Professional Documents
Culture Documents
Ophthalmic Artery Chemosurgery For Less Advanced Intraocular Retinoblastoma: Five Year Review
Uploaded by
Fahlevie EpinOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ophthalmic Artery Chemosurgery For Less Advanced Intraocular Retinoblastoma: Five Year Review
Uploaded by
Fahlevie EpinCopyright:
Available Formats
Ophthalmic Artery Chemosurgery for Less Advanced Intraocular Retinoblastoma: Five Year Review
David H. Abramson1*, Brian P. Marr1, Scott E. Brodie1,2, Ira Dunkel3, Sotiria Palioura1,4, Y. Pierre Gobin5
1 Ophthalmic Oncology Service, Memorial Sloan-Kettering Cancer Center, New York, New York, United States of America, 2 Department of Ophthalmology, Mount Sinai School of Medicine, New York, New York, United States of America, 3 Department of Pediatrics, Memorial Sloan-Kettering Cancer Center, New York, New York, United States of America, 4 Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Boston, Massachusetts, United States of America, 5 Departments of Radiology and Neurosurgery, Weill Cornell Medical College, New York, New York, United States of America
Abstract
Background: Ophthalmic artery chemosurgery (OAC) for retinoblastoma was introduced by us 5 years ago for advanced intraocular retinoblastoma. Because the success was higher than with existing alternatives and systemic side effects limited we have now treated less advanced intraocular retinoblastoma (Reese-Ellsworth (RE) I-III and International Classification Retinoblastoma (ICRB) B and C). Methodology/Principal Findings: Retrospective review of 5 year experience in eyes with Reese Ellsworth (Table 1) I (7 eyes), II (6 eyes) or III (6 eyes) and/or International Classification (Table 2) B (19 eyes) and C (11 eyes) treated with OAC (melphalan with or without topotecan) introduced directly into the ophthalmic artery. Patient survival was 100%. Ocular event-free survival was 100% for Reese-Ellsworth Groups I, II and III (and 96% for ICRB B and C) at a median of 16 months follow-up. One ICRB Group C (Reese-Ellsworth Vb) eye could not be treated on the second attempt for technical reasons and was therefore enucleated. No patient required a port and only one patient required transfusion of blood products. The electroretinogram (ERG) was unchanged or improved in 14/19 eyes. Conclusions/Significance: Ophthalmic artery chemosurgery for retinoblastoma that was Reese-Ellsworth I, II and III (or International Classification B or C) was associated with high success (100% of treatable eyes were retained) and limited toxicity with results that equal or exceed conventional therapy with less toxicity.
Citation: Abramson DH, Marr BP, Brodie SE, Dunkel I, Palioura S, et al. (2012) Ophthalmic Artery Chemosurgery for Less Advanced Intraocular Retinoblastoma: Five Year Review. PLoS ONE 7(4): e34120. doi:10.1371/journal.pone.0034120 Editor: Thomas Claudepierre, University of Leipzig, Germany Received September 14, 2011; Accepted February 22, 2012; Published April 24, 2012 Copyright: 2012 Abramson et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Funding: This work was supported by grants from the Fund for Ophthalmic Knowledge and the Alcon Research Institute. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Competing Interests: The authors have declared that no competing interests exist. * E-mail: abramsod@mskcc.org
Introduction
Ophthalmic artery chemosurgery (OAC) for retinoblastoma was first performed 5 years ago by us as in the hope of saving eyes with extensive intraocular retinoblastoma scheduled for enucleation [1]. It has now been performed successfully in 26 countries worldwide and more than 20 peer-reviewed publications have demonstrated that the majority of eyes so treated can avoid enucleation or radiation. This has been accomplished with minimal systemic toxicity, in as few as one cycle of a single drug and with acceptable local ophthalmic toxicity. The first attempt to deliver high doses to the eye while minimizing systemic exposure was performed by Reese more than 50 years ago with a very different rationale in mind [2]. Reese delivered intra-arterial Triethylene Melanamine (TEM) (a nitrogen mustard derivative) via direct carotid artery puncture on the side to be treated in an attempt to lower the dose of therapeutic radiation used to treat retinoblastoma. Intrarterial TEM allowed him to lower the dose by 50% (from 15,000cGy to 7,500cGy) and he wrote it is amazing to see the clinical regression of a lesion following employment of x-ray together with one injection of TEM by way of the carotid artery [2].
PLoS ONE | www.plosone.org 1
Investigators from Japan then began a different form of intraarterial chemotherapy in retinoblastoma for a very different reason. They developed a balloon catheter that was introduced via the femoral artery and allowed for occlusion of the internal carotid artery on the side to be treated with rapid infusion of drugs (usually single agent melphalan) proximal to the balloon-hence they called it selective intrarterial chemotherapy [3]. They were not trying to lower the dose of radiation. In Japan clinicians faced a cultural challenge. Families of children with unilateral retinoblastoma (who could be cured of disease with just an enucleation) refused curative enucleation for cultural reasons. The physicians therefore decided that they would treat eyes with everything possible in the hope of salvaging a life by saving an eye-no matter what the ocular consequences might be. They combined their intra-arterial technique with external beam irradiation, hyperthermia, intravitreal injection of chemotherapy and focal laser and/or cryotherapy in an attempt to salvage the eye. Their recent report highlighted their success in avoiding enucleation of advanced eyes and is reassuring that no long term consequences (since 1986)-especially second cancers-were observed [4].
April 2012 | Volume 7 | Issue 4 | e34120
Five Year Review
Table 1. Reese-Ellsworth (RE) Classification Scheme.
Reese-Ellsworth (RE) Classification For Intraocular Retinoblastoma GROUP I
a. Solitary tumor, less than 4 disc diameters in size, at or behind the equator b. Multiple tumors, none over 4 disc diameters in size, all at or behind the equator
GROUP II
a. Solitary tumor, less than 4 to 10 disc diameters in size, at or behind the equator b. Multiple tumors, none over 4 to 10 disc diameters in size, all at or behind the equator
GROUP III
a. Any lesion anterior to the equator b. Solitary tumors larger than 10 disc diameters behind the equator
GROUP IV
a. Multiple tumors, some larger than 10 disc diameters b. Any lesion extending anteriorly to the ora serrata
GROUP V
a. Massive tumors involving over half the retina b. Vitreous seeding
doi:10.1371/journal.pone.0034120.t001
We introduced the technique of super selective infusion by advancing a micro-catheter into the orifice of the ophthalmic artery on the side to be treated (or both sides in the same session in cases of bilateral retinoblastoma- tandem therapy [5]) after introduction of the catheter via the femoral artery. In our initial report we demonstrated that 7 of 9 eyes scheduled for enucleation could be spared enucleation as a result of this new approach [1]. Since that first report three years ago many have reported the success and complications of this technique in (very) advanced eyes-usually scheduled for enucleation. The largest report to date is from our center. Of 95 eyes treated over a four- year period 87 were advanced (Reese-Ellsworth (RE) Groups IVV) and only 8 less advanced eyes were treated [6]. 100% of the eyes treated in Miami were advanced (RE Vb or International Classification (ICRB) Group D) [7]. Similarly 100% of the eyes treated in Switzerland were advanced [8]. Of 17 eyes treated in Philadelphia all but 2 were similarly advanced [9]. Because our systemic toxicity in treating children with advanced intraocular retinoblastoma was limited (most frequently asymptomatic Grade 3 neutropenia), we began treating less advanced retinoblastoma and now report on the success and adverse events in these patients.
number of cases in RE I-III are not the same as ICRB B and C. In particular ICRB C include eyes with vitreous seeding while in RE, by definition, no seeding is present in Groups I, II or III. Examinations under anesthesia were performed every 3 or 4 weeks and included assessment of vision, motility and pupillary responses before dilation (or anesthesia) and then after dilation (under anesthesia) an ophthalmic exam including fundus photography with the RetCam, ultrasound and retinal function monitoring with our modified full electroretinogram protocol performed (including photopic and scotopic responses) [11]. As in earlier manuscripts we report 30-Hz flicker responses as a surrogate for ERG responses. Changes in 30-Hz ERG amplitudes of less than 25 mV were considered inconsequential. Fluorescein angiograms were not done on a routine basis. This study was performed with the approval of the Institutional Review Board at Memorial Sloan-Kettering Cancer Center. Written, informed consent (from parents) was obtained for all participants in this study.
Results
The demographic data of the patient population are presented in Table 3. No patient developed metastatic disease and all patients are alive. No second cancers have developed. Catheterization was successful in all patients except one. This patient was a 7 year-old girl with chromosome 13 deletion syndrome classified as ICRB C and RE Vb. The tumor had progressed despite 6 cycles of multi-agent systemic chemotherapy elsewhere and though the first attempt was successful the second treatment could not be done for technical reasons and the eye was enucleated. The child is alive and well. Ocular event-free survival (RE Group I, II and III) and patient survival were 100% at a median follow-up from the last treatment of 16 months (range 331 months). One Group C eye was enucleated after canulation was technically impossible on the second attempt. Fundus photographs of three eyes before and after treatment with ophthalmic artery chemosurgery are seen in Figure 1. There were no seizures, strokes or hospitalizations after the procedure and no significant systemic toxicities. No child has required a port. Hematologic toxicity was graded by the standard CTCAEv4 scheme. Of 68 infusions 46 (67%) were associated with no hematologic toxicity. In 16 sessions grade III hematologic toxicity developed, in 6 sessions Grade IV toxicity developed. This
2 April 2012 | Volume 7 | Issue 4 | e34120
Methods
We have previously described our technique of ophthalmic artery chemosurgery that achieves super selective delivery of chemotherapy in the eyes of children with retinoblastoma [1,3,10]. A 4-French arterial sheath is introduced into the femoral artery (alternating sides with each successive treatment) under general anesthesia and anticoagulation attained with intravenous heparin (75I U/kg). Microcatheters are then passed into the ophthalmic artery on the side to be treated using fluoroscopy and roadmapping. Both flow-directed catheters (such as the Magic-Balt Therapeutics, Montmorency, France) with outer diameters of 400 or 500 microns and guidewire-directed catheters (such as the Excelsior SL 10 Stryker, Freemont CA) with an outer diameter of 570 microns have been used. The chemotherapy drugs are then diluted with saline in a 30cc solution, injected in a pulsatile fashion over 30 minutes. At the end of the procedure the catheter is withdrawn, the femoral puncture site is compressed for hemostasis and the child discharged the same day. Children had either RE Groups I, II or III and/or ICRB B or C (Table 3). Although both RE Groups I-III and ICRB Groups B and C are considered less advanced groups each Group uses different criteria so the actual
PLoS ONE | www.plosone.org
Five Year Review
Table 2. International Classification for Retinoblastoma (ICRB) Scheme.
International Classification for Intraocular Retinoblastoma (ICRB) Group A Small intraretinal tumors away from foveola and disc * All tumors are 3 mm or smaller in greatest dimension, confined to the retina and * All tumors are located further than 3 mm from the foveola and 1.5 mm from the optic disc Group B All remaining discrete tumors confined to the retina * All other tumors confined to the retina not in Group A * Tumor-associated subretinal fluid less than 3 mm from the tumor with no subretinal seeding Group C Discrete Local disease with minimal subretinal or vitreous seeding * * * * Group D Tumor(s) are discrete Subretinal fluid, present or past, without seeding involving up to J retina Local fine vitreous seeding may be present close to discrete tumor Local subretinal seeding less than 3 mm (2DD) from the tumor
Diffuse disease with significant vitreous or subretinal seeding * * * * Tumor(s) may be massive or diffuse Subretinal fluid, present or past without seeding, involving up to total retinal detachment Diffuse or massive vitreous disease may include greasy seeds or avascular tumor masses Diffuse subretinal seeding may include subretinal plaques or tumor nodules
Group E
Presence of any one or more of these poor prognosis features * * * * * * * Tumor touching the lens Tumor anterior to anterior vitreous face involving ciliary body or anterior segment Diffuse infiltrating retinoblastoma Neovascular glaucoma Opaque media from hemorrhage Tumor necrosis with aseptic orbital cellulites Phthisis bulbi
doi:10.1371/journal.pone.0034120.t002
includes one patient (previously treated elsewhere with multi-agent systemic chemotherapy 6 times) who developed Grade III ANC twice, Grade IV once and Grade IV platelet toxicity once and required hospitalization for febrile neutropenia. Additional treatments were performed after intra-arterial chemotherapy in 11 of the 19 RE Group I-III eyes. Eight eyes (8/19; 42%) have not received additional treatments. Three eyes received both local cryotherapy and laser ablation and 8 eyes received laser ablation only. Regarding the ICRB Group B and C eyes, 19 of the 26 retained eyes were treated with focal laser only (15 eyes), cryotherapy only (1 eye), or both (3 eyes). Compared with initial results, 30 Hz ERG responses as of the most recent follow-up examination were unchanged in 7 patients, improved by at least 25 mV in 7 patients, and decreased by at least 25 mV in 5 patients. Of those ERGs that deteriorated 4 remained in our Good category (.75 mV), which is considered a normal 30 Hz ERG response amplitude in most clinical laboratories.
Discussion
Although ophthalmic artery chemosurgery was first performed just 5 years ago for childhood retinoblastoma it has rapidly become an accepted modality that saves eyes with advanced retinoblastoma that would otherwise have been enucleated. Unlike systemic chemotherapy single agent intrarterial chemotherapy can be curative alone. Because we had such success (and minimal toxicity) in advanced eyes we have now treated 19 RE and 30 ICRB eyes with less advanced intraocular disease. All patients survived and all treatable eyes were salvaged without the need for external beam irradiation (the only eye lost was one that could not be treated for technical reasons). There are other ways to manage similar eyes. Some early staged disease can be managed with laser photocoagulation alone with success [12] but the conventional management for RE I-III was primary external beam irradiation until the 1990s.
Table 3. Study patients.
Group Total No. Eyes Age at Dx, months (range) (Enucleation or EBR) Mean follow up, months Median follow up, months Range of follow up, months
I 7 3.14 (17) 0 20.8 25 7 to 27
II 6 7.67 (116) 0 17.4 15 6 to 31
III 6 10.5 (228) 0 7.6 9 3 to 10
B 19 7.21 (128) 0 17 13.5 5 to 31
C 11 5.9 (016) 1* 15.2 13 6 to 33
*Eye enucleated after inability to repeat second IA treatment because of inability to cannulate the Ophthalmic artery. Note: Because RE I, II and III have different definitions from ICRB B and C the numbers are not equivalent. The one C eye was RE Vb. doi:10.1371/journal.pone.0034120.t003
PLoS ONE | www.plosone.org
April 2012 | Volume 7 | Issue 4 | e34120
Five Year Review
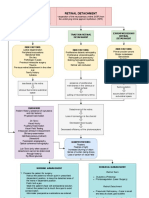
Figure 1. Digital fundus images of three retinoblastoma eyes before (left panel) and after (right panel) ophthalmic artery chemosurgery showing dramatic shrinkage of tumors without toxicity to the rest of the eye(s). doi:10.1371/journal.pone.0034120.g001
In the late 1960s Cassady reported that 78.5% of RE I-III eyes could be salvaged with radiation [13]. In the 1970s success rates of 80% were reported [14]. In the 1980s success rates of 83% were reported [15]. In the 1990s a success rate of 78.5% was reported in Groups I and II [16]. The largest report specifically on RE I-III treated with primary external beam irradiation was from our group [17]. This paper is also the only one to report specifically on radiation in RE I-III with information on ocular survival, need for additional treatment and patient survival (from metastases and second cancers). Overall, 85% of the eyes were salvaged though 53% needed additional treatments (such as laser or cryo). 4% of
patients died of metastatic retinoblastoma and Kaplan-Meier estimates of second cancer incidence was 32% at 15 years. Clinicians worldwide became progressively concerned about the risk of second cancers following radiation therapy and in the mid 1990s switched to multi-agent systemic chemotherapy as primary treatment for retinoblastoma. More than 100 papers support the success of this approach in eyes with limited disease [18]. Systemic chemotherapy (usually Carboplatin, Vincristine and Etoposide) usually causes prompt reduction in size of intraocular tumors but because sustained regression is rare supplemental focal treatments with laser, cryotherapy, radioactive plaques and even external beam irradiation are routinely employed [19]. For
4 April 2012 | Volume 7 | Issue 4 | e34120
PLoS ONE | www.plosone.org
Five Year Review
example, Gu ndu z et al. noted that no RE I-III eye was controlled with chemotherapy alone and 23% did require subsequent external beam irradiation to salvage the eye [20]. A recent report from Korea emphasized that only 86% of REI-III eyes were salvaged using multi-agent systemic chemotherapy and these authors recommended 13 cycles of chemotherapy because of persistent tumor viability [21]. They also emphasized their concern about late re-growths in eyes treated with systemic chemotherapy and the propensity for chemotherapy related second malignancies. Children with retinoblastoma have a high chance of long-term survival so complications from treatment are more than academic. As pointed out in an editorial in the Archives of Ophthalmology the overwhelming majority of papers (.90%) on the use of systemic chemotherapy (most written by ophthalmologists) for retinoblastoma include no information about side effects [22]. For those that report side effects complications such as the need for a port, transfusion, fever and neutropenia are common as is vincristine-related neurotoxicity [20]. Of further concern are recent reports highlighting late ototoxicity (as a result of carboplatin/cisplatin exposure) approaching 33% with carboplatin [2325] and 100% with cisplatin [26]. Although all of the children are too young to measure the impact on fertility, recent articles have emphasized this potential toxicity of these drugs in the pediatric cancer population and urged clinicians to find alternatives [27].
Most distressing is the recognition that children with retinoblastoma who receive chemotherapy (epipodophyllotoxins and alkylating agents) are at risk for developing secondary leukemias [28]. The true incidence is unknown but more than 20 such children have been recognized worldwide. In addition, since some (up to 24%) of children with RE I-III receiving systemic chemotherapy will require subsequent external beam irradiation the concern for radiation-related second cancers has not disappeared with the use of primary systemic chemotherapy. In conclusion, ophthalmic artery chemosurgery appears to be at least (if not more) effective than prior published series of similar eyes that were initially managed with primary radiation or systemic chemotherapy and is associated with excellent patient survival without the need for supplemental irradiation or the many unfortunate side effects of systemic chemotherapy. Many eyes achieve durable complete responses with single agent chemotherapy alone. Long-term data will be needed to confirm these encouraging findings.
Acknowledgments
We thank Lonette Sandy and Anabela C. Rodrigues for their assistance.
Author Contributions
Conceived and designed the experiments: DA YPG BM. Performed the experiments: DA YPG BM ID SB. Analyzed the data: DA SP. Wrote the paper: DA.
References
1. Abramson DH, Dunkel IJ, Brodie SE, Kim JW, Gobin YP (2008) A phase I/II study of direct intraarterial (ophthalmic artery) chemotherapy with melphalan for intraocular retinoblastoma initial results. Ophthalmology 115: 13981404. Reese AB, Hyman G, Tapley N, Forrest AW (1958) The treatment of retinoblastoma by X-ray and triethylene melamine. AMA Arch Ophthalmol 60: 897906. Kaneko A, Takayama J, Matsuoka H, Inomata M, Moori M (1990) Chemothermotherapy was successful in two cases of recurrence on intraocular retinoblastoma after irradiation [in Japanese]. Rinsho Ganka 44: 289292. Suzuki S, Yamane T, Mohri M, Kaneko A (2011) Selective ophthalmic arterial injection thereapy for intraocular retinoblastoma: the long-term prognosis. Ophthalmology 118: 20817. Abramson DH, Dunkel IJ, Brodie SE, Marr B, Gobin YP (2010) Bilateral superselective ophthalmic artery chemotherapy for bilateral retinoblastoma: tandem therapy. Arch Ophthalmol 128: 370372. Gobin YP, Dunkel IJ, Marr BP, Brodie SE, Abramson DH (2011) Intra-arterial Chemotherapy for the Management of Retinoblastoma: Four-Year Experience. Arch Ophthalmol 129: 7327. Vajzovic LM, Murray TG, Aziz-Sultan MA, Schefler AC, Wolfe SQ, et al. (2010) Supraselective intra-arterial chemotherapy: evaluation of treatmentrelated complications in advanced retinoblastoma. Clinical Ophthalmology 5: 171176. Munier FL, Beck-Popovic M, Balmer A, Gailard MC, Bovey E, et al. (2011) Ocurrence of sectoral choroidal occlusive vasculopathy and retinal anteriolar embolization after siperselective ophthalmic artery chemotherapy for advanced intraocular retinoblastoma. Retina 31: 566573. Shields CL, Bianciotto CG, Jabbour P, Ramasubramanian A, Lally SE, et al. (2011) Intra-arterial chemotherapy for retinoblastoma report no.1, control of retinal tumors, subretinal seeds, and vitreous seeds. Arch Ophthalmol 150: E1E8. Abramson DH (2010) Super selective ophthalmic artery delivery of chemotherapy for intraocular retinoblastoma: chemosurgery the first Stallard lecture. Br J Ophthalmol 94: 39699. Brodie SE, Gobin YP, Dunkel IJ, Kim JW, Abramson DH (2009) Persistence of retinal function after selective ophthalmic artery chemotherapy infusion for retinobalstoma. Doc Ophthalmol 119: 1322. Abramson DH, Schefler AC (2004) Transpupillary thermotherapy as initial treatment for small intraocular retinoblastoma: technique and predictors of success. Ophthalmology 111: 984991. Cassady JR, Sagerman RH, Tretter P, Ellsworth RM (1969) Radiation therapy of retinoblastoma: An analysis of 230 cases. Radiology 93: 405409. Egbert PR, Donaldson SS, Moazed K, Rosenthal AR (1978) Visual results and ocular complications following radiotherapy for retinoblastoma. Arch Ophthalmol 96: 18261830. 15. McCormick B, Ellsworth R, Abramson D, Haik B, Tome J, et al. (1988) Radiation therapy for retinoblastoma: Comparison of results with lens-sparing vs. lateral beam techniques. Int J Radiat Oncol Biol Phys 15: 567574. 16. Hernandez JC, Brady LW, Shields JA, Shields CL, DePotter P, et al. (1996) External beam radiation for retinoblastoma: results, patterns of failure, and a proposal for treatment guidelines. Int J Radiat Oncol Biol Phys 35: 125132. 17. Abramson DH, Ellsworth RM, Tretter P, Javitt J, Kitchin FD (1981) Treatment of bilateral groupds I through III retinoblastoma with bilateral radiation. Arch Ophthalmol 99: 17611762. 18. Kim JW, Abramson DH, Dunkel IJ (2007) Current managemnet strategies for intraocular retinoblastoma. Drugs 67: 21732185. 19. Friedman DL, Himelstein B, Shields CL, Shields JA, Needle M, et al. (2000) Chemoreduction and local ophthalmic therapy for intraocular retinoblastoma. J Clin Oncol 18: 1217. 20. Gu ndu z K, Gunalp I, Yalcindag N, Unal E, Tacyildiz N, et al. (2004) Causes of chemoreduction failure in retinoblatsoma and analysis of associated factors leading to eventual treatment with external beam radiotherapy and enucleation. Ophthalmology 111: 19171924. 21. Kim JH, Yu YS, Khwarg SI, Choi HS, Shin HY, et al. (2003) Clinical result of prolonged primary chemotherapy in retinoblastoma patients. Korean J Ophthalmol 17: 3543. 22. Rizzuti AE, Dunkel IJ, Abramson DH (2008) The adverse events of chemotherapy for retinoblastoma: what are they? Do we know? Arch Ophthalmol 126: 862865. 23. Jehanne M, Lumbroso-Le Rouic L, Savignoni A, Aerts I, Mercier G, et al. (2009) Analysis of ototoxicity in young children receiving carboplatin in the context of conservative management of unilateral or bilateral retinoblastoma. Pediatr Blood Cancer 52: 63743. 24. Pecora Liberman PH, Schultz C, Schmidt Goffi-Gomez MV, Antoneli CB, Motoro Chojniak M, et al. (2011) Evaluation of ototoxicity in children treated for retinoblastoma: preliminary results of a syetmic audiological evaluation. Clin Transl Oncol 13: 348352. 25. Bhagat SP, Bass JK, White ST, Qaddoumi I, Wilson MW, et al. (2010) Monitoring carboplatin ototoxicity with distortion-product otoacoustic emissions in children with retinoblastoma. Int J Pediatr Otorhinolaryngol 74: 11561163. 26. Toral-Martinnon R, Collado-Corona MA, Mora-Magana I, Leal-Leal C, Gutierrez-Castrellon P, et al. (2006) Evaluation of cisplatin ototoxicity by the audiometric curve in retinoblastoma. Cir Cir 74: 7982. 27. Oktay K, Rodriguez-Wallberg K, Schover L (2009) Preservation of fertility in patients with cancer. N Engl J Med 185: 24301. 28. Gombos DS, Hungerford J, Abramson DH, Kingston J, Chantada G, et al. (2007) Secondary acute myelogenous leukemia in patients with retinoblastoma: is chemotherapy a factor? Ophthalmology 114: 13781383.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13. 14.
PLoS ONE | www.plosone.org
April 2012 | Volume 7 | Issue 4 | e34120
You might also like
- Jurnal Mata 5Document6 pagesJurnal Mata 5Dahru KinanggaNo ratings yet
- 8894 Jacobs2017Document11 pages8894 Jacobs2017Fahrizal Al-fatihNo ratings yet
- Ledderose2021 Article EndoscopicEndonasalRepairOfComDocument7 pagesLedderose2021 Article EndoscopicEndonasalRepairOfComAlejandra Oliveros VargasNo ratings yet
- Articulo 8Document7 pagesArticulo 8Marcela RodriguezNo ratings yet
- Lower Eyelid Complications Associated With Transconjunctival Versus Subciliary Approaches To Orbital Floor FracturesDocument5 pagesLower Eyelid Complications Associated With Transconjunctival Versus Subciliary Approaches To Orbital Floor Fracturesstoia_sebiNo ratings yet
- Steriod Cataract PDFDocument4 pagesSteriod Cataract PDFLisa IskandarNo ratings yet
- Episcleral Brachytherapy For RetinoblastomaDocument6 pagesEpiscleral Brachytherapy For Retinoblastomamadimadi11No ratings yet
- Multimodal Treatment in Pediatric Orbital Rhabdomyosarcoma: About 8 CasesDocument3 pagesMultimodal Treatment in Pediatric Orbital Rhabdomyosarcoma: About 8 CasesIJAR JOURNALNo ratings yet
- Efficacy of Second-Course Intra-Arterial Chemo-Therapy in Children For Advanced Retinoblastoma Recurrence After Intra-Arterial ChemotherapyDocument4 pagesEfficacy of Second-Course Intra-Arterial Chemo-Therapy in Children For Advanced Retinoblastoma Recurrence After Intra-Arterial ChemotherapyilhamNo ratings yet
- Effective Dose of Dental CBCT LudlowDocument25 pagesEffective Dose of Dental CBCT LudlowMaríaPazSalinasVillagraNo ratings yet
- Retinoblastoma - EyeWikiDocument11 pagesRetinoblastoma - EyeWikimay171989No ratings yet
- Prophylactic Cervical Lymph Node Irradiation Provides No Benefit For Patients of Stage IE Extranodal Natural Killer/t Cell Lymphoma, Nasal TypeDocument8 pagesProphylactic Cervical Lymph Node Irradiation Provides No Benefit For Patients of Stage IE Extranodal Natural Killer/t Cell Lymphoma, Nasal TypeCleysser Antonio Custodio PolarNo ratings yet
- Tugas Ibu RetinoblastomaDocument7 pagesTugas Ibu RetinoblastomamalaNo ratings yet
- Efficacy and Toxicity of Intravitreous Chemotherapy For Retinoblastoma: Four-Year ExperienceDocument8 pagesEfficacy and Toxicity of Intravitreous Chemotherapy For Retinoblastoma: Four-Year ExperienceSlr RandiNo ratings yet
- Pediatric Orbital Cellulitis Experience from Tertiary CenterDocument3 pagesPediatric Orbital Cellulitis Experience from Tertiary CenterMuthu V RanNo ratings yet
- Splenectomy For Immune Thrombocytopenic Purpura: Surgery For The 21st CenturyDocument4 pagesSplenectomy For Immune Thrombocytopenic Purpura: Surgery For The 21st Centurykevin stefanoNo ratings yet
- Brolucizumab EstudioDocument13 pagesBrolucizumab EstudioJuan Carlos Mejía SernaNo ratings yet
- Iris Melanoma Diagnosis and Conservative Treatment OutcomesDocument7 pagesIris Melanoma Diagnosis and Conservative Treatment Outcomesmiftahul masruriNo ratings yet
- Articol MedicalDocument4 pagesArticol MedicalCBkingstonNo ratings yet
- None 3Document11 pagesNone 3Yehiel FlaviusNo ratings yet
- Serial Laser Treatment Controls Vocal Fold LeukoplakiaDocument8 pagesSerial Laser Treatment Controls Vocal Fold LeukoplakiaG WNo ratings yet
- Surgical Intervention of Periocular Infantile Hemangiomas in the Era of β-BlockersDocument4 pagesSurgical Intervention of Periocular Infantile Hemangiomas in the Era of β-BlockersLuisa Fernanda ArboledaNo ratings yet
- Penetrating Keratoplasty in Active Acanthamoeba KeratitisDocument5 pagesPenetrating Keratoplasty in Active Acanthamoeba Keratitisdrvishalkulkarni2007No ratings yet
- Alamanos 2016Document12 pagesAlamanos 2016dana40018256No ratings yet
- PBC 20606Document5 pagesPBC 20606skocabzzNo ratings yet
- Primary Surgery Versus Chemoradiotherapy For Advanced Oropharyngeal Cancers: A Longitudinal Population StudyDocument7 pagesPrimary Surgery Versus Chemoradiotherapy For Advanced Oropharyngeal Cancers: A Longitudinal Population StudyLuvita Amallia SyadhatinNo ratings yet
- Differences Between Children and Adults With Otitis Media With Effusion Treated With CO Laser MyringotomyDocument7 pagesDifferences Between Children and Adults With Otitis Media With Effusion Treated With CO Laser MyringotomyIndra PratamaNo ratings yet
- Tic Treatment of Teeth With Apical Period On Tit Is Single vs. Multi Visit TreatmentDocument6 pagesTic Treatment of Teeth With Apical Period On Tit Is Single vs. Multi Visit Treatmentgpv38No ratings yet
- PARS Reader's Digest - Jan 2013Document9 pagesPARS Reader's Digest - Jan 2013info8673No ratings yet
- Miiringotomi OMEDocument7 pagesMiiringotomi OMEamaliaNo ratings yet
- The Number of Karyorrhexis in PatientsDocument5 pagesThe Number of Karyorrhexis in PatientsAdhitya Sofiyati DewiNo ratings yet
- Clinical Characteristics and Surgical Outcomes in Patients With Intermittent ExotropiaDocument6 pagesClinical Characteristics and Surgical Outcomes in Patients With Intermittent ExotropiaIkmal ShahromNo ratings yet
- Survival and Complications of Zygomatic Implants (PDFDrive)Document36 pagesSurvival and Complications of Zygomatic Implants (PDFDrive)Lê Minh KhôiNo ratings yet
- Retina Clinica Trials Update - 0813 - Supp2Document16 pagesRetina Clinica Trials Update - 0813 - Supp2cmirceaNo ratings yet
- Otolaryngology Journal Article on Proliferative Verrucous LeukoplakiaDocument2 pagesOtolaryngology Journal Article on Proliferative Verrucous LeukoplakiaGus JanantaraNo ratings yet
- PARS Reader's Digest - Apr 2013Document12 pagesPARS Reader's Digest - Apr 2013info8673No ratings yet
- 102 FullDocument5 pages102 FullMohebNo ratings yet
- Effets Pronostiques de La Chirurgie Ou de La Radiothérapie Sur Le Carcinome Adénoïde Kystique de La Tête Et Du CouDocument17 pagesEffets Pronostiques de La Chirurgie Ou de La Radiothérapie Sur Le Carcinome Adénoïde Kystique de La Tête Et Du CouMamadou DIENENo ratings yet
- Dental ArticleDocument7 pagesDental ArticleBen LevineNo ratings yet
- Engel 2018Document11 pagesEngel 2018GonzaloNo ratings yet
- Research ArticleDocument10 pagesResearch ArticleastutikNo ratings yet
- 157 161 RadiotherapyDocument5 pages157 161 RadiotherapyEko SetiawanNo ratings yet
- European Multicenter Trial of The Prevention of Cystoid Macular Edema After Cataract Surgery in Nondiabetics: ESCRS PREMED Study Report 1Document11 pagesEuropean Multicenter Trial of The Prevention of Cystoid Macular Edema After Cataract Surgery in Nondiabetics: ESCRS PREMED Study Report 1salvadorNo ratings yet
- Landmark Studies in GlaucomaDocument53 pagesLandmark Studies in GlaucomaDrEknathPawarNo ratings yet
- 10.1007@s00405 016 3899 3Document5 pages10.1007@s00405 016 3899 3Vincentius Novian RomilioNo ratings yet
- Radiofrequency Ablation of Small Follicular Neoplasms Initial Clinical OutcomesDocument8 pagesRadiofrequency Ablation of Small Follicular Neoplasms Initial Clinical Outcomesivan dario hernandez erazoNo ratings yet
- 02 In-Office Laryngeal Procedures (IOLP) in CanadaDocument6 pages02 In-Office Laryngeal Procedures (IOLP) in CanadaG WNo ratings yet
- Ultrasound in Emergency Medicine: Use of Ocular Ultrasound For The Evaluation of Retinal DetachmentDocument5 pagesUltrasound in Emergency Medicine: Use of Ocular Ultrasound For The Evaluation of Retinal DetachmentZarella Ramírez BorreroNo ratings yet
- Medip,+15 59 1 CEDocument7 pagesMedip,+15 59 1 CEKabir Ahmed LaskarNo ratings yet
- Fractionated Radiation For MeningiomasDocument2 pagesFractionated Radiation For MeningiomasGil LedermanNo ratings yet
- Outcomes of Descemet Membrane Endothelial Keratoplasty in Patients With PreviouDocument6 pagesOutcomes of Descemet Membrane Endothelial Keratoplasty in Patients With PreviouRaúl Plasencia SaliniNo ratings yet
- Health Effects From Exposure To Dental Diagnostic X-Ray: Environmental Health and ToxicologyDocument6 pagesHealth Effects From Exposure To Dental Diagnostic X-Ray: Environmental Health and ToxicologyhelmysiswantoNo ratings yet
- Pediatric Sialoblastoma Evaluation and ManagementDocument22 pagesPediatric Sialoblastoma Evaluation and ManagementDear Farah SielmaNo ratings yet
- 247 2011 Article 2201 PDFDocument13 pages247 2011 Article 2201 PDFArdianNo ratings yet
- Powell 1995Document9 pagesPowell 1995Phạm Thanh NhânNo ratings yet
- A Painful Red EyeDocument2 pagesA Painful Red EyeCristhian Agustin ParedesNo ratings yet
- What's New in Spine Surgery: Specialty UpdateDocument11 pagesWhat's New in Spine Surgery: Specialty UpdatePoliceNo ratings yet
- Lack of Efficacy of Long-Term, Low-Dose Azithromycin in Chronic Rhinosinusitis: A Randomized Controlled TrialDocument12 pagesLack of Efficacy of Long-Term, Low-Dose Azithromycin in Chronic Rhinosinusitis: A Randomized Controlled Trialpaijo09No ratings yet
- Choroidal NeovascularizationFrom EverandChoroidal NeovascularizationJay ChhablaniNo ratings yet
- Blepharitis: A Comprehensive Clinical GuideFrom EverandBlepharitis: A Comprehensive Clinical GuideAsim V. FarooqNo ratings yet
- Schaum S Outline of Human A PDFDocument193 pagesSchaum S Outline of Human A PDFFahlevie EpinNo ratings yet
- I12 Surg Hand Scrub - 2 - 121945 PDFDocument6 pagesI12 Surg Hand Scrub - 2 - 121945 PDFFikaAriskaNo ratings yet
- Tranexamic Acid For Spontaneous Intracerebral Hemorrhage A Randomized Controlled Pilot TrialDocument7 pagesTranexamic Acid For Spontaneous Intracerebral Hemorrhage A Randomized Controlled Pilot TrialAnsh NviariyntiNo ratings yet
- PTC EngDocument39 pagesPTC EngFahlevie Epin100% (1)
- DM Retinopati JurnalDocument36 pagesDM Retinopati JurnalAmelia PutriNo ratings yet
- Diabetic Retinopathy:: Prevention, Treatment and DietDocument2 pagesDiabetic Retinopathy:: Prevention, Treatment and DietFahlevie EpinNo ratings yet
- DM Retinopati JurnalDocument36 pagesDM Retinopati JurnalAmelia PutriNo ratings yet
- Primary Trauma Care: Authors Douglas A Wilkinson and Marcus W SkinnerDocument51 pagesPrimary Trauma Care: Authors Douglas A Wilkinson and Marcus W SkinnerFahlevie EpinNo ratings yet
- Diabetes Retinopathy GuidelineDocument24 pagesDiabetes Retinopathy GuidelineFahlevie EpinNo ratings yet
- Antibiotics: Choices For Common InfectionsDocument30 pagesAntibiotics: Choices For Common InfectionsAlfeus GradyNo ratings yet
- WHO Pain LadderDocument1 pageWHO Pain LadderBagus Burhan MuhammadNo ratings yet
- STEMI-Optimal Antiplateletantithrombotic in Emergency DepDocument5 pagesSTEMI-Optimal Antiplateletantithrombotic in Emergency DepFadhilAfifNo ratings yet
- Kuliah Urinary Tract StoneDocument31 pagesKuliah Urinary Tract StoneMisbahsaragihNo ratings yet
- Uro - Radiologi: Iskandar ZakariaDocument47 pagesUro - Radiologi: Iskandar ZakariaFahlevie EpinNo ratings yet
- Soal-Soal UKDI dr.Rahma Tsania Zhuhra FK UNANDDocument1 pageSoal-Soal UKDI dr.Rahma Tsania Zhuhra FK UNANDFahlevie EpinNo ratings yet
- 2.1 Classification of SVT by Structures Required For Initiation and Maintenance......Document1 page2.1 Classification of SVT by Structures Required For Initiation and Maintenance......Fahlevie EpinNo ratings yet
- Kul-Tumor Traktus UrogenitalDocument26 pagesKul-Tumor Traktus UrogenitalFahlevie EpinNo ratings yet
- Jurnal ReadingDocument16 pagesJurnal ReadingFahlevie EpinNo ratings yet
- Acute Diarrhea Long FINAL 120604Document24 pagesAcute Diarrhea Long FINAL 120604Aizat KamalNo ratings yet
- Kul-Tumor Traktus UrogenitalDocument21 pagesKul-Tumor Traktus UrogenitalFahlevie EpinNo ratings yet
- Kul-Tumor Traktus UrogenitalDocument26 pagesKul-Tumor Traktus UrogenitalFahlevie EpinNo ratings yet
- Paliatif CareDocument13 pagesPaliatif CareNicholas PetrovskiNo ratings yet
- 17 Visual PathwaysDocument4 pages17 Visual PathwaysFahlevie EpinNo ratings yet
- LEUKOKORIADocument3 pagesLEUKOKORIAFahlevie EpinNo ratings yet
- Rekap Pasien Stase: BTKV Tanggal:17/8/2015: Ruangan: PJTDocument7 pagesRekap Pasien Stase: BTKV Tanggal:17/8/2015: Ruangan: PJTFahlevie EpinNo ratings yet
- Daftar PustakaDocument1 pageDaftar PustakaFahlevie EpinNo ratings yet
- Peripheral Vascular DiseaseDocument8 pagesPeripheral Vascular DiseaseFahlevie EpinNo ratings yet
- ReferensiDocument1 pageReferensiFahlevie EpinNo ratings yet
- BAB V Daftar PustakaDocument2 pagesBAB V Daftar PustakaFahlevie EpinNo ratings yet
- ReferensiDocument1 pageReferensiFahlevie EpinNo ratings yet
- Term Paper ExampleDocument16 pagesTerm Paper ExampleZhengYang ChinNo ratings yet
- Use of Oral Rehydration Therapy in The Treatment of Childhood Diarrhoea in Douala, CameroonDocument5 pagesUse of Oral Rehydration Therapy in The Treatment of Childhood Diarrhoea in Douala, CameroonKiti AstutiNo ratings yet
- Department of HealthDocument2 pagesDepartment of HealthdenNo ratings yet
- Ben - Morgan A Case of Diabetes 2Document2 pagesBen - Morgan A Case of Diabetes 2api-463462603No ratings yet
- Approach To Child With Fever: Liew Qian YiDocument33 pagesApproach To Child With Fever: Liew Qian YinavenNo ratings yet
- Swellings of The JawDocument36 pagesSwellings of The JawSumaNo ratings yet
- Essay-Mike Lemuel BacayoDocument1 pageEssay-Mike Lemuel BacayoLem MikeeNo ratings yet
- Practical Review of Diagnosis and Management of Cutaneous Tuberculosis in IndonesiaDocument6 pagesPractical Review of Diagnosis and Management of Cutaneous Tuberculosis in IndonesiaAde Afriza FeraniNo ratings yet
- Monocyte: FunctionDocument9 pagesMonocyte: FunctionMatelyn OargaNo ratings yet
- Package Leaflet: Information For The User Cetirizine Hydrochloride 5 MG/ 5 ML Oral SolutionDocument7 pagesPackage Leaflet: Information For The User Cetirizine Hydrochloride 5 MG/ 5 ML Oral SolutionZulva Chairunnisa BudimanNo ratings yet
- National Geographic USA - October 2022Document140 pagesNational Geographic USA - October 2022joaquin.ca.garcia80% (5)
- Orthopaedics: Questions&AnswersDocument49 pagesOrthopaedics: Questions&AnswersRajesh Kumar AsunalaNo ratings yet
- Alpha 1 AT DefficiencyDocument22 pagesAlpha 1 AT DefficiencySensing NonsenseNo ratings yet
- MycobacteriumDocument23 pagesMycobacteriumTJ Goli CruzNo ratings yet
- Pharm 316 Case Presentation: Statins in The Golden Years - Statin For Primary Prevention in ElderlyDocument37 pagesPharm 316 Case Presentation: Statins in The Golden Years - Statin For Primary Prevention in ElderlyKevin JiaNo ratings yet
- PDF of Cor Final DessertationDocument71 pagesPDF of Cor Final DessertationJay SharmaNo ratings yet
- Contaminated Drinking Water As A Risk Factor For Colibacilosis - PlusVet Animal HealthDocument8 pagesContaminated Drinking Water As A Risk Factor For Colibacilosis - PlusVet Animal HealthEduardo ViolaNo ratings yet
- Homeopathy For Joint PainsDocument3 pagesHomeopathy For Joint PainsstarhomeoNo ratings yet
- Safety and Operating Instructions: Hydraulic Breakers RX 2, 3, 4, 6, 8Document28 pagesSafety and Operating Instructions: Hydraulic Breakers RX 2, 3, 4, 6, 8juan gonzalez burgosNo ratings yet
- Thalassemia in Iraq Review Article: AbstractDocument4 pagesThalassemia in Iraq Review Article: AbstractRana RaedNo ratings yet
- IL Junior CI Plus Rider (U149) : (IL Unit Deduction Rider - Investment Linked Insurance Plan)Document4 pagesIL Junior CI Plus Rider (U149) : (IL Unit Deduction Rider - Investment Linked Insurance Plan)Lishalini GunasagaranNo ratings yet
- Anaphylactic Reactions 397 ReportsDocument85 pagesAnaphylactic Reactions 397 ReportsJosh SingerNo ratings yet
- Medical History FormatDocument5 pagesMedical History Formatkrzia TehNo ratings yet
- Test Bank Advanced Health Assessment Clinical Diagnosis in Primary Care 6th Edition DainsDocument4 pagesTest Bank Advanced Health Assessment Clinical Diagnosis in Primary Care 6th Edition DainsCarlton Caughey100% (36)
- AQA Biology A-Level: Required Practical 6Document4 pagesAQA Biology A-Level: Required Practical 6Alfred SangNo ratings yet
- Pollution The SDocument15 pagesPollution The SWasil SaipodenNo ratings yet
- Retinal Detachment: Traction Retinal Detachment Rhegmatogenous Detachment Exudative/Serous Retinal DetachmentDocument3 pagesRetinal Detachment: Traction Retinal Detachment Rhegmatogenous Detachment Exudative/Serous Retinal DetachmentJordz Placi100% (1)
- TOPIC 6 - Regulatory ControlDocument8 pagesTOPIC 6 - Regulatory ControlOliver100% (1)
- Value of Chest Ultrasound in Diagnosis of Community Acquired PneumoniaDocument5 pagesValue of Chest Ultrasound in Diagnosis of Community Acquired PneumoniaHarlan SiMarmutNo ratings yet
- Transes 1 (PEDIATRICS-LAB)Document2 pagesTranses 1 (PEDIATRICS-LAB)Ashley Judd EmpaynadoNo ratings yet