Professional Documents
Culture Documents
Disease of The Nose and The Paranasal Sinuses
Uploaded by
spajda69Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Disease of The Nose and The Paranasal Sinuses
Uploaded by
spajda69Copyright:
Available Formats
DISEASE OF THE NOSE AND THE PARANASAL SINUSES Dr.
Hernandez June 29,2010
I. II. III.
Mild- normal sleep, normal daily activities Moderate Severe- abnormal sleep, impairment of daily activities, problems caused at work or school.
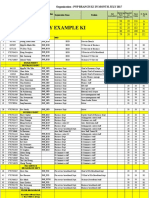
A. Rhinitis Allergic Rhinitis Viral Rhinitis Non-allergic Rhinitis Atrophic Rhinitis Rhinitis Medicamentosa B. Rhinosinusitis C. Tumors of the Nose and Paranasal Sinuses Nasal Polyps Inverting Papilloma Carcinoma Rhinitis Inflammation of the lining mucosa of the nose, characterized by one or more of the following symptoms: o Nasal congestion o Rhinorrhea o Sneezing o Itching Rhinitis may appear to be a simple disorder, but it can lead to more serious problems if overlooked and left untreated. Sequelae of Rhinitis: o Sinusitis o Otitis media o Tonsillopharyngitis o Laryngitis o Asthma
New Classification Intermittent symptoms <4 days per week or <4 weeks
Persistent symptoms Mild Normal sleep Normal daily activities, sport, leisure Normal work and school No troublesome symptoms >4 days/week and >4 weeks
Moderate-Severe (one or more items) Abnormal sleep Impairment of daily activities, sport, leisure Problems caused at work or school Troublesome symptoms
Signs and symptoms of Allergic Rhinitis Sneezing - pale boggy turbinates Nasal itchiness -conjunctiva injected Clear, watery rhinorrhea - allegic shiners and nasal salute Nasal congestion -linea nasalis
Classification of Rhinitis 1. 2. 3. Allergic Intermittent or Persistent Infectious Acute or Chronic or Idiopathic Others Idiopathic or Etc. or NARES (non allergic rhinitis with eosinophilia)
Definitions Allergic shiners- infraorbital dark circles probably related to venous plexus engorgement Dennies line- an accentuated line or atopic pleat of the lower eyelid Allergic Rhinitis (accdg to Wang De Yun) Affects about 10-20% of the world population and studies in several countries suggest that it is on the increase.
Al lergic Rhinitis Recurrent Rhinitis due to an IgE mediated reaction of the nasal mucosa to allergens Provoked by exposure to allergens in the environment o Pollens- tree such as alder, hazel, oak, elm and birch grass, weed o House dust mites o Animal danders o Cockroaches and certain mold species
International Study of Asthma and Allergies in Childhood (ISAAC) Study (Phil. 1994) Prevalence of Allergic Rhinitis has increased 6-7 years old- 26.2% 13-14 years old- 19.1% Adult- 38%
Classification of Allergic Rhinitis (ARIA 2007) 1. 2. Intermittent symptoms- <4 days per week or <4 weeks a year Persistent symptoms- >4 days/week and >4 weeks a year
United Airways (Evans R. 1993, Eggleston PA, 1988) Rhinitis and Asthma are common diseases which frequently co-exist Suggesting the concept one airway one disease
A fun hazily snail barn aftermaster
Page 1
Epidemiologic studies have consistently shown that asthma and rhinitis co-exist in the same patient 65-88% of Adults (Yaacob, 1991; Dahl, 1993) 75%of children with asthma also suffers from Allergic Rhinitis (Mercer MJ, 1991) Approximately 80% of asthmatics have allergic rhinitis Approximately 40% of allergic rhinitis patients have asthma
Rhinitis Medicamentosa A form of idiopathic rhinitis characterized by worsening rebound congestion following prolong use of topical decongestants. Topical decongestants are advised continuous use not longer than 10 days. Rhinoscopy reveals congested and swollen turbinates Treatment: discontinue topical decongestants; shifting to topical nasal steroids and systemic decongestants
Allergic Rhinitis and Its Impact on Asthma Allergic rhinitis is a major chronic airway disease Allergic rhinitis represents a risk factor for asthma A single treatment strategy is needed in patients with allergic rhinitis and asthma Practical Purposes 1. 2. 3. 4. History General ENT examination Endoscopy Radiology
Infectious Rhinitis A. Acute 1. Viral- clear watery discharge, 4-5 days in duration. Commonly caused by a cold virus which is well over a hundred rhinoviruses 2. Bacterial- mucopurulent d/c a. Streptococcus pneumonia b. H. influenza B. ChronicMycobacterium tuberculosis; Mycobacterium leprae; Klebsiella rhinoscleroma; Treponema pallidum; Fungi Other Types of Rhinitis (non-allergic, noninfective) A. B. C. D. E. F. G. H. Idiopathic NARES Occupational rhinitis Hormonal rhinitis Drug induced rhinitis Food Emotional Primary atrophic rhinitis Diagnostic Technique 1. History a. Exposure to specific allergen b. Nasal congestion, rhinorrhea, itching and sneezing c. Family history of allergy
Skin prick test may be performed for the following cases: Patients non-responsive to pharmacotherapy Patients with multiple target organ involvement Patients for hyposensitization Skin test are used to demonstrate an IgE mediated allergic reaction of the skin and represents the primary diagnostic tool in allergy. Radioallergosorbent test (RAST) and enzyme linked immunosorbent assay (ELISA) for some allergens have been shown to be as reliable as skin testing. Skin testing is less expensive, more sensitive, technically easier to perform and results can be interpreted immediately.
Idiopathic- better term than vasomotor rhinitis, presents with nasal hyperresponsiveness to non specific triggers such as strong smells(perfumes, bleach, solvents) irritants such as tobacco smoke, exhaust fumes and changes in environmental temperature and humidity. Exact mechanism is unknown Atrophic Rhinitis Chronic inflammation of the nose characterized by a progressive atrophy of the nasal mucosa and the turbinates resulting in widened nasal passages, excessive crusting and a foul odor(ozena and anosmia) Idiopathic:organisms implicated are Coccobacillus foctidus ozaena, Klebsiella ozeana Clinical picture: nasal obstruction, atrophied turbinates, excessive crusting and widened nasal cavity Therapy consists of buffered nasal saline irrigation twice daily and Vitamin A
Management of Allergic Rhinitis Allergen avoidance Pharmacotherapy o Topical and systemic anti histamines o Topical, nasal steroids and systemic steroids o Leukotriene receptor antagonist o +/- use of decongestants Immunotherapy
Pharmacotherapy of Allergic Rhinitis Antihistamines Classic Non or less sedating
Decongestant Oral Topical
A fun hazily snail barn aftermaster
Page 2
Corticosteroids Systemic Topical
Antihistamines Effects relieve pruritus prevent sneezing decrease thin secretions does not improve congestion
Mass cell stabilizers Inhaled Nasal Oral
Nasal Steroids suppress the inflammatory process and are effective in both the prevention and treatment of allergic rhinitis. They can provide effective control of all rhinitis symptoms
Anticholinergics Miscellaneous Mucolytics Montelukast
Anti- inflammatory Effects of Topical Nasal Steroids degree of inhibition of early phase reaction. Primary effect on suppression of late phase reaction Reduction of non-specific activity Inhibition of effect of cytokines
Other drug therapies have only a limited role in most patients. Allergens identification and avoidance can be helpful and other nasal disorders should always be excluded. Surgery may occasionally be needed where rhinitis is associated with a structural disorder of the nose. New Antihistaminic Characteristics Dosage once or twice daily Hepatic metabolism No drug tolerance with prolonged use Antihistamine activity equal to or better than classic antihistamines
The appropriate first choice for most patients with noninfective rhinitis is preventive therapy with a topical nasal steroid. The prevention of inflammation by steroid therapy is the best method of preventing the entire symptom complex of rhinitis. Intranasal corticosteroids are the most effective medications for treating the entire spectrum of allergic rhinitis symptoms. However, their use has been limited in children due to concerns about systemic side effect, including growth retardation.
Antihistamine Side Effect CNS Sedation (Diphenhydramine, Cetridine, Acrivastine, Ebastine at high doses) (non sedating antihistamines- Desloratadine, Fexofenadine, Loratadine) Loss of concentration Dizziness Insomnia Irritability Nervousness Tremors
Oral Bioavailability of Steroids Corticosteroids Mometasone furoate- 0.1% Fluticasone propionate- 1.0% Budesonide- 11% Beclomethasone dipropionate- 20% Flunisolide- 21% Triamcinolone- 23% Dexamethasone- 80% Rhinosinusitis Rhinosinusits is an inflammatory condition involving the paranasal sinuses, as well as the lining of the nasal passages. The most important factor in the pathogenesis of rhinosinusitis appears to be narrowing or obstruction of the sinus ostium.
Anticholinergics Dry mucous membrane Cardiac (palpitation, tachycardia) Blurred vision Constipation Dysuria impotence
(accdg. To Robert Davies) Antihistamines commonly relieve sneezing, itching and rhinorrhea in rhinitis but they have little or no effect on nasal blockade. They are not anti-inflammatory. They are used mainly in patients with mild intermittent rhinitis.
Bacterial Rhinosinusitis- Pathophysiology Viral URTI is the most common primary inciting cause Predisposing factors: o Allergic rhinitis o Nasal obstruction
A fun hazily snail barn aftermaster
Page 3
1.
2. -
3.
Pathophysiology: inflammation and accompanying edema formation leads to increase secretions which are retained in the sinuses due to impaired mucociliary clearance and obstruction of sinus ostia by edema; this leads to bacterial overgrowth Diagnosis In general, a diagnosis of acute bacterial rhinosinusitis (ABRS) may be made in adults with symptoms of a viral URTI that has not improved after 10 days or worsened after 5 to 7 days lasting up to 4 weeks Microorganisms of Acute Sinusitis
Duration of therapy for Acute Rhinosinusitis 7-14 day course Lack of response to therapy at > 72 hours is an arbitrary time established to define treatment failures If unresponsive tscan could be requested, pato medical management, CT scan may warrant Endoscopic sinus surgery
Chronic Rinusinusitis 1. Most common predisposing factor is an untreated or poorly treated acute rhinosinusitis usually of more than 3 months duration Other predisposing factors include trauma, structural deformities of the nose, allergy and presence of nasal polyps 16% of cultures- mixed infection with gram positive, gram negative and anaerobic organisms; most common organism is coagulase-negative Stapylococcus sp. Patients present with chronic nasal obstruction, chronic purulent foul smelling nasal and post nasal discharge. Symptoms are usually less severe than that of acute sinusitis Medical therapy consists of appropriate antibiotics (2-4) weeks and decongestants,mucolytic if warranted. Saline nasal irrigation and topical nasal steroid could be beneficial. No response warrants radiographic evaluation. E.g CT scan of osteomeatal complex. A referral to an Otorhinolaryngologist is advised. Endoscopic sinus surgery if indicated
Bacteria S. pneumonia- 31 H.influenza- 21% M.catarrhalis- 2% Anaerobes- 6% Staph. Aureus- 4% Staph Pyogenes- 2% Viruses Rhinoviruses Influenza virus Parainfluenza virus
2.
3.
4.
5. Acute Bacterial Rhinosinusitis 4. Symptoms include mucopurulent nasal aand post nasal discharge, congestion, pain and pressure, heaviness and tenderness over the sinuses, maxillary dental pain; rhiniscopy and endoscopy reveal purulent nasal discharge coating congested nasal mucosa Paranasal sinus series may reveal haziness, air fluid level or total opacification of the sinuses, but this is not routinely requested/ Therapy include appropriate antibiotics decongestants. Mucolytic and nasal saline irrigation when warranted. Antihistamines may be given if there is associated allergy.
6.
5.
Common Pathogens for Chronic Rhinosinusitis Coagulase negative Staph sp. (51%) S. aureus (20%) Anaerobes (3%) S. pneumonia (4%) On average, multiple organisms are found in 16% of cultures
6.
Recommended Antibiotic Therapy for ABRS Nasal Polyps No recent antimicrobial use (4-6 weeks) o Amoxicillin o Co-Amoxiclav(90mg/6.4 mg/kg per day) o Cefpodoxime proxetil o Cefuroxime axetil Use if patient is Beta-lactam allergic: o TMP-SMX o Doxycycline(among adults) o Azithromycin, Clarithromycin or erythromycin o Clindamycin o Levofloxacin, Moxifloxacin, Genfloxacin ( if not yet given among adults) Most common mass in the nasal cavity No definite etiology exist, however certain risk factors are associated with the condition: o Chronic infection o Allergies o Trauma o Metabolic disease o Aspirin intolerance Patients present with nasal obstruction, discharge and anosmia Rhinoscopy reveals presence of translucent, grayish white cystic masses
A fun hazily snail barn aftermaster
Page 4
Management is focused on the relief of symptoms 1. Management of nasal polyps is actually a spectrum between medical and surgical method with the ultimate aim of keeping the patient symptom free. Nasal steroids should now be given as first-line therapy to most patients with nasal polyp for 4-6 weeks A combination of topical and short term systemic steroid therapy can help improve symptoms thereby avoiding surgery. Antibiotics, mucolytics, decongestants may be given when there is evidence of rhinosinusitis Endoscopic sinus surgery, if signs and symptoms of sinusitis does not improve af adequate medical management.
2.
3.
4. 5.
Inverting Papilloma A unilateral bulky deep red to gray lateral nasal wall lesion which may appear like a polyp with gross translucency. Presents with unilateral nasal obstruction, epistaxis and post nasal drip Malignant transformation is considered to be less than 2% of cases develops squamous cell carcinoma. Histology shows epithelium of the lesion inverting into the underlying stroma. Management is complete excision via endoscopic sinus surgery or lateral rhinotomy with medial maxillectomy
Malignant Tumors of the Nose and Sinuses CA of the nose can present with nasal obstruction and nasal discharge and can be mistaken for rhinosinusitis. CA of the paranasal sinuses presents with one or more of the following; unilateral nasal obstruction, epistaxis, nasal mass, maxillary bulge, loose teeth, a bulging palate, diplopia and blurring of vision Maxillary CA is most common Radiographs will reveal radioopacity of the nose and sinus as well as bone destruction. Most common histopathologic picture is Squamous cell carcinoma Diagnosis: CT scan of the paranasal sinuses Biopsy: incisional via gingivo-buccal approach or biopsy of nasal extension Management: wide excision of the carcinoma or maxillectomy
*********************END OF LECTURE*************** *Disclaimer* The transcriber will not be liable for any errors or inconsistency in this trans. If there are wrong spellings sorry tao lang po me!eheheheh!- aftermaster
A fun hazily snail barn aftermaster
Page 5
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Print Vestibular ApparatusDocument2 pagesPrint Vestibular Apparatusspajda69No ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Gastric CancerDocument4 pagesGastric Cancerspajda69No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- ENT MidtermsDocument7 pagesENT Midtermsspajda69No ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- SkedDocument3 pagesSkedspajda69No ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- GIT Pathology - SurgPath 2013Document217 pagesGIT Pathology - SurgPath 2013spajda69No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Midterm Exam ENTDocument9 pagesMidterm Exam ENTspajda69No ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Day 2 Lung Plating 2011 Original in ClassDocument3 pagesDay 2 Lung Plating 2011 Original in Classspajda69No ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Causes of Semen Abnormalities Abnormal CountDocument3 pagesCauses of Semen Abnormalities Abnormal Countspajda69No ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- (Sheet Music - Piano) Mozart - Volodos - Turkish March Piano ScoreDocument13 pages(Sheet Music - Piano) Mozart - Volodos - Turkish March Piano ScoreIvanuska100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- My RecipesDocument9 pagesMy Recipesspajda69No ratings yet
- Case 11 AsthmaDocument131 pagesCase 11 Asthmaspajda69No ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Piano Level Requirements by Degree For Piano MajorDocument13 pagesPiano Level Requirements by Degree For Piano Majorspajda69100% (1)
- Tips PhotogDocument5 pagesTips Photogspajda69No ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Lightning Protection Measures NewDocument9 pagesLightning Protection Measures NewjithishNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Enrico Fermi Pioneer of The at Ted GottfriedDocument156 pagesEnrico Fermi Pioneer of The at Ted GottfriedRobert Pérez MartinezNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Ahmad Syihabudin: BiodataDocument2 pagesAhmad Syihabudin: BiodatabhjjqrgrwmNo ratings yet
- Stucor Qp-Ec8095Document16 pagesStucor Qp-Ec8095JohnsondassNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Group 2 ITI Consensus Report: Prosthodontics and Implant DentistryDocument9 pagesGroup 2 ITI Consensus Report: Prosthodontics and Implant DentistryEsme ValenciaNo ratings yet
- Changed Report 2015 PDFDocument298 pagesChanged Report 2015 PDFAnonymous FKjeRG6AFnNo ratings yet
- Dynalift Sed0804679lDocument1 pageDynalift Sed0804679lzaryab khanNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- ST3 ManualDocument48 pagesST3 ManualRon FosterNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- PNP Ki in July-2017 AdminDocument21 pagesPNP Ki in July-2017 AdminSina NeouNo ratings yet
- International Freight 01Document5 pagesInternational Freight 01mature.ones1043No ratings yet
- Java Complete Collection FrameworkDocument28 pagesJava Complete Collection FrameworkkhushivanshNo ratings yet
- Manual de Operacion y MantenimientoDocument236 pagesManual de Operacion y MantenimientoalexNo ratings yet
- Neet Question Paper 2019 Code r3Document27 pagesNeet Question Paper 2019 Code r3Deev SoniNo ratings yet
- Survivor's Guilt by Nancy ShermanDocument4 pagesSurvivor's Guilt by Nancy ShermanGinnie Faustino-GalganaNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- UFO Yukon Spring 2010Document8 pagesUFO Yukon Spring 2010Joy SimsNo ratings yet
- Ethical Conflicts in Psychology PDF DownloadDocument2 pagesEthical Conflicts in Psychology PDF DownloadAvory0% (2)
- MolnarDocument8 pagesMolnarMaDzik MaDzikowskaNo ratings yet
- Final MS Access Project Class-10Document17 pagesFinal MS Access Project Class-10aaas44% (9)
- What You Need To Know About Your Drive TestDocument12 pagesWhat You Need To Know About Your Drive TestMorley MuseNo ratings yet
- Verniers Micrometers and Measurement Uncertainty and Digital2Document30 pagesVerniers Micrometers and Measurement Uncertainty and Digital2Raymond ScottNo ratings yet
- The First Voyage Round The World by MageDocument405 pagesThe First Voyage Round The World by MageGift Marieneth LopezNo ratings yet
- Current Trends and Issues in Nursing ManagementDocument8 pagesCurrent Trends and Issues in Nursing ManagementMadhu Bala81% (21)
- Additional Article Information: Keywords: Adenoid Cystic Carcinoma, Cribriform Pattern, Parotid GlandDocument7 pagesAdditional Article Information: Keywords: Adenoid Cystic Carcinoma, Cribriform Pattern, Parotid GlandRizal TabootiNo ratings yet
- Tyler Nugent ResumeDocument3 pagesTyler Nugent Resumeapi-315563616No ratings yet
- Action ResearchDocument2 pagesAction ResearchGeli BaringNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Reflection On The PoorDocument5 pagesReflection On The Poorapi-347831792No ratings yet
- Advertisement: National Institute of Technology, Tiruchirappalli - 620 015 TEL: 0431 - 2503365, FAX: 0431 - 2500133Document4 pagesAdvertisement: National Institute of Technology, Tiruchirappalli - 620 015 TEL: 0431 - 2503365, FAX: 0431 - 2500133dineshNo ratings yet
- Environmental Science 13th Edition Miller Test BankDocument18 pagesEnvironmental Science 13th Edition Miller Test Bankmarykirbyifsartwckp100% (14)
- Republic of The Philippines Division of Bohol Department of Education Region VII, Central VisayasDocument6 pagesRepublic of The Philippines Division of Bohol Department of Education Region VII, Central VisayasJOHN MC RAE RACINESNo ratings yet
- Past Simple Vs Past ContinuousDocument3 pagesPast Simple Vs Past ContinuousNatalia SalinasNo ratings yet