Professional Documents
Culture Documents
145
Uploaded by
wiwi69Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
145
Uploaded by
wiwi69Copyright:
Available Formats
Adrenal Function and Alcoholism
I. Serum Cortisol
Jack H. Mendelson, MD,* Motoi Ogata, MD and Nancy K. Mello, PhD An increase in serum cortisol levels was found in alcoholic subjects during a period of 11-29 consecutive days of experimentally induced ethanol intoxication. Elevated serum cortisol levels were correlated with a progressive increase in blood alcohol levels, indicating a general dose response relationship. However, blood alcohol levels were influenced by factors other than the dose of alcohol ingested. Such factors included intercurrent gastrointestinal disorders and adequacy of dietary intake. Data obtained in this study demonstrate that chronic alcohol ingestion and its concomitant effects are associated with adrenal cortical activation in alcoholics.
The effects of chronic ethanol ingestion on adrenocortical function in man have not been determined. Studies of animals have shown that ethanol administration is associated with stimulation of adrenocortical secretion (1-4). These data also indicate that acute administration of ethanol induces a release of ACTH from the hypophysis. Czaja and Kalant (3) have emphasized that nonspecific stress factors, such as dose size and mode of ethanol administration, might be as significant in altering adrenocortical activity as the direct effects of ethanol are on pituitary adrenal function. Czaja and Kalant reported that intraFrom the National Center for Prevention antl Control of Alcoholism, National Institute of Mental Health, Chevy Chase, Md. Presented in part at the American Psychosomatic Society Annual Meeting, Boston, March 31, 1968. Received for publication May 15, 1970; revision received Oct 2, 1970. Address for reprint requests: Jack H. Mendelson, MD, Department of Psychiatry, Boston City Hospital, 818 Harrison Ave, Boston, Mass 02118. Professor of Psychiatry, Harvard Medical School; Director, Department of Psychiatry, Boston City Hospital, Boston, Mass 02118.
Psychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
peritoneal injection of ethanol, which produced rapid elevations of blood alcohol levels, induced adrenocortical stimulation as measured by acute changes in adrenal cholesterol and ascorbic acid levels. However, when equal doses of ethanol were administered to rats by stomach tube, adrenocortical activity appeared to be inhibited. In 1966, Ellis (4) reported data on the effects of acute ethanol administration on plasma 17-hydroxycorticosteroid (17OHCS) levels in dogs. Ellis' study differed from the work of previous investigators (1-3) in that he measured 17-OHCS directly, instead of inferring changes in adrenocortical function from determination of cholesterol or ascorbic acid concentration in the adrenal cortex. Ellis found that intravenous infusion of ethanol induced a significant elevation of plasma 17-OHCS levels; he demonstrated that this effect was not due to possible confounding variables such as repeated handling of animals, serial blood samples and volume of intravenous perfusate. Ellis also studied the effects of ethanol on
145
MENDELSON ET AL
plasma corticosterone levels in rat (5). He found an increase in plasma corticosterone levels when dosages of ethanol from 0.5 to 4.0 g/kg were administered intraperitoneally. There appeared to be a rough doseresponse relationship between amount of ethanol administered and degree of corticosteroid response. No elevation in corticosterone levels was observed when ethanol was given to hypophysectomized animals. Pretreatment of animals with pentobarbital or morphine produced a complete blockade of ethanol-induced steroid response. Ellis also found that repeated daily injections of ethanol during a 1-week period was not associated with a decreased steroid response, which would be expected if pituitary adrenal adaptation occurred. An attempt to assess adrenocortical function after chronic administration of ethanol to animals was carried out by Akabane and his associates (6). These investigators administered ethanol intraperitoneally once per day to animals for 7-63 consecutive days, in a dosage of 1.5 g/kg. They found a significant increase in adrenal weight and a significant reduction in cholesterol content after the period of chronic ethanol administration. These data suggest that chronic administration of ethanol produces a chronic stimulation of adrenocortical activity without evidence of an adaptational response. Five studies have been carried out in man in an attempt to assess effects of acute ethanol administration on adrenocortical function (7-11). Perman (8) measured urinary excretion of 17-OHCS in healthy young men after acute administration of ethanol in a dosage of 0.5-0.7 g/kg. He found no significant changes in urinary excretion of 17-OHCS after this moderate dose of alcohol. Krusius et al (7) measured plasma glucocorticoid levels in human subjects 2-4 hours after 5 ounces of beverage
146
alcohol were ingested. They found that ingestion of ethanol was not associated with evidence of adrenocortical stimulation. Kissin and his associates (9) measured plasma and urinary 17-hydroxycorticoids in both alcoholic and nonalcoholic subjects after acute administration of ethanol in a dosage of 1 ml (absolute) ethanol/kg body weight. These investigators found that after a single dose of ethanol was ingested, there was a diuresis associated with increased urinary 17-hydroxycorticoid output, and a decrease in plasma 17-OHCS levels. However, when subjects were given fluid supplementation with their alcohol dose, a rise in plasma 17-hydroxycorticoids was noted, and no change in urinary excretion of 17-OHCS occurred after acute ethanol administration. Merry and Marks (11) found that plasma-hydrocortisone levels increased in nonalcoholic individuals when their blood alcohol levels exceeded 100 mg/100 ml during experimental drinking conditions. However, alcoholics who had abstained for 3-6 weeks did not show this response. Jenkins and Connolly (10) measured serum cortisol directly after acute administration of ethanol to healthy men and women. They found that serum cortisol levels increased when blood alcohol values exceeded 100 mg/100 ml. They also found that 2 patients who had evidence of pituitary lesions failed to show an increase in cortisol levels after a high dose of ethanol. This finding suggested that ethanol effects on adrenal function were mediated via neural-pituitary pathways. The only published report of the effects of chronic ethanol administration on adrenocortical function in alcoholic and nonalcoholic subjects was the result of studies carried out in our laboratory in 1966 (12). In this study, 4 alcoholic and 4 nonalcoholic subjects were given 86-proof
Psychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
ADRENAL FUNCTION AND ALCOHOLISM
beverage alcohol in amounts equivalent to about 1 quart daily for 4 consecutive days. Alcohol was administered in a divided dosage every 4 hours, day and night. The nonalcoholic subjects developed gastrointestinal symptoms (nausea and vomiting) during ingestion of ethanol, and serum cortisol levels were elevated at this time. In alcoholic subjects, on the other hand, there were elevations of serum cortisol levels which were not specifically associated with g a s t r o i n t e s t i n a l disorders. The most marked elevations of serum cortisol levels occurred when alcoholic subjects developed withdrawal signs and symptoms after they had stopped drinking. Although these data indicated that ingestion of alcohol was associated with an increase in adrenocortical activity, the relatively short duration of the study (4 days) did not permit an examination of adrenal adaptive responses in alcoholics during long-term drinking. In addition, it appeared important to clarify further the relationship between ingestion of ethanol, gastrointestinal symptoms and alterations in serum cortisol levels. A need for long-term studies was also indicated by the claim of some investigators that chronic adrenocortical activation, associated with chronic ethanol ingestion, could result in eventual adrenocortical dysfunction (13-15). Since these investigators have advocated the use of ACTH or adrenocortical hormones in the treatment of alcoholism, because of possible ethanolinduced adrenal exhaustion, it appeared most important to assess the status of adrenocortical function in alcoholics who consumed alcohol under conditions analogous to real-life drinking episodes.
METHODS Four male alcoholics between the ages of 35 and 45 volunteered as subjects for this study. Each man
Psychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
reported a history of alcoholism of at least 5 years' duration. All men reported that they had experienced withdrawal signs and symptoms after they had stopped drinking. These volunteers were selected from a correctional institution where they had been incarcerated, and had not ingested alcohol for at least 60 days prior to the onset of this experiment. The subjects received complete physical and mental-status examinations at the correctional institution prior to their selection for the study. All were in good health and had no evidence of any major physical derangement. None reported any previous psychotic illness or drug addiction. No subject was using any form of medication at the time of the study. None had any evidence ol neurologic disease or seizure disorders; hepatic, renal, pulmonary cardiac or gastrointestinal disease; or nutritional or metabolic disorders. No subject showed any evidence of hepatic disease as measured by a bromsulphalein clearance test. The subjects were studied on a research ward, and had free access to a number of recreational facilities which included television, radio, reading material and group participation games. During the drinking phase of the experiment, at least one member of the research team was present at all times. Subjects were offered a well balanced diet which averaged 2000 calories/day. Dietary intake was recorded for each meal. Subjects were also given multivitamin capsules each morning. The experimental procedure was divided into three consecutive phases: (A) Predrtnktng phase. Physical, neurologic and mental-status examinations were carried out. In addition, measurements of social interaction parameters were obtained. Blood specimens were collected and analyzed. (B) Drinking phase. This was an 11-29 day period during which alcohol was administered. Alcohol was administered in the form of an 86-proof beverage mixture (bourbon) every 4 hours, day and night (2:00 PM, 6:00 PM, 10:00 PM, 2:00 AM, 6:00 AM, and 10:00 AM) . The subjects could ingest up to the equivalent of 4 g absolute alcohol/kg body weight/day. This amount is equivalent to 28 ounces of 43% beverage alcohol (86-proof) /day for a 70-kg man. The subjects were allowed to consume their alcohol with or without water or a carbonated beverage. They were allowed approximately 10-20 minutes to consume a single dose. 147
MENDELSON ET AL
fCJ Postdrlnklng phase. Assessments carried out during the predrinking and drinking phases were continued during this part of the experiment. Assessments of vital signs, caloric intake and weight were made daily. Blood alcohol levels were determined with a Breathalyzer.* The accuracy of the instrument was checked by comparing the readings with simultaneous blood alcohol levels determined by the enzymatic method of Bucher and Redetzki (16). The precision of the enzymatic technic had been established in previous experiments (17) in our laboratory (coefficient of variation less than 2% for concentrations of alcohol between 10 and 400mg/100cc) . Breathalyzer readings showed a mean variance of 10 mg% from simultaneous blood samples determined by the enzymatic method. Throughout the course of the experiment, blood specimens were obtained from each subject daily at 9:30 AM. These specimens were centrifuged shortly after collection, and the serum was removed and frozen for cortisol assay. Cortisol was determined by the technic described by Murphy et al (18) . This method is based on the cortisol-binding properties of plasma globulins. Cortisol C-14, added to unknown serum specimens or standards, is bound to binding sites in diluted normal plasma in proportion to the amount of total cortisol present in the sample. One cubic centimeter of serum was added to 19 cc normal saline and placed for 5 minutes in a boiling water bath. After the solution was cooled to room temperature. 0.02 /iC cortisol C-14-f- was added to each specimen. Dialysis sacks (cellulose casing % inch) , containing five 6-mm glass beads as weights and 5 cc normal plasma (diluted 1:8 with normal saline) , were placed into test tubes which contained the serum and C-14 cortisol. These tubes were then placed in a rotator (36 rpm) maintained at 6 C for 40 hours. Subsequently, 0.1 cc dialysate was pipetted from each sack into a Wheaton vial to which 1.00 cc hyamine hydroxide;} was added. Next, 5 cc scintillation fluid mixture, containing 0.6% PPO and 0.02% POP POP + in toluene and 03 cc absolute ethanol, was added to the vial. The samples were then counted in a Packard Tri-Carb Liquid Scintillation Spectrometer with a carbon-14 counting efficiency of 80%. Standard curves were Stephenson Corporation, Red Bank, NJ. f New England Nuclear Corporation, Boston, Mass. ^Packard Instrument Company, Downers Grove, 111. 148
constructed with known concentrations of crystalline hydrocortisone (Sigma) prepared in saline in dilutions of 0.05, 0.10, 0.1S, 0.20, 0.25 and 0.30<ug/cc. All determinations were carried out in duplicate. No significant quenching occurred in this system, as assessed by both the channels ratio and internal standard methods. RESULTS The data obtained in this study are presented in Fig 1-4. Serum cortisol values during the prealcohol phase were within the normal limits of values reported in the literature for healthy adult males (19, 20). A positive correlation was observed between ascending blood alcohol levels and increases in serum cortisol values for the 2 subjects studied in the 11-day alcohol administration experiment (Fig 1 and 2). In general, there was a good dose-response relationship for increases in blood alcohol concentrations, level of inebriation and progressive increases in serum cortisol values. When ethanol dosage was progressively decreased, a parallel decrease occurred in serum cortisol levels. As expected, this decrease was accompanied by a fall in serum alcohol levels and behavioral levels of intoxication. Subject GH (Fig 1) developed mild withdrawal symptoms and signs when his alcohol dosage was reduced. Peak serum cortisol levels were observed on the day when tremor and a memory deficit (a selective lacunar amnesia) occurred. This subject also reported gastrointestinal symptoms consisting of epigastric pain and nausea, and consequently decreased his food intake. After they had completely stopped drinking, subjects GH and WM (Fig 1 and 2) showed no evidence of withdrawal signs or symptoms, and serum cortisol levels tended to return to near baseline values. However, subject GH (Fig 1) showed a marked accentuation of serum cortisol levels 2 days prior
Psychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
ADRENAL FUNCTION AND ALCOHOLISM
Subject 6 H
ETOH INTAKE 0i/24h
15
17 21
CONSECUTIVE DAYS Fig 1. Serum cortisol levels during programmed ethanol administration.
to discharge from the study. During this time, he verbalized fear and apprehension about returning to his home and resuming his usual mode of spree drinking. Figures 3 and 4 present data on subjects who were permitted to drink for 27 and 29 days, respectively. Data obtained on these subjects demonstrate that high blood alcohol levels, or withdrawal signs and symptoms associated with a fall in blood alcohol, appeared to correlate more closely with elevations in serum cortisol levels
Psychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
than with the volume of ethanol consumed. The daily dosage of alcohol administered to these subjects was predicted, on the basis of their body weight, to be completely metabolized during a 24-hour interval. It can be observed, however, that both subjects achieved peak blood alcohol values only during certain phases of the experiment. Subject AR (Fig 3) showed two peaks during his drinking phase, even though ethanol dosage during the intervals be149
MENDELSON ET AL
32 28 24 20 CORTISOL M g / I O O ml 16 Subiecl WU
LEVEL OF INTOXICATION |0 o)
PULSE RATE / min
120 i IOOH 80 \60 L
ETOH INTAKE oz/24hr
9 13 17 21 25 CONSECUTIVE DAYS
29 33
Fig 2.
Serum cortisol levels during programmed ethanol administration.
tween these peaks was almost identical to the amount of alcohol he consumed when he showed high blood alcohol levels. These peak blood alcohol levels occurred when the subject reported gastrointestinal symptoms, consisting of nausea and epigastric pain. During the time the subject had these symptoms, his food intake was markedly reduced. Peak serum cortisol levels occurred for subject AR (Fig 3) in close temporal contiguity with his peak blood alcohol levels. Subject FP (Fig 4) also attained peak serum cortisol levels when blood alcohol
150
levels were high. This subject experienced gastrointestinal symptoms during the early phase of his alcohol-ingestion period and, similar to subject AR, he markedly reduced his food intake during this time. However, this subject continued to show elevated serum cortisol levels, even when blood alcohol levels and levels of inebriation were quite low. Subjects AR and FP (Fig 3 and 4) both experienced withdrawal symptoms and signs after they had stopped drinking. Although serum cortisol levels remained elevated for both subjects during the postalcoPsychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
ADRENAL FUNCTION AND ALCOHOLISM
Subject A R
PULSE RATE / mil
ETOH INTAKE
30 18
6
oz/24hr
17
21
25 DAYS
29
33
37
CONSECUTIVE
Fig 3. Serum cortisol levels during programmed ethanol administration.
hoi phase, these levels were not as high as those observed when blood alcohol levels were elevated. DISCUSSION The findings obtained in this study are in agreement with the data obtained in animal experimentsthat ethanol administration is associated with stimulation of adrenocortical secretory activity (1, 2, 4, 5). Moreover, our data corroborate the findings obtained by Ellis (5) in his studies of ratsthat a dose-response relationship exists between amount of ethanol adminisPsychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
tered and magnitude of the adrenocortical response. The lack of an adaptational response in man, as ethanol was administered throughout time, is consistent with the absence of adrenal adaptation in the rat after ethanol was repeatedly administered. Finally, there appears to be a similarity between the level of corticosterone response in the rat (the predominant adrenal steroid in these species) in relationship to blood alcohol levels and the magnitude of cortisol responses in man with similar blood ethanol levels. The mechanisms by which ethanol in151
MENDELSON ET AL
ETOH INTAKE oz/24hr
30[ 18
I I
I 5
I 9
I I I 13 17
I I I I I I I [ I I I I I 21 25 29 33 37 41 45 DAYS
CONSECUTIVE
Fig 4.
Serum cortisol levels during programmed ethanol administration.
duces elevated cortisol levels in alcoholics remain to be fully explored. Several possibilities may be mentioned. First, ethanol may induce enhanced secretion of corticotropin via activation of neural-pituitary circuits. No direct measurements of ACTH have been carried out after ethanol was administered to man or to animals. Animal studies indicate that hypophysectomized animals do not show an adrenocortical response after ethanol was administered (5). Similarly, human subjects with pituitary lesions do not have an increase in
152
serum cortisol levels after ethanol was administered (10). Thus, it is likely that ethanol stimulation of adrenocortical activity in man involves neural-pituitary mechanisms. Another factor which might account for the high levels of serum cortisol observed in alcoholics when they are drinking is a possible impairment in the catabolism of cortisol. It is known that the major site for catabolism of cortisol is the liver (21). Assessment of hepatic function in the subjects studied in our laboratory revealed no eviPsychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
ADRENAL FUNCTION AND ALCOHOLISM
dence of acute or chronic liver disease. Bromsulphalein tests prior to, during and after drinking were well within normal limits. No other evidence of impaired hepatic function, as determined by physical examination and laboratory tests for serum protein, electrolytes and SGOT levels, was detected during any phase of this study. However, it should be emphasized that these tests only assess hepatic reserve and absence of acute pathophysiologic processes. Therefore, it is possible that cortisol catabolism could be impaired even though other aspects of hepatic function appear normal. Margraf and his associates (22) found a diminished adrenocortical response, as determined by measurement of free and conjugated plasma 17-hydroxycorticosteroids in alcoholics after surgery. Assessment of cortisol secretion rate and excretion of total 17-hydroxycorticosteroids indicated that adrenocortical function in these alcoholic patients was not impaired. However, excretion of THE, THF and allo-THF cortisol metabolites was significantly decreased. These findings suggest that alterations in cortisol metabolism, rather than a disorder of adrenocortical function, existed in the alcoholic patients. Margraf and his colleagues did not examine the effects of ethanol ingestion on adrenocortical activity or steroid metabolism. However, Admirand et al (23) reported that ingestion of relatively small quantities of ethanol is associated with a four- to fivefold increase in 17-/3 hydroxysteroid sulfates in human plasma. They postulated that this was due to an ethanol-induced increase in hepatic NADH which, in turn, enhanced reductive catabolism of 17-ketosteroid sulfates. In the paper which follows, we discuss the significance of ethanol-induced shift in catecholamine metabolism, from oxidative to reductive pathways (24).
Psychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
Data obtained in this study indicate that the highest serum cortisol values were observed when subjects developed gastrointestinal symptoms during drinking, and when these symptoms were associated with decreased food intake. Decreased food intake per se may not account for these observations, since studies of the effects of fasting on adrenocortical activity reveal little or no effect of food deprivation on the secretion or metabolism of cortisol in man (25). It is also unlikely that the physical discomfort associated with gastrointestinal symptoms induces an increased degree of adrenocortical secretion, since Bush (25) has pointed out: "It is probable that very severe burns, and large doses of certain agents such as bacterial pyrogens, histamine, and peptones, cause a brisk release of ACTH, that is independent of any emotional concomitants; but it is extremely doubtful whether any of the physical stimuli which are commonly supposed to be 'stresses' are effective in causing the increased secretion of ACTH at all. Thus, severe exercise, cold, and fasting produce little or no effect on the secretion and metabolism of cortisol in man unless they are part of a situation that provokes emotion. On the other hand, strong emotion in the absence of any recognizable physical stimuli or 'stresses' regularly causes maximal increases in the secretion rate of cortisol and its concentration in peripheral blood." Although fasting or pain per se, associated with gastrointestinal disorders, may not induce an increased secretion of cortisol from the adrenal cortex, the emotional significance of these phenomena may be an effective stressor. For example, if the alcoholic perceives gastrointestinal disturbances as the heralding symptom which may prevent him from drinking in the near future, this may be an aversive emotional,
153
MENDELSON ET AL
as well as physical, stimulus. Perhaps a more parsimonious interpretation of the interacting efEects of gastrointestinal symptoms, lack of food intake and serum cortisol levels relates to the effects of food intake on ethanol metabolism. A number of studies with experimental animals have shown that decreased food intake or starving results in a decreased rate in the metabolism of ethanol (26, 27). Recent data obtained in our laboratory strongly support a correlation between decreased caloric intake from food sources other than ethanol, and a decrease in the rate of ethanol metabolism (28). In the present study, a good correlation was found between decreased food intake associated with gastritis, and an elevation in blood alcohol levels. The low blood alcohol levels shown by GH (Fig 1) during an initial period of gastritis probably reflect the comparatively low alcohol dosage and the fact that food intake remained stable. Since good dose-response relationships appeared to occur between blood ethanol levels and serum cortisol values, the sequential effects of decreased food intake on adrenocortical function in alcoholics when they are drinking are as follows: (a) gastrointestinal symptoms result in decreased food intake; (b) decreased food intake causes a lower rate of ethanol metabolism, probably via decreased regeneration of NAD from NADH in hepatic tissue; and (c) increased blood alcohol levels progressively stimulate increased cortisol secretion from the adrenal cortex via neural-pituitary activation. It is more difficult to differentiate the direct effects which ethanol may have on neural and pituitary mechanisms from the derivative peripheral adrenal effects which may occur as a concomitant of chronic drinking. Observations carried out in our laboratory (29) and in our studies of others (30) indicate that, contrary to popular be154
lief, chronic ethanol intake by the alcoholic is associated with a progressive dysphoric state, rather than alleviation of dysphoria. As the alcoholic continues to drink, he tends to become more anxious and depressed. This rather paradoxical affective change casts some doubt upon those hypotheses which primarily stress that alcohol is consumed by alcoholics to reduce aversive or unpleasant life situations. Hamburg (31) has pointed out that "the extensive research of the past decade on adrenocortical function in man in naturally occurring and experimental stress situations has provided substantial evidence of significantly increased secretory activity of the adrenal cortex under these conditions." The finding that alcoholics become progressively more anxious during drinking, and also concomitantly show elevations in serum cortisol levels, would support the notion that alcohol plays a role in inducing or exacerbating emotional stress reactions during chronic alcohol ingestion and after alcohol withdrawal. It is also possible that increased adrenocortical activity, associated with chronic drinking, may be significant in modifying those physiologic processes which determine metabolic tolerance for ethanol. The role of the glucocorticoids in affecting carbohydrate metabolism is well known, and the role of carbohydrate metabolism in the regulation of ethanol metabolism may be of primary rate-limiting significance. It is known that the glucocorticoids may act to modify the activity of a number of enzymes involved in the metabolism of a variety of endogenous and exogenous substrates (32). While there is no direct evidence that cortisol affects the activity of hepatic alcohol dehydrogenase or aldehyde dehydrogenase, it is possible that enhanced activities of these enzymes could be mediated by an increase in circulating levels of cortisol.
Psychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
ADRENAL FUNCTION AND ALCOHOLISM
There is also some evidence that adrenocortical hormones may be of importance in the degree of adaptation or centralnervous-system tolerance for ethanol. Rikimaru (33) has shown that in adrenalectomized rats, loss of the righting reflex and postataxic period was significantly prolonged after ethanol was administered, when compared with nonadrenalectomized animals. He also showed that administration of cortisone to adrenalectomized animals, which were given alcohol, reduced the duration of loss of the righting reflex and the postataxic period. Finally, he observed that adrenalectomized rats metabolized ethanol at a lower rate than did the nonadrenalectomized animals, and that treatment with cortisone reversed this effect. Kakihana and her associates (34) have found a correlation between the magnitude of plasma corticosterone response after ingestion of ethanol and the level of behavioral tolerance to ethanol in strains of mice which show different degrees of tolerance for ethanol, as assessed by behavioral technics. Those animals which appear to have the greatest tolerance for ethanol showed the highest plasma corticosterone response after ethanol administration. These data together suggest that the effects of ethanol on animal behavior may be significantly related to the responsiveness of the pituitary adrenal axis to ethanol. The possible effects of increased serum cortisol levels on adrenal medullary and adrenergic hormonal functions in alcoholics during experimentally induced intoxication and withdrawal are discussed in the paper which follows (24). The findings obtained in this study are consistent with previous data, obtained in our laboratory, on changes in serum cortisol levels during short-term alcohol ingestion by alcoholic subjects (12). In the shortterm studies, gastrointestinal symptoms ocPsychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
curred less frequently, and peak blood alcohol levels tended to be lower than during the current experiment. However, when gastrointestinal illness and decreased food intake occurred in the short-term studies, marked elevations of serum cortisol levels were noted. The short-term studies carried out in our laboratories did not permit evaluation of either adaptation, or a possible exhaustion of the adrenocortical response during chronic drinking. The findings obtained in this study indicate that neither adrenocortical adaptation nor exhaustion occurred after prolonged ingestion of alcohol. Our data do not indicate that adrenocortical steroids would be of therapeutic value in a case of acute alcohol intoxication or alcohol withdrawal.
SUMMARY
Serum cortisol levels were determined in 4 alcoholic subjects prior to, during and after a period of experimentally induced ethanol intoxication. Alcoholic subjects were allowed to consume beverage alcohol in a dosage equivalent to 4 g absolute alcohol/kg body weight (for a 70-kg man)/ day for 11-29 consecutive days. Elevations in serum cortisol levels paralleled increases in blood alcohol levels, and a rough doseresponse relationship occurred. Blood alcohol levels and degree of intoxication were not solely dependent on the amount of ethanol ingested. When subjects developed gastrointestinal symptoms and decreased food intake, there were marked accentuations in blood alcohol levels. It is concluded that ethanol induces an increased secretion of cortisol from the adrenal cortex, and that this response to ethanol is probably mediated via neural-pituitary mechanisms. No evidence of adaptation or exhaustion of cortisol response was found during drinking or after alcohol withdrawal.
155
MENDELSON ET AL
REFERENCES 1. Smith JJ: The effect of alcohol on the adrenal ascorbic acid and cholesterol of the rat. J Clin Endocr 11:792, 1951 2. Forbes JC, Duncan GM: Effects of alcohol intoxication and ACTH on liver ascorbic acid in guinea pig. Endocrinology 55:822, 1954 3. Czaja C, Kalant H: The effect of acute alcoholic intoxication and adrenal ascorbic acid and cholesterol in the rat. Canad J Biochem Physiol 39:327, 1961 4. Ellis FW: Adrenal cortical function in experimental alcoholism in dogs. Proc Soc Exp Biol Med 120:740, 1965 5. Ellis FW: Effect of ethanol on plasma corticosterone levels. J Pharmacol Exp Ther 153:121, 1966 6. Akabane J, Nakanishi S, Kohei H, et al: Responses of the adrenal cortex to longterm administration of alcohol and acetaldehyde. Med J Shinshu Univ 9:59, 1964 7. Krusius FE, Vartia KO, Forsander O: Ex perimentelle studien uber die biologische wirkung von alkohol. 2. Alkohol und nebennierenrinden-funktion. Ann Med Exp Fenn 36:424, 1958 8. Perman ES: Observations on the effect of ethanol on the urinary excretion of histamine, 5-hydroxyindole acetic acid, catecholamines and 17-hydroxycorticosteroids in man. Acta Physiol Scand 51:62, 1961 9. Kissin B, Schenker V, Schenker AC: The acute effect of ethanol ingestion on plasma and urinary 17-hydroxycorticoids in alcoholic subjects. Amer J Med Sci 239:690, 1960 10. Jenkins JS, Connolly J: Adrenocortical response to ethanol in man. Brit Med J 2: 804, 1968 11. Merry J, Marks V: Plasma-hydrocortisone response to ethanol in chronic alcoholics. Lancet 1:921, 1969 12. Mendelson JH, Stein S: Serum cortisol levels in alcoholic and nonalcoholic subjects during experimentally induced ethanol intoxication. Psychosom Med 28:616, 1966 13. Lovell HW, Tintera JW: Hypoadrenocorricism in alcoholism and drug addiction. 156
Geriatrics 6:1, 1951 14. Smith JJ: The treatment of acute alcoholic states with ACTH and adrenocortical hormones. Quart J Stud Alcohol 11:190, 1950 15. Feldman DJ, Zucker HD: Present-day medical management of alcoholism. JAMA 153: 895, 1953 16. BucherT, Redetzki H: Eine spezifische photometrische bestimmung von ethylalkohol auf fermentativem wege. Klin Wschr 29: 615, 1951 17. Mendelson JH, La Dou J: Experimentally induced chronic intoxication and withdrawal in alcoholics. Part 1. Background and experimental design. Quart J Stud Alcohol: Suppl 2:1-13, 1964 18. Murphy BP, Engelberg W, Pattee CJ: Simple method for the determination of plasma corticoids. J Clin Endocr 23:293, 1963 19. Bliss EL, Sandberg AA, Nelson DH, et al: The normal levels of 17-hydroxycorticosteroids in the peripheral blood of man. J Clin Invest 32:818, 1953 20. Silber RM, Porter CC: The determination of 17, 21-dihydroxy 20-ketosteroids in urine and plasma. J Biol Chem 210:923, 1954 21. Rosenfeld RS, Fukushima DK, Gallacher TF: Metabolism of adrenal cortical hormones, The Adrenal Cortex. Edited by AB Eisenstein. Boston, Little, Brown & Co, 1967 22. Margraf HW, Moyer CA, Ashford LE, et al: Adrenocortical function in alcoholics. J Surg Res 7:55, 1967 23. Admirand WH, Cronholm J, Sjovall J: Ethanol and steroid metabolism. Clin Res 18:126, 1970 24. Ogata M, Mendelson JH, Mello NK: Adrenal function and alcoholism. II. Catecholamines. Psychosom Med 33:159, 1971 25. Bush IE: Chemical and biological factors in the activity of adrenocortical steroids. Pharmacol Rev 14:317, 1962 26. Smith ME, Newman HW: The rate of ethanol metabolism in fed and fasting animals. J Biol Chem 234:1544, 1959 27. Forsander OA, Raiha N, Salaspuro M, et al: Influence of ethanol on the liver metaboPsychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
ADRENAL FUNCTION AND ALCOHOLISM
lism of fed and starved rats. Biochem J 94: 259, 1965 28. Mello NK, Mendelson JH: The effects of prolonged alcohol ingestion on the eating, drinking, and smoking patterns of chronic alcoholics. 1969 (in preparation) 29. McNamee HB, Mello NK, Mendelson JH: Experimental analysis of drinking patterns of alcoholics: concurrent psydiiatric observations. Amer J Psychiat 124:1063, 1968 30. Nathan PE, Titler NA, Lowenstein LM, et al: Behavioral analysis of chronic alcoholism: interaction of alcohol and human contact. Presented at the annual meetings of the Eastern Psychological Association, April, 1969
31. Hamburg DA: Genetics of adrenocortical hormone metabolism in relation to psychological stress, Behavior Genetic Analysis. Edited by J Hirsch, New York, McGraw Hill, 1967 32. Ashmore J, Morgan D: Metabolic effects of adrenal glucocorticoid hormones, The Adrenal Cortex. Edited by AB Eisenstein. Boston, Little, Brown & Co, 1967 33. Rikimaru MT: The role of the adrenal in the pharmacological effects of ethanol. Diss Abstr 28:5141-B, 1968 34. Kakihana R, Noble EP, Butte JC: Corticosterone response to ethanol in inbred strains of mice. Nature 218:360, 1968
Psychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
157
DUKE UNIVERSITY RESEARCH TRAINING PROGRAM
The Duke University Center for the Study of Aging and Human Development announces a 2-year research training program. The focus of the program will be on independent work in the Behavioral Sciences and Psychophysiology in close collaboration with faculty members. Individual planning for specific interests will be emphasized in conjunction with a series of seminars. The training is designed to provide the participant with specific skills in a specialized area within the spectrum of the life sequence, in order that he may achieve independent status as an investigator. Applicants should have completed the requirements for the PhD or MD degree. A background in Psychology, Sociology, Economics, Pediatrics, Obstetrics and Gynecology, Medicine, Psychiatry or Psychophysiology is preferred. Stipends will be determined according to the professional background of the applicant. Applicants are now being considered for July 1, 1971. For additional information and applications, please contact Carl Eisdorfer, PhD, MD, Director of Training.
158
Psychosomatic Medicine, Vol. 33, No. 2 (March-April 1971)
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Ceasarean Case StudyDocument26 pagesCeasarean Case StudyNarissa Jay Taub YlananNo ratings yet
- Topic 9.2 Graded QuizDocument8 pagesTopic 9.2 Graded QuizTran WinnerNo ratings yet
- Berat Badan Lahir Rendah (BBLR) Dengan Kejadian Stunting Pada Anak Usia 6-24 BulanDocument3 pagesBerat Badan Lahir Rendah (BBLR) Dengan Kejadian Stunting Pada Anak Usia 6-24 BulanPuskesmas BabatanNo ratings yet
- Pharmacology Workbook 101Document5 pagesPharmacology Workbook 101ryanbucoNo ratings yet
- Dental BiofilmsDocument44 pagesDental BiofilmsRamona MateiNo ratings yet
- Beta 2 AgonistsDocument198 pagesBeta 2 AgonistsLeonardo FerreiraNo ratings yet
- The Mechanism Isorhythmic: of Synchronization A-VDocument11 pagesThe Mechanism Isorhythmic: of Synchronization A-VSheila AdiwinataNo ratings yet
- How Do Magnets WorkDocument9 pagesHow Do Magnets WorkDelNo ratings yet
- MyxedemaDocument3 pagesMyxedemaBobet ReñaNo ratings yet
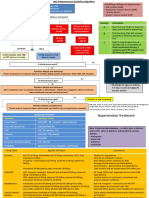
- General Population (No Diabetes or CKD) Diabetes or CKD PresentDocument2 pagesGeneral Population (No Diabetes or CKD) Diabetes or CKD PresentLalu Ranova100% (1)
- Cataract Case PresentationDocument7 pagesCataract Case PresentationShahbaz AAnsariNo ratings yet
- DrowningDocument22 pagesDrowningNovie GarillosNo ratings yet
- EUOGS OSCE Booklet 2020Document26 pagesEUOGS OSCE Booklet 2020Amanda Leow100% (1)
- Biochemical Composition of Normal Urine: Nature Precedings November 2011Document55 pagesBiochemical Composition of Normal Urine: Nature Precedings November 2011novi rahmawatiNo ratings yet
- Scenar Testimonials (Updated)Document10 pagesScenar Testimonials (Updated)Tom Askew100% (1)
- Vox Sanguin Mei 2021Document159 pagesVox Sanguin Mei 2021rsdarsono labNo ratings yet
- Self Learning Module Unit 4 Maternal ConceptsDocument36 pagesSelf Learning Module Unit 4 Maternal ConceptsTherese Margarette SantiagoNo ratings yet
- Diseases of The Newborn Part1Document2 pagesDiseases of The Newborn Part1sarguss14No ratings yet
- TB Caravan GuideDocument22 pagesTB Caravan GuideMajo Napata100% (1)
- Toxic Epidermal NecrolysisDocument13 pagesToxic Epidermal NecrolysisHend AbdallaNo ratings yet
- Case Presentation On Wilms TumorDocument25 pagesCase Presentation On Wilms TumorDeepika100% (1)
- Fluid Balance Case StudyDocument9 pagesFluid Balance Case StudyAna BienneNo ratings yet
- Knee Assessement FormDocument2 pagesKnee Assessement FormLee Woo GuanNo ratings yet
- Mean Alt Üst SD Range Mean Alt Üst SD Range Mean Alt Üst SD Mean Alt Üst SD FaktörDocument5 pagesMean Alt Üst SD Range Mean Alt Üst SD Range Mean Alt Üst SD Mean Alt Üst SD FaktörZeynep DenizNo ratings yet
- Open Book FractureDocument31 pagesOpen Book FractureMUHAMMAD ADLI ADNAN BIN JAMIL STUDENTNo ratings yet
- Pancreatic Hormones and Anti Diabetic Drugs NotesDocument8 pagesPancreatic Hormones and Anti Diabetic Drugs NotesBrunette CesaNo ratings yet
- Toxicology-Handbook PDFDocument2 pagesToxicology-Handbook PDFssb channelNo ratings yet
- Incentive SpirometerDocument25 pagesIncentive SpirometerAnalyn Salvacion100% (2)
- Module 6 Gram Staining PreLabDocument24 pagesModule 6 Gram Staining PreLabcloudNo ratings yet
- Preterm Labour and Birth PDF 1837333576645Document28 pagesPreterm Labour and Birth PDF 1837333576645Rocky.84No ratings yet