Professional Documents
Culture Documents
Chapter 19c
Uploaded by
aexillisOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 19c
Uploaded by
aexillisCopyright:
Available Formats
1/9/2013
Anatomic Structures Controlling Heart Activity: The Hearts Conduction System
Automaticity of the heart
Heart pumping blood continuously Dependent upon rhythmic stimulation of cardiac muscle cells Precise electrical events initiated by conduction system Begin with stimulation by pacemaker Transmission of action potential by conduction fibers Ensures atria contracts prior to ventricles
Anatomic Structures Controlling Heart Activity: The Hearts Conduction System
Conduction system
Specialized cardiac muscle cells Initiate and conduct electrical signals Sinoatrial (SA) node
in posterior wall of right atrium adjacent to superior vena cava initiates heartbeat referred to as pacemaker of heart
Anatomic Structures Controlling Heart Activity: The Hearts Conduction System
Conduction system (continued)
Atrioventricular (AV) node
in floor of right atrium between right AV valve and coronary sinus opening
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Figure 19.14a
Sinoatrial (SA) node (pacemaker) Right atrium Atrioventricular (AV) node Right and left bundles Purkinje fibers Purkinje fibers
Atrioventricular (AV) bundle
extends from AV node though interventricular septum divides into left and right bundles
Purkinje fibers
extend from left and right bundles from apex of heart through walls of ventricles
Atrioventricular (AV) bundle
(a) Conduction system
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Anatomic Structures Controlling Heart Activity: The Hearts Conduction System Why is the SA node referred to as the pacemaker?
The SA node initiates the signal of the heartbeat.
Conduction system
Conduction system
Electrical activity initiated at SA node Action potential transmitted through conduction system
Figure 19.15a
SA node
Initiation SA node initiates action potential.
Nodal cell
2 Spread of action potential An action potential is propagated throughout the atria, the conduction system.
(a)
1/9/2013
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Cardiac muscle cells
Cardiac muscle cells
Action potential spreads across sarcolemma of cardiac muscle cells First in atria, then in ventricles
Figure 19.15b
1 The action potential initiated in the conduction system is propagated across the sarcolemma of cardiac muscle cells.
Action potential
Cardiac muscle cell
Stimulation of the HeartElectrical Events at the SA Node: Initiation of the Action Potential
Autorhythmicity
Depolarize and fire action potential spontaneously Exhibited by SA nodal cells Depends on a series of events within SA nodal cells
Sarcolemma
2 Muscle contraction Thin filaments slide past thick filaments and sacromeres shorten within cardiac muscle cells. Sarcomeres shorten. (b)
Stimulation of the HeartElectrical Events at the SA Node: Initiation of the Action Potential
Events occurring in SA nodal cells
1) Reaching threshold
opening of slow voltage-gated Na+ channels Na+ flow into nodal cells membrane potential from -60 mV to -40 mV (threshold value)
Stimulation of the HeartElectrical Events at the SA Node: Initiation of the Action Potential
Events occurring in SA nodal cells (continued)
3) Repolarization
closure of calcium channels opening of voltage-gated K+ channels K+ flowing out membrane potential back to resting membrane potential (-60 mV) triggers reopening of voltage-gated Na+ channels
begins process again
2) Depolarization
opening of fast voltage-gated Ca2+ channels triggered entry of Ca2+ into cell membrane potential from -40 mV to just above 0 mV
Figure 19.16b
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Stimulation of the HeartElectrical Events at the SA Node: Initiation of the Action Potential
Heart rate
Process takes about 0.8 sec = HR 75 beats/min Inherent rhythm faster at 100/min Slower rate due to continuous parasympathetic stimulation
by vagus nerve this slowing of heart rate, vagal tone
+10 0 Membrane potential (mV) 10 20 30 40 50 60 70 1
RMP Pacemaker potential
2 3
Threshold voltage Action potential
1 Reaching threshold Slow voltage-gated Na+ channels open. Inflow of Na+ changes membrane potential from 60 mV to 40 mV. 2 Depolarization Fast voltage-gated Ca2+ channels open. Inflow of Ca2+ changes membrane potential from 40 mV to just above 0 mV. 3 Repolarization Fast voltage-gated Ca2+ channels close. Voltage-gated K+ channels open allowing K+ outflow. Membrane potential returns to RMP 60 mV, and K+ channels close.
0.4
0.8
1.2
1.6
Time (seconds) (b)
1/9/2013
Stimulation of the HeartElectrical Events at the SA Node: Initiation of the Action Potential
Comparison of Cardiac Nodal Cells and Neurons
Nodal cells
do not require stimulation (unlike neurons) do not have stable resting membrane potential (RMP) RMP gradually increasing to threshold without stimulation termed pacemaker potential depolarization occurs with entrance of Ca2+ into cells (unlike neurons)
Stimulation of the HeartConduction System of the Heart: Spread of the Action Potential
Action potential through conduction system
1) Action potential distributed throughout atria
relayed to AV node spread through gap junctions allows for almost instantaneous excitation of muscle cells atria contracting at same time
Stimulation of the HeartConduction System of the Heart: Spread of the Action Potential
Action potential through conduction system (continued)
2) Action potential delayed at the AV node
AV nodal cells with smaller fiber diameter and fewer gap junctions slows conduction rate with fibrous skeleton, only moves through AV node delay allows atria to finish contracting force blood into ventricles before ventricular contraction
Stimulation of the HeartConduction System of the Heart: Spread of the Action Potential
Action potential through conduction system (continued)
3) Action potential moving from AV node
moves along AV bundle moves to Purkinje fibers
4) Spreads throughout ventricles via gap junctions
begin to contract within 120 to 200 ms after firing of SA nodal cells
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Sinoatrial node and atrial myocardium 1 An action potential is generated at the sinoatrial (SA) node. SA node It spreads via gap (pacemaker) junctions between cardiac muscle cells throughout the atria AV node to the atrioventricular (AV) node. 3 The AV bundle conducts the action potential along the left and right bundle branches to the Purkinje fibers.
Bundle branches and Purkinje fibers
Atria
AV bundle
Figure 19.17
Figure 19.17 (continued)
Left and right bundle branches Purkinje fibers
Atrioventricular (AV) node 2 The action potential is delayed at the AV node before it passes to the AV bundle within the interventricular septum. AV node 4 The action potential is spread via gap junctions between cardiac muscle cells throughout the ventricles.
Ventricular myocardium
Purkinje fibers AV bundle Ventricles
1/9/2013
Stimulation of the HeartConduction System of the Heart: Spread of the Action Potential
Specialized Features Associated with Ventricles
Purkinje fibers larger in diameter than other cardiac fibers
action potential extremely rapid ensures ventricles contract at same time
Stimulation of the HeartConduction System of the Heart: Spread of the Action Potential What is the path of an action potential through the conduction system of the heart?
SA node, AV node, AV bundle, Purkinje fibers, through ventricles
Papillary muscles stimulated to contract immediately
muscles anchor chordae tendinae to AV cusps start to pull on cusps just prior to increase in pressure in ventricles
Stimulation beginning at heart apex
ensures blood efficiently ejected toward arterial trunks
Stimulation of the HeartConduction System of the Heart: Spread of the Action Potential
Clinical View: Ectopic Pacemaker
Pacemaker other than SA node Conduction system cells other than SA node
also have ability to spontaneously depolarize depolarize at slower rates than SA node
Stimulation of the HeartConduction System of the Heart: Spread of the Action Potential
Clinical View: Cardiac Arrhythmia
Abnormality in the rate, regularity, or sequence of cardiac cycle Atrial flutter
atria attempting to contract at 200-400 times per minute may persist for many years may degenerate into atrial fibrillation
AV node the default pacemaker if SA node impaired
AV node with inherent rhythm of 40 to 50 beats/min fast enough to sustain life
Atrial fibrillation
action potential more chaotic irregular heart rate may lead to serious disturbance in rhythm
Cardiac muscle with rate of 20 to 40 beats/min
usually too slow to sustain life
Stimulation of the HeartConduction System of the Heart: Spread of the Action Potential
Clinical View: Cardiac Arrhythmia (continued)
Premature ventricular contractions
result from stress, stimulants, or sleep deprivation abnormal action potential within AV node or ventricles not detrimental unless they occur in large numbers
Cardiac Muscle Cells: Repolarization and the Refractory Period
Skeletal and cardiac excitation similarities
Both with refractory period
time after depolarization when muscle cannot be restimulated
Ventricular fibrillation
life-threatening arrhythmia rapid, repetitious movement of ventricular muscle contractions not coordinated; heart unable to pump cardiac arrest shock applied to synchronize hearts electrical activity
Both with depolarization and repolarization Both with muscle contraction and relaxation Both with lag time between action potential and contraction
1/9/2013
Cardiac Muscle Cells: Repolarization and the Refractory Period
Skeletal and cardiac excitation differences
Refractory period longer in cardiac cells
has extended plateau phase needs resting membrane potential for restimulation 250 ms compared to 1-2 ms makes sustained contraction impossible in cardiac cells allows heart to always contract and relax and continue pumping
Cardiac Muscle Cells: Repolarization and the Refractory Period What is the significance of the extended refractory period in cardiac muscle?
It ensures sustained contraction does not occur (which might cause the heart to stop pumping).
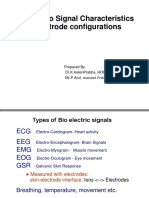
Cardiac Muscle Cells: The ECG Recording
Electrocardiogram (ECG/EKG)
Monitoring electrodes attached to skin
at wrist, ankles, and chest locations
Cardiac Muscle Cells: The ECG Recording
Waves and Segments
Has three principle deflections P wave
reflects electrical changes of atrial depolarization originates in SA node
Electrical signals collected and charted Provides assessment of electrical changes of heart Provides composite tracing of all cardiac action potentials Utilized during routine physical exam
QRS complex
electrical changes associated with ventricular depolarization atria simultaneously repolarizing but masked by above
T wave
electrical change associated with ventricular repolarization
Cardiac Muscle Cells: The ECG Recording
Waves and Segments (continued)
Two segments between waves
no electrical change
Cardiac Muscle Cells: The ECG Recording
Intervals
Two intervals P-R interval
period from beginning of P wave to beginning of QRS deflection atrial depolarization to beginning of ventricular depolarization time to transmit action potential through entire conduction system
P-Q segment
associated with atrial plateau at sarcolemma cardiac muscle cells within atria contracting
S-T segment
ventricular plateau cardiac muscle cells in ventricle contracting
Q-T interval
time from beginning of QRS and end of T wave from ventricular depolarization to repolarization interval depends upon heart rate
1/9/2013
Figure 19.20a
Cardiac Muscle Cells: The ECG Recording
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
R P-Q segment S-T segment
What events in the heart are indicated by each of the following: P wave, QRS complex, and T wave?
T P T Q
Q S P-R interval
S Q-T interval
P wave: atrial depolarization QRS complex: ventricular depolarization T wave: ventricular repolarization
QRS complex (a)
Cardiac Muscle Cells: The ECG Recording
Clinical View: Heart Blocks
Involve impairment within hearts conducting system May result in syncope (fainting), irregular heartbeats, and palpitations First-degree AV block
lengthened PR interval action potential slowed between atria and ventricles asymptomatic
Cardiac Muscle Cells: The ECG Recording
Clinical View: Heart Blocks (continued)
Second-degree block
exists along path between atria and ventricles failure of some action potentials to be conducted to ventricles
Third-degree block
complete heart block no action potentials from SA node received by ventricles life-threatening
You might also like
- Blood Pressure - Short-Term Regulation of Blood PressureDocument3 pagesBlood Pressure - Short-Term Regulation of Blood PressureaexillisNo ratings yet
- Blood Pressure - Short-Term Regulation of Blood PressureDocument3 pagesBlood Pressure - Short-Term Regulation of Blood PressureaexillisNo ratings yet
- Chapter 19d NewDocument20 pagesChapter 19d NewaexillisNo ratings yet
- Chapter 19aDocument5 pagesChapter 19aaexillisNo ratings yet
- Chapter 20aDocument7 pagesChapter 20aaexillisNo ratings yet
- Chapter 18cDocument5 pagesChapter 18caexillisNo ratings yet
- Chapter 19eDocument5 pagesChapter 19eaexillisNo ratings yet
- Chapter 20bDocument6 pagesChapter 20baexillisNo ratings yet
- Chapter 19dDocument3 pagesChapter 19daexillisNo ratings yet
- Chapter 19bDocument6 pagesChapter 19baexillisNo ratings yet
- Chapter 18aDocument5 pagesChapter 18aaexillisNo ratings yet
- Chapter 18bDocument4 pagesChapter 18baexillisNo ratings yet
- Pex 03 09Document5 pagesPex 03 09aexillisNo ratings yet
- Answer Key For Practice Quiz Blood and HeartDocument1 pageAnswer Key For Practice Quiz Blood and HeartaexillisNo ratings yet
- Pex 03 06Document6 pagesPex 03 06aexillis100% (3)
- Pex 03 07Document6 pagesPex 03 07aexillis100% (3)
- Pex 03 08Document4 pagesPex 03 08aexillisNo ratings yet
- Pex 03 04Document6 pagesPex 03 04aexillis57% (7)
- Pex 03 05Document10 pagesPex 03 05aexillis100% (5)
- Pex 03 03Document7 pagesPex 03 03aexillis75% (4)
- Pex 03 01Document8 pagesPex 03 01aexillis100% (2)
- Pex 03 02Document5 pagesPex 03 02aexillis0% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Ecg Short AnswerDocument3 pagesEcg Short AnswerZoey SanNo ratings yet
- ECG InterpretationDocument81 pagesECG InterpretationRidyah Ning Tyas100% (2)
- DC ShockDocument8 pagesDC Shockرافت العواضيNo ratings yet
- Nervous Systems - Neuron Function: Excitability Resting Potentials Graded Potential Action Potential The SynapseDocument48 pagesNervous Systems - Neuron Function: Excitability Resting Potentials Graded Potential Action Potential The SynapseRajeev AgarwalNo ratings yet
- PVC Stoelting Coex 1Document29 pagesPVC Stoelting Coex 1Rudy SiahaanNo ratings yet
- CardioversionDocument48 pagesCardioversionDeeksha RajputNo ratings yet
- Kuliah EKG AritmiaDocument38 pagesKuliah EKG AritmiaJeanetteMarchi100% (1)
- 2021-BME-22 (Lab 7) Nishwa Ijaz PDFDocument5 pages2021-BME-22 (Lab 7) Nishwa Ijaz PDFnishwaNo ratings yet
- Understanding ECGs: A Guide to ECG InterpretationDocument37 pagesUnderstanding ECGs: A Guide to ECG InterpretationAmit Pannu100% (1)
- PhysioEx Exercise 3 Activity 4Document4 pagesPhysioEx Exercise 3 Activity 4PatriNo ratings yet
- Introduction of EcgDocument52 pagesIntroduction of Ecgmiss_studyNo ratings yet
- Cardiac Conduction SystemDocument18 pagesCardiac Conduction SystemDannycanNo ratings yet
- Thornton, Andrew Simon PDFDocument201 pagesThornton, Andrew Simon PDFRamona ZavateNo ratings yet
- Electric Properties of Cardiac MusclesDocument5 pagesElectric Properties of Cardiac Musclesragulkutty72No ratings yet
- ECG Rhythm Strip Interpretation Lesson 4Document5 pagesECG Rhythm Strip Interpretation Lesson 4phoebjaetanNo ratings yet
- Bio Signal Characteristics and Electrode ConfigurationsDocument54 pagesBio Signal Characteristics and Electrode Configurationspriya dharshiniNo ratings yet
- Ambulatory ECG Monitoring in The Age of SmartphonesDocument11 pagesAmbulatory ECG Monitoring in The Age of SmartphonesSaul PeñaNo ratings yet
- Adult Cardiac Arrest AlgoritmaDocument1 pageAdult Cardiac Arrest AlgoritmaYouniehacibie Ichisky ChildNo ratings yet
- Unit 1 Part 3 SignallingDocument32 pagesUnit 1 Part 3 SignallingAnn NguyenNo ratings yet
- A Visual Guide To ECG Interpretation 2e 40 Jan 1 2017 41 40 1496321537 41 40 LWW 41Document1,578 pagesA Visual Guide To ECG Interpretation 2e 40 Jan 1 2017 41 40 1496321537 41 40 LWW 41xtineNo ratings yet
- Electrogram Recording and Analyzing Techniques ToDocument14 pagesElectrogram Recording and Analyzing Techniques ToTanah PantaiNo ratings yet
- ATLSDocument34 pagesATLSalice DillerudNo ratings yet
- Cardiac Action PotentialDocument9 pagesCardiac Action PotentialswennecaNo ratings yet
- EARTHWORM NERVE ACTION POTENTIALS REPORTDocument5 pagesEARTHWORM NERVE ACTION POTENTIALS REPORTMarie Guia Stella MiguelNo ratings yet
- DysrhythmiasDocument67 pagesDysrhythmiashhh hhhNo ratings yet
- Acls - MegacodeDocument11 pagesAcls - MegacodeEllen Joyce FlorNo ratings yet
- Membrane PotentialsDocument24 pagesMembrane PotentialsJeff ParkNo ratings yet
- ECG A Methodical Approach - Leaflet Print - Patient UKDocument7 pagesECG A Methodical Approach - Leaflet Print - Patient UKBen MpanzuNo ratings yet
- ECG Abnormalities Summary: Sinus Rhythm to Atrial FlutterDocument8 pagesECG Abnormalities Summary: Sinus Rhythm to Atrial FlutterChristine Nancy NgNo ratings yet
- MultiClamp 700BDocument174 pagesMultiClamp 700BmgiuglianoNo ratings yet