Professional Documents
Culture Documents
Refusing Smokers Is Unethical and Dangerous Precedent: To Treat A
Uploaded by
Ionut Bălănescu SonnyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Refusing Smokers Is Unethical and Dangerous Precedent: To Treat A
Uploaded by
Ionut Bălănescu SonnyCopyright:
Available Formats
Considerable evidence exists regarding the adverse effect of continued smoking on vein graft patency rates and early
operative mortality and morbidity. One study has reported a reduction in the relative survival of younger patients who smoke,36 and, although little work has been done, it would seem likely that continued smoking will negate the beneficial effect of surgery in patients whose life expectancy would be expected to improve after operation. Subjecting patients who conninue to smoke, and for whom the only indication for operation is the relief of angina, to the increased risks of surgery in the face of a remediable cause is not justified.
1 Nikutta P, Uchtlen PR, Wiese B, Jost S, Dekkers J, Rafflenbeul W, et al. Influence of cigarette smoking on the progression of coronary artery disease within three years: results of the INTACT study. J Am Coil Cardiol 1990;15:181A. 2 Fielding JE. Smoking. Health effects and control (part one). N Engl J7 Med 1985;313:491-8. 3 Suttorp MJ, Kingma JH, Vos J, Koomen EM, Tijssen JGP, Vermeulen FEC, et al. Determinants for early mortality in patients awaiting coronary artery bypass graft surgery: a case-control study. EurHeartj 1992;13:238-42. 4 CASS Principal Investigators and their Associates. Coronary artery surgery study (CASS): a randomised trial of coronary artery surgery: quality of life in patients randomly assigned treatment groups. Circulation 1983;68: 951-60. 5 Peduzzi P, Hultgren H, Thomsen J, Detre K. Ten year effect of medical and surgical therapy on quality of life: Veterans Administration cooperative study of coronary artery surgery. AmJCardiol 1987;59:1017-23. 6 Silverman KJ, Grossman W. Angina pectoris: natural history and strategies for evaluation and management. NEnglJMed 1984;310:1712-7. 7 Cameron EWJ, Walker WS. Coronary artery bypass surgery. BMJ 1990;300: 1219-20. 8 Badimon JJ, Ip J, Badimon L, Fuster V. Thrombosis and accelerated atherosclerosis in coronary bypass surgery and restenosis after percutaneous transluminal coronary angioplasty: implications for therapy. Coronary Artery Disease 1990;2: 170-9. 9 ACC/AHA Task Force. Guidelines and indications for coronary artery bypass graft surgery. A report of the American College of Cardiology/American Heart Association Task Force on assessment of diagnostic and therapeutic cardiovascular procedures._JAm Coil Cardiol 1991 ;17:543-89. 10 Smith SH, Geer JC. Morphology of saphenous vein-coronary artery bypass grafts: 7-116 months postoperatively. Arch Pathol Lab Med 1983;107:13-8. 11 Goldman S, Copeland J, Moritz T, Henderson W, Zadina K, Ovitt T, et al. Improvement in early saphenous vein patency after coronary artery bypass surgery with antiplatelet therapy: results of a Veterans Administration cooperative study. Circulation 1988;77:1342-52. 12 Bosch X, Perez-Villa F, Sanz G. Effect of smoking habits on the preventive effect of aspirin and dipyridamole on early aortocoronary bypass occlusion. Eur HeartJ 1991;12:170. 13 Levine PH. An acute effect of cigarette smoking on platelet function. Circulation 1973;48:619-23. 14 Galea G, Davidson RJL. Haematological and haemorheological changes associated with cigarette smoking. Clin Pathol 1985;38:978-84. 15 Fitzgerald GA, Oates JA, Nowak J. Cigarette smoking and haemostatic function. Amn Heart3 1988;115:267-7 1.
_
16 Wilhelmsen L, Svardsudd K, Korsan-Bengtsen K. Fibrinogen as a risk factor for stroke and myocardial infarction. N EnglJ Med 1984;311:501-5. 17 Fuster V, Chesebro JH, Frye RL, Elveback LR. Platelet survival and the development of coronary artery disease in the young adult: effects of cigarette smoking, strong family history and medical therapy. Circulation 1981 ;63:546-5 1. 18 Solymoss BC, Nadeau P, Millette D, Inge B, Campeau L. Late thrombosis of saphenous vein coronary bypass grafts related to risk factors. Circulation 1988;78(suppl I): 140-3. 19 Wiseman S, Kenchington G, Dain R, Marshall CE, McCollum CN, Greenhalgh RM, et al. Influence of smoking and plasma factors on the patency of femoropopliteal grafts. BMJ 1989;298:643-6. 20 Greenhalgh RM, Laing SP, Cole PV, Taylor GW. Smoking and arterial reconstruction. BrJSurg 1981;68:605-7. 21 Nietzel GF, Baboriak JJ, Pintar K, Quershi I. Atherosclerosis in aortocoronary bypass grafts. Morphological study and risk factor analysis 6-12 years after surgery. Arteriosclerosis 1986;6:594-600. 22 Campeau L, Enjalbert M, Lesperance J, Bourassa MG, Kwiterovitch P, Wacholder S, et al. The relation of risk factors to the development of atherosclerosis in saphenous vein bypass grafts and the progression of the disease in the native circulation. A study 10 years after aortocoronary bypass surgery. NEnglJMed 1984;311:1329-32. 23 Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli P. High density lipoprotein cholesterol and cardiovascular disease: four year prospective American studies. Circulation 1989;79:8-15. 24 Stampfer MJ, Sacks FM, Salvini S, Willett WC, Hennekens CH. A prospective study of cholesterol. apolipoproteins and the risk of myocardial infarction. NEnglJfMed 1991;325:373-81. 25 Criqui MH, Wallace RB, Heiss G, Mislakel M, Schonfeld G, Jones GTL. Cigarette smoking and plasma high-density cholesterol. Circulation 1980;62
(suppl IV):70-6.
26 FitzGibbon GM, Leach AJ, Kafka HP. Atherosclerosis of coronary artery bypass grafts and smoking. Can AledAssocj 1987;136:45-7. 27 Vekkala K, Jarvinen A, Virtanen K, Keto P, Pellinen T, Salminen US, et al. Indications for and risks in reoperation for coronary artery disease. Scan J
Thorac Cardiwvasc Surg 1990;24:1-6.
28 Dougenis D, Naik S, Hedley Brown A. Is repeated coronary surgery for recurrent angina cost effective? EurHeart3 1992;13:9-14. 29 Nair UR, Campell CC, Dark JF, Deiranya AK, Lawson RA, Mousalli H, et al. Reoperation for recurrent coronary artery and graft disease. A review of 73 patients in a group of 2573 consecutive first operations. J Cardiovasc Surg 1989;30:656-60. 30 Ivert TS, Ekestrom S, Peterffy A, Welti R. Coronary artery reoperations. Early and late results in 101 patients. Scand J Thorac Cardiovasc Surg 1988;22:1 11-8. 31 Wamer M, Offord KP, Wamer ME, Lennon RL, Conover MA, JanssonSchumacher U, et al. Role of preoperative cessation of smoking and other factors in postoperative pulmonary complications: a blinded prospective study of coronary artery bypass patients. Mayo Clin Proc 1989;64:609-16. 32 Carrel T, Scmid ER, von Segesser L, Vogt M, Turina M. Preoperative assessment of the likelihood of infection of the lower respiratory tract after cardiac surgery. Thorac Cardiovasc Surg 199 1;39:85-8. 33 Nagachinta T, Stephens M, Reitz B, Polk BF. Risk factors for surgical wound infection following cardiac surgery. 7 Infect Dis 1987;156:967-73. 34 Engblom E, Ronnemaa T, Hamalainen H, Kallio V, Vantinen E, Knutz LR. Coronary heart disease risk factors before and after bypass surgery: results of a controlled trial on multifactorial rehabilitation. EurHeartJ 1992;13:232-7. 35 Brook RH, Park RE, Winslow CM, Chassin MR, Winslow CM, Hampton JR. Diagnosis and treatment of coronary disease: a comparison of doctors attitudes in the USA and the UK. Lancet 1988;ii:750-3. 36 Ramanathan KB, Vander Zwaag R, Maddock V, Kroetz FW, Sullivan JM, Mirvis DM. Interactive effects of age and other risk factors on long term survival after coronarv artery surgery. JAm cOi Cardiol 1990;15:1493-9.
Refusing to treat smokers is unethical and a dangerous precedent
Matthew Shiu
Should cigarette smokers be offered coronary artery bypass graft operations? Some specialists are adamant that they should not unless they promise to give up smoking. With increasing resource limitations, such views may soon become accepted policy. Some of the argument would seem well founded on several fronts: the known adverse effect of smoking on the use of anaesthetics; the known adverse effects of continued smoking on graft survival and progression of coronary artery disease; and limited resources with ever increasing demand. There is no doubt that cigarette smoking is harmful to coronary arteries. The medical profession is united in condemning smoking and has been fairly successful. Working as a general practitioner and with a special interest in cardiology, I spend much of my time getting patients off cigarettes. There is, however, a small group of patients who truly cannot give up their habit. All anti-smoking clinics have such examples. The medical profession does not have a satisfactory treatment for true cigarette addiction. So is it right to completely deny this group of high risk patients a
1048
recognised form of treatment because they cannot give up smoking? According to a spokesperson at the Medical Defence Union, should a case ever be brought to the court it would be difficult to defend such a stand if treatment was refused solely on those grounds. Some patients are denied investigations on the grounds that surgery will not be offered. The outcome of coronary artery surgery can be compromised by other factors such as hypertension, diabetes, age, female gender, obesity, and hypercholesterolaemia. These are all accepted as deleterious but not absolute overriding contraindications. Is it right to isolate one risk factor and make a firm policy without taking other issues into consideration? Diabetic patients are operated on-even the ones who cannot stay on a strict diet. Will patients be refused surgery because they cannot stick to a cholesterollowering diet? Resources are limited and will continue to be limited. If we examine the resource issue more closely, however, the argument does not seem so strong. The financial cost of not operating is often much higher BMJ VOLUME 306
17 APRIL 1993
than the cost of operating. Patients not given operations are unemployable, need sickness benefits, remain on multiple expensive medication, and require repeated hospital admissions for chest pains. Money is saved on the surgical units at the expense of the state.
"Has self infliction in any other condition ever barredpatients from receiving proper care in Britain?"
But the real issue is not money but ethics. Limited resources should be a problem for the health care system. Instead of withholding treatment, doctors should use their influence in the proper channel. One surgeon said he would not operate on smokers even with all the resources available in the NHS for he
does not wish to construct walls for people who are busy knocking them down. If we accept this are- rnent, then more than half the genitourinary clinics cat. .Jose down. Asthmatic smokers will not be given nebulisers. It has been argued that damage caused by smoking is self inflicted, hence smokers do not deserve treatment. But has self infliction in any other condition ever barred patients from receiving proper investigation and treatment in Britain? I would like to believe that up to now doctors have always treated patients, irrespective of the degree of culpability of the person concemed. Drunken victims of road traffic accidents are never made to promise total alcohol abstinence before they are given first aid. Patients who attempt suicide are always treated. My view is that once we accept an absolute bar to surgery for smokers, we would next refuse lifesaving treatment to asthmatic smokers and soon may well be on the slippery slope to withholding treatment for the unmotivated and the unfit.
Human frailty should not be penalised
Roger Higgs
"Well, yes, I must admit I smoke." "I am glad to hear it. A man should always have an occupation of some kind."
Lady Bracknell's marital history taking from the hapless Mr Worthing is still as funny as when Oscar Wilde introduced The Importance of Being Ernest to the stage a hundred years ago. But since then attitudes to smoking and to medical care have changed beyond recognition. The modem Mr Worthing's misfortune is no longer that he was born in a handbag, with or without handles. For the young man now who smokes and has coronary artery disease, the uncertainty is from the budgetary plans of the health authority over which Mrs Bracknell now presides. M J Underwood and J S Bailey give her clear advice. This is an expensive operation, and should not be offered without careful thought. In an area of great complexity, guidelines are vital. Apart from the technical issues, there have been traditionally two separate levels of decision making about such treatments. The first is that of indications (or contraindications). At this level the evidence is carefully considered, based it is hoped on good research, and guidelines are established about the circumstances in which a particular intervention would be helpful. This is quite separate from the consideration of an individual case and should apply whatever the particular circumstances of the health care system in question. The second level is that of engaged clinical judgment, or advice about an individual's medical care. Here the first level clinical guidelines are of great importance but are certainly not the only issues which lead to the decision. Of course it would be quite wrong from any point of view to recommend a procedure for anyone who would stand to run great risks and reap few benefits from it. But where a positive balance is to be struck, however small, other factors must be taken into account: the patient's wishes, the overall clinical picture, the social situation, and so forth. How widely the net is to be cast is not formalised, but this level of decision making is shared between doctor and patient. The autonomy of both is respected, and the need for mutual exchange of information and understanding underpins the decision. Medical care is not based on prescience but on probability-good guesses, perhaps, but no more. Nobody can predict with certainty the BMJ VOLUME 306
17 APRIL 1993
degree of benefit (or the lack of it) in the individual case, but it is assumed by all that the doctor is advising with the patient's manifest best interests in mind. In between these levels, however, is a third and quite distinct type of decision making, based on the resources available. In a closed system, one person's benefit may be another person's loss or lack of benefit.
"To disenfranchise certain groups for certain types of expensive health care... should make usfeel uneasy."
There is nothing new in this, except that until recently this has not been part of explicit clinical decision making at the other two levels. This causes confusion unless the reasons are clear and are made explicit. If we are forced to take resourcing factors into account, these have to be openly explained. The health authority must be told by clinicians what benefit could be obtained for whom and to what degree. The cut off point either way is for negotiation. Likewise, the clinician must be open to the patient about the degree of benefit and risks of harm to the individual, and the degree of benefit that the system can offer. Patients should be told which of the three levels they are receiving advice on: whether the treatment is indicated, whether it can be afforded, or whether in balance it is the best for them. If the information to make the first level decision is available and valid, a scoring system for the individual level could presumably be created which could aid in the individual case. But within this, as Matthew Shiu points out, for coronary artery surgery, smoking would be just one factor among many, even before personal issues were taken into account. The obese diabetic non-smoker who takes no exercise and has a poor family history, for example, might well stand to reap fewer benefits than the exercising smoker without other risk factors, and so on. In selection for surgery, if we abandon the universally available queue and reject a lottery we should presumably be aiming at more overall quantification as an aid in the traditional process of clinical judgment. Good clinical judgment is thus seen as consistent and
1049
You might also like
- Walt DisneyDocument56 pagesWalt DisneyDaniela Denisse Anthawer Luna100% (6)
- Manual of Seamanship PDFDocument807 pagesManual of Seamanship PDFSaad88% (8)
- Hypertensive Heart DiseasesDocument5 pagesHypertensive Heart DiseasesserubimNo ratings yet
- CT of The Heart PDFDocument391 pagesCT of The Heart PDFZornić AlemNo ratings yet
- IMS-PRO-02 Hazard and Risk Assessment & Aspect ImpactDocument6 pagesIMS-PRO-02 Hazard and Risk Assessment & Aspect ImpactISO Consultancy100% (1)
- ObliconDocument3 pagesObliconMonica Medina100% (2)
- Acute Coronary Syndrome inDocument2 pagesAcute Coronary Syndrome inpaul_preda_bvNo ratings yet
- SM1 EsmDocument12 pagesSM1 EsmjujuNo ratings yet
- B. Collection of Key Landmark Articles in Cardiothoracic SurgeryDocument8 pagesB. Collection of Key Landmark Articles in Cardiothoracic SurgeryGregNo ratings yet
- Pub 1Document5 pagesPub 1Web ResearchNo ratings yet
- Understanding The Nexus High Blood Pressure Among Cancer Patients During TreatmentDocument5 pagesUnderstanding The Nexus High Blood Pressure Among Cancer Patients During TreatmentWeb ResearchNo ratings yet
- Cardiology: Stenting vs. Endarterectomy For Carotid Artery Stenosis: What Are The Trade-Offs?Document8 pagesCardiology: Stenting vs. Endarterectomy For Carotid Artery Stenosis: What Are The Trade-Offs?juanpavNo ratings yet
- StrokeDocument67 pagesStrokeGagi MiloševićNo ratings yet
- Comment: Vs 140 (61 4%) of 228 Patients Hazard Ratio (HR)Document2 pagesComment: Vs 140 (61 4%) of 228 Patients Hazard Ratio (HR)Barbara Sakura RiawanNo ratings yet
- Ghid de Evaluare Si Tratament Al Sindroamelor Coronariene Acute Fara Supradenivelare Persistenta de ST - An 2003Document40 pagesGhid de Evaluare Si Tratament Al Sindroamelor Coronariene Acute Fara Supradenivelare Persistenta de ST - An 2003LoredanaMunteanuNo ratings yet
- BibiliographyDocument5 pagesBibiliographyOleOhhNo ratings yet
- Selected Citations in Trauma and Emergency MedicineDocument2 pagesSelected Citations in Trauma and Emergency MedicineWendy LiNo ratings yet
- Coronary Heart Disease Seondary Prevention - Review ArticleDocument12 pagesCoronary Heart Disease Seondary Prevention - Review ArticleqanitaNo ratings yet
- REFERENCESDocument61 pagesREFERENCESTasya IrwanNo ratings yet
- Riddell PDFDocument24 pagesRiddell PDFMartha Yaneth VelasquezNo ratings yet
- Oronary Disease in HypothyroidismDocument2 pagesOronary Disease in HypothyroidismyaacoubNo ratings yet
- BibliographyDocument10 pagesBibliographySoumyaReddyNo ratings yet
- Cardiology: Improvement in U.S. Heart Failure Outcomes, 1998-2008Document8 pagesCardiology: Improvement in U.S. Heart Failure Outcomes, 1998-2008juanpavNo ratings yet
- 3210 FullDocument1 page3210 FullGiorgiana NicoletaNo ratings yet
- Packer 2019Document14 pagesPacker 2019Renata D GNo ratings yet
- Schouten, OlafDocument415 pagesSchouten, OlafGima Amezia SariNo ratings yet
- Prognosis: Prognosis - Diabetes Mellitus - Body, Effects, DiseaseDocument8 pagesPrognosis: Prognosis - Diabetes Mellitus - Body, Effects, DiseaseSulistiyawati CuplizNo ratings yet
- Ehab 268Document2 pagesEhab 268yori yarson tonNo ratings yet
- 1 Running Head: Preventing Recurrent Myocardial InfarctionsDocument10 pages1 Running Head: Preventing Recurrent Myocardial InfarctionsIsaacNo ratings yet
- Usefulness of Diabetes Mellitus To Predict Long-Term Outcomes in Patients With Unstable Angina Pectoris.Document15 pagesUsefulness of Diabetes Mellitus To Predict Long-Term Outcomes in Patients With Unstable Angina Pectoris.Diah Kris AyuNo ratings yet
- Atrial Fibrillation With PVC Bigeminy in RHD Patient FinalDocument2 pagesAtrial Fibrillation With PVC Bigeminy in RHD Patient FinalNathania HoswandiNo ratings yet
- Heart 2012 Rathod A82Document2 pagesHeart 2012 Rathod A82Wahyu SholekhuddinNo ratings yet
- Estimacion de EdadDocument2 pagesEstimacion de EdadsuarezjiNo ratings yet
- ECG Scoring For The Evaluation of Therapy Naive Cancer Patients To Predict CardiotoxicityDocument11 pagesECG Scoring For The Evaluation of Therapy Naive Cancer Patients To Predict CardiotoxicityjuanpbagurNo ratings yet
- Stroke PDFDocument67 pagesStroke PDFBadrul MunirNo ratings yet
- Dapus RifDocument8 pagesDapus RifarieftamaNo ratings yet
- New England Journal Medicine: The ofDocument14 pagesNew England Journal Medicine: The ofIMNo ratings yet
- Clinical Features and Outcomes of Takotsubo Stress Cardiomyopathy NEJMoa1406761Document10 pagesClinical Features and Outcomes of Takotsubo Stress Cardiomyopathy NEJMoa1406761William LeeNo ratings yet
- Heartfailure FixDocument10 pagesHeartfailure FixdhikaNo ratings yet
- Urgent Surgery Ulcerative: LeadingDocument2 pagesUrgent Surgery Ulcerative: LeadingYaumil ChoiriNo ratings yet
- Estudio de Endarterectomía CarotídeaDocument9 pagesEstudio de Endarterectomía CarotídeaErnest Pardo RubioNo ratings yet
- Applications of Cardiac Computed Tomography in The Cardio-Oncology PopulationDocument13 pagesApplications of Cardiac Computed Tomography in The Cardio-Oncology Populationricardo villaNo ratings yet
- Published,, Noval Anti-Cancer TherapiesDocument10 pagesPublished,, Noval Anti-Cancer Therapiesshayma rafatNo ratings yet
- In Search of The Optimal Iron Chelation Therapy For Patients With Thalassemia MajorDocument4 pagesIn Search of The Optimal Iron Chelation Therapy For Patients With Thalassemia MajorAnonymous 7jKR9XbNo ratings yet
- MinaDocument6 pagesMinaminamoharebNo ratings yet
- tmpD49B TMPDocument2 pagestmpD49B TMPFrontiersNo ratings yet
- Madit CRTNEJMseot 09Document10 pagesMadit CRTNEJMseot 09binh doNo ratings yet
- Pci On Infark MyocardDocument10 pagesPci On Infark MyocardDinny Novia WNo ratings yet
- Lung CancerDocument2 pagesLung Cancerkaustuv2uNo ratings yet
- Heart Failure Thesis PDFDocument6 pagesHeart Failure Thesis PDFafknwride100% (2)
- PREMIER'06Document8 pagesPREMIER'06NagatzulNo ratings yet
- Aspiration Thrombectomy For Acute ST-Elevation Myocardial Infarction: Literature ReviewDocument9 pagesAspiration Thrombectomy For Acute ST-Elevation Myocardial Infarction: Literature ReviewArdiana FirdausNo ratings yet
- Recents Advances in Menopause ManagementDocument134 pagesRecents Advances in Menopause ManagementVania ParamithaNo ratings yet
- Nej Me 2210183Document2 pagesNej Me 2210183lakshminivas PingaliNo ratings yet
- Surgery Elderly 4Document5 pagesSurgery Elderly 4mx.pramirezNo ratings yet
- CourageDocument14 pagesCourageSuryaNo ratings yet
- Castle AfDocument11 pagesCastle AfgustavoNo ratings yet
- CABANADocument14 pagesCABANAIsmael Rivera DiazNo ratings yet
- DAFTAR PUSTAKA-GeriatricDocument4 pagesDAFTAR PUSTAKA-Geriatricmarlin berliannandaNo ratings yet
- Recommendation-Specific Supportive TextDocument22 pagesRecommendation-Specific Supportive Textodaliz.berrocalNo ratings yet
- Treatment Option 1Document6 pagesTreatment Option 1Elena-Dana OpreaNo ratings yet
- Role of The Nurse in Stroke RehabilitationDocument2 pagesRole of The Nurse in Stroke RehabilitationAnonymous mTqyS6No ratings yet
- Myocardial Contractile Dispersion: A New Marker For The Severity of Cirrhosis?Document5 pagesMyocardial Contractile Dispersion: A New Marker For The Severity of Cirrhosis?triNo ratings yet
- Imaging in Peripheral Arterial Disease: Clinical and Research ApplicationsFrom EverandImaging in Peripheral Arterial Disease: Clinical and Research ApplicationsNo ratings yet
- Configuring Srewquid Proxy ServerDocument4 pagesConfiguring Srewquid Proxy ServerPendekar BlankNo ratings yet
- Financial Management Model Question PaperDocument2 pagesFinancial Management Model Question PaperdvraoNo ratings yet
- A Brief History & Development of Banking in India and Its FutureDocument12 pagesA Brief History & Development of Banking in India and Its FutureMani KrishNo ratings yet
- The MinoansDocument4 pagesThe MinoansAfif HidayatullohNo ratings yet
- Carollo Motion To StayDocument7 pagesCarollo Motion To Stayal_crespoNo ratings yet
- Time ClockDocument21 pagesTime ClockMarvin BrunoNo ratings yet
- Bakst - Music and Soviet RealismDocument9 pagesBakst - Music and Soviet RealismMaurício FunciaNo ratings yet
- Sunbeam Model - Fpsbcmm901Document10 pagesSunbeam Model - Fpsbcmm901Andreah YoungNo ratings yet
- A Term Paper On The Application of Tort Law in BangladeshDocument7 pagesA Term Paper On The Application of Tort Law in BangladeshRakib UL IslamNo ratings yet
- S F R S (I) 1 - 2 1: Accounting For The Effects of Changes in Foreign Currency Exchange RatesDocument40 pagesS F R S (I) 1 - 2 1: Accounting For The Effects of Changes in Foreign Currency Exchange RatesRilo WiloNo ratings yet
- Case Exercise On Layer Unit (2000 Birds)Document2 pagesCase Exercise On Layer Unit (2000 Birds)Priya KalraNo ratings yet
- SCDL Strategic ManagementDocument6 pagesSCDL Strategic ManagementMicky StarNo ratings yet
- John Carroll University Magazine Winter 2008Document69 pagesJohn Carroll University Magazine Winter 2008johncarrolluniversityNo ratings yet
- Catalogu PDFDocument24 pagesCatalogu PDFFer GuNo ratings yet
- CrackJPSC Mains Paper III Module A HistoryDocument172 pagesCrackJPSC Mains Paper III Module A HistoryL S KalundiaNo ratings yet
- Power of The High Courts To Transfer CasesDocument2 pagesPower of The High Courts To Transfer CasesShweta ChauhanNo ratings yet
- Eapp Module 7 W11Document5 pagesEapp Module 7 W11Valerie AsteriaNo ratings yet
- Universalism and Cultural Relativism in Social Work EthicsDocument16 pagesUniversalism and Cultural Relativism in Social Work EthicsEdu ArdoNo ratings yet
- Gyges RingDocument1 pageGyges RingCYRINE HALILINo ratings yet
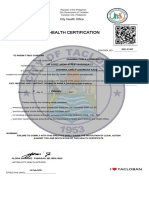
- Health CertsxDocument2 pagesHealth Certsxmark marayaNo ratings yet
- Section 6 in The Hindu Succession Act, 1956Document2 pagesSection 6 in The Hindu Succession Act, 1956Sathish KumarNo ratings yet
- 11 - Comment Review SheetDocument1 page11 - Comment Review SheetMohamed ShokryNo ratings yet
- Week 5 6 Diass 3.0Document7 pagesWeek 5 6 Diass 3.0Jonathan ReyesNo ratings yet
- 2018-2019 D7030 Rotaract Plans and Objectives (English) PDFDocument58 pages2018-2019 D7030 Rotaract Plans and Objectives (English) PDFDynutha AdonisNo ratings yet
- Udom Selection 2013Document145 pagesUdom Selection 2013Kellen Hayden100% (1)