Professional Documents
Culture Documents
Managing Difficult Airway in Obstetric Anesthesia
Uploaded by
Roman AureliaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Managing Difficult Airway in Obstetric Anesthesia
Uploaded by
Roman AureliaCopyright:
Available Formats
DIFFICULT AIRWAY IN OBSTETRIC ANESTHESIA
Sonia Vaida
Anesthetic management of parturient patients is a challenge, as it involves simultaneous care of two lives. Studies from the USA and United Kingdom have consistently shown that maternal mortality is greater with general anesthesia than regional anesthesia. Most of the deaths were due to hypoxia, secondary to difficult or failed intubation or to pulmonary aspiration of gastric contents.1,2 Failed endotracheal intubation and ventilation are still a major concern of anesthesia-related maternal mortality occurring during cesarean deliveries.3 The incidence of difficult airway in the pregnant population is eight times higher than in the non-pregnant population or about 1 in 250-300 patients.3-5 The morbidity associated with difficult intubation is about thirteen times higher than the general population.4 The trend is to perform lower and lower rates of general anesthesia for cesarean delivery, which accounts for the relative inexperience with the obstetric airway. A major challenge facing obstetric anesthesiologists is teaching general anesthesia to new trainees. With the steady decrease in the use of general anesthesia, residents may go through their training without administering general anesthesia for a Cesarean section. Difficult airway in obstetric anesthesia is mostly attributable to: airway edema, weight gain during pregnancy and preexisting anatomical deformities.6 Airway edema Airway edema results from hormonally (progesterone) induced fluid retention during pregnancy, and it can be amplified by pregnancy-induced hypertension, fluid overload, head-down position, oxytocin infusion (fluid retention due to the antidiuretic effect), prolonged Valsalva efforts during delivery, and b- adrenergic tocolytic therapy. Using photographs taken in
Department of Anesthesiology Penn State College of Medicine
a standardized fashion, Pilkington et al. showed that the Mallampati classification of the airway changed between the first and third trimesters. 7 Vascular engorgement of the respiratory tract and oro-pharyngeal mucosa during pregnancy accounts for reduced internal diameter of the trachea and increased risk of bleeding during airway manipulation. Weight Gain Obesity is frequently encountered during pregnancy; the parturient can gain 20 kg or more during pregnancy. In the morbidly obese parturient the cesarean delivery rate exceeds 50%. Difficult intubation in the obese patient may be due to a short neck or large tongue and breasts, which make laryngoscopy and intubation laborious. Chest compliance is often poor, and mask ventilation may prove to be difficult. Preexisting anatomical deformities Examples of conditions involving the airway: facial and upper airway abnormalities, airway tumors, immobile cervical spine, surgical induced deformities, and selected systemic diseases. Risk of hypoxia Pregnant women become hypoxemic more rapidly than non-pregnant women during episodes of apnea because of: reduced functional capacity, (resulting in airway closure and an increased alveolararterial oxygen gradient during normal tidal respiration) higher oxygen consumption, decreased cardiac output in supine position. (aorto-caval compression). Therefore, the pregnant woman requires more efficient denitrogenation and preoxygenation prior to induction of general anesthesia. Risk of Aspiration Gastrointestinal system also undergoes significant change and every parturient should be considered at risk of aspiration during induction of general anesthesia. The pressure from the enlarging uterus increases intragastric pressure. The lower esophageal sphincter tone decreases secondary to the hormones of pregnancy. As a result, barrier pressure (lower esophageal
32
Timi[oara, 2005
pressure minus intragastric pressure) decreases and reflux occurs.8 Among the hormonal factors, increased gastrin, secretin and progesterone and decreased secretion of motilin are responsible for the delay in gastric emptying.6 Pharmacologic prophylaxis usually consists of intravenous administration of an H2 receptor antagonist and metoclopramide combined with oral administration of an clear, non-particulate antacid before induction. Cricoid Pressure These changes emphasize the need for the application of cricoid pressure before the patient loses consciousness in order to prevent aspiration or regurgitation during induction of general anesthesia. Cricoid pressure is applied directly over the cricoid cartilage, the only solid structure in the larynx, with the intent of applying pressure on the esophagus and preventing regurgitation into the oropharynx. However, the effectiveness of cricoid pressure has been questioned. Additionally, the technique of cricoid pressure is often inappropriately applied. Appropriate application of cricoid pressure in an upward and backward direction may improve the view at laryngoscopy.7,8
PREPARATION FOR GENERAL ANESTHESIA
Vigilance is the key along with back-up plan and the availability of necessary equipment. Positioning of operating room the table: should be adjusted to the level of the laryngoscopist intercostals margin, and tilted 15 degree to the left, to avoid aortocaval compression. Patient position: appropriate neck flexion is facilitated by placing several pads or blankets under the shoulder an upper back, thereby flattening the kyphotic curvature of the thoracic spine. The head also must be extended on the neck (extension of the atlanto occipital joint) to bring the oral axis in line with the pharyngeal and laryngeal axis (Magill or Sniffing position).
Have a strategic plan in place for every patient. It is necessary to apply a variety of criteria to identify potential difficult airway. The positive predictive value of the difficult airway is improved if combinations tests are used. (Mallampati classification, mouth opening, sternomental/ thyromental distance, atlanto-occipital extension, evaluation of teeth, etc). Identify cricothyroid membrane If there is any doubt regarding the ability to maintain airway patency during general anesthesia, consider: 1. Regional anesthesia 2. Awake fiberoptic intubation Regional anesthesia is the best choice for cesarean section in most cases of anticipated difficulty with endotracheal intubation.1-9 However, the anesthesiologist should understand that regional anesthesia itself does not solve the problem of a difficult airway, anticipate potential complications (e.g., failed anesthesia, total spinal anesthesia), and be fully prepared to administer general anesthesia. Spinal anesthesia is preferred over epidural anesthesia because of: higher success rate, faster onset, lower risk of total spinal anesthesia and local anesthetic toxic reaction. A combination spinal-epidural anesthesia (CSE), a relatively new technique, has gained popularity. Awake fiberoptic intubation . Although awake intubation can be time-consuming, there are several convincing reasons to perform the procedure in a patient with a recognized difficult airway: 1) the natural airway is better maintained in an awake patient; 2) adequate muscle tone helps maintain the natural separation of the upper airway structures, which facilitates the identification of anatomical landmarks and 3) induction of general anesthesia and muscle paralysis results in anterior movement of the larynx, which impedes visualization of the larynx during direct laryngoscopy.1,6,10 The Unrecognized Difficult Airway The Patient Who Cannot Be Intubated but Can Be Ventilated by Mask with no Fetal Distress - Awake the patient! Cricoid pressure should be maintained until the patient is fully awake. Further management: regional anesthesia vs awake intubation. The Patient Who Cannot Be Intubated but Who Can Be Ventilated by Mask with Fetal Distress Present Management options: Awaken the patient Continue anesthesia via mask ventilation while an assistant maintains cricoid pressure
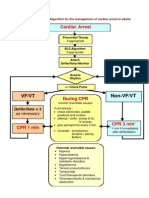
MANAGEMENT OF THE DIFFICULT AIRWAY DECISION MAKING
Management depends on whether surgery is elective or urgent, the condition of the fetus, and whether a difficult airway is predicted. Recognized difficult airway Airway assessment Preparatory efforts enhance success and minimize risk to the patient.
Actualit\]i <n anestezie, terapie intensiv\ [i medicin\ de urgen]\
33
Laryngeal Mask (does not provide effective protection from aspiration, problematic with cricoid pressure) An endotracheal tube can also be inserted through an LMA, either blindly or with the aid of a fiberscope. Proseal (a new laryngeal mask device with a modified cuff and a drainage tube designed to isolate the airway from the digestive tract) Intubating Laryngeal Maks (Fastrach) LMA Ctrach Combitube
not fully allowed by maintenance of an inspiration to expiration ratio of at least 1:3.1-6 Compared with emergency surgical cricothyrotomy or tracheostomy, establishment of percutaneous TTJV is quicker and simpler. Cricothyroidomy. Seldinger type needle and wire technique, over which a guide and then a single one-step dilator is passed.
SUMMARY
1. Assume that every parturient has a potentially difficult airway. 2. Evaluate the airway of every parturient; have a back-up plan for every patient. 3. Have difficult airway equipment available. 4. When faced with a difficult intubation, practitioners should choose the device they are most experienced using. Do what you do best. 5. Optimize patients position for intubation. 6. Provide adequate muscular relaxation. 7. Dont start surgery if oxygenation and ventilation are unsatisfactory. 8. Choose regional anesthesia whenever possible.
REFERENCES
The Patient Who Cannot Be Intubated or Ventilated by Mask (Cannot Ventilate, Cannot Intubate) Life threatening situation!!! Consider: LMA, Proseal, Intubating Laryngeal Mask, Combitube Transtracheal jet ventilation (TTJV). TTJV is used when other modalities of ventilation, including LMA and Combitube, fail or are not available. It consists of a simple I.V. plastic cannula (14 or 16 gauge) inserted through the cricothyroid membrane. A jet injector provides ventilation with oxygen pressurized to 50 pounds per square inch (psi). The major risk of TTJV is barotrauma, which may occur if the inflation pressure was not controlled by a pressureregulator, and emptying of the lungs is
1. Department of Health and others. Why mothers die 1997 1999. The Confidential Enquiries into Maternal Deaths in the United Kingdom. London: RCOG Press; 2001. 2. Hawkins JL, Koonin LM, Palmer SK, Gibbs CP. Anesthesiarelated deaths during obstetric delivery in the United States, 19791990. Anesthesiology1997;86:27784. 3. Kuczkowski KM, Reisner LS, Benumof JL. The difficult airway: Risk, Prohpilaxis, and Management in Chestnut DH. Obstetric Anesthesia: Principles and Practice. 3 rd Edition. Mosby Inc 2004. p. 535-62. 4. Hagberg CA: Handbook of Difficult Airway Management. Philadelphia, Churchill Livingstone, 2000, p 301-18 5. Barnardo PD, Jenkins JG. Failed tracheal intubation in obstetrics: a 6-year review in a UK region. Anaesthesia. 2000;55:690-4. 6. Ezri T, Szmuk P, Evron S, Geva D, Hagay Z, Katz J. Difficult airway in obstetric anesthesia: a review. Obstet Gynecol Surv. 2001;56:631-41. 7. Pilkington S, Carli F, Dakin MJ, et al. Increase in Mallampati score during pregnancy. Br J Anaesth 1995;74:63842 8. Douglas J. General anesthesia and obstetrics: a deadly combination? Can J Anaesth 2004;51:R1R4 9. Davies JM, Weeks S, Crone LA, Pavlin E: Difficult intubation in the parturient. Can J Anaesth 1989;36:66874. 10. Munnur U, Suresh MS. Airway problems in pregnancy. Crit Care Clin. 2004;20:617-42.
34
Timi[oara, 2005
You might also like
- Anesthesiology Resident Manual of Procedures: A Step-by-Step GuideFrom EverandAnesthesiology Resident Manual of Procedures: A Step-by-Step GuideNo ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Epidural Anatomy & PhysiologyDocument14 pagesEpidural Anatomy & PhysiologyAbel AxelNo ratings yet
- Failed Spinal Anaesthesia Mechanisms, Management and PreventionDocument6 pagesFailed Spinal Anaesthesia Mechanisms, Management and Preventiondrhemantt1279No ratings yet
- Joint Replacement Anesthesia ManagementDocument55 pagesJoint Replacement Anesthesia ManagementRaguNo ratings yet
- Failed Spinal AnaesthesiaDocument10 pagesFailed Spinal Anaesthesian12345678n100% (1)
- Fred Rotenberg, MD Dept. of Anesthesiology Rhode Island Hospital Grand Rounds February 27, 2008Document53 pagesFred Rotenberg, MD Dept. of Anesthesiology Rhode Island Hospital Grand Rounds February 27, 2008lmjeksoreNo ratings yet
- Anaesthesia in Obese PatientsDocument72 pagesAnaesthesia in Obese PatientsPraveen RamasamyNo ratings yet
- Thoraxic Region Nerve Block - ESADocument35 pagesThoraxic Region Nerve Block - ESAMaraNo ratings yet
- Awareness in Anesthesia FinalisedDocument42 pagesAwareness in Anesthesia FinalisedLean CyNo ratings yet
- Complication of Spina AnesthesiaDocument8 pagesComplication of Spina AnesthesiaSandroLaoNo ratings yet
- Anaesthesia VaporisersDocument4 pagesAnaesthesia VaporisersTAMAR HEALTHCARENo ratings yet
- Extubation After AnaesthesiaDocument7 pagesExtubation After AnaesthesiaaksinuNo ratings yet
- 21 Obstetric Anaesthesia PDFDocument0 pages21 Obstetric Anaesthesia PDFjuniorebindaNo ratings yet
- 7..intravenous Anaesthesia 2Document23 pages7..intravenous Anaesthesia 2Mwiliza BrendaNo ratings yet
- Anesthesia For GeriatricDocument21 pagesAnesthesia For GeriatricintanNo ratings yet
- Paediatric Anaesthesia PDFDocument33 pagesPaediatric Anaesthesia PDFMarcelitaTaliaDuwiriNo ratings yet
- Ultrasound-Guided Regional Anesthesia TechniquesDocument59 pagesUltrasound-Guided Regional Anesthesia TechniquesAdi Nugroho Melyana100% (1)
- Comparison of Two Approaches ofDocument96 pagesComparison of Two Approaches ofJacob OrtizNo ratings yet
- Bronchial AsthmaDocument25 pagesBronchial AsthmaKamil HannaNo ratings yet
- Anesthesia Challenges in Trauma & Shocked PatientsDocument126 pagesAnesthesia Challenges in Trauma & Shocked PatientsabdishakurNo ratings yet
- Asa 2013Document1,076 pagesAsa 2013Marwa Mahrous100% (4)
- Obstetrics AnesthesiaDocument31 pagesObstetrics AnesthesiaNorfarhanah ZakariaNo ratings yet
- Airway Management Saq 47Document47 pagesAirway Management Saq 47RaMy “MhMd” ElaRabyNo ratings yet
- Elsevier - Anaesthesiology Clinics - Vol.26, Issues 1 - Obstetric Anesthesia (2008) PDFDocument230 pagesElsevier - Anaesthesiology Clinics - Vol.26, Issues 1 - Obstetric Anesthesia (2008) PDFMila KarmilaNo ratings yet
- Technique For Awake Fibre Optic IntubationDocument3 pagesTechnique For Awake Fibre Optic Intubationmonir61No ratings yet
- Management of Intraoperative Bronchospasm: Dr. ImranDocument49 pagesManagement of Intraoperative Bronchospasm: Dr. ImranhellodrvigneshwarNo ratings yet
- Anaesthesia and Sedation Outside TheatresDocument15 pagesAnaesthesia and Sedation Outside Theatresمحمد زينNo ratings yet
- Anesthesia PresentationDocument19 pagesAnesthesia PresentationJohnyNo ratings yet
- Pregnancy & Its Anaesthetic ImplicationsDocument29 pagesPregnancy & Its Anaesthetic ImplicationsDadik WijayaNo ratings yet
- Anesthesia Machine: Ventilator, Vaporizer & Scavenging SystemDocument76 pagesAnesthesia Machine: Ventilator, Vaporizer & Scavenging SystemMohmmed MousaNo ratings yet
- Complications of Spinal and Epidural AnesthesiaDocument45 pagesComplications of Spinal and Epidural AnesthesiashikhaNo ratings yet
- Liver Disease in AnesthesiaDocument31 pagesLiver Disease in AnesthesiaAnnan Agyekum JoshuaNo ratings yet
- Anesthesia For Bariatric SurgeryDocument47 pagesAnesthesia For Bariatric Surgerydkhiloi100% (1)
- Epidural AnesthesiaDocument5 pagesEpidural AnesthesiaImran MukhlessNo ratings yet
- Spinal Anesthesia - Technique - UpToDateDocument37 pagesSpinal Anesthesia - Technique - UpToDateSamir Perez CasadiegoNo ratings yet
- Anesthesia For ElderlyDocument27 pagesAnesthesia For ElderlyApril Joy CalayagNo ratings yet
- Intrathecal MorphineDocument6 pagesIntrathecal MorphineJoana MoreiraNo ratings yet
- Prehospital Anesthesia HandbookDocument46 pagesPrehospital Anesthesia HandbookoscarNo ratings yet
- Factors Affectin Block HeightDocument37 pagesFactors Affectin Block HeightshikhaNo ratings yet
- Principles of AnesthesiaDocument60 pagesPrinciples of AnesthesiaTakale BuloNo ratings yet
- Immediate Post Anesthetic RecoveryDocument12 pagesImmediate Post Anesthetic Recoverysubvig100% (2)
- 3.preoperative Patient Assessment and ManagementDocument76 pages3.preoperative Patient Assessment and Managementoliyad alemayehuNo ratings yet
- Obesity & Anaesthesia: Co-Ordinator - Dr. Chavi Sethi (MD) Speaker - Dr. Uday Pratap SinghDocument56 pagesObesity & Anaesthesia: Co-Ordinator - Dr. Chavi Sethi (MD) Speaker - Dr. Uday Pratap SinghRafi ramdhanNo ratings yet
- Update EmergenciesDocument84 pagesUpdate EmergenciesElaineNo ratings yet
- Management of Acute PainDocument76 pagesManagement of Acute PainAnonymous nruHyuwtJ100% (1)
- AnaesthesiaDocument8 pagesAnaesthesiarakeeb qadriNo ratings yet
- GeneralAnesthetics and Stages of AnesthesiaDocument27 pagesGeneralAnesthetics and Stages of AnesthesiaNaghman Zuberi100% (1)
- Modern Anaesthesia Machines: Upgrading and SafetyDocument24 pagesModern Anaesthesia Machines: Upgrading and SafetyShiva Kumar P SNo ratings yet
- Controlled Hypotension: Moderator: DR V. Y. Srinivas Presenter: Dr. Ann Susan MathewDocument49 pagesControlled Hypotension: Moderator: DR V. Y. Srinivas Presenter: Dr. Ann Susan MathewAnn Susan MathewNo ratings yet
- Preoperative Patient Assessment and Management: Roxanne Jeen L. FornollesDocument61 pagesPreoperative Patient Assessment and Management: Roxanne Jeen L. FornollesRyan FornollesNo ratings yet
- Neuroanesthesia Crisis ManualDocument56 pagesNeuroanesthesia Crisis ManualChrismas BangunNo ratings yet
- Anesthesia Considerations For Neuromuscular DiseaseDocument42 pagesAnesthesia Considerations For Neuromuscular Diseasesamrox54No ratings yet
- Pediatric Anesthesiology Review: Clinical Cases for Self-AssessmentFrom EverandPediatric Anesthesiology Review: Clinical Cases for Self-AssessmentNo ratings yet
- Anesthesia - State of Narcosis, Analgesia, Relaxation, and Loss of Reflex. Effects of AnesthesiaDocument3 pagesAnesthesia - State of Narcosis, Analgesia, Relaxation, and Loss of Reflex. Effects of AnesthesiaJhevilin RMNo ratings yet
- Management of Failed Block - Harsh.Document48 pagesManagement of Failed Block - Harsh.Faeiz KhanNo ratings yet
- Anaesthesia For Thyroid Surgery....Document46 pagesAnaesthesia For Thyroid Surgery....Parvathy R NairNo ratings yet
- Safe Pediatric AnesthesiaDocument24 pagesSafe Pediatric AnesthesiamdNo ratings yet
- Do We Need Other GuidelinesDocument7 pagesDo We Need Other GuidelinesRoman AureliaNo ratings yet
- Clinical Practice Guidelines For The Management of The Diffcult AirwayDocument12 pagesClinical Practice Guidelines For The Management of The Diffcult AirwayRoman AureliaNo ratings yet
- ASL AlgorithmDocument1 pageASL AlgorithmRoman AureliaNo ratings yet
- Anaesthesia For Caesarean Section in Patients With Preterm HELLP SyndromeDocument6 pagesAnaesthesia For Caesarean Section in Patients With Preterm HELLP SyndromeRoman AureliaNo ratings yet
- Allergic Reactions To Anaesthetic DrugsDocument25 pagesAllergic Reactions To Anaesthetic DrugsRoman AureliaNo ratings yet
- Anesthetic Management of Delivery in Women With PregnancyDocument33 pagesAnesthetic Management of Delivery in Women With PregnancyRoman AureliaNo ratings yet
- Anaesthetic Considerations For Patients With Pre-Existing NeDocument16 pagesAnaesthetic Considerations For Patients With Pre-Existing NeRoman AureliaNo ratings yet
- Airway Management - Supraglottic Airway PDFDocument4 pagesAirway Management - Supraglottic Airway PDFPiet Pogen PoelNo ratings yet
- Allergic Reactions During AnesthesiaDocument14 pagesAllergic Reactions During AnesthesiaRoman AureliaNo ratings yet
- AmilazemieDocument1 pageAmilazemieRoman AureliaNo ratings yet
- Rectal and Genital Examination 2Document56 pagesRectal and Genital Examination 22013SecBNo ratings yet
- Ecg in BciDocument7 pagesEcg in BciRoman AureliaNo ratings yet
- Valori NormaleDocument4 pagesValori NormaleDragomirescu Ana-cristinaNo ratings yet
- Tissue Procurement, Processing, and Staining TechniquesDocument10 pagesTissue Procurement, Processing, and Staining TechniquesMuhammad JameelNo ratings yet
- Lefort 1 OsteotomyDocument16 pagesLefort 1 Osteotomyabhiram.ramesh1290No ratings yet
- 12 White Blood Cell Counting Techniques in BirdsDocument5 pages12 White Blood Cell Counting Techniques in BirdsPablo LópezNo ratings yet
- X - Problem Prioritization and NCPDocument5 pagesX - Problem Prioritization and NCPMartin Lєtmaku Espina100% (2)
- Snakes in India - Tradition and The Truth PDFDocument5 pagesSnakes in India - Tradition and The Truth PDFhoticeforuNo ratings yet
- Chronic UrticariaDocument40 pagesChronic UrticariaeeeeewwwwwNo ratings yet
- Limbic System (Behaviour and Emotion)Document19 pagesLimbic System (Behaviour and Emotion)Patterson MachariaNo ratings yet
- Arab Board Orthopedic Exam June 2013Document35 pagesArab Board Orthopedic Exam June 2013Nasser AlbaddaiNo ratings yet
- Acute and Chronic PyelonephritisDocument7 pagesAcute and Chronic PyelonephritisMatthew Ryan100% (1)
- Holter SolutionsDocument4 pagesHolter SolutionsgimenNo ratings yet
- Fluid Volume DeficitDocument2 pagesFluid Volume DeficitpeternohibiNo ratings yet
- GIT - Dr. Allam 2021 PDFDocument47 pagesGIT - Dr. Allam 2021 PDFMohammedNo ratings yet
- Language and BrainDocument23 pagesLanguage and Brainalbino100% (1)
- The Integumentary System: Layers and Functions of SkinDocument8 pagesThe Integumentary System: Layers and Functions of SkinAmanuel MaruNo ratings yet
- Basic PhysiologyDocument58 pagesBasic PhysiologyVidit JoshiNo ratings yet
- PsychSim 5 Quizzing - Chapter 6-Sensation and PerceptionDocument5 pagesPsychSim 5 Quizzing - Chapter 6-Sensation and Perceptionneecee126100% (1)
- From: Rapid Interpretation of EKG'sDocument14 pagesFrom: Rapid Interpretation of EKG'sLucija Kljaić100% (1)
- แนวข้อสอบ National license - Hematology PDFDocument7 pagesแนวข้อสอบ National license - Hematology PDFTanawat SingboonNo ratings yet
- Evaluation of Preoperative Pulmonary RiskDocument19 pagesEvaluation of Preoperative Pulmonary RiskCharlieBrown_QBNo ratings yet
- NPTEL Stress Management MCQ AssignmentDocument5 pagesNPTEL Stress Management MCQ AssignmentSnehaNo ratings yet
- Effects of Social Media On The Psychology of PeopleDocument6 pagesEffects of Social Media On The Psychology of PeopleIJAFRCNo ratings yet
- 0610 - 2016 - 41 Paper 4Document20 pages0610 - 2016 - 41 Paper 4Muhammad HassaanNo ratings yet
- Surface Anatomy (Part 2) : Oral Exam VideoDocument63 pagesSurface Anatomy (Part 2) : Oral Exam VideoAna UsharidzeNo ratings yet
- Vocal AnatomyDocument8 pagesVocal AnatomyfunktotumNo ratings yet
- Hyperlipedemia PPDocument51 pagesHyperlipedemia PPrabarNo ratings yet
- Buteyko Breathing ExercisesDocument5 pagesButeyko Breathing ExercisesjoseNo ratings yet
- Standard and Cardiopulmonary Exercise Testing HandoutDocument17 pagesStandard and Cardiopulmonary Exercise Testing HandoutDarcyNo ratings yet
- Enteral NutritionDocument11 pagesEnteral NutritionEso Soso0% (1)
- Role Play KomkepDocument7 pagesRole Play KomkepSyubban AfifNo ratings yet
- Liver Cirrhosis NCP 1Document6 pagesLiver Cirrhosis NCP 1Paolo Rafael D EsguerraNo ratings yet