Professional Documents
Culture Documents
Asthma in Children
Uploaded by
Helmi HaronOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Asthma in Children
Uploaded by
Helmi HaronCopyright:
Available Formats
CLINICAL PRACTICE GUIDELINE FOR ASTHMA IN CHILDREN 0-4 YEARS OF AGE AND 5-11 YEARS OF AGE
Asthma often begins in childhood. 50 to 80% of children with asthma develop asthma symptoms (coughing, wheezing, shortness of breath or rapid breathing, chest tightness) before 5 years of age. Factors associated with onset of asthma symptoms in children include: allergy, a family history of asthma and/or allergy, perinatal exposure to tobacco smoke, viral respiratory infections, smaller airways at birth and in early life, male gender and low birth weight. Asthma in children should be considered when there is a history of recurrent cough (especially nocturnal), wheezing, shortness of breath or rapid breathing and chest tightness. It should also be considered with repeated diagnoses of: reactive airway disease, allergic bronchitis, wheezy bronchitis, asthmatic bronchitis, recurrent pneumonia or recurrent bronchiolitis. Asthma in this age group can be divided into four classifications: Intermittent, Mild Persistent, Moderate Persistent and Severe Persistent. For any child with asthma, the severity of the disease can change over time. Any child with asthma may have a severe exacerbation. Classifying a child as having mild asthma (either intermittent or mild persistent) does not rule out the possibility of a severe exacerbation. Children with viral-induced wheezing may have severe episodes with complete resolution between episodes, and may remain symptom free for months. Children with more than two episodes of asthma symptoms per month have persistent asthma. How do you classify the childs asthma severity? 1. BEFORE THERAPY is started; classify severity according to the clinical features of the childs asthma. *See the classifying charts attached with this guideline. 2. BEFORE OPTIMAL THERAPY IS ATTAINED (i.e. the child is taking medication but optimal control of the childs asthma has not yet been achieved), classify severity according to the clinical features of the childs asthma, as indicated in the attached classifying charts. 3. AFTER OPTIMAL THERAPY IS ATTAINED, the childs asthma severity can be classified according to the level of treatment needed to maintain control. For example: For intermittent asthma, no daily medication is needed. However, the use of shortacting beta2-agonist more than 2 times per week may indicate the need to start long-term control medication. For mild persistent asthma, one daily long-term control medication is necessary. For moderate persistent asthma, inhaled corticosteroids with or without additional long-term control medications are recommended. For severe persistent asthma, multiple long-term control medications are required, including high-dose inhaled corticosteroids and, if needed, other medication, including oral corticosteroids.
H:\QI\QI\Practice Guidelines\2012\COMPLETED\Asthma_in_Children.doc
Guideline 4, Page 1
It is recommended that practitioners providing care to asthmatic patients document in the patients medical record the severity of the asthma using the four classifications: Intermittent, Mild Persistent, Moderate Persistent and Severe Persistent. Managing the Child with Asthma Successful asthma management has 4 components: 1. Regular assessment and monitoring 2. Control of factors that contribute to symptoms and disease severity 3. Pharmacologic therapy 4. Patient education The aim of asthma therapy in children is to maintain control of asthma with the least amount of medication and, hence, minimal risk for adverse effects. Management: *See attached tables for children aged 0-4 and children aged 5-11. Goals of Therapy for the Child with Asthma 1. Prevent chronic and troublesome symptoms. 2. Prevent exacerbations of symptoms. 3. Maintain normal activity levels. 4. Maintain normal pulmonary function. 5. Optimize pharmacotherapy, minimize side effects. 6. Satisfy the childs and the familys expectations/goals for asthma care. Referral to an asthma specialist (for consultation or co-management) is recommended when: The child has had a life-threatening asthma exacerbation. Goals of asthma therapy are not being met after 3-6 months of treatment; earlier if the child appears unresponsive to treatment. Signs and symptoms are atypical, or there are problems in differential diagnosis. Other conditions complicate asthma or its diagnosis (e.g., untreated sinusitis, rhinitis). Additional diagnostic testing is indicated (e.g., pulmonary function testing, allergy skin testing). The child or family needs additional education and guidance on complications or therapy, problems with adherence, or avoidance of triggers. The child is being considered for immunotherapy. The child has severe persistent asthma. The child is under 3 years of age and has moderate or severe persistent asthma. The child has used long-term oral corticosteroid therapy, high-dose inhaled corticosteroid therapy, or more than 2 bursts of oral corticosteroids in 12 months. The AAAAI (American Academy of Allergy, Asthma and Immunology) recommends that anyone with the diagnosis of asthma be seen by an allergy specialist at least once for diagnostic evaluation and skin testing to exclude allergy as a cause or etiology of their asthma.
H:\QI\QI\Practice Guidelines\2012\COMPLETED\Asthma_in_Children.doc
Guideline 4, Page 2
Identification of allergens in the environment may allow modification of that environment which in and of itself may allow management and excellent control without life long chronic use of medications. References: National Asthma Education and Prevention Program. NAEPP Expert Panel Report Guidelines for the Diagnosis and Management of Asthma-Update on Selected Topics 2002. NIH Publication No. 02-5075. June 2002. Reprinted May 2003. Pediatrics in Review, Volume 30, Number 10, October, 2009. National Heart, Lung and Blood Institute. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. US Department of Health and Human Services, National Institutes of Health, August 2007. American Academy of Allergy Asthma & Immunology. Pediatric Asthma-Promoting Best Practice. 2002.
Chief Medical Officer - Pro Tem Medical Associates Clinic & Health Plans
Date
President Medical Associates Clinic
Date
Original: Revised: Revised: Revised:
10/99 02/01 03/02 03/03
Revised: Revised: Revised: Revised:
06/04 01/05 07/06 06/07
Revised: Reviewed: Revised: Reviewed:
07/08 10/09 02/11 02/12
H:\QI\QI\Practice Guidelines\2012\COMPLETED\Asthma_in_Children.doc
Guideline 4, Page 3
H:\QI\QI\Practice Guidelines\2012\COMPLETED\Asthma_in_Children.doc
Guideline 4, Page 4
H:\QI\QI\Practice Guidelines\2012\COMPLETED\Asthma_in_Children.doc
Guideline 4, Page 5
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The China Study PDFDocument7 pagesThe China Study PDFPatrice108365No ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Advances in Extraction TechniquesDocument13 pagesAdvances in Extraction TechniquesashajangamNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Clinical Cases For MRCPCH PART 2 Applied Knowledge in PracticeDocument218 pagesClinical Cases For MRCPCH PART 2 Applied Knowledge in Practiceaeyousef88% (16)
- Sanctification of The Heart 4th Edition by DR Michelle StrydomDocument771 pagesSanctification of The Heart 4th Edition by DR Michelle StrydomDios Estrella67% (3)
- Moh ExamsDocument12 pagesMoh ExamsPankaj Jindal100% (5)
- Review of Literature on Rabies Prevention and ControlDocument24 pagesReview of Literature on Rabies Prevention and ControlBeah Claudette AbundoNo ratings yet
- Nephrons (Functional Unit)Document44 pagesNephrons (Functional Unit)Nur SanaaniNo ratings yet
- Treatment of Cardiac Arrest in The Hyperbaric Environment - Key Steps On The Sequence of Care - Case ReportsDocument8 pagesTreatment of Cardiac Arrest in The Hyperbaric Environment - Key Steps On The Sequence of Care - Case Reportstonylee24No ratings yet
- AcanthamoebaDocument7 pagesAcanthamoebaYohanna YohannaNo ratings yet
- ACS, ZaiDocument61 pagesACS, ZaiHelmi HaronNo ratings yet
- Ascitesupdate2013 PDFDocument27 pagesAscitesupdate2013 PDFKun Anupong WansukhNo ratings yet
- Tumor Jinak PayudaraDocument2 pagesTumor Jinak PayudaraHelmi HaronNo ratings yet
- Femur and Pelvis Fracture (Trauma)Document20 pagesFemur and Pelvis Fracture (Trauma)Ree YahNo ratings yet
- QuestionsDocument6 pagesQuestionsLorvic Andrew Juanson UmaliNo ratings yet
- Not Eligible As No Experience of Teaching and ResearchDocument5 pagesNot Eligible As No Experience of Teaching and ResearchVasanth Kumar AllaNo ratings yet
- Int Obs PDFDocument37 pagesInt Obs PDFsurgeon77No ratings yet
- Amavatha & VathasonithaDocument125 pagesAmavatha & VathasonithaCicil AbrahamNo ratings yet
- Journal BalakrishnaDocument3 pagesJournal BalakrishnafandheanayaNo ratings yet
- Multiple PregnancyDocument16 pagesMultiple Pregnancyjane7arian7berzabalNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaNurfauziyahNo ratings yet
- Understanding the Benefits of Physical ActivitiesDocument17 pagesUnderstanding the Benefits of Physical ActivitiesRealisan DulnuanNo ratings yet
- Stanford Letter Criticizes Trump COVID-19 AppointeeDocument11 pagesStanford Letter Criticizes Trump COVID-19 AppointeeBayAreaNewsGroup100% (2)
- Prostaglandins: An Overview of Structure and FunctionDocument33 pagesProstaglandins: An Overview of Structure and FunctionMuhammad JamalNo ratings yet
- Mgi Presentation - ReyDocument65 pagesMgi Presentation - ReyCharlot Jade Paderes67% (3)
- Abu Dhabi DRGDocument62 pagesAbu Dhabi DRGDolly creationsNo ratings yet
- Hypokalemia and Hyperkalemia in Infants and Children: Pathophysiology and TreatmentDocument11 pagesHypokalemia and Hyperkalemia in Infants and Children: Pathophysiology and TreatmentAnantaBenvenutoNo ratings yet
- 2012 Karshaniya YavaguDocument4 pages2012 Karshaniya YavaguRANJEET SAWANTNo ratings yet
- Delafloxacin 4Document23 pagesDelafloxacin 4Muhammad RamzanNo ratings yet
- Anterior Segment OctDocument53 pagesAnterior Segment OctA.c. RaghuNo ratings yet
- Nursing Management - Colon CancerDocument7 pagesNursing Management - Colon CancerReese Alessandra GandulfoNo ratings yet
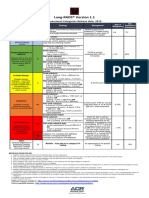
- Lung RADS® Version 1.1: Assessment Categories Release Date: 2019Document1 pageLung RADS® Version 1.1: Assessment Categories Release Date: 2019S Francisco MotNo ratings yet
- List of Empanelled Hospitals in CGHS NagpurDocument58 pagesList of Empanelled Hospitals in CGHS NagpurRajatNo ratings yet
- Audiometric Evaluation Report .: Left Ear Right EarDocument1 pageAudiometric Evaluation Report .: Left Ear Right EarRaja IsaacNo ratings yet
- Prevalence of Hypothyroidism in Adults An EpidemioDocument6 pagesPrevalence of Hypothyroidism in Adults An EpidemioCindy Auliah NasutionNo ratings yet