- Presentation On Data Integrity in PharmaDocument80 pagesPresentation On Data Integrity in Pharmaskvemula67% (3)
- Evolution Chart 3Document1 pageEvolution Chart 3sasupraNo ratings yet
- SEXUALABUSEDocument12 pagesSEXUALABUSERyoman EchozenNo ratings yet
- PR Cuisine vs US CuisineDocument2 pagesPR Cuisine vs US CuisineJannette HernandezNo ratings yet
- Electrolyte AE 11 - MSDSDocument8 pagesElectrolyte AE 11 - MSDSShinta Nugraha MughniNo ratings yet
- Flexible and Alternative Seating: in ClassroomsDocument5 pagesFlexible and Alternative Seating: in ClassroomsweningNo ratings yet
- Carbon Cycle Game Worksheet - EportfolioDocument2 pagesCarbon Cycle Game Worksheet - Eportfolioapi-264746220No ratings yet
- Limetas Maximos ResidualesDocument27 pagesLimetas Maximos ResidualesXjoelx Olaya GonzalesNo ratings yet
- El Bill PDFDocument2 pagesEl Bill PDFvinodNo ratings yet
- The Congressional Committee and Philippine Policymaking: The Case of The Anti-Rape Law - Myrna LavidesDocument29 pagesThe Congressional Committee and Philippine Policymaking: The Case of The Anti-Rape Law - Myrna LavidesmarielkuaNo ratings yet
- Catalogo Unidad Enfriadora Trane R-407C PDFDocument8 pagesCatalogo Unidad Enfriadora Trane R-407C PDFJUAN FRANCISCO AYALANo ratings yet