Professional Documents
Culture Documents
The Role of The Lumbar Multifidus in Chronic Low Back Pain
Uploaded by
Hugo FalquetoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Role of The Lumbar Multifidus in Chronic Low Back Pain
Uploaded by
Hugo FalquetoCopyright:
Available Formats
Clinical Review: Focused
The Role of the Lumbar Multidus in Chronic Low Back Pain: A Review
Michael D. Freeman, PhD, MPH, DC, Mark A. Woodham, DC, Andrew W. Woodham, BA
Low back pain (LBP), a highly prevalent problem in society, is often a recurrent condition. Recent advances in the understanding of the biomechanics of LBP have highlighted the importance of muscular stabilization of the neutral zone range of motion in the low back. The lumbar multidus muscles (LMM) are important stabilizers of this neutral zone, and dysfunction in these muscles is strongly associated with LBP. The dysfunction is a result of pain inhibition from the spine, and it tends to continue even after the pain has resolved, likely contributing to the high recurrence rate of LBP. Persisting LMM dysfunction is identied by atrophic replacement of multidus muscle with fat, a condition that is best seen on magnetic resonance imaging. Muscle training directed at teaching patients to activate their LMM is an important feature of any clinical approach to the LBP patient with demonstrated LMM dysfunction or atrophy. PM R 2010;2:142-146
INTRODUCTION
Low back pain (LBP) is a highly prevalent problem in society; approximately 60% to 80% of the population will experience an episode of LBP during their lifetime, and 60% to 86% of these people will have more than one episode of LBP [1,2]. A relatively recent shift in the view of LBP has gone from classifying it as a self-limited acute condition to a recurrent syndrome [3]. The purpose of this review is to discuss the role of the lumbar multidus muscles (LMM) in recurrent LBP, as well as to discuss literature-based clinical approaches to assessment and treatment of multidus dysfunction. Spinal stabilization therapy has been observed to be more effective over time in treating LBP than minimal intervention and exercise therapy alone, and has also been observed to reduce pain, disability, and medication intake, as well as recurrence rates [4,5]. As a consequence, treatment focus has shifted to reactivation and strengthening of the smaller muscles of the spine to improve long-term stabilization of the vertebral column. Biomechanical research has increased the understanding of mechanisms of low back injury and pain, specically regarding the ability to stabilize the neutral zone of the lumbar spine with tonic muscle control. Panjabi [6] has described the neutral zone as the part of the range of intervertebral motion, measured from the neutral position, in which spinal motion can occur with minimal nonmuscular passive resistance from the spine. Suni and colleagues [2] described a randomized controlled trial of a neuromuscular training program directed at neutral zone stabilization on a population of patients with recent back injury. These authors demonstrated a signicant decrease in the intensity of LBP in the treatment group that was not seen in the control group, and concluded that control of the lumbar neutral zone was an important component of LBP and disability prevention.
M.D.F. Department of Public Health and Preventive Medicine, Oregon Health and Science University School of Medicine 1234 SW 18th Ave, Portland, OR 97205. Address correspondence to: M.F.; e-mail: forensictrauma@ gmail.com Disclosure: nothing to disclose M.A.W. Private practice, Tacoma, WA Disclosure: nothing to disclose A.W.W. Department of Genetic, Molecular, and Cellular Biology, University of Southern California, Los Angeles, CA Disclosure: nothing to disclose Disclosure Key can be found on the Table of Contents and at www.pmrjournal.org Submitted for publication May 15, 2009; accepted November 19.
MULTIFIDUS FUNCTION
It is well established that the LMM are important stabilizers of the lumbar neutral zone; Wilke et al [7] found that the actions of the multidi account for more than two thirds of the stiffness of the spine when in the neutral zone. In comparison with all lumbar muscles, the LMM are short and stout, with a high cross-sectional area (CSA) and short muscle bers. Furthermore, these
PM&R
2010 by the American Academy of Physical Medicine and Rehabilitation
Vol. 2, 142-146, February 2010 DOI: 10.1016/j.pmrj.2009.11.006
142
1934-1482/10/$36.00 Printed in U.S.A.
PM&R
Vol. 2, Iss. 2, 2010
143
authors found that at the foundation of this high CSA was a high mass, which allows for packing of a large number of muscle bers into relatively small space. This morphology allows the LMM to produce very large forces over a small operating range, and makes the LMM ideally suited for stability as opposed to motion [8,9]. Functionally, the LMM are divided into deep and supercial bers, with deep bers spanning 2 vertebral segments and functioning tonically, and the supercial bers spanning 3 to 5 levels and functioning phasically [10,11]. This arrangement makes the deep bers of the LMM anatomically and biomechanically well suited for stabilization.
MULTIFIDUS ATROPHY AND LOW BACK PAIN
A number of prior investigations have described the LMM atrophy and replacement by fat after low back injury, a pathologic process that is closely correlated with LBP. Kjaer and colleagues [12] evaluated the lumbar magnetic resonance imaging (MRI) results for 412 adult and 442 adolescent subjects in a cross-sectional study of LMM atrophy. These authors categorized the degree of observed atrophy in the LMM as none, slight, and severe, and correlated the ndings with complaints of LBP. They found that fat inltrations of the LMM were strongly associated with LBP in adults, and that the association was independent of body mass index (BMI). Kader et al [13] performed a retrospective study of 78 patients with LBP and either with or without leg pain. The authors assessed the correlation between MRI changes in the LMM and leg pain. It was reported that LMM atrophy was present in 80% of the patients with LBP and that there was a signicant correlation between LMM atrophy and referred leg pain. The authors theorized that LMM atrophy may be caused by dorsal ramus syndrome, which has been described as LBP with referred leg pain, produced by irritation of anatomic structures supplied by the dorsal ramus nerve, ie, the facet joints and LMM. The authors further concluded that abnormalities of the LMM may explain referred leg pain in the absence of other MRI abnormalities. Hides et al [14] described a study of 26 subjects with unilateral LBP, some with referred lower extremity pain. The authors assessed LMM atrophy among the subjects using ultrasound imaging, noting marked asymmetry of the LMM that was localized to a single vertebral level in most cases. The authors noted that the level of LMM asymmetry correlated with the neurologic level of the symptoms in 24 of the 26 subjects in the study.
brous tissues. The authors established a ranked grading scale for LMM atrophy consisting of mild, moderate, and severe, corresponding to atrophy in less than 10% of CSA of the LMM, more than 10% and less than 50%, and more than 50%, respectively (Figures 1-3). Two readers assessed the degree of LMM atrophy among the subjects, with good interobserver agreement noted. Kjaer et al [12] described the blinded assessment of LMM atrophy in 854 MRI scans of adults and adolescents using a grading scale similar to that used by Kader et al [13]. The authors found good intraobserver and interobserver agreement among the readers for the adult group. The authors noted that fatty inltration after LMM atrophy could be measured in a noninvasive manner using MRI. Barker et al [15] performed MRI on 50 patients presenting to a back pain clinic with unilateral persisting LBP. The authors measured the CSAs of the left and right psoas and LMM and correlated their ndings with the distribution and duration of symptoms among the subjects. A signicant positive correlation between the side of LMM atrophy and the distribution of the LBP was found, as well as between the degree of atrophy and the duration of the symptoms. CT has been evaluated as a relatively lower-cost and more accessible alternative to MRI for assessment of LMM atrophy. Danneels et al [16] described a study of CT assessment of 32 LBP patients and 23 active volunteers. The study design included CT of the CSA of the LMM at 3 levels. The authors found macroscopic atrophic changes in the LMM in 80% of the patients with LBP, and that the atrophy in the LMM at the lowest levels of the lumbar spine correlated signicantly with LBP status. The authors concluded that the most important nding from their study was the nding of a signicant correlation between LMM atrophy and radicular and nonradicular leg pain. The utility and reliability of US relative to MRI scanning, have also been evaluated as a means of assessing LMM CSA. Hides et al [17] compared the CSA assessment of the LMM among healthy young adults using MRI and US, following a strict protocol The authors determined that LMM CSA could be measured as accurately with US as with MRI, although they did not assess the ability of US to discriminate the degree of atrophy in the LMM.
REFLEX INHIBITION MODEL OF LOCALIZED MULTIFIDUS ATROPHY
Macintosh et al [11] described the morphology of the LMM by means of the dissection of 12 adult cadaver spines. In contrast to previous determinations that each LMM is innervated by a number of spinal nerves, these authors found that the LMM is divided into 5 distinct myotomes that are each innervated by a single spinal segment. They found that all muscle bers attaching to the spinous process or lamina of a particular vertebra are segmentally innervated by the same nerve; the medial branch of the dorsal ramus that originates
IMAGING OF MULTIFIDUS ATROPHY
There are numerous publications describing the morphologic assessment of the LMM using MRI, computed tomography (CT), and ultrasound (US). Kader et al [13] used MRI in evaluating LMM atrophy, which they dened as muscular replacement with fat and
144
Freeman et al
ROLE OF THE LUMBAR MULTIFIDUS IN CHRONIC LOW BACK PAIN
inferior to the respective vertebra (Figure 4). Thus, the muscle that moves a given spinal segment is supplied by the nerve for that segment. The authors postulated that from an anatomic perspective, the shared innervation of the zygapophyseal joints means that pain emanating from these joints could result in a reex inhibition of the LMM at the same level. Indahl et al [18] noted that the injection of saline into the zygapophyseal joint in a porcine model resulted in decreased activity of the multidus muscle. They concluded that the effect of the injection was to activate a stretch reex in the joint capsule, which in turn excited inhibitory interneurons in the spinal cord, which in turn inhibited the motor neurons and decreased the muscle response. The authors inferred that LMM atrophy seen in the human spine is a result of reex inhibition caused by afferent feedback from the zygapophyseal joint, which in turn impedes the voluntary activation of the LMM. The authors pointed to their results as evidence that multidus atrophy seen in back pain patients is more likely a result of dysfunction rather than disuse. The authors postulated that inhibitory discharges from the zygapophyseal joints may explain the efcacy of manual medical approaches to back pain such as manipulation and mobilization directed at the zygapophyseal joints. Hodges et al [19] demonstrated, also in a porcine model, the rapid onset of LMM atrophy within 3 days after an experimentally induced nerve root injury. After transection of the medial branch of the L3 nerve root, the ipsilateral LMM CSA adjacent to the L4, L5, and L6 spinous processes was reduced by 13%, 20%, and 12%, respectively, by 72 hours after injury. The changes were isolated to the side of injury; there were no differences in the CSA or muscular activity levels of the contralateral LMM, as determined by US assessment. The authors also investigated the changes in the LMM
after experimentally induced disk injury in the porcine model. A stab wound was introduced to the left anterolateral aspect of the L3-4 intervertebral disk, and this was followed by focal atrophy and a reduction of the CSA of the left LMM by 17%. The authors opined that it was unlikely that the injury resulted from LMM denervation (owing to nerve root injury) as the atrophy was only at the level of the disk, whereas single nerve roots innervate three levels of LMM. The authors noted that the posttraumatic changes in the LMM noted in their study were undoubtedly attributable to a reduction in neural drive to the muscle, but that the mechanism that accounted for the reduction was unclear. Hides et al [20] provided further evidence that the pattern of LMM atrophy is local rather than general in a study that compared multidus size and bilateral symmetry between chronic LBP patients and healthy asymptomatic subjects. The authors reported that at the L4 and L5 levels, asymptomatic subjects were found to have signicantly larger multidus muscles in comparison with chronic LBP patients. They also found that the greatest asymmetry was seen at the L5 vertebral level in patients with unilateral pain presentations. The authors concluded that their ndings support a clinical approach to LBP that uses exercise therapy that focuses on localized muscle impairments. Wallwork et al [21] demonstrated that LMM atrophy was associated with a reduction in the ability to voluntarily contract the muscle. The authors used diagnostic US to measure contractions of the LMM by comparing the thickness of the muscle at rest to when it was contracted. Study subjects with chronic LBP and LMM atrophy demonstrated signicantly decreased ability to perform isometric contractions of their LMM. These study results reinforced the ndings of prior authors and emphasized the clinical perspective that rehabilitation in LBP patients may need to target localized impairments in motor control.
MULTIFIDUS ATROPHY TREATMENT
Danneels et al [4] assessed the efcacy of 3 different treatment modalities on multidus CSA in chronic LBP patients. A group of 59 patients were randomly allocated to one of 3 programs: stabilization training, stabilization training combined with dynamic resistance, and stabilization training combined with dynamic-static resistance. Using CT scanning, LMM CSAs were measured before and after 10 weeks of training. The CSA of the LMM muscle was signicantly increased at all vertebral levels only in the dynamic-static resistance training group. The authors concluded that the static holding component between concentric and eccentric contraction phases was critical to induction of muscle regrowth. A randomized controlled trial performed by Van et al [22] used real-time visual feedback by means of US to improve the isometric contraction capability of the LMM in healthy sub-
Figure 1. Mild multidus muscle atrophy, per Kader et al [13] grading criteria (less than 10% of CSA of muscle replaced with fat).
PM&R
Vol. 2, Iss. 2, 2010
145
Figure 2. Moderate multidus muscle atrophy, per Kader et al [13] grading criteria (more than 10% but less than 50% of CSA of muscle replaced with fat).
jects. The authors applied motor learning principles to train the subjects in voluntary contraction of the multidus and gave verbal feedback to one group, and verbal and visual feedback to the other. They found that providing the subjects with visual feedback of their performance resulted in better quality muscle contraction of the LMM as well as better memory of how to contract the multidi after reassessment a week later. Sung [23] evaluated the question of whether an exercise program designed to increase the ability to contract the LMM improves functional status or reduces LBP. This author described a short-term cohort study that assessed the effect of a 4-week spinal stabilization exercise program in a group of LBP patients, reporting a signicant improvement in LMM function, as well as a reduction in LBP disability. Hides et al [5] described the effects of stabilization training on LMM CSA among elite athletes (cricketers) with LBP, concluding that LMM atrophy can exist in highly active, elite athletes. The authors demonstrated that the stabilization training increased the CSA of the LMM, and that the training was associated with a decrease in symptoms of LBP. Their results showed that specic training that aims at activation of the LMM is associated with both an increase in functional status and a reduction in LBP. In an earlier study by Hides et al [24], the authors demonstrated that LMM function recovery is not necessarily associated with the resolution of painful symptoms in LBP patients. The authors studied a group of 39 patients with a rst episode of acute unilateral LBP and corresponding unilateral segmental inhibition of the LMM. The patients were randomly allocated to 2 groups, only one of which performed specic exercises designed to reactivate the LMM through facilitating an isometric contraction of these muscles. The
group that did not perform the exercises had decreased LMM size at a 10-week follow-up examination even though they had resumed normal levels of activity and had a remission of painful symptoms, whereas the group that performed the isometric contractions showed more rapid and complete LMM recovery. The authors suggested that the continued dysfunction of the LMM in such patients may be one reason for the high recurrence rates of LBP after an initial episode. MacDonald et al [25] assessed muscular control of long and short LMM bers in 15 recurrent LBP patients and 19 control subjects. The authors used EMG to determine whether LMM control at the L5 level differed between the groups. They found that there were changes in motor control of the LMM among the patients that primarily affected the shorter bers, and that these changes were greater on the previously painful side of the low back. These ndings support the use of a specically designed stabilization exercise program directed toward the LMM and specically the deeper shorter bers that serve to stabilize the spine. The authors concluded that the abnormal pattern of muscle control they observed may leave the spine vulnerable to reinjury, thus predisposing the spine to recurrent episodes of LBP. The authors postulated that the observed motor control problem among the recurrent LBP patients implied that pain and functional performance should not be the only outcome measures after an acute episode of LBP.
CONCLUSIONS
The LMM are important stabilizers of the lumbar spine neutral zone, and atrophy of the muscle decreases the ability to
Figure 3. Severe multidus atrophy, per Kader et al [13] grading criteria (more than 50% of CSA of muscle replaced with fat).
146
Freeman et al
ROLE OF THE LUMBAR MULTIFIDUS IN CHRONIC LOW BACK PAIN
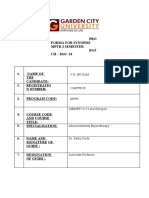
Transverse Process Spinous Process Intervertebral Disc Facet Joint Medial Branch of The Dorsal Ramus Multifidus Muscle
Figure 4. Schematic representation of orientation and innervation of a lumbar multidus muscle.
control the neutral zone and is strongly associated with LBP. This atrophy appears to help perpetuate an inhibitory feedback loop that begins with pain in the spine, possibly stemming from the intervertebral disks or zygapophyseal joints, followed by reex inhibition of the multidus, and then atrophy and fatty replacement of the muscle. Amelioration of the LBP does not necessarily result in resumption of normal LMM function, and decreased LMM function is likely implicated in recurrent LBP. Muscle training directed at teaching patients to activate their LMM is an important feature of any clinical approach to the patient with LBP who demonstrates LMM dysfunction or atrophy.
REFERENCES
1. Aure O, Nilsen J, Vasseljen O. Manual therapy and exercise therapy in patients with chronic low back pain: A randomized, controlled trial with 1-year follow-up. Spine 2003;28:525-532. 2. Suni J, Rinne M, Natri A, Pasanen M, Parkkari J, Alaranta H. Control of the lumbar neutral zone decreases low back pain and improves selfevaluated work ability. Spine 2006;31:E611-E620. 3. Von Korff M, Saunders K. The course of back pain in primary care. Spine 1996;21:2833-2837. 4. Danneels L, Vanderstraeten G, Cambier D, et al. Effects of three different training modalities on the cross sectional area of the lumbar multidus muscle in patients with chronic low back pain. Br J Sports Med 2001;35:186-191. 5. Hides J, Stanton W, McMahon S, Sims K, Richardson C. Effect of stabilization training on multidus muscle cross-sectional area among young elite-cricketers with low back pain. J Orthop Sports Phys Ther 2008;38:101-108. 6. Panjabi M. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord 1992;5:390-397. 7. Wilke H, Wolf S, Claes L, Arand M, Wiesend A. Stability of the lumbar spine with different muscle groups. Spine 1995;20:192-198.
8. Ward S, Kim C, Eng C, et al. Architectural analysis and intraoperative measurements demonstrate the unique design of the multidus muscle for the lumbar spine stability. J Bone Joint Surg 2009;91:176-185. 9. Rosatelli AL, Ravichandiran K, Agur AM. Three-dimensional study of the musculotendinous architecture of lumbar multidus and its functional implications. Clin Anat 2008;21:539-546. 10. MacDonald D, Moseley G, Hodges P. The lumbar multidus muscle: does the evidence support the clinical beliefs. Man Ther 2006;11:254263. 11. Macintosh J, Valencia F, Bogduk M, Munro R. The morphology of the lumbar multidus. Clin Biomech 1986;1:196-204. 12. Kjaer P, Bendix T, Sorensen J, Korsholm L, Leboeuf-Yde C. Are MRIdened fat inltrations in the multidus muscles associated with low back pain? BMC Medicine 2007;5:2. 13. Kader D, Wardlaw D, Smith F. Correlation between the MRI changes in the lumbar multidus muscles and leg pain. Clin Radiol 2000;55:145149. 14. Hides J, Stokes M, Saide M, Jull G, Cooper D. Evidence of lumbar multidus muscle wasting ipsilateral to symptoms in patients with acute/ subacute low back pain. Spine 1994;19:165-172. 15. Barker K, Shamley D, Jackson D. Changes in the cross-sectional area of multidus and psoas in patients with unilateral back pain. Spine 2004;29:E515-E519. 16. Danneels L, Vanderstraeten G, Cambier D, Witvrouw E, De Cuyper H. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J 2000;9:266-272. 17. Hides J, Richardson C, Jull G. Magnetic resonance imaging and ultrasonography of the lumbar multidus muscle comparison of two different modalities. Spine 1995;20:54-58. 18. Indahl A, Kaigle A, Reikers O, Holm S. Interaction between the porcine lumbar intervertebral disc, zygapophyseal joints, and paraspinal muscles. Spine 1997;22:2834-2840. 19. Hodges P, Holm A, Hansson T, Holm S. Rapid atrophy of the lumbar multidus follows experimental disc or nerve root injury. Spine 2006; 31:2926-2933. 20. Hides J, Gilmore C, Stanton W, Bohlscheid E. Multidus size and symmetry among chronic LBP and healthy asymptomatic subjects. Man Ther 2008;13:43-9. Epub 2006 Oct 27. 21. Wallwork TL, Stanton WR, Freke M, Hides JA. The effect of chronic low back pain on size and contraction of the lumbar multidus muscle. Man Ther 2009;14:496-500. Epub 2008 Nov 21. 22. Van K, Hides J, Richardson C. The use of real-time ultrasound imaging of lumbar multidus muscle contraction in healthy subjects. J Orthop Sports Ther 2006;36:920-925. 23. Sung P. Multidus muscle median frequency before and after spinal stabilization exercises. Arch Phys Med Rehabil 2003;84:1313-1318. 24. Hides J, Richardson C, Jull G. Multidus muscle recovery is not automatic after resolution of acute, rst-episode low back pain. Spine 1996;21:2763-2769. 25. MacDonald D, Moseley G, Hodges P. Why do some patients keep hurting their back? Evidence of ongoing back muscle dysfunction during remission from recurrent back pain. Pain 2009;142:183-188. This CME activity is designated for 1.0 AMA PRA Category 1 Credit and can be completed online at me.aapmr.org. Log on to www.me.aapmr.org, go to Lifelong Learning (CME) and select Journal-based CME from the drop down menu. This activity is FREE to AAPM&R members and $25 for non-members.
You might also like
- Sports Hernia and Athletic Pubalgia: Diagnosis and TreatmentFrom EverandSports Hernia and Athletic Pubalgia: Diagnosis and TreatmentDavid R. DiduchNo ratings yet
- Subgroups of Lumbo-Pelvic Flexion Kinematics Are Present in People With and Without Persistent Low Back PainDocument13 pagesSubgroups of Lumbo-Pelvic Flexion Kinematics Are Present in People With and Without Persistent Low Back Painjul yanNo ratings yet
- Group Pattern Muscle Activity Lower Back PainDocument8 pagesGroup Pattern Muscle Activity Lower Back PainHossam BarghashNo ratings yet
- Effect of NMES Vs Isometric Exercise in OA of Knee-With-Cover-Page-V2 Removed RemovedDocument5 pagesEffect of NMES Vs Isometric Exercise in OA of Knee-With-Cover-Page-V2 Removed RemovedZahra SativaniNo ratings yet
- s12891 018 2387 XDocument15 pagess12891 018 2387 XVizaNo ratings yet
- Effects of Low-Load Motor Control Exercises and A High-Load Lifting Exercise On LumbarDocument7 pagesEffects of Low-Load Motor Control Exercises and A High-Load Lifting Exercise On LumbarYoh ChenNo ratings yet
- Lumb Strenghth and MckenzieDocument5 pagesLumb Strenghth and MckenzieSahithya MNo ratings yet
- Dolor Espalda 6Document7 pagesDolor Espalda 6Pablo Ignacio Nova BaezaNo ratings yet
- Lumbar InstabilityDocument6 pagesLumbar InstabilityCotta MüllerNo ratings yet
- Effect of Chronic Low Back Pain On Lumbar Spine Lordosis During Sit-to-Stand and Stand-to-SitDocument14 pagesEffect of Chronic Low Back Pain On Lumbar Spine Lordosis During Sit-to-Stand and Stand-to-SitVictor CristianNo ratings yet
- Muscle Functions and Functional Performance Among PDFDocument11 pagesMuscle Functions and Functional Performance Among PDFmehdi.chlif4374No ratings yet
- Thoracic MET 2003Document16 pagesThoracic MET 2003sulis tiyowatiNo ratings yet
- BMC Musculoskeletal DisordersDocument8 pagesBMC Musculoskeletal DisordersGabriela Corrales CerdeiraNo ratings yet
- 2019 Article 2625Document9 pages2019 Article 2625consuelo amadoNo ratings yet
- Synopsis Template - MPTR 2022 - For Merge-1Document13 pagesSynopsis Template - MPTR 2022 - For Merge-1sriram gopalNo ratings yet
- Segmental Instability of The Lumbar SpineDocument13 pagesSegmental Instability of The Lumbar Spineiss kim100% (1)
- Ribeiro2018 Article ThePrevalenceOfMyofascialTriggDocument13 pagesRibeiro2018 Article ThePrevalenceOfMyofascialTriggThomas PurbaNo ratings yet
- Rehabilitation of LumbarDocument1 pageRehabilitation of LumbarYoh ChenNo ratings yet
- Tennis Elbow JOSPT ArticleDocument11 pagesTennis Elbow JOSPT ArticleHasan RahmanNo ratings yet
- The Provocative Lumbar Facet JointDocument10 pagesThe Provocative Lumbar Facet JointfilipecorsairNo ratings yet
- Ultrasound Assessment of Trunk Muscles and Back Flexibility, Strength and Endurance in Off-Road Cyclists With and Without Low Back PainDocument10 pagesUltrasound Assessment of Trunk Muscles and Back Flexibility, Strength and Endurance in Off-Road Cyclists With and Without Low Back PainSebastian EderNo ratings yet
- CMRT Position StatementDocument3 pagesCMRT Position StatementTito AlhoNo ratings yet
- An Adherent Nerve Root - Classification and Exercise Therapy in A PatientDocument4 pagesAn Adherent Nerve Root - Classification and Exercise Therapy in A PatientPablo Zamora MillanNo ratings yet
- MulliganDocument13 pagesMulliganAgustina AverameNo ratings yet
- Efficacy of Lumbar Mobilization On Postpartum Low Back Pain in Egyptian Females: A Randomized Control TrialDocument12 pagesEfficacy of Lumbar Mobilization On Postpartum Low Back Pain in Egyptian Females: A Randomized Control TrialAlekaNo ratings yet
- JANSSENS L IMTaffectsPropriocepticeUseAndLowBackPainDocument8 pagesJANSSENS L IMTaffectsPropriocepticeUseAndLowBackPainDaniel A Llanes MolinaNo ratings yet
- Accepted Manuscript: 10.1016/j.clinbiomech.2017.03.004Document30 pagesAccepted Manuscript: 10.1016/j.clinbiomech.2017.03.004Ambar Dani SyuhadaNo ratings yet
- BMC Musculoskeletal DisordersDocument10 pagesBMC Musculoskeletal DisordersVizaNo ratings yet
- NIH Public AccessDocument13 pagesNIH Public AccessMahida El shafiNo ratings yet
- Mechanical or Inflammatory Low Back Pain PDFDocument7 pagesMechanical or Inflammatory Low Back Pain PDFHugo FalquetoNo ratings yet
- HVT With Lumbar Disc HerniationDocument12 pagesHVT With Lumbar Disc HerniationSheena McLennanNo ratings yet
- Lumbar StabilizationDocument16 pagesLumbar StabilizationSahithya MNo ratings yet
- Aama Myofascial Meridians ArticleDocument8 pagesAama Myofascial Meridians Articledoktormin106No ratings yet
- Allet 2012Document8 pagesAllet 2012suhaidi.ikhlasNo ratings yet
- Treating Lumbar SpondylosisDocument10 pagesTreating Lumbar SpondylosisDiyya Awaliah Nurhakiimah IbrahimNo ratings yet
- Applied Kinesiology and The Cervical SpineDocument5 pagesApplied Kinesiology and The Cervical SpineScott CuthbertNo ratings yet
- The Effect of Manual Therapy and Neuroplasticity Education On Chronic Low Back Pain: A Randomized Clinical TrialDocument9 pagesThe Effect of Manual Therapy and Neuroplasticity Education On Chronic Low Back Pain: A Randomized Clinical TrialAlvaro Alarcon ValenzuelaNo ratings yet
- Orthopaedic JournalDocument6 pagesOrthopaedic JournalZiad AlazthaNo ratings yet
- Manual Therapy: Julie Hides, Warren Stanton, M. Dilani Mendis, Margot SextonDocument5 pagesManual Therapy: Julie Hides, Warren Stanton, M. Dilani Mendis, Margot SextonYoh ChenNo ratings yet
- Research Proposal FinalDocument9 pagesResearch Proposal Finalapi-621048040No ratings yet
- Artigo Grupo 1Document6 pagesArtigo Grupo 1reila taina oliveira silvaNo ratings yet
- The Fall of The Postural-Structural-Biomechanical Model in Manual and Physical TherapyDocument8 pagesThe Fall of The Postural-Structural-Biomechanical Model in Manual and Physical Therapycecilia martinezNo ratings yet
- Construct Validity of Lumbar Extension Measures in Mckenzie'S Derangement SyndromeDocument7 pagesConstruct Validity of Lumbar Extension Measures in Mckenzie'S Derangement SyndromeTomáš KrajíčekNo ratings yet
- Meralgia Paresthetica: A Review of The LiteratureDocument11 pagesMeralgia Paresthetica: A Review of The LiteratureEileen Torres CerdaNo ratings yet
- Lower Limb Involvement in Spinal Function PDFDocument1 pageLower Limb Involvement in Spinal Function PDFToni DNo ratings yet
- JCM 10 04983Document14 pagesJCM 10 04983Einar Cumplido MartínezNo ratings yet
- Effects of Thoracic Mobilization and Manipulation On Function and Mental State in Chronic Lower Back PainDocument4 pagesEffects of Thoracic Mobilization and Manipulation On Function and Mental State in Chronic Lower Back PainRatna Sulistya DewiNo ratings yet
- FINAL Version 1.0. Effectiveness of LASER Therapy in Managing Upper Trapezius-MPSDocument65 pagesFINAL Version 1.0. Effectiveness of LASER Therapy in Managing Upper Trapezius-MPSJan Wesley FelipeNo ratings yet
- 16IJPHY343 C.doneDocument6 pages16IJPHY343 C.doneMiaNo ratings yet
- 2007 Lumbar Stabilization Part 2 PDFDocument9 pages2007 Lumbar Stabilization Part 2 PDFPatricia Andrea Acevedo ArancibiaNo ratings yet
- Prevalence of Myofascial Trigger Points in Spinal Disorders: A Systematic Review and Meta-AnalysisDocument22 pagesPrevalence of Myofascial Trigger Points in Spinal Disorders: A Systematic Review and Meta-AnalysisGabriel Gaspar Bike FitNo ratings yet
- Comparison of Conservative Exercise Therapy With and Without Maitland Thoracic Manipulative Therapy in Patients With Subacromial Pain: Clinical TrialDocument8 pagesComparison of Conservative Exercise Therapy With and Without Maitland Thoracic Manipulative Therapy in Patients With Subacromial Pain: Clinical Trialelchinovichileno420No ratings yet
- Altered Cocontraction Patterns of Humeral Head Depressors in Patients With Subacromial Pain Syndrome: A Cross-Sectional Electromyography AnalysisDocument7 pagesAltered Cocontraction Patterns of Humeral Head Depressors in Patients With Subacromial Pain Syndrome: A Cross-Sectional Electromyography Analysis오현수No ratings yet
- M W M K C W S e P P S: R C TDocument10 pagesM W M K C W S e P P S: R C TDaniel GuevaraNo ratings yet
- Moore 2013Document9 pagesMoore 2013Andrés MardonesNo ratings yet
- Zane Clayton ThesisDocument133 pagesZane Clayton Thesisyoav6829No ratings yet
- Kilby 2012Document4 pagesKilby 2012DOUTOR HérniaNo ratings yet
- 45 Llps Vs HlbsDocument4 pages45 Llps Vs HlbsSudhir MishraNo ratings yet
- Bauer 2019Document10 pagesBauer 2019Rafa ZalfaNo ratings yet
- Electromyographic Analysis of The Hip Extension Pattern in Visually Impaired AthletesDocument9 pagesElectromyographic Analysis of The Hip Extension Pattern in Visually Impaired AthletesVizaNo ratings yet
- Repeated and Interrupted Resistance Exercise Induces The Desensitization and Re-Sensitization of mTOR-Related Signaling in Human Skeletal Muscle FibersDocument18 pagesRepeated and Interrupted Resistance Exercise Induces The Desensitization and Re-Sensitization of mTOR-Related Signaling in Human Skeletal Muscle FibersHugo FalquetoNo ratings yet
- Opioid and Chemokine Receptor - Nature (2015)Document10 pagesOpioid and Chemokine Receptor - Nature (2015)Hugo FalquetoNo ratings yet
- Chronic Pain The Role of Learning and Brain Mansour-Farmer-Baliki-Apkarian - IB-04.01.2013Document31 pagesChronic Pain The Role of Learning and Brain Mansour-Farmer-Baliki-Apkarian - IB-04.01.2013Hugo FalquetoNo ratings yet
- Beta Amiloid SleepDocument6 pagesBeta Amiloid SleepHugo FalquetoNo ratings yet
- What Is This Thing Called Pain (2010)Document3 pagesWhat Is This Thing Called Pain (2010)Hugo FalquetoNo ratings yet
- From Acute To Chronic Back PainDocument607 pagesFrom Acute To Chronic Back PainHugo Falqueto100% (2)
- BAAR K. Signals Mediating Skeletal Muscle Remodeling by Resistance Exercise JapplphysiolDocument8 pagesBAAR K. Signals Mediating Skeletal Muscle Remodeling by Resistance Exercise JapplphysiolHugo FalquetoNo ratings yet
- Horizontal and Vertical Jump PDFDocument9 pagesHorizontal and Vertical Jump PDFHugo FalquetoNo ratings yet
- Mechanical or Inflammatory Low Back Pain PDFDocument7 pagesMechanical or Inflammatory Low Back Pain PDFHugo FalquetoNo ratings yet
- A Modern Approach To Abdominal TrainingDocument5 pagesA Modern Approach To Abdominal TrainingHugo FalquetoNo ratings yet
- What Is Clinical PharmacyDocument4 pagesWhat Is Clinical PharmacySethiSheikhNo ratings yet
- ExrxDocument3 pagesExrxapi-463720918No ratings yet
- Assessment of Knowledge of Public On Coronary Artery Disease, Hypertension and Diabetes MellitusDocument5 pagesAssessment of Knowledge of Public On Coronary Artery Disease, Hypertension and Diabetes MellitusMythili MuthappaNo ratings yet
- Nursing Care of Stroke - NewDocument4 pagesNursing Care of Stroke - Newninda saputriNo ratings yet
- Acutes by LucDocument7 pagesAcutes by LucaldodiasNo ratings yet
- Placenta PreviaDocument9 pagesPlacenta PreviaVishal GuptaNo ratings yet
- Anti Anxiety MedicationsDocument2 pagesAnti Anxiety MedicationsjhgkhgkhgNo ratings yet
- Episiotomy TeachingDocument16 pagesEpisiotomy TeachingkamalbakshirNo ratings yet
- SCOLIOSISDocument4 pagesSCOLIOSISapi-3822433No ratings yet
- 1 Octeto de DefronzoDocument23 pages1 Octeto de DefronzoLesli Rodriguez50% (2)
- AaaDocument313 pagesAaaDanesh RafaNo ratings yet
- Hypnotist Harley Sears Joins "The Wellness Collaborative" in Kansas CityDocument2 pagesHypnotist Harley Sears Joins "The Wellness Collaborative" in Kansas CityPR.comNo ratings yet
- NAPLEX Drugs TableDocument71 pagesNAPLEX Drugs Tablestarobin100% (3)
- A. List Names of Antipsychotic Medications and Their Usual Range of Daily Dose For AdultsDocument7 pagesA. List Names of Antipsychotic Medications and Their Usual Range of Daily Dose For AdultsAbbie_Borromeo_1036No ratings yet
- Effect of Footwear On Dynamic Stability During Single-Leg Jump LandingsDocument6 pagesEffect of Footwear On Dynamic Stability During Single-Leg Jump Landingserwan.gir26No ratings yet
- Work Setting of CounselorDocument3 pagesWork Setting of CounselorAngel Rose Sierda MedinaNo ratings yet
- Genetic DisordersDocument19 pagesGenetic DisordersRohit patilNo ratings yet
- Blood Transfusion and NebulizationDocument12 pagesBlood Transfusion and NebulizationRachel Ann BatayolaNo ratings yet
- Thymatron 4Document8 pagesThymatron 4srinivasanaNo ratings yet
- Second Announcement Sunshine 2019Document20 pagesSecond Announcement Sunshine 2019alvinNo ratings yet
- Managment of Sepsis and Septic ShockDocument2 pagesManagment of Sepsis and Septic ShockDavid Simon CruzNo ratings yet
- Local Weekend Events in Mercury Bay, Whitianga, Tairua, PauanuiDocument28 pagesLocal Weekend Events in Mercury Bay, Whitianga, Tairua, PauanuiThe InformerNo ratings yet
- Breast Cancer ProtocolDocument24 pagesBreast Cancer Protocolsilveo100% (1)
- Remy Soap Note UpdatedDocument8 pagesRemy Soap Note Updatedapi-704750924No ratings yet
- FENO As Monitoring Tool in Bronchial Asthma A Randomised Control TrialDocument23 pagesFENO As Monitoring Tool in Bronchial Asthma A Randomised Control TrialYadvir GargNo ratings yet
- Ayurvedic Itihas Module - Final - 10-05-17Document7 pagesAyurvedic Itihas Module - Final - 10-05-17Vd Nisha ParmarNo ratings yet
- Oiucm InfoDocument1 pageOiucm InfoPrakash VerekarNo ratings yet
- Neurospa - Manual 2016 - 220829 - 202650Document8 pagesNeurospa - Manual 2016 - 220829 - 202650Liza HaeberleNo ratings yet
- Tuberculosis For Dec 1Document23 pagesTuberculosis For Dec 1Tony Rose Reataza-BaylonNo ratings yet
- Hypertension Management-1Document15 pagesHypertension Management-1Ali Sibra MulluziNo ratings yet