Professional Documents
Culture Documents
Hiponatremia Hipernatremia
Uploaded by
Mabel Straccia0 ratings0% found this document useful (0 votes)
27 views4 pagesHyponatremia is not rare (1% to 2% of hospitalised patients), and hypernatremia is about 10 times less frequent. The main goal of the treatment is not to normalize numbers, but to treat symptoms. A hypotonic state will be considered in association with hypovolemia, euvolemia or hypervolemia.
Original Description:
Original Title
Hiponatremia hipernatremia
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentHyponatremia is not rare (1% to 2% of hospitalised patients), and hypernatremia is about 10 times less frequent. The main goal of the treatment is not to normalize numbers, but to treat symptoms. A hypotonic state will be considered in association with hypovolemia, euvolemia or hypervolemia.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
27 views4 pagesHiponatremia Hipernatremia
Uploaded by
Mabel StracciaHyponatremia is not rare (1% to 2% of hospitalised patients), and hypernatremia is about 10 times less frequent. The main goal of the treatment is not to normalize numbers, but to treat symptoms. A hypotonic state will be considered in association with hypovolemia, euvolemia or hypervolemia.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
M
I
N
E
R
V
A
M
E
D
I
C
A
C
O
P
Y
R
I
G
H
T
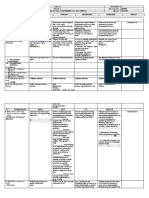
MINERVA ANESTESIOL 2006;72:353-6
Hyponatremia, hypernatremia:
a physiological approach
G. OFFENSTADT
1
, V. DAS
2
1
Medical Intensive Care Unit
Hpital Saint-Antoine, Paris, France
2
Epidemiology Research Unit
Systmes d'Information et Modlisation
INSERM (U707), Paris, France
Natremia belongs to the toolbox of the practicing
intensivist. It is an indicator of the hydration sta-
tus, which is an item that must be continuously
monitored in critically ill patients. Hyponatremia
is not rare (1% to 2% of hospitalised patients),
and hypernatremia is about 10 times less fre-
quent while hypernatremia always indicates
hypertonicity, hyponatremia is not equivalent
to hypotonicity. Diagnosis depends on the his-
tory, clinical examination and basic biochemi-
cal data. It should be kept in mind that obtain-
ing urine samples is as important as plasma sam-
ples in this respect. The first step consists in con-
firming that hyponatremia is hypotonic. The sec-
ond step is to assess the renal response to hypo-
tonicity. Hypotonic hyponatremia will be con-
sidered in association with hypovolemia, euv-
olemia or hypervolemia. The constitution of a
hyperosmolar state requires an inadequate water
intake The main goal of the treatment is not to
normalize numbers (they must always be checked
first), but to treat symptoms. Tolerance must
always be appreciated. The mathematical for-
mulas proposed are of interest for a better under-
standing, but should not be followed strictly.
Key words: Sodium - Hyponatremia - Hyper-
natremia.
N
atremia belongs to the toolbox of the prac-
ticing intensivist. It is an indicator of the
hydration status, which is an item that must be
continuously monitored in critically ill patients.
Normal natremia ranges from 135 to 145
mmoL/L. Changes in plasmatic osmolality cause
fluid shifts between extra and intracellular
spaces. Osmolality is precisely regulated to pre-
vent changes in cellular volume which is the pri-
mary consequence of osmolality variation.
Neurologic cell damage may arise not only dur-
ing hypo- or hyperosmolality, but also when
correcting the disorders. Hyponatremia is not
rare (1% to 2% of hospitalised patients), and
hypernatremia is about 10 times less frequent.
1
In Intensive Care Units (ICU), the occurrence is
higher. In patients admitted to the medical ICU
of Saint-Antoine Hospital in Paris in 2004,
among 713 ionograms, 14.6% indicated hypona-
tremia (130 mmoL/L), 2.3% were 120
mmoL/L and 0.7% were 150 mmoL/L.
Among 12 853 ionograms in the emergency
room at the same hospital in 2004 , there
were 7.9% with natremia (130, 0.66% (120
and 0.16% (150 mmoL/L.
Physiopathology
Water diffuses freely across cell membrane
barrier, driven by plasmatic tonicity which is
Vol. 72, N. 6 MINERVA ANESTESIOLOGICA 353
Address reprint requests to: G. Offenstadt, Service de ra-
nimation mdicale, hpital Saint Antoine, 184 rue du Faubourg
Saint Antoine, 75012 Paris, France.
E-mail : georges.offenstadt@sat.aphp.fr
M
I
N
E
R
V
A
M
E
D
I
C
A
C
O
P
Y
R
I
G
H
T
OFFENSTADT HYPONATREMIA, HYPERNATREMIA: A PHYSIOLOGICAL APPROACH
the osmotic pressure generated by all non
diffusive molecules dissolved in one litre of
plasma. Tonicity can only be calculated by
summing the osmotic pressures of all non
diffusible molecules. If there is no tonicity
change, there is no net water movement
across the cell membrane.
2, 3
While hypernatremia always indicates
hypertonicity, hyponatremia is not equiva-
lent to hypotonicity.
Cells shrink in case of extracellular hyper-
tonicity, and will expand with hypotonicity.
These changes in volume are tempered in
brain cells, since they have a particular sys-
tem for changing their osmotic content.
Natremia and plasmatic tonicity depend
on exchangeable potassium and sodium and
mainly on total body water. However they
do not inform on sodium balance which is a
major determinant of volemia.
Regulation of plasmatic tonicity results from
thirst, renal excretion of water and release
of anti diuretic hormone (ADH).
In subjects with normal renal function,
urine tonicity ranges from 50 to 1200
mOsm/kg.
In addition to changes in plasma osmolal-
ity, pain, hypotension, hypovolemia, nau-
sea,hypoxia, hypoglycemia, some drugs, may
trigger vasopressin release.
4
Thirst stimuli are
identical to those of ADH release.
Clinical aspects and etiology of hypo-osmo-
lar states
In most patients, hyponatremia is asymp-
tomatic, because the decrease in natremia is
a slow process allowing brain volume cells to
adapt. Most authors consider hyponatremia as
acute when it appears in less than 48 hours.
Acute hyponatremia are less frequent than
chronic hyponatremia and less well tolerated
depending on the level of encephalopaty.
Diagnosis depends on the history, clinical
examination and basic biochemical data. It
should be kept in mind that obtaining urine
samples is as important as plasma samples in
this respect.
Eliminating iso or hyperosmolar hypona-
tremia
The first step consists in confirming that
hyponatremia is hypotonic.
Pseudohyponatremia is a laboratory artifact
which is now obsolete thanks to modern
direct potentiometry instruments using sodi-
um ion specific electrodes.
Hyponatremia may be associated with
hyperosmolar state because of the increased
concentration of an effective solute in the
extra cellular fluid compartment.
Osmotic gap is increased above 10
mosm/kg. The most frequent cause is hyper-
glycemia with a correcting factor reported to
range between 1.4 and 2.4 mmoL/L for an
increase in glycemia of 5.5 mmoL/L.
5
Less
common causes include sick cell syndrome.
Assessing the renal response
The second step is to assess the renal
response to hypotonicity. Is renal dilution
capacity normal but exceeded by a too large
input of water? In this case, the ratio of urine
osmolality to plasmatic osmolality is below 1,
suggesting potomania.
If the ratio is above 1, diagnosis will
depend on the state of extra-cellular hydra-
tion. Appreciation of this state is not always
straightforward, and based on the associa-
tion of clinical and biological signs.
6
Natriuria
is very important in this respect.
Hypotonic hyponatremia will be consid-
ered in association with hypovolemia, euv-
olemia or hypervolemia.
Hyponatremia with increased extracellu-
lar volume occurs in oedematous state, where
there is a low effective arterial volume (con-
gestive heart failure, hepatic cirrhosis,
nephrotic syndrome..).
In hyponatremia with clinical normal extra-
cellular volume, there is free water gain with
negligible sodium loss. The most common
cause is syndrome of inappropriate antidi-
uretic hormone secretion (SIADH).
4
The diag-
nostic criteria for SIADH include: hypo-osmo-
lar hyponatremia, inappropriately concen-
trated urine, clinical euvolemia and normal
adrenal, thyroid, cardiac, hepatic and renal
function. Hypouricemia is frequent and char-
acteristic. Causes of SIADH are getting more
and more numerous, in particular among
pharmacologic drugs.
Among euvolemic hyponatremia, two oth-
354 MINERVA ANESTESIOLOGICA Giugno 2006
M
I
N
E
R
V
A
M
E
D
I
C
A
C
O
P
Y
R
I
G
H
T
HYPONATREMIA, HYPERNATREMIA: A PHYSIOLOGICAL APPROACH OFFENSTADT
er situations have to be reported: the debat-
able post surgical acute hyponatremia,
7
and,
importantly, hyponatremia associated with
thiazidic diuretics which although classically
thought as hypovolemic is often euvolemic.
8
Hyponatremia with extra cellular dehydration
Thirst vasopressin release are triggered by
decrease in effective arterial volume, con-
tributing to the hypo-osmolar state. Two
groups may be constituted depending on uri-
nary sodium concentration: a low urinary
sodium (below 20 mmoL/L) suggests extra-
renal sodium and water losses (gastro intesti-
nal disorders, severe burns, ...). In contrast
urinary sodium above 20 mmoL/L reflects
renal and water losses (nephropathy, diuret-
ic use ...). We stress two more causes: acute
hyponatremia among marathon runners,
9
and
cerebral salt wasting syndrome.
10
Clinical aspects and etiology of
hyperosmolar states
The constitution of an hyperosmolar state
requires an inadequate water intake. Neu-
rologic signs directly associated to dehydra-
tion are difficult to appreciate. Are they cause
or consequence of intracellular dehydration?
Here also, the appreciation of extra cellu-
lar volume leads the diagnosis.
Hyperosmolar states without hypertonicity
First, hyperosmolar states without hyper-
tonicity must be eliminated. It is the case
when there is an increase of extracellular
solutes, like urea or ethanol, diffusing to the
intracellular space.
Hyperosmolar states with hypertonicity
1. Loss of water almost free of electrolytes.
Polyuria of diabetes insipidus if not com-
pensated may generate this disorder.
2. Loss of water and electrolytes.
In this case, hypovolemia may be associ-
ated. Hypotonic losses can be classified as
renal or extra-renal. A frequent renal loss is
osmotic polyuria complicating hyperglycemia.
3. Gains of non diffusible electrolytes.
The most frequent cause is hyperglycemia.
Iatrogenic sodium gain is rare.
Treatment
The main goal of the treatment is not to
normalize numbers (they must always be
checked first), but to treat symptoms.
Tolerance must always be appreciated.
Of course, the cause(s) and the risk(s) fac-
tors must be treated, but we shall focus on
symptomatic treatment.
Mathematical formulas proposed
11
are of
interest for a better understanding, but should
not be followed strictly. They do not take
into account that the system is open, and
require an unknown theoretical body
weight.
12
Hyperosmolar state
Rehydration is always necessary. The oral
route should be favoured because it easily
allows pure water replacement. If the patient
is hypovolemic, volume resuscitation must
be a priority. Because of the risk of cerebral
oedema, current practice guidelines recom-
mend lowering the serum sodium concen-
tration to 0.5 to 1 mmoL/h, with a maximum
decrease of 12 mmoL/day.
Hypo-osmolar state
Treatment of acute hyponatremia
Rapid correction (1 to 5 mmoL/L/h) is only
indicated in patients with severe symptoms
(seizure, coma),
13
and possibly with identified
risk factors (pre-menopausal woman, chil-
dren, hypoxemia). Treatment is based on
injection of an average 2 g NaCl/h, possibly
associated with loop diuretic, cautiously mon-
itored and stopped as soon as the symptoms
disappear.
Treatment of chronic hyponatremia
Most of the times, chronic hyponatremia is
well tolerated. Correction has to take into
Vol. 72, N. 6 MINERVA ANESTESIOLOGICA 355
M
I
N
E
R
V
A
M
E
D
I
C
A
C
O
P
Y
R
I
G
H
T
OFFENSTADT HYPONATREMIA, HYPERNATREMIA: A PHYSIOLOGICAL APPROACH
account the risk of appearance of the osmot-
ic demyelination syndrome (ODS). The
appearance of the ODS has been reported
after too rapid correction of chronic hypona-
tremia. This situation is not the main cause of
ODS which has been essentially described
in alcoholic patients with malnutrition.The
patient has usually gone through a biphasic
clinical course, initially encephalopathic, then
recovering rapidly as natremia is normalised,
only to deteriorate several days later
(dysarthria, flaccid quadriparesis,variable
changes in conscious,locked-in syndrome...).
The appearance of lesions on MRI may be
significantly delayed by several days or
weeks.Prevention relies on a slow correction
with a target below 12 mmoL/L in the first 24
hours and below 18 mmoL/L in the first 48
hours. The prognosis is classically dismal.
Recently, the reinduction of hyponatremia
has been reported efficient in two patients
14,
15
but this treatment has to be more precise-
ly evaluated.
Riassunto
Iposodiemia e ipersodiemia: un approccio fisiologico
La sodiemia rappresenta un punto di riferimento
per lintensivista pratico. Essa un indicatore dello sta-
tus didratazione, un aspetto che deve essere contin-
uamente monitorato nei pazienti criticamente
ammalati. Liposodiemia non rara (1-2% dei pazienti
ricoverati), mentre lipersodiemia 10 volte meno
frequente delliposodiemia. Mentre lipersodiemia
indica sempre lipertonicit, liposodiemia non
equivalente allipotonicit. La diagnosi dipende dal-
lanamnesi, dallesame clincio e dai dati biochimici di
base. A questo proposito si dovrebbe ricordare che la
raccolta di un campione di urine importante quan-
to la raccolta di un campione di plasma. Il primo pas-
so consiste nel confermare che liposodiemia indichi
ipotonia. Il secondo passo quello di valutare la
risposta renale allipotonicit. Liposodiemia ipoton-
ica si assocer ad ipovolemia, euvolemia o iperv-
olemia. Linstaurarsi di uno stato iperosmolare richiede
un apporto inadeguato di acqua. Lobiettivo principale
del trattamento non quello di normalizzare i
numeri (che devono comunque essere valutati pri-
ma) ma di trattare i sintomi. Si deve sempre tener
conto della tolleranza. Le formule matematiche pro-
poste sono interessanti per comprendere meglio il
problema, ma non devono essere seguite stretta-
mente.
Parole chiave: Sodiemia - Iponatremia - Ipernatremia.
References
1. Fraser CL, Arieff AI. Epidemiology, pathophysiology,
and management of hyponatremic encephalopathy.
Am J Med 1997;102:67-77.
2. Moritz ML, Ayus JC. The pathophysiology and treatment
of hyponatraemic encephalopathy: an update. Nephrol
Dial Transplant 2003;18:2486-91.
3. Oster JR, Singer I. Hyponatremia, hyposmolality, and
hypotonicity: tables and fables. Arch Intern Med
1999;159:333-6.
4. Verbalis JG. Disorders of body water homeostasis. Best
Pract Res Clin Endocrinol Metab 2003;17:471-503.
5. Hillier TA, Abbott RD, Barrett EJ. Hyponatremia: eval-
uating the correction factor for hyperglycemia. Am J
Med 1999;106:399-403.
6. McGee S, Abernethy WB, 3rd, Simel DL. The rational
clinical examination. Is this patient hypovolemic? JAMA
1999;281:1022-9.
7. Wijdicks EF, Larson TS. Absence of postoperative
hyponatremia syndrome in young, healthy females.
Ann Neurol 1994;35:626-8.
8. Spital A. Diuretic-induced hyponatremia. Am J Nephrol
1999;19:447-52.
9. Noakes TD. Overconsumption of fluids by athletes.
BMJ 2003;327:113-4.
10. Singh S, Bohn D, Carlotti AP, Cusimano M, Rutka JT,
Halperin ML. Cerebral salt wasting: truths, fallacies,
theories, and challenges. Crit Care Med 2002;30:2575-
9.
11. Adrogue HJ, Madias NE. Hyponatremia. N Engl J Med
2000;342:1581-9.
12. Liamis G, Kalogirou M, Saugos V, Elisaf M. Therapeutic
approach in patients with dysnatraemias. Nephrol Dial
Transplant 2006; Epub ahead of print(doi:10.
1093/ndt/gfk090).
13. Soupart A, Decaux G. Therapeutic recommendations
for management of severe hyponatremia: current con-
cepts on pathogenesis and prevention of neurologic
complications. Clin Nephrol 1996;46:149-69.
14. Oya S, Tsutsumi K, Ueki K, Kirino T. Reinduction of
hyponatremia to treat central pontine myelinolysis.
Neurology 2001;57:1931-2.
15. Soupart A, Ngassa M, Decaux G. Therapeutic relowering
of the serum sodium in a patient after excessive correc-
tion of hyponatremia. Clin Nephrol 1999;51:383-6.
356 MINERVA ANESTESIOLOGICA Giugno 2006
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Link To Publication in University of Groningen/UMCG Research DatabaseDocument19 pagesLink To Publication in University of Groningen/UMCG Research Databaseovr79100% (1)
- Canadian Medical Residency GuideDocument239 pagesCanadian Medical Residency GuideSym Y100% (1)
- Peripheral Neuropathies FOR CLASSIFICATIONDocument9 pagesPeripheral Neuropathies FOR CLASSIFICATIONAnnie JoNo ratings yet
- Laminates AND Veneers: Dr. Sakshi Rawal Department of Prosthodontics MDS II YearDocument76 pagesLaminates AND Veneers: Dr. Sakshi Rawal Department of Prosthodontics MDS II Yearsapna100% (2)
- 1 - Hifumax 1Document25 pages1 - Hifumax 1Get It SuplementosNo ratings yet
- Monitoring Levels of Iron, TIBC, HB, Transferrin and Ferritin During Pregnancy Trimesters and Lactation in Sulaimania City /iraqDocument3 pagesMonitoring Levels of Iron, TIBC, HB, Transferrin and Ferritin During Pregnancy Trimesters and Lactation in Sulaimania City /iraqMabel StracciaNo ratings yet
- Mycobacterium Tuberculosis,: Molecular Epidemiology of Buenos Aires, ArgentinaDocument4 pagesMycobacterium Tuberculosis,: Molecular Epidemiology of Buenos Aires, ArgentinaMabel StracciaNo ratings yet
- NIH Public Access: Vitamin D and Gestational Diabetes MellitusDocument10 pagesNIH Public Access: Vitamin D and Gestational Diabetes MellitusMabel StracciaNo ratings yet
- Hashimoto 2015Document4 pagesHashimoto 2015Mabel StracciaNo ratings yet
- Lucica GA-L Glycated Albumin Assay Kit: A New Diagnostic Test For Diabetes MellitusDocument3 pagesLucica GA-L Glycated Albumin Assay Kit: A New Diagnostic Test For Diabetes MellitusMabel StracciaNo ratings yet
- Transferable Vancomycin Resistance in A Community-Associated MRSA LineageDocument8 pagesTransferable Vancomycin Resistance in A Community-Associated MRSA LineageMabel StracciaNo ratings yet
- Palliative Care: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document101 pagesPalliative Care: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)jackeline RodriguezNo ratings yet
- Pterygium CaseDocument8 pagesPterygium CaseNandita JaliNo ratings yet
- Induction and Augmentation of LaborDocument20 pagesInduction and Augmentation of Laborjssamc prasootitantraNo ratings yet
- Krisdayani Martha Sukma (P1337424117012) Vio Waliyatun Hasna (P1337424117036)Document5 pagesKrisdayani Martha Sukma (P1337424117012) Vio Waliyatun Hasna (P1337424117036)LabibaNo ratings yet
- B2 MicroglobulinDocument1 pageB2 MicroglobulinPhong Nguyễn WindyNo ratings yet
- Case Formulation in PsychiatryDocument8 pagesCase Formulation in PsychiatryMarius PaţaNo ratings yet
- Odontogenic CystsDocument5 pagesOdontogenic CystsBH ASMRNo ratings yet
- Definition of Terms: Herbaceous Plant Costaceae Brazil Bahia Espirito SantoDocument1 pageDefinition of Terms: Herbaceous Plant Costaceae Brazil Bahia Espirito SantoAshly Jamiah DelRosario ManatoNo ratings yet
- Position PaperDocument1 pagePosition PaperTristan Josh FortichNo ratings yet
- Traumatic Aortic RuptureDocument20 pagesTraumatic Aortic RuptureLisa MoyoNo ratings yet
- IHD - JalalDocument46 pagesIHD - JalalMituran IshwarNo ratings yet
- Viral Diseases in Honey BeesDocument7 pagesViral Diseases in Honey BeesMalsawmsanga ChhakchhuakNo ratings yet
- Management of Renal Stones: Theme From January 2013 ExamDocument123 pagesManagement of Renal Stones: Theme From January 2013 ExamBela VitoriaNo ratings yet
- Love To Fear You - Kati McRaeDocument310 pagesLove To Fear You - Kati McRaeKlee IdkNo ratings yet
- MHP 1Document3 pagesMHP 1Asna anwerNo ratings yet
- Efficacy of The anti-VZV (anti-HSV3) Vaccine in HSV1 and HSV2 Recurrent Herpes Simplex Disease: A Prospective StudyDocument8 pagesEfficacy of The anti-VZV (anti-HSV3) Vaccine in HSV1 and HSV2 Recurrent Herpes Simplex Disease: A Prospective StudymostafaNo ratings yet
- English 3 w5Document6 pagesEnglish 3 w5Almie Adarayan BrosotoNo ratings yet
- Fish and Shell Fish Immunology: Full Length ArticleDocument9 pagesFish and Shell Fish Immunology: Full Length ArticleKirana Rahmada SafitriNo ratings yet
- CS Drug Study NotesDocument11 pagesCS Drug Study NotestwnynyiskaNo ratings yet
- Kathryn Clavier ResumeDocument2 pagesKathryn Clavier Resumeapi-654404237No ratings yet
- DLL Mapeh g4 q2 w3Document6 pagesDLL Mapeh g4 q2 w3Daniel MingoyNo ratings yet
- April 3, 2020 Strathmore TimesDocument12 pagesApril 3, 2020 Strathmore TimesStrathmore TimesNo ratings yet
- TPS 2020 Bahasa InggrisDocument9 pagesTPS 2020 Bahasa InggrisYopi Panca YudhaNo ratings yet
- Urinary Tract InfectionDocument50 pagesUrinary Tract InfectionJanuaryNo ratings yet
- Chole CystitisDocument1 pageChole CystitisEirah Nicole JumawanNo ratings yet