Professional Documents
Culture Documents
Neurology Domain Guide
Uploaded by
mina000005Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neurology Domain Guide
Uploaded by
mina000005Copyright:
Available Formats
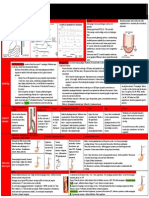
Age of Onset Diabetic Peripheral Neuropathy Werdnig-Hoffman Disease (SMA type I) Amyotrophic Lateral Sclerosis Guillain-Barre Syndrome Charot-Marie-Tooth
(HSMN type 1) Adult-onset
Diseases of Peripheral n (neuropathies) Location of Lesion Pathogenesis Clinical Presentation Symmetric distal polyneuropathy Degeneration of LMN UMN & LMN Degeneration of peripheral nn Segmental demyelination Decreased sensation in distal extremities
At birth or w/in 1st 4 months Middle aged/elderly
Autosomal recessive Mutation in SMN1 (missing exon 7) Autosomal dominant Degeneration of LMN and UMN Immune-mediated disorder
Childhood, Degeneration of Autosomal dominant early peripheral nn Chromosome 7 adulthood duplication; PMP 22 Neurogenic atrophy: atrophy in m fibers due to pathological changes in n or PNS Denervation atrophy: myocytes atrophy due to axon/myelin sheath degeneration Wallerian degeneration: axonal degeneration distal to point of axonal damage or cell body damage Disease of NMJ Myasthenia Gravis NMJ Immune-mediated loss of Begins with extraocular m weakness; Ach receptors ptosis, double vision; generalized weakness Myopathies: have elevated creatine kinase and proximal weakness; random necrosis and/or m fiber regeneration Neuropathies: distal weakness; group atrophy; fiber type grouping
LMN lesion; gen weakness, hypotonia, m wasting, tongue fasciculations; floppy baby UMN lesion deficits (hyperreflexia, Babinski) LMN lesion (fasciculations, wasting, weakness) Ascending paralysis; weakness in distal limbs w/ rapid advance to proximal mm, slow n conduction Distal m weakness; inverted champagnelike calf; pescavas, hammertoes
Gross/Micro Pathology Axonal neuropathy Segmental demyelination, thickening of endoneurial arterioles, hyalinization Atrophy of ventral horns/n roots; neurogenic atrophy Atrophy of ventral horns/n roots; Wallerian degen Chronic inflammation, seg demyelination Onion bulb-Segmental demyelinationremyelination;
Electrophysiological tests: nerve conduction and electromyography; n/m biopsy
Increased ICP Cingulate gyrus Herniation Uncal Herniation
Increased Intracranial Pressure and Herniation Etiology Compression Clinical Features Depends on age of pt and speed of expansion Headache, vomiting, pailledema maybe (swollen optic n), abducens n. palsy Factors depend on speed of expansion, age of patient; Blurred optic discs; focal neurologic signs: limb weakness >200mm water in LP Herniates under the falxcerebri Hemorrhage, neoplasms, infections Uncus herniates across tentorium cerebelli -compress structures in post fossa; Compress PCA, midbrain cerebral peduncle, CN III, brainstem downward Cerebellar tonsil herniation thru foramen magnum Ptosis, dilated pupil, fully abducted eye, fixed pupil, infarct of unilateral occ lobehomonymous hemianopsia/hemianopia; Duret hemorrhages due to downward brainstem compression Brainstem compression: central herniation or rostrocaudal deterioration Compresses medullary respiratory centers leading to death
Cerebellar Tonsil Herniation Midline shift Central Herniation Rostrocaudal deterioration
Lateral displacement of diencephalon may produce decreased level of consciousness Supratentorial Small reactive pupils (loss of sympathetic), Dilated, fixed (loss CNIII parasympathetics because the parasympathetics travel in the space occupying PERIPHERY of CNIII), Midposition, fixed: compression of both III and midbrain (loss of sympa/para) mass; downward Duret hemorrhages may also occur displacement of Changes in consciousness (drowsiness, stupor, coma), resp changes; postural changes: Decorticate rigidity (leg extension/arm brainstem flexion); Decerebrate rigidity (leg/arm extension) *Cheyne-stokes in diencephalon *Central neurogenic hyperventilation in midbrain *Apneustic Respiratory in pons *Ataxic Respiratory in medulla * In infants, skull may expand and in elderly, brain may have atrophied due to old age, so may have more room for expansion. Infections involving Nervous System Etiologic Agents Pathogenesis Clinical Features Spinal Notes Fluid Changes Epidural/Subdural Abscess or Pyogenic bacteria: Direct inoculation or spread from nearby infection Localized collection of Complications: Empyema step, staph pus Hydrocephalus Meningitis Bacterial Homogenous spread Purulent exudate in SAS w/ Hydrocephalus, edema P Edema from body to brain; PMN, bacteria, vasculitis; Edema, ICP, seizures, glucose CN palsies Pyogenous direct inoculation, cellular infiltration of CN/sp thrombosis, abscess, protein Thrombosis direct spread roots CN palsies cells Brain abscess Viral Aseptic Normal P Seizures Acute Lymphocytic Normal glc
Fungal Chronic
Viral Encephalitis
Candidiasis, Cryptococcus, tubercle bacillus, T. pallidum (syphilis) Depend on age, location of pt, time of year
Exudate, mononuclear infiltrate, vasculitis Granulomatous Meningoencephalitis, encephalomyelitis Homogenous spread after viremia, spread along nn Arthropod-bourne VE Epidemic; 10% by arbovirus HSV Type 1 Tx w/ acyclovir, effect mood, memory, behavior HSV Type 2 Meningitis or encephalitis Rabies Negri bodies: inclusions in pyramidal neurons of hippocampus VZV shingles granulomatous arteritis infarcts CMV common in opportunistic viral pathogens in HIV pts Poliomyelitis infect antierior horn neurons, motor deficits, flaccid paralysis Intracerebral inflammation called granulomas Homogenous spread; caused by acute bacterial endocarditis, cyanotic congenital heart disease; Discrete lesions w/ liquefactive necrosis, with zone of fibrous tissue Infiltration of meninges & vessels by lymphocytes/ plasma cells Atrophy, loss of cortical neurons in frontal lobes, gliosis, prolif microglial cells, perivasc lymphocytes, spirochetes Perivascular cuffing, neuronal/hemorrhagic necrosis, microglial nodules/proliferation, inclusion bodes
protein cells P glc ptn cells
RBCs present
Intracranial Abscess
Pyogenic bacteria (Staph/strep)
Progressive focal deficits, gen signs of increased ICP
pressure, few cells, WBC/ptn; normal glc
HIV-associated CNS Meningovasculitis Syphilis General Paresis
Meningitis, or vascular occlusion; similar to low-grade meningitis or stroke Mental changes, progressing to dementia, headache
Lightening pains, sensory deficits, loss PT/MVP; argullrobertson pupils Progressive Multifocal In pts w/ Viral encephalitis Intellectual Normal Death in 2-6 Leukoencephalopathy associated Latent infection of polyomavirus in kidney/B deterioration and mos immune lymphocytes dementia, visual, motor supp/chronic dis Demyelination; inclusion oligodendroglia nuclei dx, abnmvmts SubacuteSclerosingPanencepha Progressive Persistent but nonproductive infection of the CNS by Intellectual gamma Death in litis (SSPE) encephalitis altered measles virus; inclusion bodies in deterioration, seizures, globulin several years associated with oligodendroglia, neurons, astrocytes, perivascular spasticity of limbs, Ab titer altered measles cuffing, neuronal loss, gliosis, demyelination progressive personality against virus changes mealses CNS development dx, including malformations, perinatal brain injury, cerebral palsy Pathology Causes Clinical Features Types Diagnosis Cerebral Palsy Intraparenchymal Asphyxia, maternal high Ataxia/athetosis, Spastic: increased m tone; Correctly diagnosed bet 12-24 hemorrhage originating bp. Diabetes, trauma, dystonia, paresis, stiff/jerky mvmts mos in germinal matrix infarctions, hemorrhages spasticity Ataxic: decreased m tone/ -floppy/limp body OR stiffness of arms/legs in 1st few mos poor coordination -no smile by 3 mos Athetoid: due to -poor head control at 3-4 mos hyperbilirubinemia; cant -no sit up by 8 mos hold selves upright -difficulty standing at 12 mos -inability to walk by 18-20 mos Germinal Matrix Subependymal matrix hemorrhages; due to cerebral hypoxia between 25 th and 35th week of gestation Hemorrhage (Intraparenchymal) Periventricular Infarcts occur in the periventricular white matter; cyst may form Leukomalacia Chalky yellow plaques of discrete regions of white matter necrosis and calcification Ulegyria Due to ischemic lesionssulci bear the burnt of injury thinned-out, glioticgyri Cerebrovascular Diseases Epidural Hematoma Subdural Hematoma Disease Location/Etiology Pathogenesis Notes Stroke Ischemic 1% of head trauma admin; Bilateral in 10% of cases; Thrombosis 4:1 male to female; rare b4 more common in elderly Embolism age 2 & after age 60 Hemorrhagic Acute: Chronic: SAH, ICH Trauma, Infants, contusion elderly, dev Hypoxic Pyramidal cells of hippo, Decreased bld flow, anoxic poisons Man in barrel Death may occur 2-12
Tabes Dorsalis
Inflammation of meninges in SAS/dorsal n roots; wallerian degeneration
Encephalopathy (border zone: watershed infarcts) Focal Cerebral Ischemia Thrombotic Due to focal cerebral arterial occlusion Pale Infarct Non-hemorrhagic
pukinjie cells of cerebellum, GP neu Atherosclerotic plaque formation, coagulability of blood, vasc occl, ateriopathy, cerebral amyloid angiopathy, drug abuse, aneurysm
(CO, CN, CS2, hypoglycemia)
syndrome
hours after injury; causes uncal herniation or dnwd
over mos, dementia
Ischemia due to Embolism Thrombotic embolus in MCA Venous or Dural Sinus Thrombosis Spontaneous INtraparaencymal Hemorrhage
Sudden onset of focal impairment
Gross Path: 6-12hrs: no lesion discerned. 48 hrs: tissue pale, soft, swollen, gray-white matter jxn indistinct. 2-10 days: gelatinous, friable. 10d-3wks: tissue liquefies Micro Path: 12hrs: neu nuclear pyknosis, cytoplasmic eosinophilia; 1-3days: PMN, cap prom, endo swell, vacuolation of white matter. 3-5days: m appear. 7-21d: astrocytes proliferate, gemistocytic Shrinkage, distortion of structures, cysts, compensatory ventricular enlargement Ischemic neu (eosinophilic/red neurons); capillary prominence, vacuolation of white matter, macrophages, astrocytes become gemistocytic Hemorrhagic infarction; characterized by petechial hemorrhages
Skull fracture rupture of MMA-rapid bleeding mass effect Unconsciousness, lucid interval, coma, focal signs, ICP, death may occur 2-12 hrs due to herniation; obtundation, contra hemiparesis, ipsi pupillary dilation
Aneurysms Berry/Saccular/ Congenital Vascular Malform. AVM
Blood stasis in large vv/venous sinuses leads to infarction; increased pressure disrupts capillaries causing blood to enter infracted areas Hypertension; others are Arteriolosclerosis ; thickening of AV malformation, vessels, hyalinization, form of sm ruptured aneurysm, aneurysms; Charcot-Bouchard amyloid angiopathy, Aneurysms leukemia Uncal herniation-brainstem --basal ganglia/thalamus compression & 2 Duret brainstem and pons and cerebellum hemorrhages Occur at bifurcations of Rapidly developing severe headache Common cause of vessels at base of brain SAH
Shearing of bridging veins; accum around parenchymal laceration; 2 to accdeceleration injury No lucid interval Nonlocalizing, headache, confusion, progressive neurologic deteriation Chronic: seizures, headache, confusion, behave changes, signs of ICP Crescentic mass of high attenuation, may cross sutures; do NOT cross midline; less dense than EDH, but high density on CT Remove blood & associated organization tissue
Biconvex high density; sharply defined; rarely cross sutures, may cross midline & tentorium
AV Shunt Lacunes Infarcts
Tangles of abnormal vessels Seizure, headache, focal neurological signs Causes high output cardiac failure; generally involves vein of Galen and MCA or PCA Small infarcts, associated with HTN ; tissue loss with scattered lipid-laden macrophages and surrounding gliosis
Slit Hemorrhages Hypertensive Encephalopathy
Rupture of penetrating arterioles small ICH resorption leaving slit-like cavity Rapidly evolving syndrome of severe HTN Headache, nausea, & vomiting
Epidemiology/ Demographics Etiology
General Features Clinical manifestations/ course
Diagnosis
Seizures 3% of all ppl living to age 80 will be diagnosed w/ epilepsy; highest incidence in young children and elderly ; 70% well controlled w/ meds, 30% w/ intractable epilepsy Newborn Asphyxia, intracranial hemorrhage, hypocalcemia, hypoglycemia, hyperbilirubinemia, water intoxication, inborn errors of metabolism, trauma Infancy Febrile (5 mos-5 yrs), CNS infection, trauma, congenital defects, inborn errors of metabolism Childhood Trauma, CNS infection, arteriovenous malformation, congenital defects, tumor Adolescence Trauma, CNS infection, tumor, arteriovenous malformation, drgus/alcohol Early Adulthood Late Adulthood Drugs/alcohol, trauma, tumor, vascular disease, degenerative disease, CNS infection Generalized Seizures Partial Seizures No aura, postictal confusion (not in absence/myoclonic Simple: no alteration in level of consciousness, no postictal state seizure); may have bowel or bladder incontinence, tongue Complex: alteration (not loss) in LOC; may have aura, postictal confusion trauma Tonic m. rigidity (extension or flexion) Motor Tonic or clonic, versive head or eye movements Clonic Gen. m. jerking activity Sensory Positive phenomena: parasthesias/dysesthesias, visual halllucinations Tonic-Clonic Rigidity followed by jerking; ictal scream; Autonomic/ Gustatory, olfactory, epigastric fullness, nausea, pupillary Grand mal apnea may appear Visceral changes Atonic Bried loss of m. tone fall or head drop Psychic Dj vu, jamais vu, depersonalization Petit mal Absence Staring spell 5-15 sec; provoked by hyperventiliation (only in childhood); no postictal Myoclonic Localized/widespread jerking mvmts; infantile, juvenile CT or MRI, EEG, hematology (CBC, electrolytes, Ca, Phosphate)
Primary Tumors
More in adults than in children
Usually supratentorial; can spread via CSF, but no spread beyond CNS
Children ICP may be only sign presented
Intracranial Neoplasms Pilocytic astrocytoma Medulloblastoma Most common Ependymoma Retinoblastoma Neuroblastoma Gliomas Astrocytomas Grade 2: diffuse Grade 3: anaplastic Grade 4: glioblastoma Oligodendrogliomas Ependymomas Primary Brain Lymphoma Germ Cell Tumors Pineal Parenchymal Tumors Meningiomas
Adult 50-75% are primary
Cystic lesion with mural nodule of tumor; good prognosis; grade 1; in cerebellum Grade 4; usually in cerebellum; poorly differentiated neoplasm; truncal ataxia, ICP; seeding thruout SAS; mitotically active prognosis: gloomy Mostly in 4th ventricle; due to ICP; solid tumor, true ependymal rosettes Sometimes bilateral, may extend to optic n; good prognosis PNS, often in adrenal gland; poor prognosis Cerebral hemispheres; low grades=firm, white/gray, poorly circumscribed, infiltrates & distorts brn tissue; grade 3-4: well circumscribed, infiltrates widely, many colors due to hemorrhage, necrosis, &cysts Often in cerebral hemispheres; fried egg appearance; slow-growing tumor Within skull are rare; often in lateral ventricles more common in the spinal cord From B lymphocytes in CNS to deep cerebral hemispheres headache, seizures; soft, multiple separate nodules Origin: ectopic germ cells; location: midline (pineal/suprasellar region); good prognosis Clinical effects: visual disturbances and headache Well-circumscribed mass, no invasion; whorls or sheets of meningothelial cells, psammoma bodies
Metastatic Tumors
Intra-Axial Tumors
Extra-Axial
Frequently multiple, distributed by volume, supratentorial Meningioma Metastasis Schwannoma Neurofibroma Astrocytoma
Spread via CSF
Grade 2: nuclear pleomorphism (solid, infiltrating, may show
Survival over 5 years is rare
Tumors
Diagnosis VonHippelLind au Syndrome Hemangio blastoma Neurofibro matosis I Neurofibro matosis II Tuberous Sclerosis
Ependymoma Oligodendrogli oma Metastasis Always cranial MRI with gadolinium enhancement Mutation in tumor Multiple CNS hemangioblastomas Increased renal cell carcinoma
cystic change Grade 3: plus mitotic activity Grade 4: Glioblastoma: Necrosis with palisading, and/or vascular endothelial proliferation; may show hemorrhage Usually in spinal cord in adults (4th ventricle in children) Can be associated with loss of chromosome 1p and 19q
Prognosis related to resectibility
Thin-walled vessels w/ vacuolated cells; cystic lesion with mural nodule usually in cerebellum; 10% of patients have polycythemia when tumor cells make erythropoietin Mutation in Chromosome 17; peripheral neurfibromas may show malignant degeneration; pilocyticastrocytomas (optic nerve) Multiple meningiomas& bilateral acoustic schwannomas, ependymoma, mutation on chromosome 22-merlin protein Cortical tubers, angiomyolipoma of kidney, renal cell carcinoma, renal/hepatic cysts
Disease Clinical Features Hypokinetic Movement Disorders Parkinson Rigidity, gait instability, resting Disease tremor, bradykensia --mood dx, later dementia, dysautonomia --olfactory dysfxn, constipation, autonomic, dysfxn, sleep dx, dep/anxiety
Pathology
Movement Disorders Epidemiology 11/100,000 in general population 50/100,000 over age 50 Cumulative lifetime risk: 2.7%; Slightly more common in men Risk Factors: age, severe head trauma, family history, env exposure, low uric acid Protective factors: estrogen, caffeine, heavy alcohol, smoking, NSAIDS
Differential Diagnosis Secondary Parkinsonism Other Tremor Syndromes Akinetic-Rigid Syndromes Drug-induced, post-traumatic, post-infectious, immune-mediated, vascular, normal pressure hydrocephalus Essential, myoclonic, dystonic
Degeneration of pigmented brainstem neurons in substantianiagra, lewy bodies, Da in striatum
Hereditary disorders w/ Parkinsonism
Progressive Supranuclear PalsyAccumulation of hyperphosphorylated tau ptn in neuronCBT/CST signs, wide unblinking face, axial rigidity, dn gaze paresis Multiple System Atrophy Cerebellar signs, dysautonomia, CST signs, stridor Corticobasal Degeneration Progressive asymmetric rigidity, apraxia, alien limb, rarely gaze palsy Diffuse Lewy Body Disease Wilsons: AR, deficient copper excretion, serum/urine copper hepatic failure, basal gangliaakinetic-rigid, wing-beating tremor Huntingtons
Hyperkinetic Movement Disorders Tremor Repetitive rhythmic alternating contractions of agonistic/antagonistic muscles: terminal, resting, postural/action, wing-beating tremor Dystonia Sustained and/or phasic contraction of m causing abnormal posture or repetitive movements Myoclonus Rapid, lightning-like m contraction producing irregular jerking Chorea Brief, irregular jerking movements flowing from on body part to the next (metabolic, auto-immune, degenerative, vascular, drugs) Huntingtons Disease: expansion of CAG: chorea, dementia, psychiatric, cerebellar features, prominent atrophy of caudate nuclei Hemiballismus Rapid, large amplitude, unilateral, proximal flinging movements Tics Repetitive, stereotypic, brief semi-involuntary movements
Disease Multiple Sclerosis Autoimmune Dx
Neuromyelitis Optica (Devic Dis) Acute Disseminated Encephalomyelitis Acute Necrotizing Hemorrhagic Encephalomyelitis Central Pontine Myelinolysis Three Vital Signs Glaucoma Optic Neuritis Giant Cell Arteritis
Demyelinating Diseases Etiology & Pathogenesis Pathological Changes Diagnosis CD4 TH1, TH17 cells react Initially: Optic neuritis MRI, CSF analysis : oligoclonal against self-myelin Ag & Plaques of demyelination in bands, IgG secrete cytokines, B cells, T white matter of brain/sp cd, not CSF: gamma globulin elevated, cells, & innate immune oligoclonal gamma globulin PNS; # of oligodendrocytes, systemdemyelination bands gliosis, activation of microglia and macrophages Remitting and relapsing Development of both optic neuritis and spinal cord demyelination at similar points in time Age of Onset/ Epi Age of onset: 2050; more common in women and Caucasians 30-300/100,000 Rapidly progressive diffuse demyelinating disease, develops 1-2 wks after viral infection Demyelination in perivenous distribution Common in young adults and children, usually in upper resp infection; CNS demyelination Demyelination in basis pontis and pontine tegmentum; classically associated with rapid correction of hyponatremia Visual System Disorders Visual acuity, Pupils, Pressure
Treatment Ag non-selective immunomodulators : copaxone, inhibits myelin basic protein (MBP)
Headache, jaw claudication, weight loss, malaise A true neuro-ophthalmic emergency Vestibular System Disorders Central Causes Vertigo, diplopia, weakness, and/or numbness TIA not only vertigo, but combo of diplopia, dysarthria, numbness, incoordination Tumor or mass rarely with isolated vertigo; tx w/ traditional prophylactic migraine meds Migraine
Traumatic Optic neuropathy Disease Vertigo Sensation of movement of self/env, often rotary. Mismatch of visual, vestibular, & sensory proprioception Clinical Features Nystagmus, (hallmark) Peripheral Causes Vertigo, hearing loss, tinnitus Benign Paroxysmal Positional Vertigo Vestibular most common cause of vertigo; Dix-Hallpike testing (pt rapidly moved from seated position to lying position Vestibular Neuritis monophasic episode of vertigo; days to weeks, nausea/vomiting; tx w/vestibular suppressants (meclizine, diazepam, Dramamine, lorazpam) Menieres Disease endolymphatic regulatory dysfunction; last hours; ear pressure/fullness, change in tinnitus & hearing
Etiology Concussion Contussion Diffuse Axonal Injury Spinal Cord Lesions (Direct v. Indirect) Trauma
Multiple Sclerosis important cause Nervous System Trauma Clinical Manifestation Transient acute unconsciousness, headache, cognitive and sleep disturbances, vertigo Areas of hemorrhagic necrosis, Brain moves linearly or rotates, slam into skull Located in deep white matter regions, Diffusion of tensor imaging Sensory loss of sensation in a specific dermatone indicated location of lesion Headache Characteristics
function Trauma Notes Not an anatomic lesion No evidence of permanent structural damage Coup lesions, counter coup, intermediary lesions Major cause of prolonged traumatic coma, and poor neurological outcome Macrophages, gliosis, loss of architecture Contusions, Wallerian degeneration
Trauma most common: orbital gyri, temp/occ pole Trauma; present in 35% head trauma deaths Blow to back of neck or trunk Trauma to C4, C5, C6, C7, T1 or T12, L1, L2 Epidemiology Duration of Episode 30 min-7 days
Location Bilateral
Treatment Regular meals, hydration, rest, remove stress, anxiolytics Abortive Preventive NSAIDS, Anti-depressants, antihistamines, anti-convulsants, -adr blockers, adr blockers, occ/supraneuroleptics orbital n block Ergotamines, Lithium, topiramate, lidocaine, ergotamine prednisone, verapamil, sodium 100% O2, valporate sumatriptan NSAIDS, salicylates Doesnt respond to O2
Tension
Both genders Age 20-60 Female Age 20-50
Migraine
No aura: 4-72 hrs Aura: 2 or more attacks
Progresses throughout day, no aura, no phonophobia/photophobia, no N/A, pulsating, tightening, pressing, no aggravation by exertion Can be with or w/o aura Aura: N/V, photophobia, phonophobia
Unilateral
Cluster
Male
Histamine mediated Eye swollen and red, lacrimation, ptosis, miosis, eyelid edema, nasal congestion, rhnorrhea, facial sweating No frank Horners syndrome; extremely responsive to indomethacin
Unilateral
Paroxysmal hemicrania
Female
Vascular Giant Cell (temporal) Arteritis Trauma-associated Intracranial Disorders Metabolic Cranial Neuralgias
Secondary Headaches Sentinel bleed (AVM, SAH), stroke, arteritis, carotid/vertebral dissection, venous/sinus thrombosis, arterial hypertension Sentinel Thunderclap Headache: worst headache of life, ruptured aneurysm Older patient Achiness in jaw, neck, palpate artery, get sed rate, CRP Subdural hemorrhage, SAH, concussive, post-concussive Increased ICP w/ mass, benign intracranial HTN, intracranial infection, low ICP even Hypoxia, hypercapnia, hypoglycemia, dialysis; non-cephalic infection, facial pain Trigeminal Neuralgia Severe pain in face, stabbing electric shockTx: Carbamazepine, gabapentin, lamotrigine, Tic Douloureux like pain baclofen; Surgery: rhizotomy, microsurgical decompression, gamma knife 2 to compression/inflammation of CN V Glossopharyngeal Neuralgia Lancinating pain referred to tongue, ear Anticonvulsants, microsurgical decompression 2 base of skull lesion, neck mass, vasc compression Occipital Neuralgia Aching pain, referred over scalp Unilateral Anticonvulsants, occipital n branch block, microsurgical decompression 2 to cervical trauma, arthritis, C1-C2 Drug overuse, non-compliance, somatization, anger/anxiety, family dysfunction Discontinue offending analgesics, EDUCATE, hydrate, preventive pharmacotheraphy Toxic, acquired metabolic, and nutritional dx of the CNS Source or Clinical Effects Notes Deficiency Paints chips or paint CNS: in cerebral or cerebellar cortex dust in homes -Acute: seizures, ataxia, ICP -Chronic: seizures, attention/mental deficits, loss of motor skills PNS: in motor nn segmental demyelination; wrist-drop, slowed n conduction Vapor Inhaled dental Negligible analgams Methyl Fish Visual field constriction & ataxia Ethyl Thimerosal in No evidence of damaging effects vaccines Insecticide Miosis, blurring vision, chest tightness, wheezing, GI, increased Tx w/ Atropine sweating, increased salivation Workplace Organic affective syndrome: irritability, fatigability, difficulty in concentrating, loss of interest Mild chronic toxic encephalopathy: personality or mood change, impairment in intellectual function
Rebound
Lead Motor peripheral neuropathy
Mercury
Organophosphate Insecticide Organic solvents
Botulinun Toxin
Clostridia
Tetanus
C. tetani Soils and spores Ventilation of heating sources, engine exhaust Direct effects or 2 nutritional deficits
Carbon Monoxide Methanol Toxicity Ethanol
Radiation Wernickes encephalopathy & Korsakoffs syndrome Thiamine, vitamin B1 deficiency
Severe chronic toxic encephalopathy: dementia with global deterioration of memory & other cognitive functions Mechanism of Action Clinical Effects Cause deficiency of synaptic Nausea, dry mouth, double vision, transmission; must enter weakness, difficulty speaking and axon terminal; prevent swallowing; symmetrical flaccid synaptic vesicles from paralysis docking/fusing w/ presyn term Tetanospasm; inactivates Lock jaw, opisthotonos synaptobrevin (block synaptic transmission that normally inh MN Form carboxyhemoglobin Headache, myalgia, dizziness, neuronal necrosis, and neuropsychological impairment apoptosis confusion, loss of consci, death Degeneration of retinal ganglion cells blindness Effects are reversible; atrophy and loss of granule cells 1 in anterior vermis Unsteady gait and nystagmus Symptoms of intracranial mass, headaches, nausea, vomiting, papilledema Large areas of necrosis and adjacent edema Wernickes Encephalopathy: ataxia, confusion, ophthalmoplegia Korsakoffs pyschosis: severe memory defects and confabulation Pathological changes: vascular changes, capillary tortuosity, prominence, endothelial swelling, petechial hemorrhage, neuronal damage, macrophage response and gliosis Numbness, paresthesias, weakness Degeneration of both myelin & axons w/ axonal reaction in anterior horn cells Peripheral neuropathy, optic neuropathy; associated with pernicious anemia Loss of MVP, LE weakness, DTR, babinski signs; degeneration of post/lat columns Spongy degeneration of white matter Hypoalbuminemia is a cause Anoxia, acidosis Amidation of glutamateglutamine via glu synthetase takes place in
Located in mammillary bodies , periaqueductal gray
Alcoholic Polyneuropathy Subacute combined degeneration Vitamin B12 deficiency
Kernicterus Hepatic encephalopathy
Bilirubin toxicity
Neuronal Storage Diseases Leukodystrophies Mitochrondrial Encephalomyopathies Common Sphingolipidoses Tay-Sachs Disease (type of Neuronal Storage Disease) Metachromatic Leukodystrophy Krabbe Disease
Location Gray matter Myelin and white matter Gray matter and skeletal muscle Age of Onset 3-8 mos Early childhood 3-6 mos
astrocytes Brain edema, disturbances in consciousness & motor abnormalities (pre-dominately involves glial Alzheimer type II cells in gray matter Inherited Nervous System Metabolic Diseases Deficit Result Genetic inheritance Clinical Expression Lysosomal enzyme Accumulation of Autosomal recessive Can range from focal (usually) enzyme substrate abnormalities to mental retardation Variety of clinical Autosomal recessive expression Oxidative Mitochondrial encephalopathy lactic acidosis phosphorylation stroke-like episodes Accumulated Product GM2 gangliosides Sulfides Galacto-cerebroside Clinical Signs Psychomotor arrest, exaggerated startle reflex, seizures, cherry red spot Progressive mental and motor deterioration, peripheral neuropathy signs Mental and motor deterioration, seizures, irritability, crying Pathology Storage in central and peripheral neurons Myelin deficit in CNS/PNS, storage in glia Myelin deficit; globoid cells (large nucleated macrophages)
Enzyme Deficiency Hexosaminidase A Cerebroside sulfatase Galacto-cerebrosde -galactosidase
Alzheimers Disease
Age of Onset >60 years Early: 40-60
Location of Lesions Cortex, hippocampus, entorhinal, perirhinal cortex, basal forebrain Subcortical areas and substantia nigra Frontal and temporal lobes
Degenerative Diseases Clinical Features Memory loss, dementia Gait normal, no focal weakness or sensory loss
Gross/Microscopic Pathology Accumulation of tau, amyloid, neuritic bodies (extracellular), neurofibrillary tangles (intracellular) Presenilin 1: chromosome 14; age 30-50 onset Presenilin 2: chromosome 1; age 30-65 onset Amyloid Precursor ptn: chrm 21; age 40-60 Apolipoptn E (e4 carriersmore amyloid plaques) Lewy bodies with -synuclein and ubiquitin Faster progression/shorter survival knife-blade like atrophy of frontal and temporal lobe
Diagnostic Tests Neuritic bodies, neurofibrillary tangles
Dementia with Lewy Bodies (DLB) Frontotemporal Lobar Degeneration
Elderly Late-middle/ elderly
Dementia plus 2 of 3: parkinsonism, hallucinations, or fluctuating alertness/attn Similar to Alzheimers Behavioral changes most prominent , perseveration, decreased verbal
Sensitive to antipsychotic meds Inclusion bodies with tau fibrils in neurons
(Picks disease) Huntingtons Disease Wilsons Disease (hepatolenticular degeneration) Amyotrophic Lateral Sclerosis Spinocerebellar Ataxias
30-50 years
Caudate, putamen, GP, cortex Liver, brain, and eye Ventral horns, cortical atrophy in precentral gyrus Cerebellum
fluency Behavioral, cognitive changes and/or movement dx, esp chorea Liver dysfunction Mvmt dx (dystonia) Behavior/cog changes Gradual weakness w/ no sensory deficit
Gain of function of Huningtin gene CAG expansion; extensive gliosis Inborn error of Cu metabolism accumulation of Cu in liver, brain, eye Degeneration of BOTH UMN/LMN. Neurogenic atrophy
atrophy of caudate nucleus w/ ventricular dilation
10-30 years Middleaged/ elderly Mean age: 11
Creutzfeldt-Jakob Disease (CJD) Familial Fatal Insomnia Variant Creutzfeldt-Jakob Disease (vCJD) Disease Delirium Think: metabolic, toxic, aseptic, increased ICP Dementia Think Alzheimers or vascular dementia Vascular Dementia
Friedreich ataxia, hand clumsiness, Trinucleotide expansion in intron sensory deficits, progressive deterioration Prion diseases Age of Onset Location of Lesions Clinical Features Gross/Microscopic Pathology Diagnostic Tests 10% Polymorphism at codon Rapidly progressive Cortical atrophy and ventricular CSF 14,3,3 protein inherited 129 with Val; dementia and startle dilation, spongiform encephalitis MRI changes myoclonus (some ataxia) Polymorphism at codon Insomnia Neuronal loss, and gliosis in specific thalamic nuclei and 129 with Met inferior olivary nucleus Cortical plaques with surrounding halo of spongiform change; mad cow disease
Dementia and delirium Clinical Features Diagnosis Agitation, acute, inconsistent, fluctuating alertness, Acute onset & fluctuating course, hallucinations, inattention inattention, disorganized thinking, altered Widespread reduction in cerebral oxidative LOC metabolism; failure of cholinergic metabolism Chronic, progressive, memory loss, alert/attn ok, disorientation, constructional apraxia Focal motor, sensory, or reflex changes, sudden and/or multi-stepwise decline; focal cognitive impairments (visuospatial disturbance + aphasia) Neuropathology: neurofibrillary tangles/neuritic plaques in AD; lewy bodies in PD/DLB; structural/functional imaging, biomarkers (amyloid) Imaging: infarcts; ischemia
Treatment Prevention, treat underlying illness, antipsychotics, supportive care Contraindications: benzodiazepines, sedative-hypnotic, anti-cholinergics, drugs of parkinsonism, narcotic analgesics, histamine-2-receptor blockers
Atypical Vascular Dementia: insidiously progressive; not stepwise showing extensive confluent white matter
Normal Pressure Hydrocephalus Dementia associated with Movement Disorders Infectious causes
Gait disorder, urinary incontinence, dementia (triad); enlarged ventricles
abnormalities on T2 and FLAIR imaging 70% respond to shunting
HIV-associated Dementia (HAD) Can be somewhat reversible
Drug Cocaine
Lidocaine
Ester/Amide Estermetabolized by pl/hepatic cholinesterases AmideWeak bases; insoluble to water Metabolized by liver P450
Potency Low
Intermediate
Bupivicaine Mepivicaine Procaine (Novacain) Tetracaine Epinephrine
High Intermediate Low
Local Anesthetics Mechanism Topical Uses Blocks voltageLaryngeal, nasal gated Na surgery, UG channels by prolonging their inactivation Dermal (Shingles, state rash), laryngeal, oral (prevent Cation is active ventricular form arrhythmias) None Non-ionized form cross into m. None None
Parenteral Uses None
General uses Topical (lidocaine) Infiltration
Adverse Effects CNS: restlessness, dizziness, confusion, circumoral paresthesis, tinnitus, tremors, seizures CV: bradycardia, hypotension, heart block, cardiac arrest Peripheral neurotoxicity, hypersensitivity reactions, ester typesPABA (sensitizing)
Epidural, infiltration, nerve block, spinal Epidural, infiltration, nerve block, spinal Epidural, infiltration, nerve block, spinal Infiltration, nerve block, spinal anes Adjunct for local vasoconstriction;
Nerve block & field block Spinal/Epidural anesthesia
Should not be used in areas of end aa (fingers, nose, penis and toes) ears too Adverse Effects Explosive, airway irritation, stable CV response
Drug Diethyl ether
Mechanism of Action Correlation between lipid solubility/potency Potentiate GABA effects; hyperpolarization & excitability due to Clinflux and K efflux
Specific Actions
General Analgesics Potency
General uses Stages: I: analgesia II: delirium III: surgical analgesia IV: meduallary depression
Chloroform Nitrous Oxide (laughing gas) Desflurane Loss of consciousness & analgesia due to disruption of neuronal firing & sensory Fast induction and elimination Decrease vascular resistance, not CO High MAC, not metabolized MAC 6 Hypnosis Homeostasis Analgesia Amnesia
Arrhythmogenic, hepatotoxic, well tolerated Autonomic instability Hypothermia Cardiac
Enflurane Propofol IV
processing in thalamus Reduced motor activity due to inhibition of neuronal firing in layer IV of cerebral cortex
Decrease CO; produce bronchodiliation Facilitate effects of GABA at GABAClionophore
MAC 1.7 Rapid emergence, less confusion compared to thiopental
Muscle relaxation HHAAM Hypotension, resp depression, reduce cerebral bld flow/ ICP ; not analgesic, not amnestic if conscious, antiemetic Unconsciousness slower in onset, longer than thiopental Increased HR, BP, ICP and sympathetic tone
dysrhythmias Nausea Vomiting Delirium 1/250000 estimated deaths
Midazolam IV
Facilitate effects of GABA Produce amnesia
Less respiratory depression than propofol/thiopental, little effect on CVS Cause analgesia, sensory perception, immobility and amnesia Lower MAC
Ketamine
Blocks NMDA receptors Dissociative anesthesia dream-like w/o loss of consciousness
Thiopental Produce CNS, resp, IV CV depression The Ideal Anesthetic: potent, non-irritating, noninflammable, not toxic, not metabolized, not arrythmogenic, stable cardiovascular response, very slightly soluble in water, quite soluble in oil, unable to trigger malignant hyperthermia, stable in soda/lime, not harmful to metal fittings, potent m relaxant Anticonvulsants Drug Mechanism of Metabolism Clinical Use Drug-Specific Adverse Effects Common Adverse Action Effects Phenytoin Na ch blockade Hepatic- P450 Partial seizures, Ataxia,nystagmus, drowsiness, lethargy, Fatigue (Dilantin) system generalized seizures nausea, vomiting, rash, gingival hyperplasia, Dizziness blood dyscrasias Ataxia Diplopia Carbamazepine Na ch blockade P450; induce own Partial seizure; avoid in Dizziness, diplopia, nausea, ataxia, blurred Nystagmus (Tegretol) metab; primary generalized vision, aplastic anemia, agranulocytosis, epoxidation to seizures thrombocytopenia, Stevens-Johnson syndrome 10,11-epoxide Oxcarbazepine Na ch blockade Hepatic- induces Seizures Dizziness, nausea, headache, drowsiness, (Trileptal) hepatic enzymes ataxia, diplopia, fatigue, and nervousness; hyponatremia Ethosuximide Inhibits T type Cach Absence seizures only Nausea, GI, anorexia, wt loss Pregabalin Unknown- potential Renal excretion Adjunct to partial Confusion, edema, wt gain, typical side effects (Lyrica) effect on -2 seizures
Ketamine: trauma victims, sedation of children; coadmin w/ benzodiazepine to prevent delirium and hallucinations
Levetiracetam (Keppra) Valproic acid (Depakote) Gabapentin (Neurontin) Lorazepam Lamotrigine (Lamictal) Topiramate (Topamax) Zonisamide (Zonegran)
subunit of Cach Unknown Enhances GABA; modulate VG Na ch, inh T type Cach Enhance GAD; binds -2 subunit of C ach Na ch blockade Unknown Not completely understood; T- type Ca channels, Na channels, carbonic anhydrase inhibition
Renal excretion HepaticGlucuronidation Renal excretion, not metabolized HepaticGlucuronidation Renal and hepatic elimination Renal excretion
In combo with other AEDs Primarily generalized epilepsy- 1st line Partial seizures, neuropathic pain Partial and generalized seizures Multiple seizure types Adjunct tx for partial seizures
Somnolence, fatigue, ataxia, behavioral abnormalities; rare decrease in Hb& erythrocyte count Nausea, tremor, sedation, confusion, wt gain, hair loss, acute pancreatitis, bone mar sup, rash, hyperammonemia (fat, bald, & shaky) Somnolence, dizziness, nystagmus, ataxiz, fatigue, weight gain Ataxia, dizziness, diplopia, N/V, Stevens Johnson; 1% child/0.3% adults Somnolence, dizziness, ataxia, difficulty w/ memory, speech/langdysfxn, diplopia, aggressive behave, anorexia, renal lithiasis Somnolence, ataxia, dizziness, fatigue, renal lithiasis, anorexia
Phenobarbitol Drug Endophins Enkephalins Synthesis Or Distribution Arcuate nucleus & ant. pit Synthesized in small interneurons Found in Periacqueductal grey, lamina I/II Brain; often together w enkephalins Papaversomniferum Contraindications: Types Opioid Analgesics Agonistic Action General uses Mu/delta receptors LeuMetMu/delta receptors Adverse Effects Actions Mediated by Receptor Subtypes Analgesia: mu, kappa, delta Feeding: mu/kappa/delta GI fxn: mu/kappa Sedation: mu/kappa Psychotomimesis: Kappa Diuresis: kappa Resp fxn: mu
Dynorphins Morphine
A, B, alpha-neoPharmacokinetics Well abs; high 1st pass effect; conjugate to
Kappa receptors Mu/kappa/delta Inhibit adenylcyclase Clinical Use: PAIN: post-operative, acute MI, renal/biliary colic CV: myocardial O2 demand, vasodilation, hypotension, ICP
Major: head injuries, seizures, alcohol intoxication Relative: asthma, renal insufficieny, history of opioid abuse, liver disease
glucuronide in intestines/liver Peak effect: 1 hr after inj; duration: 3-4 hrs
hyperpolarization
pain; chronic pain
Analgesia, euphoria or dysphoria, inh of cough reflex, miosis, physical dependence, resp depression, sedation *w/o loss of consciousness
GI: constipation, biliary sphincter tone/pressure, nausea/vomiting GU: bladder sphincter tone, prolongation of labor, urinary retention Overdosestupor/coma, respdep, miosis; tx w/ naloxone
Withdrawal Effects: Vomiting, chills, fever, lacrimation, diarrhea, rhinorrhea, seeking, craving behavior Occur after 8-12 hrs of last dose Occur after 3 hrs last dose Onset after 24-48 hrs last dose
Meperidine
Methadone Fentanyl Oxycodone Buprenorphine Codeine
1/10th analgesic potency of morphine; poor oral abs; equivalent respdep; miosis (mydriasis at toxic doses); high addiction liability; short duration of action; metabolized to normeperidinerisk of seizures Slightly more potent than morphine; less sedative &spasmogenic; effective orally 100x more potent than morphine as analgesic; given via IV & as transdermal patch Use in combo w/ acetaminophen (7.5mg) or aspirin (5mg) 1/10th analgesic potency of morphine; less constipation, lower addiction liability, less sedation/respdep; used orally in combo w/ acetaminophen or aspirin for moderate pain; converted to morphine by CYP 2D6 Mixed opioid agonist (kappa)/antagonist (mu) Opioid receptor competitive antagonist (mu, delta, and kappa)
Help wean off heroin addict; maintain at 40-100mg Patch: useful in chronic pain (3 days)
Resp depression, nausea, vomiting, ICP, postural hypotension, constipation, urinary retention, itching & urticarial, restlessness, tremulousness, hyperactivity
Antitussive (suppress coughing)
Nalbuphine Parenteral only Naloxone IV Naltrexone Oral Tramadol
Synthetic codeine
Treats opioid overdose; blocks effects of morphine and other drugs Opioid antagonist, mu, delta, kappa Used to prevent relapse in chronic alcoholics Non-opioid Analgesic Weak mu agonist Mild to moderate pain
No dependence liability; all others do; no constipation Longer duration of action than naloxone
Dry mouth, dizziness, sedation,
analog
Inhibit uptake of NE and 5HT
headache, seizures, abuse potential-unclear
Drug Levodopa Carbidopa Bromocriptine Ropinirole Pramipexole Selegiline Rasagiline Entacapone Amantadine Benztropine Apomorphine
Drugs for Parkinsons Disease Notes Adverse Effects 100-250mg, 3-4 times daily Nausea, orthostatic hypotension, hallucinations, dyskinesias Less effective with food High dose lead to dyskinesias (peak dose chorea, biphasic chorea, dystonia) Works peripherally to block L-DOPA-DDC DA but cannot cross BBB; decrease symptoms in periphery, no CNS effects; does not effect parkinsonism For PD, DA agonist at D2 receptors Da agonists at D2 Longer duration of action, Low standing BP, nausea, dyskenisa, hallucinations, sleepiness but not as effective as Rare; lung & cardiac valve fibrosis, leg edema, compulsive behaviors levodopa MAO-B inhibitors Mechanism L-DOPA (amino acid)
COMT inhibitor used in combo therapy Blocks NMDA, weak inducer of DA rel; can treat dyskinesias Anticholinergics; block mAch receptor; offsets the imbalance between Ach and DA DA agonist at D1 and D2 receptors Drugs for Multiple Sclerosis Drug Type of Drug Mechanism of Action Adverse Effects Interferone-beta Ag non-selective immunomodulators, proposed to act through inhibiting IFN-gamma activity Glatiramer acetate Ag selective Natalizumab Humanized monoclonal Reduce the ability of immune cells to cross BBB Progressive multifocal leukoencephalopathy Ab against cell adhesion IV molecule alpha4integrin Antithrombotic agents Clopidogrel Pro-drug, function Irreversible inhibits P2Y12 receptor which is Hemorrhage, neutropenia related to ADP receptor important in platelet aggregation and crosson platelet cell linking of fibrin by blocking the activation of membrane P2Y12 glycoprotein IIa/IIIb pathway; metabolized by CYP2C19 Aspirin Irreversibly inhibits COX 1 GI ulcers, stomach bleeding, tinnitus Drugs for Dementia
Donepezil Galantamine Rivastigmine Memantine
Cholinesterase inhibitors NMDA antagonist
Slows the breakdown of Ach by blocking acetylcholinesterase levels of Ach increase
Nausea, vomiting, loss of appetite, increased frequency of bowel movements/diarrhea
No evidence it can prevent or slow neurodegeneration Drugs for Migraine Sumatriptan Abortive for cluster and 5HT agonist; exerted in bile and urine migraine 4-6mg sc at onset for cluster H/A, poor bioavailability with oral administration, faster acting, but with shorter duration with injection Dihydroergotamine Abortive for cluster and Act on 5HT receptors (agonistic) May increase BP, coronary artery vasopasm, migraine vasoconstriction; inhibition of proMI, ventricular fibrillation inflammatory neuropeptide release Propanolol Prophylactic for migraine, Decrease frequency and severity of migraines Drowsiness, difficulty breathing, slow -adr blocker heartbeat, cold hands/feet, depression Valproic acid Prophylactic for migraine, and cluster H/A, anti-convultant Amitryptyline Prophylactic for migraine, tricyclic anti-depressant-inhibits 5HT/NE uptake Causes delirium Topiramate Prophylactic for migraine and cluster, anti-convulsant Know that the following classes of drugs can cause Delirium Anticholinergics, Opioids, Benzodiazepines, narcotic analgesics, sedative-hypnotic, histamine 2-receptor blockers
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hyponatremia Algorithm GuideDocument2 pagesHyponatremia Algorithm Guidemina000005100% (1)
- Blood Cell Morphology TutorialDocument176 pagesBlood Cell Morphology TutorialCharles Jebb Belonio JuanitasNo ratings yet
- National policies shaping communication between educators and physiciansDocument1 pageNational policies shaping communication between educators and physiciansmina000005No ratings yet
- Toronto Notes DermatologyDocument52 pagesToronto Notes Dermatologyalphabeta101100% (1)
- HypertensionDocument7 pagesHypertensionmina000005No ratings yet
- 14 - Toronto Notes 2011 - GynecologyDocument52 pages14 - Toronto Notes 2011 - GynecologyZiyad100% (4)
- Breast Cancer Resistance Research AbstractDocument1 pageBreast Cancer Resistance Research Abstractmina000005No ratings yet
- Toronto Notes 2011 PsychiatryDocument52 pagesToronto Notes 2011 Psychiatrymina000005100% (1)
- Musculoskeletal ChartsDocument27 pagesMusculoskeletal Chartsmina000005100% (1)
- Metabolic Endocrine Reproductive Domain Study PacketDocument173 pagesMetabolic Endocrine Reproductive Domain Study Packetmina000005No ratings yet
- Digestive Domain GuideDocument31 pagesDigestive Domain Guidemina000005No ratings yet
- Nina Bacteria Chart Medical School Step 1Document11 pagesNina Bacteria Chart Medical School Step 1M PatelNo ratings yet
- Nephron MapDocument1 pageNephron MapJessica MooreNo ratings yet
- Heme-Onc-Anemia Blank TableDocument2 pagesHeme-Onc-Anemia Blank TableM PatelNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Coexistena de Adenopatii Mediastinale de Etiologii Diferite - Caz ClinicDocument9 pagesCoexistena de Adenopatii Mediastinale de Etiologii Diferite - Caz ClinicConstantin PopescuNo ratings yet
- Cancer Rehabilitation AssessmentDocument21 pagesCancer Rehabilitation AssessmentLiliana Carolina Guzman RiosNo ratings yet
- Final Written ENT With CoverDocument231 pagesFinal Written ENT With CoverAlyAl-MakhzangyNo ratings yet
- The Borax ConspiracyDocument3 pagesThe Borax Conspiracyz987456321100% (2)
- Poster Number Name Country Remarks TitleDocument26 pagesPoster Number Name Country Remarks TitleAndy F Monroe0% (1)
- Avn - LatinDocument9 pagesAvn - Latinaleena jaya100% (1)
- What Is The Best Indicator To Determine Anatomic PDocument12 pagesWhat Is The Best Indicator To Determine Anatomic PjhidalgomdNo ratings yet
- AbstractsDocument92 pagesAbstractsmissrinwaNo ratings yet
- Emetogenic Potential of Antineoplastic Agents PDFDocument1 pageEmetogenic Potential of Antineoplastic Agents PDFalfox2000No ratings yet
- CWU CholedocholithiasisDocument30 pagesCWU CholedocholithiasisAthirahRaraNo ratings yet
- Radiology Imaging of Urinary TractDocument40 pagesRadiology Imaging of Urinary TractMuhammad Zaniar RamadhaniNo ratings yet
- H4K20me0 Recognition by BRCA1-BARD1 Directs HR To Sister Chromatids. Nakamura K Et Al.-Nat Cell Biol 2019 PDFDocument14 pagesH4K20me0 Recognition by BRCA1-BARD1 Directs HR To Sister Chromatids. Nakamura K Et Al.-Nat Cell Biol 2019 PDFhutten7No ratings yet
- AXR PresentationDocument30 pagesAXR PresentationLalit KumarNo ratings yet
- (Saul McLeod) Cognitive-Dissonance ArticleDocument6 pages(Saul McLeod) Cognitive-Dissonance ArticleJohn ReyesNo ratings yet
- Chapter 20 Solutions Molecular Biology of The CellDocument15 pagesChapter 20 Solutions Molecular Biology of The CellAkshey BadrinarayanNo ratings yet
- Research Ni LagneDocument8 pagesResearch Ni LagneqtiejeydNo ratings yet
- Final Coaching CLUSTER 5 Radiologic Technology Licensure Examination ReviewDocument24 pagesFinal Coaching CLUSTER 5 Radiologic Technology Licensure Examination ReviewSamiracomputerstation Kuya Marvs100% (1)
- RT PediatricDocument9 pagesRT Pediatricfaza mawaddahNo ratings yet
- Test 1 Science Form 3Document7 pagesTest 1 Science Form 3Zunaizah Yahaya100% (1)
- About Cervical Cancer: Overview and TypesDocument9 pagesAbout Cervical Cancer: Overview and TypesAlexa jaye BalinoNo ratings yet
- Prostate CancerDocument34 pagesProstate CancerKoRnflakes100% (1)
- Bank Pharmacology and Clinical Pharmacy ENGDocument99 pagesBank Pharmacology and Clinical Pharmacy ENGSh A NiNo ratings yet
- Tudor Cozma - Coordinator Prof. Univ. Dr. Elena-Carmen Cotrutz - Scientific Leader Assist. Univ. Dr. Pavel OnofreiDocument10 pagesTudor Cozma - Coordinator Prof. Univ. Dr. Elena-Carmen Cotrutz - Scientific Leader Assist. Univ. Dr. Pavel OnofreiCozma TudorNo ratings yet
- Retinal Vein Occlusion Concept MapDocument2 pagesRetinal Vein Occlusion Concept MapJoe RealNo ratings yet
- Orbital CellulitisDocument20 pagesOrbital CellulitissarahNo ratings yet
- RNDocument16 pagesRNrunnermn100% (1)
- Mindoro's Largest Hospital OpensDocument17 pagesMindoro's Largest Hospital OpensParisGeronimo80% (5)
- Physical Therapy Practice QuestionsDocument53 pagesPhysical Therapy Practice QuestionsJohn Ryan ParisNo ratings yet
- The Use of Artificial Dermis in The Reconstruction.9Document9 pagesThe Use of Artificial Dermis in The Reconstruction.9Resurg ClinicNo ratings yet