Professional Documents
Culture Documents
Protokol Kemoterapi
Uploaded by
Dala VWOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Protokol Kemoterapi
Uploaded by
Dala VWCopyright:
Available Formats
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
CHEMOTHERAPY PROTOCOLS
V10.0
Issue Date:
30th October 2012
Page 1 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
CCC Chemotherapy Protocols
2012
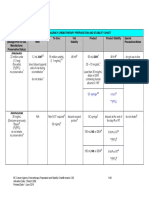
General observations ................................................................................................................................. 5 Protocol Additions 2012............................................................................................................................. 5 Cancer Drugs Fund ................................................................................................................................... 5 Off Protocol Treatment Policy ................................................................................................................... 5 Trials .......................................................................................................................................................... 5 Co-payments / top-ups / additional private care........................................................................................ 5 Dose Capping............................................................................................................................................ 6 Breast Cancer.............................................................................................................................................. 7 Adjuvant..................................................................................................................................................... 7 Neo-adjuvant ........................................................................................................................................... 11 Advanced disease ................................................................................................................................... 12 Patients with compromised liver or marrow function............................................................................... 16 Bone directed therapy ............................................................................................................................. 18 Management of patients with HER2 positive cancers............................................................................. 19 Gastrointestinal Cancer............................................................................................................................ 21 Oesophageal Carcinoma......................................................................................................................... 21 Adjuvant ............................................................................................................................................... 21 Neoadjuvant......................................................................................................................................... 21 Gastric / Adenocarcinomas of Gastro-oesophageal junction Carcinoma ............................................... 24 Neoadjuvant / Adjuvant........................................................................................................................ 24 Adjuvant ............................................................................................................................................... 24 Pancreatic cancer.................................................................................................................................... 28 Adjuvant ............................................................................................................................................... 28 Cholangiocarcinoma / Gall Bladder Carcinoma ...................................................................................... 31 Advanced ............................................................................................................................................. 31 Hepatocellular carcinoma* ...................................................................................................................... 33 Neuroendocrine tumours ......................................................................................................................... 34 Colorectal ................................................................................................................................................ 36 Adjuvant ............................................................................................................................................... 36 Rectal cancer - Chemoradiation.............................................................................................................. 38 Advanced Colorectal Cancer................................................................................................................... 39 Anal Carcinoma ....................................................................................................................................... 47 Gynaecological Cancer ............................................................................................................................ 49 Epithelial Ovarian Cancer........................................................................................................................ 49 Epithelial Ovarian Cancer Mucinous Histology .................................................................................... 56 Endometrial Carcinoma ........................................................................................................................... 58 Cervical Cancer ....................................................................................................................................... 60 Adjuvant ............................................................................................................................................... 60 Haematological Malignancies .................................................................................................................. 65
Issue Date: 30th October 2012 Page 2 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Hodgkins disease .................................................................................................................................... 65 Non-Hodgkins Lymphoma....................................................................................................................... 67 Head and Neck Cancer ............................................................................................................................. 72 Nasopharyngeal Carcinoma.................................................................................................................... 75 Thyroid Cancer ........................................................................................................................................ 76 Lung Cancer ..............................................................................................................................................77 Small Cell ................................................................................................................................................ 77 Non-Small Cell Lung Cancer ................................................................................................................... 80 Mesothelioma ............................................................................................................................................ 87 Melanoma................................................................................................................................................... 88 Sarcomas ................................................................................................................................................... 89 Soft Tissue Sarcoma ............................................................................................................................... 89 Adjuvant ............................................................................................................................................... 89 Neo-adjuvant........................................................................................................................................ 89 Osteosarcoma / MFH of bone / Leiomyosarcoma of Bone ..................................................................... 91 Advanced Osteosarcoma ........................................................................................................................ 93 Ewings Sarcoma...................................................................................................................................... 94 Neoadjuvant......................................................................................................................................... 94 Aggressive fibromatosis .......................................................................................................................... 99 Rhabdomyosarcoma ............................................................................................................................... 99 IVADo Regime for High Risk Rhabdomyosarcoma............................................................................... 101 Gastro-intestinal Stromal Tumours (GIST)............................................................................................ 103 Urological Cancer ................................................................................................................................... 104 Bladder Cancer - Transitional cell ......................................................................................................... 104 Renal cancer ......................................................................................................................................... 108 Prostate Cancer..................................................................................................................................... 111 Germ Cell Tumours ............................................................................................................................... 113 Adjuvant ............................................................................................................................................. 113 Primary CNS Malignancy ....................................................................................................................... 117 Adjuvant Temozolomide .................................................................................................................... 117 Primary CNS Lymphoma ........................................................................................................................ 121 Adenocarcinoma of Unknown Primary Origin ..................................................................................... 124 CCC Emergency Chemotherapy Drugs ................................................................................................ 125 Bone Metastases..................................................................................................................................... 126 CCC anti-emetic guidelines for cytotoxic chemotherapy ................................................................... 127 GCSF ........................................................................................................................................................ 130 Primary Prophylaxis............................................................................................................................... 130 Secondary Prophylaxis.......................................................................................................................... 130 Erythropoietin.......................................................................................................................................... 132 Intrathecal (IT) Chemotherapy ............................................................................................................... 133 Creatinine Clearance .............................................................................................................................. 134
Issue Date: 30th October 2012 Page 3 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Calvert formula for Carboplatin dosage ............................................................................................... 134 Cisplatin dose guidelines....................................................................................................................... 134 Cisplatin Hydration Policy...................................................................................................................... 135 Haematological Indices Guidelines for the administration of chemotherapy ............................... 136 Capecitabine-........................................................................................................................................... 136 Renal function recommendations ......................................................................................................... 136 Neutropenic Sepsis Policy ..................................................................................................................... 137 Platelet Transfusion Policy .................................................................................................................... 138 Hypocalcaemia ........................................................................................................................................ 138 Hypomagnesaemia ................................................................................................................................. 138 Ifosfamide Encephalopathy and Methylene Blue ................................................................................ 139 Ifosfamide Renal Toxicity....................................................................................................................... 139 Folinic acid rescue for High Dose Methotrexate ................................................................................. 140 CCC Dose Banding Policy...................................................................................................................... 140 Surface Area Nomogram ........................................................................................................................ 148
Issue Date:
30th October 2012
Page 4 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
General observations
There is now an electronic version of the protocol book which is available on CCO Comms and the CCC internet site. This will be updated as required during the year and represents the working version of the book. The paper version will continue but will only be updated annually.
Protocol Additions 2012
Maintenance pemetrexed in advanced NSCLC
Pazopanib in advanced renal cell carcinoma
Gefitinib in advanced NSCLC
In addition we have included all drugs currently funded by the Cancer Drugs Fund. Please refer to the NW Cancer Drugs Fund website for the latest funding policy and conditions for approval. Please note that there may be a 90 day period before a NICE approved drug is funded routinely and therefore doesnt need a CDF application.;
Cancer Drugs Fund
A number of treatments are now available via the Cancer Drugs Fund. The process for accessing the fund is as follows:
Complete the relevant application form which can be found on the North West Cancer Drugs Fund web site. The easiest way to find this is to type nw cancer drugs fund into google and select the application forms button in the header on the home page.
E-mail the completed form to the pharmacy dept at CCC using: ccf-tr.CytoPharmacy@nhs.net this address can be found by typing cco pharmacists into the address book in outlook.
Off Protocol Treatment Policy
Inevitably situations will arise that are not covered by the standard CCC protocols. Consultants who wish to use a non-protocol regimen should complete the non-protocol treatment form and submit it to the Clinical Director for Chemotherapy for approval at least 5 days prior to the date of cycle 1 of the proposed treatment. All reasonable requests will be granted.
Trials
Entry to clinical trials should be considered for all patients but individual studies have not been listed due to frequent changes.
Co-payments / top-ups / additional private care
The uptake of co-payments has been minimal and has been further reduced by the introduction of the Cancer Drugs Fund. However the process is still in place and is outlined below.
Issue Date: 30th October 2012 Page 5 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Co-payment refers to top-up funding by an NHS patient for an otherwise unavailable treatment. NHS policy allows patients to fund elements of their care not currently available on the NHS without losing their entitlement to continue with free NHS care.
The CCC co-payments policy considers access to systemic cancer treatments - chemotherapy or targeted therapies - that are currently not funded for use in NHS patients. A copy of the policy can be obtained from pharmacy or found on the CCC website and includes all the required documentation:
Co-payment algorithm Additional Private Treatment Form Patient information leaflet. Financial agreement forms.
The self-funded drug may be a single agent or given in combination with standard treatments, in which case the costs incurred relate only to the self-funded drug. However it should always be clear which components of treatment are privately funded and which are provided as NHS treatments.
The patient commits to self-funding the treatment for the duration of the entire programme under supervision by the responsible consultant i.e. a specific number of cycles or indefinite period while there is evidence of a maintained benefit and response. This will include the costs of treatment preparation and delivery, payment of any investigations needed, and any supportive care drugs given as a direct consequence of receiving the self-funded treatment.
Dose Capping
In line with ASCO guidelines we have removed routine dose capping for patients with a surface area in excess of 2m .
2
Issue Date:
30th October 2012
Page 6 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Breast Cancer
Adjuvant
Epi-CMF
2
Epirubicin 100mg/m IV day 1 repeated at 21 day intervals x 4 cycles
followed by CMF x 4 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion LV ejection fraction prior to cycle 1 if history of cardiac problems FBC prior to each cycle. CMF Cyclophosphamide Methotrexate Fluorouracil 100mg/m po 40mg/m IV 600mg/m IV
2 2 2
days 1-14 in divided doses days 1 and 8 days 1 and 8
For patients unable to tolerate oral cyclophosphamide substitute IV cyclophosphamide 600mg/m days 1 and 8
2
Folinic acid rescue not normally required unless patients develop signs of Methotrexate toxicity, then 15mg 6 hourly x 6 doses starting 24hrs post Methotrexate with subsequent cycles
Cycles are repeated at 28 days from day 1 to a total of 6 cycles.
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion but Methotrexate is hazardous in the presence of renal insufficiency FBC prior to each cycle, not required on day 8 Standard FBC limits for administration apply AC Doxorubicin 60mg/m + cyclophosphamide 600mg/m IV day 1 repeated at 21 day intervals for 4 cycles has been shown to be equivalent to 6 cycles of CMF.
2 2
Issue Date:
30th October 2012
Page 7 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion LV ejection fraction prior to cycle 1 if history of cardiac problems FBC prior to each cycle Standard FBC limits for administration apply EC Epirubicin 90mg/m IV + cyclophosphamide 600mg/m IV day 1 repeated at 21 day intervals for 4 cycles. Alternative to AC in this situation
2 2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion LV ejection fraction prior to cycle 1 if history of cardiac problems FBC prior to each cycle Standard FBC limits for administration apply FEC / Docetaxel This protocol is available for node positive or high risk node negative patients.
Patients should receive primary prophylaxis with pegfilgrastim after each cycle
2 2 2
FEC
Fluorouracil Epirubicin Cyclophosphamide
500mg/m IV day 1 100mg/m IV day 1 500mg/m IV day 1
Repeat at 21 day intervals for 3 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion LV ejection fraction prior to cycle 1 if history of cardiac problems FBC prior to each cycle Standard FBC limits for administration apply Followed by
Issue Date:
30th October 2012
Page 8 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Docetaxel 100 mg/m IV x 3 cycles at 21 day intervals
Pre-medication: Dexamethasone 8mg oral bd x 3 days start 24hrs pre-docetaxel
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Standard FBC limits for administration apply NB: See section on advanced disease for dose modifications and precautions.
Trastuzumab For patients with HER2 positive cancers
Non-metastatic potentially operable primary invasive breast cancer HER2 positive (IHC 3+ and / or FISH positive) Completed definitive surgery and radiotherapy Completed at least 4 cycles of adjuvant or neoadjuvant chemotherapy Within 9 weeks of chemotherapy / radiotherapy / surgery, whichever is last.
Trastuzumab
ECOG PS 0 or 1 Baseline LVEF normal after completing anthracycline chemotherapy No serious cardiac illness
8mg/kg IV loading dose over 90min then 6mg/kg over 60min and thereafter over 30 min every 3 weeks for 12 months (18 cycles) if no problems. May be given concurrently with docetaxel.
Stop at any time if CCF develops
LVEF at 3, 6, 9 and 12 months Stop trastuzumab if LVEF falls by 10 points or to <50% Repeat after 3-4 weeks and if LVEF: 50+ continue with trastuzumab 44-49 and within 10 points of baseline continue with trastuzumab < 44 stop trastuzumab
Issue Date:
30th October 2012
Page 9 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
In patients at significant risk of cardiac problems:
HER2 negative
2
TC
Docetaxel
75mg/m IV
2
Cyclophosphamide
600mg/m IV
Repeat at 21 day intervals for 4-6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion LV ejection fraction prior to cycle 1 if history of cardiac problems FBC prior to each cycle Standard FBC limits for administration apply HER2 positive
2
TCH
Docetaxel
75mg/m IV
Carboplatin AUC6
Trastuzumab 8mg/kg iv loading dose over 90min then 6mg/kg over 60min and thereafter over 30 min every 3 weeks for 12 months (18 cycles) if no problems commencing with first cycle of chemotherapy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion LV ejection fraction prior to cycle 1 if history of cardiac problems FBC prior to each cycle Standard FBC limits for administration apply
Issue Date:
30th October 2012
Page 10 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Neo-adjuvant
Indication / Treatment plan Patients with locally advanced disease or to allow less radical surgery in patients with operable tumours.
Options include six cycles of EC/AC or four cycles EC/AC followed by four cycles docetaxel at 100mg/m
2
HER-2 positive patients may commence trastuzumab following completion of anthracycline based treatment i.e. concurrently with docetaxel if this is being given provided LVEF normal after completion of the anthracycline. Patients should then have the remaining 14 cycles of trastuzumab as adjuvant treatment.
Patients should receive primary prophylaxis with pegfilgrastim after each cycle
2
AC/EC
Doxorubicin
60mg/m IV day 1 or
2
Epirubicin
90mg/m IV day 1 +
2
Cyclophosphamide
600mg/m IV day 1
Repeat at 21 day intervals for up to 6 cycles.
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion LV ejection fraction prior to cycle 1 if history of cardiac problems FBC prior to each cycle Standard FBC limits for administration apply Docetaxel 100 mg/m IV q 21 days x 4 cycles
2
Pre-medication:
Dexamethasone 8mg oral bd x 3 days start 24hrs pre-docetaxel
Issue Date:
30th October 2012
Page 11 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Standard FBC limits for administration apply NB: See section on advanced disease for dose modifications and precautions.
Advanced disease
First line Doxorubicin 75mg/m IV day 1
2
Repeat at 21 day intervals usually to a maximum of 6 cycles
AC/EC
Doxorubicin or Epirubicin Cyclophosphamide
50mg/m IV
2
day 1
90mg/m IV 500mg/m IV
2
day1 day 1
Repeat at 21 day intervals usually to a maximum of 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion LV ejection fraction prior to cycle 1 if history of cardiac problems FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 12 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Docetaxel
75-100 mg/m IV day 1 q 21 days, max 6 cycles
Pre-medication:
Dexamethasone 8mg oral bd x 3 days start 24hrs pre-docetaxel
Criteria
Previously received full dose anthracycline as adjuvant therapy or
Less than six months since anthracycline based adjuvant therapy or
Unsuitable for anthracycline therapy
nd rd
NB: See section on 2 /3 line treatment for dose modifications and precautions.
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Docetaxel / Capecitabine Docetaxel 75mg/m IV day 1 + Capecitabine 1000mg/m bd oral days 1-14 NB see capecitabine renal function recommendations p130
2 2
Pre-medication
Dexamethasone 8mg bd x 3 days start 24hrs pre-docetaxel
Repeat at 21 day intervals, max 6 cycles
Criteria
PS 0-1 NB very fit patients only Recurrent following adjuvant anthracycline therapy
Issue Date:
30th October 2012
Page 13 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Paclitaxel / Gemcitabine Paclitaxel 175mg/m IV
2 2
day 1
Gemcitabine
1250mg/m IV
days 1 and 8
Pre-medication
Chlorphenamine Dexamethasone Ranitidine
10mg 16mg 50mg
Repeat at 21 day intervals, max 6 cycles
Criteria PS 0-1 NB very fit patients only Recurrent following adjuvant anthracycline therapy Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply *Bevacizumab 10mg/kg IV infusion
Repeat at 14 day intervals
Criteria Advanced disease Triple negative First line chemotherapy In combination with paclitaxel
*NB available via the Cancer Drugs fund
Issue Date:
30th October 2012
Page 14 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
*Eribulin 1.23mg/m eribulin mesylate IV days 1 and 8 of a 21 day cycle
Criteria At least 2 prior chemotherapy regimens for advanced disease Evidence of response to prior chemotherapy
*NB available via the Cancer Drugs fund
Everolimus + exemestane Everolimus 10mg oral daily
Exemestane 25mg oral daily
Continue until progression / unacceptable toxicity
Criteria
progression on non-steroidal aromatase inhibitor
*NB available via the Cancer Drugs fund
Issue Date:
30th October 2012
Page 15 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Patients with compromised liver or marrow function
Doxorubicin 20mg/m IV weekly for patients with compromised liver or marrow function due to tumour infiltration
2
Laboratory Investigations Ensure normal renal function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Patients with abnormal hepatic function should be treated cautiously Where renal / hepatic function are abnormal treatment is at physician discretion LV ejection fraction prior to cycle 1 if history of cardiac problems FBC prior to each cycle. Normal limits for administration apply with the exception that for patients with marrow infiltration treatment may be continued at lower platelet and neutrophil counts at treating physician discretion.
Continue with weekly treatment usually for 6-8 weeks before changing to fortnightly or 21 day cycles depending on response. Maximum total dose 450mg/m
2 2
Paclitaxel 80mg/m IV weekly for patients with compromised liver or marrow function who have previously received anthracyclines.
Pre-medication Dexamethasone 8mg IV before first cycle 4mg IV before second and subsequent cycles Chlorphenamine Ranitidine 10mg IV 50mg IV
Laboratory investigations Ensure normal renal function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Patients with abnormal hepatic function should be treated cautiously Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle. Normal limits for administration apply with the exception that for patients with marrow infiltration treatment may be continued at lower platelet and neutrophil counts at treating physician discretion.
Issue Date:
30th October 2012
Page 16 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Vinorelbine
25 - 30mg/m IV
2
day 1 and 8 of a 21 day cycle. or
60- 80mg/m oral
day 1 and 8 of a 21 day cycle
Repeat at 21 days from day 1
Reassess after every 2 cycles, maximum 6 cycles Criteria: WHO performance status 0-1 Endocrine resistant Prior alkylating agent therapy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Capecitabine 1000-1250mg/m oral twice daily for 14 days followed by 7 days off
2
Or
2
850-1000mg/m twice daily for 14 days followed by 7 days off if heavily pre-treated or elderly NB see capecitabine renal function recommendations p130
Repeat at 21 days from day 1 for up to six cycles.
Criteria
Failed or unsuitable for anthracycline and/or taxane PS 0-2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 17 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Bone directed therapy
Bisphosphonate Zoledronic acid 4mg IV in 100mls Sodium chloride 0.9% over 15-30 minutes repeated at 28 day intervals.
Criteria:
Performance status 0-2 Symptomatic / extensive bone metastases
Calcium supplements:
Patients should have their serum calcium measured every four weeks and Adcal D3 tablets prescribed as necessary.
Renal impairment Cr clearance >60 50 - 60 40 - 49 30 39 < 30 Dose 4.0mg 3.5mg 3.3mg 3.0mg no treatment
Serum creatinine should be repeated every 4 weeks and if it rises significantly during treatment zoledronic acid should be witheld until the creatinine has returned to within 10% of the baseline prior to starting.
For patients with creatinine clearance < 30ml/min ibandronic acid 50mg weekly oral may be considered.
*This is available via the off-protocol mechanism
*Denosumab
120mg sc monthly
Criteria
Patients ineligible for IV bisphosphonate due to poor venous access or renal impairment
*NB available via the Cancer Drugs fund
Issue Date:
30th October 2012
Page 18 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Management of patients with HER2 positive cancers
Trastuzumab 4 mg/kg loading dose IV. over 90 minutes followed by 2mg/kg/week IV over 30 minutes for 8 doses then 6mg/kg every 3 weeks over 30minutes.
or
8mg/kg IV loading dose over 90min then 6mg/kg over 60min for one dose and then over 30 min thereafter if no problems every 3 weeks
Criteria:
Strongly HER2 positive (HER2 3+ by IHC or FISH positive) Trastuzumab given together with a taxane or vinorelbine as first or second line treatment or second / third line as a single agent.
NB not with anthracycline and with care within close proximity to anthracycline therapy (< 6 months).
LVEF: baseline ECHO/MUGA + 3 monthly repeat advised for patients receiving treatment with trastuzumab.
*Lapatinib (Tyverb) + capecitabine
Lapatinib 1250mg po daily continuously + Capecitabine 1000mg/m oral twice daily for 14 days followed by 7 days off or 850mg/m twice daily for 14 days followed by 7 days offif heavily pre-treated or elderly
2 2
NB see capecitabine renal function recommendations p130
Repeat at 21 days until progression or toxicity. For some responding patients continuing with lapatinib alone may be the right approach if capecitabine toxicity becomes unacceptable.
Criteria
Prior anthracycline, taxane and trastuzumab PS 0-2 IHC 3+ or FISH positive cancer
Issue Date:
30th October 2012
Page 19 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply *Available via the Cancer Drug Fund *Paclitaxel Albumin (Abraxane) 260mg/m2 IV repeat at 21 day intervals
Consider if no longer safe to continue with paclitaxel or docetaxel. Patients may be able to receive Abraxane with premedication and appropriate precautions.
Criteria Metastatic breast cancer Situations where taxanes are indicated
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply *Available via the Cancer Drugs Fund
Issue Date:
30th October 2012
Page 20 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Gastrointestinal Cancer
Oesophageal Carcinoma
Adjuvant Not currently recommended as standard therapy Neoadjuvant Cisplatin/5FU
Cisplatin Fluorouracil
80mg/m2 IV 1g/m2 over 24hrs IV or
day 1 days 1-4
Capecitabine
1000mg/m2 bd x 14 days
Repeat at 21 days for two cycles.
Criteria
PS 0-1 Cr Cl > 50ml/min Operable oesophageal cancer
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Locally advanced
Chemo-radiation protocol
2
Cisplatin/5FU
Cisplatin Fluorouracil
80mg/m IV day 1 and 29 1g/m IV over 24hrs days 1-4 and 29-32 or
2 2
Capecitabine + XRT
825mg/m oral bd Mon-Fri during XRT
followed by two additional cycles after completion of XRT
Issue Date:
30th October 2012
Page 21 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Cisplat/Capecitabine + XRT (SCOPE trial protocol) Cisplatin 60mg/m IV + Capecitabine 625mg/m oral bd
2 2
day 1
days 1-21
NB see capecitabine renal function recommendations p130
Repeat at 21 day intervals for 4 cycles with radiotherapy concurrent with cycles 3 and 4
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Metastatic Cisplatin/5FU Cisplatin Fluorouracil 80mg/m IV 1g/m IV over 24hrs or Capecitabine 1000mg/m bd x 14 days
2 2 2
day 1 days 1-4
Repeat at 21 day intervals, max 4-6 cycles
Issue Date:
30th October 2012
Page 22 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 23 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Gastric / Adenocarcinomas of Gastro-oesophageal junction Carcinoma
Neoadjuvant / Adjuvant For patients with operable cancers after initial staging
ECF/X x 3 cycles
Surgery -2 2
ECF/X x 3 cycles
ECF/X
Epirubicin Cisplatin Fluorouracil
50mg/m IV 60mg/m IV
2
day 1 day 1
200mg/m / day via continuous IV infusion for 21 days or
2
Capecitabine 625mg/m bd
days 1-21
NB see capecitabine renal function recommendations p130 Repeat at 21 day intervals
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Adjuvant EOF/X
Epirubicin Oxaliplatin Fluorouracil
50mg/m IV 130mg/m IV
2 2
day 1 day 1
200mg/m / day via continuous IV infusion for 21 days or
Capecitabine 625mg/m2 bd
days 1-21
NB see capecitabine renal function recommendations p130
Repeat at 21 day intervals for a maximum of 6 cycles Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date: 30th October 2012 Page 24 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Locally advanced / metastatic ECF/X Epirubicin Cisplatin Fluorouracil 50mg/m IV 60mg/m IV
2 2 2
day 1 day 1
200mg/m / day via continuous IV infusion for 21 days or
2
Capecitabine 625mg/m bd
days 1-21
NB see capecitabine renal function recommendations p130
Repeat at 21 day intervals for a maximum of 4-6 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply EOF/X Epirubicin Oxaliplatin Fluorouracil 50mg/m IV 130mg/m IV
2 2 2
day 1 day 1
200mg/m / day via continuous IV infusion for 21 days or
Capecitabine 625mg/m2 bd
days 1-21
NB see capecitabine renal function recommendations p130
Repeat at 21 day intervals for a maximum of 4-6 cycles
Issue Date:
30th October 2012
Page 25 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Cisplatin/fluoropyrimidine/Herceptin
2
Cisplatin
80mg/m IV day 1 Fluorouracil 1g/m over 24hrs IV days 1-4 or Capecitabine 1000mg/m bd x 14 days
2 2
Repeat at 21 day intervals for 6 cycles
Herceptin
8mg/kg IV day 1 loading dose 6mg/kg IV every 21 days until progression
Criteria
PS 0-1 Cr Cl > 50ml/min HER 2 status IHC 3+ or FISH positive
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 26 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
*Cisplatin/Teysuno
2
Cisplatin
75mg/m IV day 1 Teysuno 25mg/m bd po for 21 days
2
Repeat at 28 day intervals for up to 6 cycles
Criteria
PS 0-1 Cr Cl > 50ml/min Intolerant of capecitabine / 5FU or at high risk of cardiac toxicity
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
*available via the off protocol mechanism
Second line
2
Irinotecan
250mg/m IV day one of a 21 day cycle repeat x 4 cycles
2
Option to increase to 350mg/m if well tolerated
atropine 600micrograms s/c prior to irinotecan
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 27 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Pancreatic cancer
Adjuvant Fluorouracil+Folinic acid
Fluorouracil 425mg/m2 IV Folinic acid 50mg IV
daily days 1-5 daily days 1-5
Cycles are repeated at 28 days for 6 cycles.
NB: For patients over 70yrs and those with borderline performance status the dose of Fluorouracil should be reduced to 370mg/m2 per day.
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Gemcitabine 1g/m
2
IV weekly for 3 weeks followed by one week break Repeat 28 day cycles for up to 6 cycles.
Criteria
PS 0-2 R0, R1 resection M0
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated NB: transaminases may rise during gemcitabine therapy Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Advanced
First line
Gemcitabine + Capecitabine Gemcitabine Capecitabine 1g/m
2 2
IV days 1, 8, 15 po bd for 21 days
825mg/m
NB see capecitabine renal function recommendations p130 Repeat 28 day intervals for up to 6 cycles.
Issue Date:
30th October 2012
Page 28 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Criteria
PS 0-1
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated NB: transaminases may rise during gemcitabine therapy Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle CA19-9 every 4 weeks Day 8 or 15 Platelets 75 99 x10 /l Platelets < 75x10 /l
2 9 9
continue at full dose omit gemcitabine
Gemcitabine
1g/m
IV weekly for 3 weeks followed by one week break Repeat 28 day cycles for up to 6 cycles. or IV weekly for seven weeks followed by one week break for first cycle then 3 weeks on, one off as above.
Criteria
PS 0-2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated NB: transaminases may rise during gemcitabine therapy Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle CA19-9 every 4 weeks Day 8 or 15 Platelets 75 99 x10 /l Platelets < 75x10 /l
9 9
continue at full dose omit gemcitabine
Second line Ox-Cap Oxaliplatin Capecitabine 85 mg/m IV day 1 900mg/m oral bd x 9 days NB see capecitabine renal function recommendations p130
2 2
Repeat at 14 day intervals for 6 cycles then reassessment
Criteria
PS 0-2 Relapse < 6 months post adjuvant chemotherapy Progression free interval > 3 months following first line therapy
Issue Date:
30th October 2012
Page 29 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and creatinine prior to each cycle Normal FBC limits for administration apply with the exception that the lower limit for platelets for administration of Ox-Cap is 75 x 10 /l
2 9
OxMdG
Oxaliplatin Folinic acid Fluorouracil Fluorouracil
85 mg/m IV
2
day 1
350mg flat dose two hour IV infusion day 1 400mg/m 15 minute IV bolus 2400mg/m 46hr IV infusion start
2
day 1 day 1
Repeat at 14 day intervals for 6 cycles then reassessment
Avoid in patients with pre-existing neuropathy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply with the exception that the lower limit for platelets for administration of OxMdG is 75 x 10 /l
9
Issue Date:
30th October 2012
Page 30 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Cholangiocarcinoma / Gall Bladder Carcinoma
Advanced Gemcitabine + Cisplatin Gemcitabine 1000mg/m day 1 and 8
2 2
Cisplatin
25mg/m
day 1 and 8
Repeat at 21 day intervals for a maximum of 6 cycles
Criteria PS 0-1
Issue Date:
30th October 2012
Page 31 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle CA19-9 every 4 weeks Normal FBC limits for administration apply
2
Gemcitabine
1g/m
IV weekly for 3 weeks followed by one week break Repeat 28 day cycles for 4- 6 cycles.
Criteria
PS 0-2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle CA19-9 every 4 weeks Normal FBC limits for administration apply ECF/EOX Epirubicin Cisplatin Fluorouracil 50mg/m IV 60mg/m IV
2 2 2
day 1 day 1
200mg/m / day via continuous IV infusion or
2
Oxaliplatin Epirubicin
130mg/m IV 50mg/m IV
2 2
day 1 day 1 days 1-21
Capecitabine 625mg/m bd
NB see capecitabine renal function recommendations p130
Repeat at 21 day intervals for a maximum of 4-6 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date: 30 October 2012
th
Page 32 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Hepatocellular carcinoma*
Sorafenib Sorafenib Initial dose 200mg bd increasing to 400mg bd over 4 weeks to 400mg bd oral continuously
Continue until disease progression
Criteria
PS
0-2 Normal bilirubin Transaminases < 2xULN Normal renal function
Laboratory investigations FBC, U/Es, LFTs prior to each cycle Where renal / hepatic function are abnormal treatment is at physician discretion Discontinue if deteriorating renal or liver function Normal FBC limits for administration apply
*NB Available via the Cancer Drugs
Issue Date:
30th October 2012
Page 33 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Neuroendocrine tumours
High mitotic rate, anaplastic histology, clinically aggressive
2
Etoposide / cisplatin
Etoposide Cisplatin
120mg/m IV 70mg/m IV
2
days 1-3 days 1
Repeat at 21 day intervals max 6 cycles
Criteria
PS 0-1 Cr cl > 50ml/min Patients with rapidly progressive disease
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Low mitotic rate, well differentiated histology, clinically indolent
Somatostatin short acting analogue titrated to achieve maximum benefit then switch to long acting preparation
Pancreatic neuroendocrine tumours
*Everolimus (Afinitor)
10mg oral daily
Laboratory Investigations Ensure normal renal and hepatic function prior to each cycle 1 Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply First or Second line therapy
Criteria
*NB
Available via the Cancer Drug Fund
*Sunitinib (Sutent)
Issue Date: 30th October 2012
37.5mg oral daily
Page 34 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to each cycle 1 Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Criteria
No prior anti-VEGF therapy
*NB
Available via the Cancer Drugs Fund
Progression on first line therapy
Streptozotocin/Doxorubicin Streptozotocin Doxorubicin 500mg/m IV 50mg/m
2 2
days 1-5 repeat every 6 weeks day 1 repeat every 3 weeks
IV
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
*Octreotide
Octreotide LAR 20-30mg IM monthly
Criteria non-functioning neuroendocrine tumour of mid gut or uncertain primary origin Locally inoperable or metastatic disease Well differentiated histology
*Available via the Cancer Drugs Fund
Issue Date:
30th October 2012
Page 35 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Colorectal
Adjuvant 5FU/FA Fluorouracil 370mg/m IV + folinic acid 50 mg IV weekly x 24 weeks
2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to every fourth week Normal FBC limits for administration apply Capecitabine 1250mg/m oral twice daily for 14 days followed by 7 days off Consider 1000mg/m for patients over 70yrs
2 2
NB see capecitabine renal function recommendations p130 Repeat at 21 days from day 1 for eight cycles.
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Repeat creatinine if clinically indicated Normal FBC limits for administration apply XELOX Oxaliplatin Capecitabine 130 mg/m IV day 1 1000mg/m oral bd x 14 days
2 2
NB see capecitabine renal function recommendations p130
Repeat at 21 day intervals for 8 cycles then reassessment
Consider carefully in patients with pre-existing neuropathy
Consider omitting oxaliplatin if persistent neuropathy develops.
Issue Date:
30th October 2012
Page 36 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated. Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle. Normal FBC limits for administration apply. OxMdG Oxaliplatin Folinic acid Fluorouracil Fluorouracil 85 mg/m IV
2 2
day 1
350mg flat dose two hour IV infusion day 1 400mg/m 15 minute IV bolus 2400mg/m 46hr IV infusion
2
day 1 start day 1
Repeat at 14 day intervals for 12 cycles
Consider carefully in patients with pre-existing neuropathy
Consider omitting oxaliplatin if persistent neuropathy develops.
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply with the exception that the lower limit for platelets for administration of OxMdG is 75 x 10 /l
9
Issue Date:
30th October 2012
Page 37 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Rectal cancer - Chemoradiation
5FU + XRT Fluorouracil 1000mg/m IV days 1-4 and 22-26 (or final week)
2
Or
2
Fluorouracil 300mg/m + Folinic acid 50mg IV weekly during the radiotherapy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Capecitabine + XRT Capecitabine 825mg/m oral bd Mon-Fri during XRT NB see capecitabine renal function recommendations p130
2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC each week during chemotherapy Normal FBC limits for administration apply 5FU/FA Fluorouracil 300mg/m IV + folinic acid 50 mg IV weekly during XRT
2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to every fourth week Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 38 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Advanced Colorectal Cancer
First line
Single agent
MdG
MdG:
Folinic acid 350mg flat dose two hour IV infusion day 1 Fluorouracil 400mg/m 15 minute IV bolus Fluorouracil 2800mg/m 46hr IV infusion start
2 2
day 1 day 1
repeat at 14 day intervals, re-evaluate after 6 cycles.
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Capecitabine 1250mg/m oral twice daily for 14 days
2 2
Consider 1000mg/m if age >70yrs NB see capecitabine renal function recommendations p130
Repeat at 21 day intervals for a maximum of 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and creatinine prior to each cycle Normal FBC limits for administration apply Raltitrexed (Tomudex) 3mg/m IV repeat at 21 day intervals for a maximum of 6 cycles
2
Criteria:
Patients intolerant of fluoropyrimidines
Issue Date:
30th October 2012
Page 39 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and creatinine prior to each cycle Normal FBC limits for administration apply Combination chemotherapy IrinMdG Irinotecan 180mg/m IV + atropine 600micrograms s/c prior to irinotecan
2
MdG:
Folinic acid 350mg flat dose two hour IV infusion day 1 Fluorouracil 400mg/m 15 minute IV bolus Fluorouracil 2400mg/m 46hr infusion
2 2
day 1 start day 1
Repeat at 14 day intervals Review after 12 weeks and consider continuing to 24 weeks if:
SD / response. Acceptable toxicity
Criteria: PS 0-2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply I-Cap Irinotecan 180mg/m IV + atropine 600micrograms s/c prior to irinotecan Capecitabine 900mg/m oral bd x 9 days NB see capecitabine renal function recommendations p130
2 2
Repeat at 14 day intervals
Review after 12 weeks and consider continuing to 24 weeks if:
SD / response. Acceptable toxicity
Criteria: PS 0-1
Issue Date:
30th October 2012
Page 40 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and creatinine prior to each cycle Normal FBC limits for administration apply OxMdG Oxaliplatin Folinic acid Fluorouracil Fluorouracil 85 mg/m IV
2 2
day 1
350mg flat dose two hour IV infusion day 1 400mg/m 15 minute IV bolus 2400mg/m 46hr IV infusion
2
day 1 start day 1
Repeat at 14 day intervals for 6 cycles then reassessment
Avoid in patients with pre-existing neuropathy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply with the exception that the lower limit for platelets for administration of OxMdG is 75 x 10 /l
2 9
Ox-Cap
Oxaliplatin Capecitabine
85 mg/m IV day 1 900mg/m oral bd x 9 days
2
NB see capecitabine renal function recommendations p130 Repeat at 14 day intervals for 6 cycles then reassessment
Avoid in patients with pre-existing neuropathy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and creatinine prior to each cycle Normal FBC limits for administration apply with the exception that the lower limit for platelets for administration of Ox-Cap is 75 x 10 /l
2 9
XELOX
Oxaliplatin Capecitabine
130 mg/m IV day 1 1000mg/m oral bd x 14 days
Page 41 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
2
Issue Date:
30th October 2012
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
NB see capecitabine renal function recommendations p130
Repeat at 21 day intervals for 4 cycles then reassessment
Avoid in patients with pre-existing neuropathy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply. OxMdG + Cetuximab Oxaliplatin Folinic acid Fluorouracil Fluorouracil Cetuximab 85 mg/m IV
2 2
day 1
350mg flat dose two hour IV infusion day 1 400mg/m 15 minute IV bolus 2400mg/m 46hr IV infusion start
2 2 2
day 1 day 1
Week 1 500mg/m IV day 1 over 2 hours using 0.2um in-line filter Then 500mg/m IV over 1 hour every 2 weeks
Premedication
Dexamethasone 8mg Chlorphenamine 10mg Ranitidine 150mg
Repeat at 14 day intervals for 6 cycles then reassessment
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and biochemistry prior to each cycle Normal FBC limits for administration apply with the exception that the lower limit for platelets for administration of OxMdG is 75 x 10 /l
9
Criteria
KRAS wild type cancer PS 0-1 Metastatic disease confined to the liver and potentially resectable if downsized Primary resected or resectable Avoid in patients with pre-existing neuropathy
Issue Date:
30th October 2012
Page 42 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
IrinMdG + Cetuximab Irinotecan Folinic acid Fluorouracil Fluorouracil Cetuximab 180mg/m IV + atropine 600micrograms s/c prior to irinotecan 350mg flat dose two hour IV infusion day 1 400mg/m 15 minute IV bolus day 1 2400mg/m 46hr infusion start day 1 Week 1 500mg/m IV day 1 over 2 hours using 0.2um in-line filter Then 500mg/m IV over 1 hour every 2 weeks
2 2 2 2 2
Premedication
Dexamethasone 8mg Chlorphenamine 10mg Ranitidine 150mg
Repeat at 14 day intervals. Review after 12 weeks and consider continuing to 24 weeks if:
SD / response. Acceptable toxicity
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and biochemistry prior to each cycle Normal FBC limits for administration apply with the exception that the lower limit for platelets for administration of OxMdG is 75 x 10 /l
9
Criteria
KRAS wild type cancer PS 0-1 Metastatic disease confined to the liver and potentially resectable if downsized Primary resected or resectable
*Bevacizumab 14 day schedules: 21 day schedules
Bevacizumab 5mg/kg IV infusion Bevacizumab 7.5mg/kg IV infusion
Criteria
Advanced colorectal cancer First line chemotherapy With oxaliplatin or Irinotecan based combination chemotherapy
*NB
Available via the Cancer Drug Fund
Issue Date:
30th October 2012
Page 43 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Second / third line chemotherapy
Irinotecan + MdG (see above)
Oxaliplatin + MdG (see above)
I-Cap (see above)
Ox-Cap (see above)
2
Irinotecan
180mg/m IV day 1 of a 14 day cycle atropine 600micrograms s/c prior to irinotecan
or
2
350mg/m IV day one of a 21 day cycle atropine 600micrograms s/c prior to irinotecan
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
*Bevacizumab
14 day schedules: 21 day schedules
Bevacizumab 5mg/kg IV infusion Bevacizumab 7.5mg/kg IV infusion
Criteria
Advanced colorectal cancer Second line chemotherapy With oxaliplatin based combination chemotherapy
*NB
Available via the Cancer Drug Fund
*Irinotecan + Cetuximab
Criteria - Must have KRAS wild type cancers - Previously responded to chemotherapy - Second or third line chemotherapy - Performance status (0-1)
Issue Date: 30th October 2012 Page 44 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Cetuximab
Week 1 Then
2
500mg/m IV day 1 over 2 hours using 0.2um in-line filter 500mg/m IV over 1 hour every 2 weeks
2
Irinotecan
180mg/m IV every 2 weeks + atropine 600micrograms s/c
Premedication Dexamethasone 8mg Chlorphenamine 10mg Ranitidine 150mg
Continue until progression / unacceptable toxicity
*Available via the Cancer Drug Fund * Cetuximab single agent Criteria - Must have KRAS wild type cancers - Previously responded to chemotherapy - Third line chemotherapy - Performance status (0,1)
2 2
Cetuximab
Week 1 Then
500mg/m IV day 1 over 2 hours using 0.2um in-line filter 500mg/m IV over 1 hour every 2 weeks
Premedication Dexamethasone 8mg Chlorphenamine 10mg Ranitidine 150mg
Continue until progression / unacceptable toxicity
*Available via the Cancer Drug Fund
2
MMC + MdG
Mitomycin-C 7mg/m IV day 1 repeat every 6 weeks (max 4 doses) + Folinic acid 350mg flat dose two hour infusion Fluorouracil 400mg/m 15 minute IV bolus day 1 Fluorouracil 2400mg/m 46hr IV infusion start day 1
2 2
Repeated at 14 day intervals
Issue Date:
30th October 2012
Page 45 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply MMC + Capecitabine Mitomycin-C 7mg/m IV day 1 repeat every 6 weeks, max 4 doses Capecitabine 1000mg/m oral bd for 14 days repeat at 21 day intervals NB see capecitabine renal function recommendations p130
2 2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and biochemistry prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 46 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Anal Carcinoma
Localised squamous carcinoma of the anus
Combined XRT + chemotherapy
2
Mitomycin C Fluorouracil Fluorouracil
12mg/m IV day 1 only (max 20mg) 1000mg/m IV over 24hrs days 1-4 1000mg/m IV over 24hrs daily x 4 during final week of XRT or
2 2 2
Capecitabine
825mg/m bd oral on each XRT treatment day NB see capecitabine renal function recommendations p130
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Palliative / Metastatic
2
Cisplatin/5FU
Cisplatin Fluorouracil
60mg/m IV (max 120mg) 1g/m IV over 24hrs or
2 2
day 1 days 1-4
Capecitabine
1000mg/m bd x 14 days
Repeat at 21 day intervals max 4 courses
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 47 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Mitomycin C / Fluoropyrimidine Mitomycin C Fluorouracil 7mg/m IV day 1 repeat every 6 weeks, max 4 cycles 1000mg/m IV over 24hrs days 1-4 repeat at 21 day intervals or Capecitabine 1000mg/m bd po days 1-14 repeat at 21 day intervals
2 2 2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 48 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Gynaecological Cancer
Epithelial Ovarian Cancer
First Line Chemotherapy
Paclitaxel/Carboplatin Paclitaxel Carboplatin
175mg/m2 AUC 5/6
IV over 3 hours IV over 1 hour
Paclitaxel premedication
Chlorphenamine Dexamethasone Ranitidine
10mg 20mg 50mg
Repeat at 21 day intervals maximum 6 courses
Criteria
Stage Ib-IV
Minimal residual disease / bulk residual disease PS 0-1 Cr Cl > 50ml/min
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply *Paclitaxel/Carboplatin/Bevacizumab Paclitaxel Carboplatin Bevacizumab 175mg/m IV over 3 hours AUC 5/6 IV over 1 hour 7.5mg/kg
2
Paclitaxel premedication
Chlorphenamine Dexamethasone Ranitidine
10mg 20mg 50mg
Repeat at 21 day intervals maximum 6 cycles chemotherapy max 18 cycles bevacizumab Criteria Stage III (residual disease >1cm) or IV PS 0-1 Cr Cl > 50ml/min
Issue Date: 30 October 2012
th
Page 49 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply *Available via the cancer drugs Fund
or
Carboplatin
Carboplatin AUC 5/6 x (GFR + 25) IV at 21-28 day intervals x max 6 cycles
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply Second line chemotherapy Relapse > 6 months post platinum
Single agent carboplatin Carboplatin AUC 5-6 IV repeated every 28 days x 4-6 cycles
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply
Issue Date: 30th October 2012 Page 50 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0 Author: Dr. D.B. Smith Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Single agent cisplatin Cisplatin 80mg/m IV repeated every 21 days x 4-6 cycles
2
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply Paclitaxel + carboplatin See 1 line section for doses + pre-medication schedule
st
Repeat at 21 day intervals, max 6 doses
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply Carboplatin + Gemcitabine Carboplatin Gemcitabine AUC4 IV at 21 day intervals 1000mg/m IV days 1 and 8 of a 21 day cycle
2
Repeat at 21 day intervals to a maximum of 6 cycles Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply
Issue Date: 30th October 2012 Page 51 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0 Author: Dr. D.B. Smith Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Carboplatin + Liposomal Doxorubicin (Caelyx) Carboplatin Liposomal Doxorubicin (Caelyx) AUC5 30mg/m IV
2
Repeat at 28 day intervals to a maximum of 6 cycles
Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply Single agent Paclitaxel Paclitaxel 70mg/m IV weekly
2
Pre-medication Dexamethasone 8mg IV before first cycle 4mg IV before second and subsequent cycles Chlorphenamine Ranitidine 10mg IV 50mg IV
Laboratory investigations Ensure normal renal function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Patients with abnormal hepatic function should be treated cautiously Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle. Normal limits for administration apply with the exception that for patients with marrow infiltration treatment may be continued at lower platelet and neutrophil counts at treating physician discretion.
Issue Date:
30th October 2012
Page 52 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Second / Third line chemotherapy options Paclitaxel 175mg/m IV over 3hrs or 135mg/m IV over 3hrs (depending on PS / prior treatment)
2 2
Premedication
Chlorphenamine Dexamethasone Ranitidine
10mg IV 20mg IV 50mg IV
Repeat at 21 day intervals, max 6 cycles
Criteria PS 0-1 No prior taxane therapy Previous platinum
2
Liposomal doxorubicin (Caelyx) 40-45mg/m by IV infusion initially at 1mg/min q 28 days Maximum 6 cycles
Criteria
PS 0-2 Platinum resistant / refractory No evidence of intestinal obstruction
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply Topotecan 1.25mg/m daily IV over 30 minutes for 5 days q 21 days or 3mg/m IV weekly on days 1, 8, 15 of a 28 day cycle
2 2
Maximum 4 cycles
Criteria
PS 0-2 Platinum resistant / refractory Cr Cl > 40ml/min
Issue Date:
30th October 2012
Page 53 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each dose Normal FBC limits for administration apply Gemcitabine 1000mg /m IV days 1,8,15 of a 28 day cycle. Criteria PS 0-2
2
Platinum resistant / refractory
Reassess after 3 cycles, maximum 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each dose Normal FBC limits for administration apply Etoposide 50mg bd oral x 7days of 21 day cycle max 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply Chlorambucil 10mg daily oral x 14 days of 28 day cycle max 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply
Issue Date: 30 October 2012
th
Page 54 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Doxorubicin
60mg/m IV q21 days, max 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply Consider LV ejection fraction if history of cardiac disease
Issue Date:
30th October 2012
Page 55 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Epithelial Ovarian Cancer Mucinous Histology
First line Carboplatin / Paclitaxel or single agent carboplatin
Platinum refractory
2
Capecitabine 1250mg/m oral twice daily for 14 days NB see capecitabine renal function recommendations p130
Repeat at 21 day intervals for a maximum of 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and creatinine prior to each cycle Normal FBC limits for administration apply Capecitabine should be the treatment of choice where a central line is contra-indicated eg
I-Cap
Failed central venous catheterisation Receiving anticoagulants but NB interaction between warfarin and capecitabine
2
Irinotecan 180mg/m IV + atropine 600micrograms s/c prior to irinotecan Capecitabine 900mg/m oral bd x 9 days NB see capecitabine renal function recommendations p130
2
Repeat at 14 day intervals
Review after 12 weeks and consider continuing to 24 weeks if:
SD / response. Acceptable toxicity
Criteria: PS 0-1
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and creatinine prior to each cycle
Issue Date: 30th October 2012 Page 56 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Normal FBC limits for administration apply Ox-Cap Oxaliplatin Capecitabine 85 mg/m IV day 1 900mg/m oral bd x 9 days
2 2
NB see capecitabine renal function recommendations p130
Repeat at 14 day intervals for 6 cycles then re-assessment
Avoid in patients with pre-existing neuropathy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC and creatinine prior to each cycle Normal FBC limits for administration apply with the exception that the lower limit for platelets for administration of Ox-Cap is 75 x 10 /l
9
Issue Date:
30th October 2012
Page 57 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Endometrial Carcinoma
Epithelial
Advanced
Doxorubicin/Cisplatin/Paclitaxel Doxorubicin Cisplatin Paclitaxel 45mg/m IV 50mg/m
2 2 2
day 1 day 1 day 2
IV
160mg/m IV
Premedication
Chlorphenamine Dexamethasone Ranitidine
10mg 20mg 50mg
Maximum of 6 cycles at 21 day intervals
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Mixed Mullerian Tumours
Doxorubicin
Doxorubicin 75mg/m IV at 21 day intervals x 6 cycles depending on response
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Consider LV ejection fraction if history of cardiac disease or
2
Cisplatin Cisplatin 80mg/m IV at 21 day intervals x 6 cycles
Issue Date:
30th October 2012
Page 58 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply or
2 2
Doxorubicin/Cisplatin
Doxorubicin 50mg/m IV Cisplatin 50mg/m IV
Maximum of 6 cycles at 21 day intervals
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Consider LV ejection fraction if history of cardiac disease
Issue Date:
30th October 2012
Page 59 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Cervical Cancer
Adjuvant Not currently recommended as standard therapy
Pre-XRT
BMC
Bleomycin Mitomycin-C Cisplatin
30,000 iu IV day 1 10mg/m IV cycles 1,3 50mg/m IV day 1
2 2
Repeat every 14 days for 2-4 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Advanced Squamous Carcinoma
Cisplatin / Topotecan Criteria 1. 2. 3. >6m from completion of chemo-radiation to relapse no prior radiosensitising cisplatin PS 0-1
2
Cisplatin Topotecan
50mg/m IV 0.75mg/m IV
2
day 1 days 1-3
Repeat at 21 day intervals for 4-6 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date: 30th October 2012 Page 60 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0 Author: Dr. D.B. Smith Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Paclitaxel/Cisplatin Paclitaxel Cisplatin 135mg/m IV over 3 hours 50mg/m IV
2 2
Paclitaxel premedication
Chlorphenamine Dexamethasone Ranitidine
10mg 20mg 50mg
Repeat at 21 day intervals maximum 6 courses
Criteria
1. 2. 3.
>6m from completion of chemo-radiation to relapse no prior radiosensitising cisplatin PS 0-1
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Topotecan Topotecan 1.2mg/m (max 2mg) IV days 1-5
2
Repeat at 28 day intervals for 4-6 cycles
Criteria
1. 2. 3.
PS 0-2 <6 months post chemoradiation prior radiosensitising cisplatin
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 61 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Dose Modification Episode of neutropenic sepsis reduce dose for ensuing cycles by 40% Interval neutrophil count 0.5-1.0 x10 /l or platelets 10 50 x10 /l 20% reduction Interval neutrophil count <0.5x10 /l or platelets <10x10 /l 40% reduction
9 9 9 9
Advanced Non-squamous carcinoma
Paclitaxel/Cisplatin Paclitaxel Cisplatin 135mg/m IV over 3 hours 50mg/m IV
2 2
Paclitaxel premedication
Chlorphenamine Dexamethasone Ranitidine
10mg IV 20mg IV 50mg IV
Repeat at 21 day intervals maximum 6 courses
Criteria
1. 2. 3.
>6m from completion of chemo-radiation to relapse no prior radiosensitising cisplatin PS 0-1
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Paclitaxel Paclitaxel 135mg/m IV over 3hrs
2
Premedication
Chlorphenamine Dexamethasone Ranitidine
10mg 20mg 50mg
Repeat at 21 day intervals, max 6 cycles
Criteria
1.
PS 0-2
2. <6 months post chemoradiation 3. prior radiosensitising cisplatin
Issue Date: 30th October 2012 Page 62 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Chemo-radiotherapy schedules Criteria bulky 1B or 2B PS 0-1 Normal liver / renal / haematology
2
(1)
Cisplatin weeks
40mg/m IV (max 70mg) in 1 litre Sodium chloride 0.9% over 60min weekly x max 6
2
30mg/m if XRT fields large
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply or
2
(2)
Cisplatin Fluorouracil
80mg/m IV day 1 1g/m IV days 1-4 and 29-32
2
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Erythropoietin may be used to maintain haemoglobin levels during combined modality therapy in these patients.
Issue Date: 30th October 2012 Page 63 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Carcinoma of the Vulva
Chemoradiation Mitomycin C Fluorouracil 12mg/m (max 20mg) IV day 1 1000mg/m IV days 1-4 and 29-32
2 2
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 64 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Haematological Malignancies
Hodgkins disease
Early HD PET/CT as part of staging
Group I
Involved field XRT
Group II
ABVD x 3 + IF XRT
Group III
Three cycles full dose chemotherapy + IF XRT or 6 cycles full dose chemotherapy + IF XRT if residual abnormality
Advanced HD Stages III / IV or I / II with mediastinal bulk + / - B symptoms
2
ABVD
Doxorubicin Bleomycin Hydrocortisone Vinblastine Dacarbazine
25mg/m IV 10000iu/m IV 100mg IV 6mg/m IV 350mg/m IV
2 2 2
day 1 and 15 day 1 and 15 day 1 and 15 day1 and 15 (max 10mg) day 1 and 15
Repeat at 28 day intervals to CR + 2, min 6 max 8 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply ChlVPP Vinblastine 6mg/m IV Chlorambucil 6mg/m po Prednisolone 40mg po Procarbazine 50mg oral tds
2 2
days 1 and 8 (max 10mg) days 1-14 days 1-14 days 1-14
Repeat 28 days from day 1 x 6 cycles)
Issue Date:
30th October 2012
Page 65 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 66 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Non-Hodgkins Lymphoma
Low grade First line CVP-R Cyclophosphamide Vincristine Prednisolone Rituximab 600mg/m2 IV 1.4mg/m2 IV 50mg orally 375mg/m2 IV day 1 day 1 (maximum 2mg) days 1-5 day 1
Repeat at 21 day intervals to a maximum of 6-8 cycles.
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply *Bendamustine 120mg/m IV days 1 and 2 Repeat at 21 day intervals to a maximum of 8 cycles
2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply *NB available via the Cancer Drug Fund
2
CHOP-R
Cyclophosphamide Doxorubicin Vincristine Prednisolone Rituximab
750mg/m IV 50mg/m IV 1.4mg/m IV 50mg po 375mg/m IV
2 2 2
day 1 day 1 day 1 days 1-5 day 1
Repeat at 21 day intervals for 6 cycles
Criteria: fit patients with bulky disease
Issue Date:
30th October 2012
Page 67 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply *Maintenance Rituximab Rituximab 375mg/m
2
IV every 3 months for 2 years
Criteria CR or PR following first line therapy Must commence within 2 months of completion of first line therapy
*NB available via the Cancer Drug Fund
Mantle Cell Lymphoma
2
*Bendamustine
120mg/m IV days 1 and 2
Repeat at 21 day intervals to a maximum of 8 cycles
Criteria Option for first line therapy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply *NB available via the Cancer Drug Fund Second Line
2
*Bendamustine
120mg/m IV days 1 and 2
Repeat at 21 day intervals to a maximum of 8 cycles
Issue Date:
30th October 2012
Page 68 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Criteria Unable to receive R-CHOP Unable to receive high dose therapy
*NB available via the Cancer Drug Fund
Second / third line
Chlorambucil +/- Prednisolone
Chlorambucil + Prednisolone
10mg daily orally for 14 days
20mg oral daily for 14 days
Repeat at 28 day intervals for up to 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Fludarabine Fludarabine 40mg/m orally days 1-5 (only 3 days if heavily pre-treated)
2
Repeat at 28 day intervals max 6 cycles
Criteria
Progressed after alkylating agents and anthracyclines Age < 75yrs PS 0-1 Normal marrow function
NB: patients receiving fludarabine should have all blood products Irradiated
Issue Date:
30th October 2012
Page 69 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Rituximab Rituximab 375mg/m
2
in 500ml Sodium chloride 0.9% IV weekly x 4
Criteria
Stage III / IV follicular / Mantle cell NHL Chemoresistant (prior alkylating agent and anthracycline chemotherapy)
Normal renal / hepatic function Anticipated survival > 3 months Age < 65yrs PS 0-2 Not eligible for a clinical trial
Intermediate / High grade
Stage I CHOP x 3 + involved field XRT
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Stage II-IV
2
CHOP-R
Cyclophosphamide Doxorubicin Vincristine
750mg/m IV 50mg/m IV 1.4mg/m IV
2 2
day 1 day 1 day 1 (max. 1mg if aged >70)
Prednisolone Rituximab
50mg po 375mg/m IV
2
days 1-5 day 1
Repeat at 21 day intervals for 6 cycles
Issue Date:
30th October 2012
Page 70 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Relapsed Intermediate / High grade A proportion of patients with relapsed intermediate / high grade NHL may be salvaged with high dose chemotherapy + marrow / PBSC rescue. Patients in this situation should be discussed with the NHL MDT at the Royal Liverpool Hospital.
Issue Date:
30th October 2012
Page 71 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Head and Neck Cancer
Locally advanced disease XRT +Cisplatin/5FU Cisplatin 80mg/m IV
2 2
day 1 days 1-4
Fluorouracil 1g/m over 24hrs IV
Repeat at 21 day intervals for 2-4 cycles prior to XRT
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply or
2
XRT + Cisplatin
Cisplatin
100mg/m IV days 1, 22, and 43 with concomitant XRT
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply or
XRT + Cisplatin / 5FU / Docetaxel Cisplatin Fluorouracil Docetaxel 80mg/m IV 1000mg/m over 24hrs IV 75mg/m IV
2 2 2
day 1 days 1-4 day 1
Repeat at 21 day intervals for 3 cycles prior to CTX/XRT
Criteria
Locally advanced SCC suitable for CTX/XRT PS 0/1 Creatinine clearance > 50mls/min
Issue Date:
30 October 2012
th
Page 72 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply XRT + Cetuximab Cetuximab 400mg/m IV loading dose 1 week prior to XRT 250mg/m IV weekly during XRT
2 2
Criteria
Locally advanced SCC suitable for CTX/XRT Unsuitable for cisplatin eg creatinine clearance < 50mls/min PS 0/1
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Recurrent or Metastatic Disease
2
Cisplatin/5FU
Cisplatin Fluorouracil
80mg/m IV 1g/m IV over 24hrs
2
day 1 days 1-4
or
2
Cisplatin
Cisplatin
100mg/m IV
Repeat at 21 day intervals max 6 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date: 30th October 2012 Page 73 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0 Author: Dr. D.B. Smith Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
*Cisplatin or Carboplatin + /5FU + Cetuximab Cisplatin/5FU Cisplatin 5Fluorouracil 80mg/m IV 1g/m IV over 24hrs
2 2
day 1 days 1-4
Repeat at 21 day intervals max 6 cycles Or Carboplatin/5FU Carboplatin Fluorouracil AUC 5 1g/m IV over 24hrs
2
Day 1 Days 1-4
Repeat at 21 day intervals max 6 cycles
2 2
Cetuximab
400mg/m IV loading dose week 1 250mg/m IV weekly during chemotherapy and may be continued until progression
Criteria
Ist line chemotherapy for advanced disease PS 0/1
No prior treatment with cetuximab
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
*Available via the cancer drugs fund
nd
Line Chemotherapy for advanced disease
2
Paclitaxel
135-175mg/m IV over 3hrs
Dose depends on PS and extent of prior therapy
Premedication
Chlorphenamine Dexamethasone Ranitidine
10mg IV 20mg IV 50mg IV
Repeat at 21 day intervals, max 6 cycles Criteria
Issue Date:
PS 0-1
Page 74 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
30th October 2012
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Nasopharyngeal Carcinoma
Chemoradiation + Adjuvant Chemotherapy Criteria Nasopharyngeal carcinoma Stage III/IV Creatinine clearance > 50ml/min
Chemoradiation Cisplatin 100mg/m2 days 1, 22, 43 to start prior to XRT
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply followed by: Adjuvant chemotherapy Commencing 21 days after 3rd cycle of cisplatin
2
Cisplatin Fluorouracil
80mg/m IV 1g.m IV over 24 hrs
2
day 1 days 1-4
Repeat at 21 day intervals for 3 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 75 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Thyroid Cancer
Medullary Thyroid Cancer
*Vandetanib Continue until disease progression
Criteria PS
0-2
Locally advanced unresectable / metastatic First line
Laboratory investigations FBC, U/Es, LFTs prior to each cycle Where renal / hepatic function are abnormal treatment is at physician discretion Discontinue if deteriorating renal or liver function
Normal FBC limits for administration apply
*NB available via the Cancer Drug
Papillary or Follicular Thyroid Cancer
Sorafenib
400mg bd oral continuously
Continue until disease progression
Criteria PS 0-2 Refractory to radioiodine
Laboratory investigations FBC, U/Es, LFTs prior to each cycle Where renal / hepatic function are abnormal treatment is at physician discretion Discontinue if deteriorating renal or liver function Normal FBC limits for administration apply
*NB available via the Cancer Drugs fund
Issue Date:
30th October 2012
Page 76 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Lung Cancer
Small Cell
Good PS + Limited stage
2 2
Cisplatin/etoposide
Etoposide 120mg/m IV days 1-3 (or PO 240mg/m days 2-3 in 2 divided doses)
2
Cisplatin 70mg/m IV
days 1
Repeat at 21 day intervals max 4 cycles
XRT commences with cycle 2
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Concurrent chemotherapy + XRT Cisplatin + etoposide as above with XRT commencing with cycle 2
Good / Intermediate PS Carboplatin / Etoposide Carboplatin Etoposide Etoposide AUC 5 IV 100mg/m IV 200mg/m PO in 2 divided doses
2 2
day 1 day 1 days 2 and 3
Repeat at 21 day intervals x 4 - 6 cycles
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle
Issue Date: 30th October 2012 Page 77 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Normal FBC limits for administration apply Poor PS Many poor PS patients will be too ill potentially to benefit from chemotherapy and symptomatic care will be the most appropriate option. For those judged to be fit enough the following may be considered:
(1) Carboplatin
AUC 4 / 5 IV q 21 days x 4 cycles
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply (2) Etoposide 50mg oral bd x 7 - 10 days repeat at 21 days from day 1max 6 courses
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Second Line Chemotherapy
(1) Etoposide
50mg oral bd x 7 - 10 days repeat at 21 days from day 1max 6 cycles / progression
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply (2) Carboplatin AUC x 5-6 IV q 21 days for 4 cycles
Issue Date:
30th October 2012
Page 78 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply (3) CAV Cyclophosphamide Doxorubicin Vincristine 750mg/m IV 50mg/m IV 1.4mg/m IV
2 2 2
Repeat at 21 days for 4 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply (4) Topotecan 2.3mg/m oral daily for 5 days
2
Repeat at 21 day intervals , maximum 4 cycles
Criteria
PS 0-2 Cr Cl > 40ml/min
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion CA125 prior to each cycle FBC prior to each dose Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 79 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Non-Small Cell Lung Cancer
Adjuvant Criteria Stage 1-3 completely resected PS 0-1
2 2
Cisplatin/Vinorelbine
Cisplatin
80mg/m IV day 1
2
Vinorelbine 25mg/m IV day 1 and 8 or oral 60mg/m day 1 and 8
Repeated at 21 day intervals x 3 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply or Carboplatin/Vinorelbine Carboplatin AUC x 5 IV Vinorelbine 25mg/m IV days 1 and 8 or 60mg/m oral day 1 and 8
2 2
21 28 day cycle x 3 cycles
Laboratory Investigations Ensure normal hepatic function prior to cucle 1 and repeast during subsequent cycles if clinically indicated. Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Carboplatin/Vinorelbine (split dose)
Carboplatin AUC x 2.5 IV days 1 and 8 Vinorelbine 25mg/m2 IV days 1 and 8 or 60mg/m2
oral day 1 and 8
21 28 day cycle x 3 cycles
Issue Date:
30th October 2012
Page 80 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Locally advanced Chemotherapy + XRT Cisplatin 20mg/m IV days 1-4 and 16 - 19 + Vinorelbine 15mg/m IV with XRT fractions 1, 6, 15 and 20 Followed at 4-6 weeks by: Cisplatin 80mg/m
2 2 2 2
day 1 day 1 and 8
Vinorelbine 25mg/m
Repeated at 21 day intervals x 2 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Advanced Cisplatin / Pemetrexed Cisplatin 75mg/m IV Pemetrexed 500mg/m IV
2 2
Repeat at 21 day intervals x 4 cycles
Vitamin B12 injection IM 1 week prior to start + every 9 weeks until completion
Folic acid 400micrograms daily oral during treatment Dexamethasone 4mg bd for 3 days start day before pemetrexed Stop all NSAIDS during chemotherapy
Criteria: Non-squamous carcinomas PS 0-1
Issue Date: 30th October 2012 Page 81 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Cisplatin/Vinorelbine Cisplatin 80mg/m IV day 1
2 2 2
Vinorelbine 25mg/m IV day 1 and 8 (oral vinorelbine 60mg/m day 1and 8)
Repeated at 21 day intervals x 4 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Gemcitabine/Carboplatin Carboplatin AUC x 5 IV Gemcitabine 1250mg/m IV
2
day 1 days 1 and 8
21 28 day cycle x 4 cycles
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated NB: transaminases may rise during treatment Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 82 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Carboplatin/Vinorelbine
Carboplatin Vinorelbine Or oral vinorelbine
AUC x 4/5 IV 25mg/m IV
2 2
day 1 days 1 and 8
60mg/m
days 1 and 8
21 28 day cycle x 4 cycles
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Vinorelbine 25-30mg/m IV days 1 and 8 of a 21 day cycle or 60-80mg/m oral days 1 and 8
2 2
Max 4 courses
Criteria:
No prior chemotherapy PS 0-2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Gemcitabine Gemcitabine 1000mg/m IV days 1, 8, 15 of a 28 day cycle
2
Laboratory Investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated NB: transaminases may rise during treatment Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date: 30th October 2012 Page 83 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Gefitinib (Iressa)
Gefitinib
250mg oral daily
Criteria
Locally advanced / metastatic NSCLC EGFR mutation positive First line
Erlotinib (Tarceva)
Erlotinib
150mg oral daily
Criteria
EGFR mutation positive First line
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Maintenance Pemetrexed Maintenance pemetrexed is available through the normal funding mechanism for patients who fulfil the criteria set out by NICE and who did not receive pemetrexed as part of first line therapy. For those patients who received pemetrexed as part of first line therapy and who fulfil the criteria funding is available via the CDF
Pemetrexed
500mg/m2 IV
Repeat at 21 day intervals until progression
Vitamin B12 injection IM 1 week prior to start + every 9 weeks until completion
Folic acid 400micrograms daily oral during treatment Dexamethasone 4mg bd for 3 days start day before pemetrexed Stop all NSAIDS during chemotherapy
Criteria: Non-squamous carcinomas PS 0-1 CR/PR/SD following first line chemotherapy First line CTX with Platinum + vinorelbine/paclitaxel/gemcitabine/docetaxel
*Pemetrexed
500mg/m2 IV
Issue Date:
30th October 2012
Page 84 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Repeat at 21 day intervals until progression Vitamin B12 1mg injection IM 1 week prior to start + every 9 weeks until completion Folic acid 400micrograms daily oral during treatment Dexamethasone 4mg bd for 3 days start day before pemetrexed Stop all NSAIDS during chemotherapy
Criteria: Non-squamous carcinomas PS 0-1 CR/PR/SD following first line chemotherapy First line chemotherapy with Cisplatin + Pemetrexed
*Available via the Cancer Drugs Fund
Second line Chemotherapy
2
Docetaxel
75mg/m
IV q 21 day cycle x max 4 cycles
Dexamethasone 8mg bd x 3 days start 24hrs pre-docetaxel
Criteria
PS 0-1 Previous response or stable disease to platinum based chemotherapy Progression free interval following platinum based chemotherapy > 6m
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Erlotinib (Tarceva)
Erlotinib
150mg oral daily initially for 4 weeks and continued thereafter if symptomatic or objective response
Criteria
Progression following chemotherapy for advanced disease Fit to receive docetaxel as second line therapy No prior anti EGFR therapy
Issue Date:
30th October 2012
Page 85 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 86 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Mesothelioma
Cisplatin / Pemetrexed Cisplatin 75mg/m IV Pemetrexed 500mg/m IV
2 2
Repeat at 21 day intervals for a maximum of 6 cycles
Vitamin B12 injection IM 1 week prior to start + every 9 weeks until completion
Folic acid 400micrograms daily oral during treatment Dexamethasone 4mg bd for 5 days, start day before pemetrexed Stop all NSAIDS during chemotherapy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Carboplatin / Pemetrexed Carboplatin AUC 4/5 Pemetrexed 500mg/m IV
2
Repeat at 21 day intervals for a maximum of 6 cycles
Vitamin B12 injection IM 1 week prior to start + every 9 weeks until completion
Folic acid 400micrograms daily oral during treatment Dexamethasone 4mg bd for 5 days start day before pemetrexed Stop all NSAIDS during chemotherapy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 87 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Melanoma
Advanced
2
Dacarbazine
850mg/m IV q 21 days max 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Gemcitabine + treosulphan
2
Gemcitabine 1000mg/m IV days 1 and 8 Treosulphan 3500mg/m IV days 1 and 8
2
Repeat at 28 day intervals for a maximum of 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply *Ipilimumab 3mg/kg IV over 90min
Repeat at 21 day intervals for 4 cycles
*NB available via the Cancer Drugs fund
*Vemurafenib
960mg bd until progression
Criteria
Tumour contains BRAF 600 mutation Unresectable or metastatic disease
*NB available via the Cancer Drugs fund
Issue Date:
30th October 2012
Page 88 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Sarcomas
Soft Tissue Sarcoma
Adjuvant There is no proven role for adjuvant chemotherapy for soft tissue sarcomas. However treatment may be considered when chemo-sensitive tumours such as rhabdomyosarcoma, synovial sarcoma are resected with close margins.
Neo-adjuvant Suggested protocol for down sizing prior to surgery
Doxorubicin Mesna prior to ifosfamide Ifosfamide + Mesna
20mg/m2 3g/m2
day 1,2,3 day 1,2,3
3g/m2 / 3g/m2 day 1,2,3 day 1,2,3
Mesna post ifos/mesna infusion 3g/m2
Advanced There is no evidence that combinations are superior to single agents as palliative chemotherapy
First line Doxorubicin Doxorubicin 75mg/m IV q 21 days x 6 cycles
2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Second line Ifosfamide Mesna prior to ifosfamide Ifosfamide/Mesna Mesna post ifos/mesna infusion 3g/m days 1,2,3 3g/m days 1,2,3 3g/m days 1,2,3
2 2 2
Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Repeat at 21 day intervals for up to 6 cycles Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
30th October 2012 Page 89 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Issue Date:
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Dacarbazine
800mg/m IV day 1
Repeat at 21 day intervals for up to 6 cycles Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated *Trabectedin Consider in select cases of advanced STS- Failure after treatment with anthracyclines and ifosfamide or intolerant/contraindications to anthracyclines and ifosfamide. Consider in Myxoid liposarcomas and leiomyosarcomas. PS 0-2
2
Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
1.5 mg/m as IV infusion over 24 hours every 21 days.
*NB Available via the off-protocol mechanism
Issue Date:
30th October 2012
Page 90 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Osteosarcoma / MFH of bone / Leiomyosarcoma of Bone
Neoadjuvant / Post operative schedule
PAM x 2 -> Surgery (week 10) -> PAM x 2 -> Doxorubicin - Methotrexate x 2
2 2
PAM
Cisplatin Doxorubicin Methotrexate
60mg/m IV 25mg/m IV 12g/m IV
2
day 1, 2 days 1, 2, 3 days 22 and 29
Folinic acid rescue Start 24 hrs post start of Methotrexate infusion with 30mg IV 6 hourly Switch to oral after 6 doses if not vomiting Methotrexate levels at 24, 48, 72 hrs etc. Continue until Methotrexate undetectable ie <0.1M usually 4-5 days
Methotrexate level < 0.1M <0.5-5M 5-50M >50M
Folinic acid dose 6hrly Stop rescue 15-30mg 6hrly 200mg/m 6hrly 1000mg/m 6hrly
2 2
In addition patients urinary pH should be >7 prior to starting Methotrexate infusion
NB: do not give methotrexate if renal function is abnormal or in the presence of a third space. Also avoid all non-steroidal anti-inflammatory agents prior to treatment and until Methotrexate undetectable.
Doxorubicin /Methotrexate Doxorubicin Methotrexate 37.5mg/m IV 12g/m IV
2 2
days 1, 2 days 15 and 22
Folinic acid rescue see above
Criteria
Age < 40yrs PS 0-2
Issue Date:
30th October 2012
Page 91 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Cisplatin/Doxorubicin
Cisplatin
100mg/m IV day 1
2 2
Doxorubicin 25mg/m IV days 1, 2, 3 (20mg/m days 1-3 age > 60yrs)
Repeat at 21 days x 3 cycles then surgery then 3 further cycles.
Criteria
Not suitable for PAM schedule. PS 0-2
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 92 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Advanced Osteosarcoma
Cisplatin/Doxorubicin Cisplatin 100mg/m IV
2 2
day 1 days 1, 2, 3
Doxorubicin 25mg/m IV
Repeat at 21 days x 6 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion LV ejection fraction prior to cycle 1 if history of cardiac problems FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 93 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Ewings Sarcoma
Non-metastatic Ewings Sarcoma/PNET/Askin tumour / Rhabdomyosarcoma Laboratory Investigations FBC/Biochemistry/Ca/Mg/Cl/HCO3 each cycle Early morning urine PO4, Creatinine, osmolarity at baseline and repeat every other cycle of VIDE Echo/MUGA baseline/cycle 4 if indicated/cycle 6/ end Rx / pregnant Bone scan/CT chest/MRI primary/Marrow biopsy at baseline MRI primary after cycles 2, 4, 6(omit after 2 if good response) Neoadjuvant VIDE (cycles 1-6) Vincristine Doxorubicin Mesna Etoposide Ifosfamide/Mesna Mesna 1.5mg/m (max 2mg) IV day 1 20mg/m IV 1g/m
2 2 2 2
days 1-3 day 1 days 1-3
2
150mg/m IV 1.5g/m / 1.5g/m IV 1.5g/m IV
2 2
days 1-3 days 3
Pegfilgrastim
6mg subcutaneous injection
day 4
Evaluation after cycle 4: If surgical resection likely proceed to cycles 5 and 6 If radiotherapy to be definitive local therapy proceed to cycles 5 and 6 If disease progression discontinue and consider surgery or radiotherapy If pre-surgery XRT planned proceed to cycles 5 and 6 omitting doxorubicin
Dose modifications
Haematological toxicity Delayed recovery of wbc / platelets > 6 days reduce etoposide 20% Neutropenic sepsis grade 3 or 4 reduce etoposide 20% Further episodes repeat etoposide 20% reductions
GI / Mucositis Graded 3 or 4 reduce etoposide by 20%
Cardiac function LVEF < 40% omit doxorubicin and substitute Dactinomycin1.5mg/m
2
Repeat echo after next cycle and consider reintroducing doxorubicin if LVEF has recovered.
Issue Date:
30th October 2012
Page 94 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Definitive local treatment Surgery should occur 21 days after cycle 6 or as soon as recovery allows. Radiotherapy should commence concurrent with cycle 7 omitting Dactinomycin from concurrent cycles. If radiation is required following surgery it should commence after cycle 8 omitting Dactinomycin from concurrent cycles.
2
VIA (cycles 7-14) Vincristine Dactinomycin Mesna prior to ifosfamide Ifosfamide/Mesna
1.5mg/m (max 2mg) IV 0.75mg/m (max 1.5mg)IV 1g/m
2 2 2 2 2
day 1 days 1-2 days 1-2 days 1-2 days 1-2
1.5g/m / 1.5g/m IV
Mesna post ifos/mesna infusion 1.5g/m
NB: omit Dactinomycin during radiotherapy
Haematological toxicity Delayed recovery of wbc/platelets > 6 days reduce Dactinomycin & Ifosfamide by 20% Neutropenic sepsis grade 3 /4 reduce Dactinomycin & Ifosfamide by 20% + add GCSF Further episodes should be managed with serial 20% reductions GI / Mucositis Grade 3 or 4 reduce Ifosfamide + Dactinomycin by 20%
Renal Toxicity GFR > 60 no change GFR 40-59 reduce Ifosfamide by 30%, reduce etoposide by 30% GFR < 40 switch Ifosfamide to cyclophosphamide 1500mg/m on day 1 only reduce etoposide by 30%
2
Cardiac function LVEF < 40% or 10% decrease from previous level, delay chemotherapy and repeat in 7 days. If recovered proceed with chemotherapy. If still impaired consider omission or dose reduction of Ifosfamide.
Issue Date:
30th October 2012
Page 95 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
VAC
Vincristine Dactinomycin
1.5mg/m IV (max 2mg) 0.75mg/m IV (max 1.5mg)
2 2 2 2 2
day 1 day 1-2 day 1 day 1
Mesna prior to cyclophosphamide 500mg /m IV pre cyclophosphamide Cyclophosphamide/Mesna 1500mg/m / 1500mg/m IV
Mesna post cyclo/mesna infusion 1500mg/m IV post cyclophosphamide/mesna day 1
Repeat at 21 days for 4 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
VACA (In patients unsuitable for VIDE previously NOT exposed to anthracyclines. Dactinomycin and doxorubicin on alternate cycles)
Vincristine
1.5mg/m IV (max 2mg)
2 2 2 2
day 1 day 1 day 1 day 1 days 1-3
Mesna prior to cyclophosphamide 500mg /m IV Cyclophosphamide/Mesna 1200mg/m / 1200mg/m IV
2
Mesna post cyclos/mesna infusion 1200mg/m IV Dactinomycin 0.5mg/m IV (max 1mg) Alternating with Doxorubicin 20mg/m IV
2
days 1-3
Etopside / Ifosfamide Etoposide Mesna prior to ifosfamide Ifosfamide/Mesna 120mg/m2 IV 500mg/m2 3g/m2 / 3g/m2 IV days 1-3 days 1-3 days 1-3 days 1-3
Mesna post ifos/mesna infusion 1.5g/m2 IV
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 96 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Palliative Ewings Etoposide / cisplatin Etoposide Cisplatin or Carboplatin Etoposide Etoposide AUC 5 IV 120mg/m IV 240mg/m PO
2 2
120mg/m IV 50mg/m IV
2
days 1-3 days 1-2
day 1 day1 days 2,3
Repeat at 21 day intervals max 6 cycles
Criteria
PS 0-1 Cr cl > 50ml/min for cisplatin
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Cyclophosphamide/ Topotecan Relapsed Ewings sarcoma Relapsed/ 2
nd
line rhabdomyosarcoma
2 2
Topotecan 0.75 mg/m
Days 1-5 Days 1-5
Cyclophosphamide 250 mg/m Cycle repeated every 21 days
Gemcitabine/Docetaxel Relapsed metastatic osteosarcoma Selected metastatic soft tissue sarcomas (3 line)/ uterine leiomyosarcoma Relapsed Ewings (if other 2
nd rd
line is not suitable)
2
Day 1
Gemcitabine
675 mg/m IV over 90 minutes
Issue Date:
30th October 2012
Page 97 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Day 8
Gemcitabine Docetaxel
675 mg/m2 IV over 90 minutes followed by 75-100mg/m2 IV over 60 minutes
Dexamethasone 8 mg bd for 3 days to start 24 hours pre docetaxel (ie Days 7-9)
Cycle repeated every 21 days
Irinotecan/Temozolomide Relapsed Ewings sarcoma Relapsed/ 2nd line rhabdomyosarcoma
Irinotecan 20 mg/m2 IV Temozolomide 100mg/m2 po Cycle repeated every 21-28 days
Days 1-5, Days 8-12 Days 1-5
Paclitaxel Angiosarcomas (2nd line or 1st line if not suitable for doxorubicin)
2
80 mg/m weekly up to 12 weeks 175 mg/m every 21 days (4-6 cycles, review after cycle 3)
2
Oral Etoposide Palliative metastatic Ewings or rhabdomyosarcoma
Etoposide 50-100mg bd 7-14 days (at clinicians discretion)
Issue Date:
30th October 2012
Page 98 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Aggressive fibromatosis
1 Line Tamoxifen +/- NSAIDs
nd st
Line
2 2
Methotrexate 30 mg/m (usually 50mg total dose) Vinblastine 6 mg/m (usually 10mg total dose)
Every 1-2 weeks Duration of course at clinicians discretion
Vinorelbine can replace vinblastine if neuropathy is a problem.
Rhabdomyosarcoma
Baseline investigations: FBC, U+Es, LFTs Bone chemistry CT thorax / Abdo staging Bone marrow aspirate and trephine Bone Scan If paramningeal site- CSF Consider early morning urine for phosphate, creatinine, osmolarity for Ifosfamide containing regimes
For patients aged < 40 years: IVADo regime for high risk rhabdomyosarcoma (see separate regime)
Maintenance therapy:
2
Vinorelbine 25 mg/m IV D 1, 8, 15 Cyclophosphamide 25 mg/m PO OD D 1-28 Every 28 days
2
Maintenance therapy following IVADo to be used in:
1. For Alveolar Rhabdomyosarcoma maintenance therapy following IVADo for 6 cycles ( i.e. 6 months) 2. For metastatic disease on intensive treatment, if no residual disease or limited residual disease, IVADo to be followed by maintenance treatment for 12 cycles
Issue Date:
30th October 2012
Page 99 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
For patients > 40 years: IVAD Vincristine 1.4 mg/m2 (max dose 2mg) D1 Doxorubicin 30 mg/m2 D1, D2 Mesna 1.2g/m pre ifosfamide D1,D2 Ifosfamide 3g/m D1,D2 Mesna 2.4g/m post ifosfamide in 2 divided doses D1,D2
2 2 2
Repeat at 21 day intervals for 6 cycles
VAC Vincristine Dactinomycin 1.5mg/m IV (max 2mg) 0.75mg/m IV (max 1.5mg)
2 2 2 2 2
Day 1 Day 1 and 2 Day 1 Day 1 Day 1
Mesna prior to cyclophosphamide 500mg /m IV pre cyclophosphamide Cyclophosphamide/Mesna 1500mg/m / 1500mg/m IV
2
Mesna post cyclo/mesna infusion 1500mg/m IV post cyclophosphamide/mesna
Repeat at 21 day intervals for 4-6 cycles
IVA Vincristine Dactinomycin Mesna prior to ifosfamide Ifosfamide/Mesna 1.5mg/m2 (max dose 2mg) 1.5 mg/m2 (max single dose 2mg) 1.2g/m day 3 g/m / 3 g/m2
2 2 2
Day 1 Day 1 Days 1-2 Days 1-2 Day 2
Mesna post ifos/mesna infusion 2.4g/m split into 2 doses
Repeat at 21 day intervals for 6 cycles
Issue Date:
30th October 2012
Page 100 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
IVADo Regime for High Risk Rhabdomyosarcoma
Cycle 1 Cycle 2 Cycle 3 Cycle 4
Surgery/ IVADo V V IVADo V V IVADo IVADo Radiotherapy
Week
10
Cycle 5
Cycle 6
Cycle 7
Cycle 8
Cycle 9
IVA Week 13 14 15
IVA 16 17 18
IVA 19 20 21
IVA 22 23 24
IVA 25
I=
Mesna prior to ifosfamide 1.2g/m over 1 hour Ifosfamide/Mesna 3g/ m / 3g/m over 3 hours
2 2 2
Days 1-2
Mesna post ifos/mesna infusion 2.4g/m over 8 hours (split into 2 doses)
2
V=
Vincristine 1.5mg/m (max single dose 2mg)
2
Day 1
A=
Dactinomycin 1.5 mg/m (max single dose 2mg)
2
Day 1
Do=
Doxorubicin 30 mg/m
Days 1-2 for cycles 1-4
Each cycle: WCC>2 Neutrophils> 1.0 ( or physicians discretion) Platelets > 80 Weekly vincristine to be given irrespective of pancytopenia unless unwell
rd nd
Reassess after cycle 3. If not CR or PR > 1/3 consider 2 line treatment + RT
Issue Date:
30th October 2012
Page 101 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
PAM Chemotherapy for Resectable Osteosarcoma
Cycle 1 AP 1 Week Cycle 4 AP 17 Week 18 19 M 20 M 21 A 2 3 M 4 M 5 AP 6
Cycle 2 M 7 8 9 M 10
SURGERY AP 11 12 Cycle 6 M 25 A 26 27 M 28
Cycle 3 M 13 14 15 M 16
Cycle 5 M 23 24
M 29
22
AP -
Doxorubicin 25 mg/m2
Days 1-3 Days 1-2
2
Cisplatin 60mg/m2 MA-
Methotrexate 12 g/m2 (With folinic acid rescue) Day 1 Doxorubicin 37.5 mg/m Days 1-2
Issue Date:
30th October 2012
Page 102 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Gastro-intestinal Stromal Tumours (GIST)
*Adjuvant Imatinib po 400mg daily for 36 months
Criteria
Tumour Mitoses
> 5cm > 5 mitoses/50 HPF
SI / colonic primary
*Available via the Cancer Drugs Fund
Imatinib (Glivec)
Imatinib 400mg daily orally until progression
Criteria c-Kit positive
PS 0-2
locally advanced / metastatic disease
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC / biochemistry prior to each visit Normal FBC limits for administration apply Dose reduce if significant toxicity / rising hepatic transaminases Sunitinib (Sutent)* Sunitinib 50mg orally daily for 4 weeks followed by a two week break
Criteria
PS 0-2 c-Kit positive locally advanced / metastatic disease previous response to imatinib
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC / biochemistry prior to each visit Normal FBC limits for administration apply *Available via the off protocol mechanism
Issue Date:
30th October 2012
Page 103 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Urological Cancer
Bladder Cancer - Transitional cell
Neoadjuvant Cisplatin/Gemcitabine Cisplatin Gemcitabine
2
70mg/m IV 1g /m IV
2
day 1 days 1, 8, 15
Repeat at 28 day intervals for 3 cycles prior to cystectomy
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Cisplatin / Gemcitabine split dose Cisplatin Gemcitabine 35mg/m
2 2
IV days IV days
1 and 8 1 and 8
1000mg/m
Repeated on a 21 day schedule for up to 4 cycles
Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 104 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Concurrent Cisplatin / XRT Cisplatin/XRT Cisplatin 30-40mg/m IV weekly x 4-6 weeks as an outpatient (max 60mg) IV over 1 hour
2
XRT 55Gy in 20# (4 x weekly cisplatin infusions) or XRT 64Gy in 32# (6 x weekly cisplatin infusions)
Criteria
PS 0-1 Poorly differentiated TCC bladder pT2-4a, N0, M0
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply 5FU + Mitomycin C/XRT Fluorouracil 500mg/m2 days 1-5 and 16-20 of concurrent XRT
Mitomycin C
12mg/m2
day 1 of concurrent XRT
Criteria
impaired renal function
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 105 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Advanced Cisplatin/Gemcitabine
2
Cisplatin Gemcitabine
70mg/m IV day 1 1g /m
2
IV
days 1, 8
Repeat at 21 day intervals for up to 6 cycles.
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Cisplatin / Gemcitabine split dose Cisplatin Gemcitabine 35mg/m
2 2
IV days IV days
1 and 8 1 and 8
1000mg/m
Repeated on a 21 day schedule for up to 4 cycles Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Carboplatin/Gemcitabine Carboplatin Gemcitabine AUC4 / 5 IV 1g /m IV
2
day 1 days 1, 8 of a 21 day cycle
For patients with impaired renal function
Repeat at 21/28 day intervals for up to 6 cycles.
Issue Date:
30th October 2012
Page 106 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigation Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate or measure creatinine clearance prior to first cycle and before subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 107 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Renal cancer
Advanced
First line
Interferon
Alpha Interferon
by s/c injection:
Week 1
Mon 5million units Wed 5million units Fri 10million units
Weeks 2+
10million units Mon / Wed / Fri
Criteria
PS 0-1 Relapse post nephrectomy > 12 months Low volume disease Patients should have 2 out of 3 criteria
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Sunitinib (Sutent) Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Sunitinib 50mg daily x 4 weeks followed by 2 week break
6 week cycles repeated until progression
Criteria
PS 0-1
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Pazopanib Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Pazopanib 800mg daily Criteria First line advanced disease No prior cytokine therapy
Issue Date:
30th October 2012
Page 108 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Sorafenib Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Sorafenib 400mg bd orally continuously until progression
Criteria
PS 0-1 Progression on/following cytokine therapy
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated *Temsirolimus Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Temsirolimus 25mg IV weekly
Premedication
Chlorphenamine 10mg
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Criteria
First line therapy Poor risk patients
*NB
Only available via the Cancer Drug Fund
*Everolimus (Afinitor) Everolimus10mg oral daily
Issue Date:
30th October 2012
Page 109 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to each cycle 1 Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Criteria
Second line therapy Biopsy proven RCC Must have had prior VEGF inhibitor
*NB
Only available via the Cancer Drug Fund
Issue Date:
30th October 2012
Page 110 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Prostate Cancer
Mitoxantrone Mitoxantrone 12mg/m IV (max 20mg) q 21 days Maximum total dose 140mg/m
2 2
Criteria
Endocrine refractory disease PS 0-1 Normal FBC, renal, liver function No cardiac failure
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Docetaxel Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
2
Docetaxel Prednisolone Dexamethasone
75mg/m IV q21 days 10mg daily until completion of chemotherapy 8mg bd x 3 days start 24hrs pre-docetaxel
Reassessment after two cycles and continue to a maximum of 10 only if responding or stable disease.
Criteria: WHO Performance Status 0-1 Hormone resistant
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Abiraterone Abiraterone 1000mg oral daily Prednisolone 10mg daily until completion of chemotherapy
Criteria
Castrate resistant Prior docetaxel chemotherapy
*Abiraterone
Issue Date:
Abiraterone 1000mg oral daily
Page 111 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
30th October 2012
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Prednisolone 10mg daily until completion of chemotherapy
Criteria
Castrate resistant No prior chemotherapy for advanced disease PS 0-1
*Available via the Cancer Drugs Fund
2
*Cabazitaxel
Cabazitaxel Prednisolone
25mg/m IV infusion. 10mg daily until completion of chemotherapy
premedication
Chlorphenamine 10mg Dexamethasone 16mg Ranitidine 50mg
Repeat at 21 day intervals to a maximum of 10 cycles
nd
Criteria
2 line following docetaxel PS 0-2
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
*NB
Available via the Cancer Drug Fund
Issue Date:
30th October 2012
Page 112 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Germ Cell Tumours
Adjuvant Stage I Pure Seminoma
Carboplatin
Carboplatin
AUC x 7 IV - one dose only
Laboratory investigations EDTA clearance required to calculate AUC Ensure normal hepatic function prior to treatment Normal FBC limits for administration apply
Stage I Non-seminomatous testicular GCT
Criteria: vascular or lymphatic invasion
BEP3
Bleomycin Etoposide Cisplatin
30000iu IV 165mg/m IV 50mg/m IV
2 2
day 1, 8, 15 days 1-3 days 1-2
Repeat at 21 day intervals for 2 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion Tumour markers: HCG,AFP,LDH where appropriate prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply Low risk all GCT
BEP3
Bleomycin Etoposide Cisplatin
30000iu IV 165mg/m IV 50mg/m IV
2 2
day 1, 8, 15 days 1-3 days 1-2
Repeat at 21 day intervals for 3 cycles.
Issue Date:
30th October 2012
Page 113 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion Tumour markers: HCG,AFP,LDH where appropriate prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply Intermediate / High risk all GCT
BEP5
Bleomycin Etoposide Cisplatin
30000iu IV 100mg/m IV 20mg/m IV
2 2
days 1, 5, 15 days 1-5 days 1-5
cycles 1-3
Repeat at 21 day intervals x 3 cycles then EP5 for a further 3 cycles (i.e. omit bleomycin) Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion Tumour markers: HCG,AFP,LDH where appropriate prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply CNS disease
POMB / ACE + Intrathecal (IT) Methotrexate
POMB
Day 1
Vincristine Methotrexate Folinic acid
2mg IV 1g/m IV over 24hrs (Standard dose is 300mg/m ) 15mg 6hrly x 12 doses start 12 hrs after completion of
2 2
Methotrexate Day 2 Day 3 Day 4
Issue Date:
Bleomycin Bleomycin Cisplatin
15mg IV over 24hr 15mgIV over 24 hr 120mg/m IV over 12hr
Page 114 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
2
30th October 2012
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion Tumour markers: HCG,AFP,LDH where appropriate prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply ACE Dactinomycin Etoposide Cyclophosphamide 0.5mg IV 100mg/m IV 500mg/m IV
2 2
days 1-3 days 1-3 day 3
Intrathecal (IT) Methotrexate
12.5mg flat dose (folinic acid rescue 15mg 6hrly x 4 start at 24hrs)
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Repeat cycles at 14 days from day 1, POMB, POMB, ACE, POMB, ACE etc 4-5 cycles of POMB.
Initial organ failure
2
Low dose cisplatin / etoposide
Cisplatin 20mg/m IV Etoposide 100mg/m IV Repeat daily x 2-3days depending on clinical situation
2
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion Tumour markers: HCG,AFP,LDH where appropriate prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 115 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Relapsed NSGCT
2
TIP
Paclitaxel Ifosfamide Cisplatin
175mg/m IV 3hr infusion day 1 1000mg/m (+mesna) IV days 1-5 20mg/m IV
2 2
days 1-5
Premedication
Chlorphenamine Dexamethasone Ranitidine
10mg IV 20mg IV 50mg IV
Repeat at 21 day intervals x 4 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion Tumour markers: HCG,AFP,LDH where appropriate prior to each cycle FBC prior to each cycle Normal FBC limits for administration apply High dose chemotherapy May be curative in selected patients with drug sensitive relapsed disease.
Issue Date:
30th October 2012
Page 116 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Primary CNS Malignancy
Glioblastoma Multiforme concomitant Temozolomide + XRT
2
Temozolomide
75mg/m oral daily day 1 to completion of XRT
Dose 1 hour pre-XRT and in am at weekends
Co-trimoxazole 960mg oral daily Mon / Wed / Fri until lymphocyte count normal after completing XRT
Laboratory investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC weekly if neutrophils < 1.5 or Platelets < 100
Withhold Temozolomide until neuts > 1.5 and platelets > 100
If neutrophils < 0.5 or platelets < 10 stop Temozolomide
Criteria
Age 18 70 PS 0 1 Absence of HIV, chronic hepatitis B and hepatitis C
Adjuvant Temozolomide Temozolomide 150mg/m oral 200mg/m oral
2 2
days 1-5 cycle 1 days 1-5 cycle 2-6 if nadir neutrophil count > 1.5 on cycle 1
Laboratory investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply If at any time neutrophil recovery is delayed by > 21 days treatment is discontinued
Issue Date:
30th October 2012
Page 117 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Astrocytoma
First line
Lomustine (CCNU) 40mg oral daily days 1-4 Repeat at 4-6 week intervals until progression / unacceptable toxicity
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Second line (1) Temozolomide Temozolomide 150mg/m oral daily for 5 days Escalate to 200mg/m /day for 5 days depending on toxicity
2 2
Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Repeat at 28 day intervals maximum 6 cycles
Criteria: PS 0-3 Glioblastoma multiforme / anaplastic astrocytoma Prior nitrosourea Adequate marrow reserve (plts >100 neut > 1.5) No prior Temozolomide
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Third line options Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
(1)
Etoposide
50mg oral bd for 14 days q 21-28 days
Issue Date:
30th October 2012
Page 118 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated (2) Procarbazine Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
2
100-150mg/m /day oral days 1-14 repeated every 28 days
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Oligodendroglioma / mixed tumours
First line
2
PCV
Procarbazine
60mg/m oral
2 2
days 8-21 day 1 day 8 and 29
Lomustine (CCNU) 110mg/m oral Vincristine 1.4mg/m (max 2mg) IV
Repeat on a 6 week schedule
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Second line Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Consider radiotherapy
Issue Date:
30th October 2012
Page 119 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Third line Temozolomide Temozolomide 150mg/m oral daily for 5 days
2 2
Escalate to 200mg/m /day for 5 days depending on toxicity
Repeat at 28 day intervals maximum 6 cycles
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 120 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Primary CNS Lymphoma
De Angelis (Modified) Vincristine 1.4mg/m (max 2mg) IV bolus weeks 2,
2 2
Weeks 1, 5, 9
Day -1-7 allopurinol 300mg/day
Methotrexate
3500mg/m IV over 6 hours
With adequate folinic acid rescue (see below) and urinary alkalinisation
2
Procarbazine
100mg/m oral daily for 7 days
Weeks 3, 7
2
Vincristine
1.4mg/m (max 2mg) IV bolus weeks 2,
2
Methotrexate
3500mg/m IV over 6 hours
With adequate folinic acid rescue (see below) and urinary alkalinisation
Dexamethasone
16mg/day week 1 12mg / day week 2 8mg/day week 3 6mg/day week 4 4mg/day week 5 2mg/day week 6
Folinic acid rescue Start 24 hrs post start of Methotrexate infusion with 30mg IV 6 hourly Switch to oral after 6 doses if not vomiting Methotrexate levels at 24, 48, 72 hrs etc. Continue until Methotrexate undetectable ie <0.1M usually 4-5 days
Methotrexate level < 0.1M <0.5-5M 5-50M >50M
Folinic acid dose 6hrly Stop rescue 15-30mg 6hrly 200mg/m 6hrly 1000mg/m 6hrly
2 2
Issue Date:
30th October 2012
Page 121 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
In addition patients urinary pH should be >7 prior to starting Methotrexate infusion
NB: do not give methotrexate if renal function is abnormal or in the presence of a third space. Also avoid all non-steroidal anti-inflammatory agents prior to Rx and until Methotrexate undetectable.
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer methotrexate only if clearance is > 50mls/min Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply Medulloblastoma (adult) Relapse following surgery / XRT
First line PCV Procarbazine Lomustine Vincristine 60mg/m oral 110mg/m oral
2 2 2
days 8-21 day 1
1.4mg/m (max 2mg) IV day 8 and 29
Repeat on a 6 week schedule
Laboratory investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Second line
2
Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Temozolomide
Temozolomide 150mg/m oral daily for 5 days
2
Escalate to 200mg/m /day for 5 days depending on toxicity
Repeat at 28 day intervals maximum 6 cycles
Issue Date:
30th October 2012
Page 122 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Laboratory Investigations Ensure normal renal and hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 123 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Adenocarcinoma of Unknown Primary Origin
Possible GI primary MdG / capecitabine / gemcitabine
Possible breast primary Manage as for similar stage breast cancer
Possible ovarian primary Carboplatin 5 x (GFR+25)
Possible lung primary
Carboplatin / Gemcitabine
Midline nodal disease
+/- lung metastases
BEP3 x max 4 cycles depending on response Undifferentiated carcinoma Etoposide / platinum
2 2
Etoposide Cisplatin
120mg/m days 1-3 (or oral 240mg/m ) 70mg/m days 1
2
Repeat at 21 day intervals max 6 cycles
Laboratory investigations Ensure normal hepatic function prior to cycle 1 and repeat during subsequent cycles if clinically indicated Calculate creatinine clearance prior to each cycle and administer cisplatin according to guidelines Where renal / hepatic function are abnormal treatment is at physician discretion FBC prior to each cycle Normal FBC limits for administration apply
Issue Date:
30th October 2012
Page 124 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
CCC Emergency Chemotherapy Drugs
Likely cancers requiring treatment: Lymphoma Germ Cell Tumours Small Cell Lung Cancer
Drugs Available Cisplatin Etoposide Doxorubicin Cyclophosphamide Vincristine Pegfilgrastim 30mg in 250ml Sodium chloride 0.9% x 2 doses 100mg x 2 doses 50mg 800mg 2mg 6mg
These drugs will be stored in oncology pharmacy in the fridge in the dispensary area labelled Fridge 3. The fridge will be labelled as containing Emergency Chemotherapy Drugs. Cisplatin will be stored at room temperature on top of fridge 3.
Emergency chemotherapy should be prescribed by a consultant and entry to the pharmacy will be via the CCC bleep holder only.
Issue Date:
30th October 2012
Page 125 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Bone Metastases
There is increasing evidence from studies in a number of malignancies that intravenous bisphosphonate therapy can ameliorate bone pain and reduce the risk of skeletal complications in patients with bone metastases. At present for suitable patients the recommended treatment is zelodronate + Adcal D3 until progression.
Bisphosphonates
Zoledronic acid 4mg IV in 100mls Sodium chloride 0.9% over 15-30 minutes repeated at 28 day intervals.
Criteria:
Performance status 0-2 Symptomatic / extensive bone metastases
Calcium supplements: Patients should have their serum calcium measured every four weeks and Adcal D3 prescribed as necessary.
Renal impairment:
Cr clearance (Cockcroft-Gault) >60 50 - 60 40 - 49 30 39 < 30
Dose of zoledronic acid
4.0mg 3.5mg 3.3mg 3.0mg no treatment
Serum creatinine should be repeated every 4 weeks and if it rises significantly during treatment zoledronic acid should be witheld until the creatinine has returned to within 10% of the baseline prior to starting.
Ibandronate (Bondranat) Bondranat has yet to be shown to be as effective as zoledronic acid in reducing the incidence of skeletal events and thus we cannot recommend it as routine treatment. However for patients who have difficulties with venous access or renal impairment it may be requested via the off protocol mechanism.
*Denosumab
Denosumab 120mg sc monthly Criteria Patients ineligible for IV bisphosphonate due to poor venous access or renal impairment
*NB Available via the Cancer Drugs Fund
Issue Date: 30th October 2012 Page 126 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
CCC anti-emetic guidelines for cytotoxic chemotherapy
Oral And IV anti-emetic formulations have equivalent efficacy
CCC Classification of chemotherapy by emetic potential (updated February 2012) LEVEL AGENT High Emetic Risk Cisplatin 50mg/m (>90 % frequency of Cyclophosphamide > 1500mg/m emesis) Dacarbazine Procarbazine (oral) Streptozocin AC Combination defined as either doxorubicin or epirubicin with cyclophosphamide 2 Doxorubicin >60mg/m 2 Epirubicin >90ml/m 2 Ifosfamide > 10g/m Moderate Emetic Risk (30-90 % frequency of emesis) Bendamustine Carboplatin Cisplatin < 50mg/m Cyclophosphamide 1500mg/m Cyclophosphamide (oral) Dactinomycin 2 Doxorubicin <60mg/m 2 Epirubicin <90mg/m Etoposide (oral) Ifosfamide <10g/m Interferon alpha >10million international 2 units/m Irinotecan Lomustine Melphalan >50mg/m Methotrexate> 250 mg/m Oxaliplatin Temozolomide (oral) Vinorelbine (oral)
2
Low Emetic Risk (10-30 % frequency of emesis)
Cabazetaxel Capecitabine Docetaxel Doxorubicin (Liposomal) Eribulin Etoposide (IV) Evorolimus Fludarabine (oral) Fluorouracil Gemcitabine
Interferon alpha >5 <10million 2 international units/m Methotrexate >50mg/m < 250mg/m Mitomycin Mitoxantrone Nilotinib Paclitaxel Paclitaxel-albumin (Abraxane) Pemetrexed Sunitinib Topotecan Vandetanib Melphalan (oral low-dose) Methotrexate 50mg/m Pazopanib Panitumumab Rituximab Sorafenib Rituxumab Temsirolimus Trastuzumab Vinblastine Vincristine Vinorelbine (IV)
Minimal Emetic Risk (<10 % frequency of emesis)
Alemtuzumab Alpha Interferon Bevacizumab Bleomycin Cetuximab Chlorambucil (oral) Erlotinib Fludarabine Gefitinib Imatinib (oral) Interferon alpha <5million 2 international units/m Ipilimumab Lapatinib
Page 127 of 148 Filename:
Issue Date:
30th October 2012
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Emetic Risk HIGH CISPLATIN REGIMENS Aprepitant 125mg PO day 1, 80mg PO daily days 2-3 + Dexamethasone 12mg PO/IV day 1then 4mg BD PO days 2-4 (as TTH) + Ondansetron 24mg PO or 12mg IV (maximum 32mg) day 1 + Domperidone 10-20mg four times a day as required HIGH NOT CONTAINING CISPLATIN Dexamethasone 12mg IV/oral PO/IV day 1 then 4mg BD PO days 2-4 (as TTH) + Ondansetron 24mg PO or 12mg IVday 1, then 8mg twice a day PO days 2-4 (as TTH) + Domperidone 10-20mg four times a day as required
Second Line
Antiemetic Failure
Ondansetron 8mg + dexamethasone 8mg + Lorazepam 1mg by IV infusion over 24 hours
Ensure antiemetics have been taken regularly. Commence on first line antiemetics for breakthrough nausea and vomiting Treat on subsequent courses of chemotherapy with second line agents
Aprepitant 125mg PO day 1, 80mg PO daily days 2-3 + Dexamethasone 12mg PO/IV day 1then 4mg twice a day PO days 2-4 (as TTH) + Ondansetron 24mg PO or 12mg IV (maximum 32mg) day 1
Ensure antiemetics have been taken regularly. Commence on first line antiemetics for breakthrough nausea and vomiting Treat on subsequent courses of chemotherapy as for second line
MODERATE Dexamethasone 8mg PO/IV day 1 then 4mg twice a day PO days 2-4 (as TTH) + Ondansetron 16mg PO or 8mg IV (maximum 32mg/day) day 1 + Domperidone 10-20mg four times a day as required LOW Dexamethasone 8 mg PO or IV day 1 + Domperidone 10-20mg four times a day as required Aprepitant 125mg PO day 1, 80mg PO daily days 2-3 + Dexamethasone 12mg PO or IV days 1-4 + Ondansetron 16-24mg PO or 8-12mg IV (maximum 32mg) day 1 Ensure antiemetics have been taken regularly. Commence on first line antiemetics for breakthrough nausea and vomiting Treat on subsequent courses of chemotherapy as for high risk Ensure antiemetics have been taken regularly. Commence on first line antiemetics for breakthrough nausea and vomiting Treat on subsequent courses of chemotherapy as for moderate risk Recommend Domperidone post chemotherapy to be taken regularly. Commence on first line antiemetics for breakthrough nausea and vomiting Treat on subsequent courses of chemotherapy as for low risk
Page 128 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
MINIMAL Routine prophylaxis not always required. Domperidone 10-20mg four times a day as required
Issue Date:
30th October 2012
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
ALTERNATIVES/BREAKTHROUGH Cyclizine 50mg three times a day is often used for protracted nausea Prochlorperazine 5-10mg oral three times a day Prochlorperazine Suppositories 25mg three times a day Metoclopramide 10-20mg four times a day Levomepromazine 6mg at night (this can be increased to 12mg)
Issue Date:
30th October 2012
Page 129 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
GCSF
Primary Prophylaxis
Patients receiving FEC/Docetaxel adjuvant chemotherapy for breast cancer, EC/AC neoadjuvant chemotherapy for breast cancer and VIDE for STS have a high risk of neutropenic events and in line with ASCO guidelines we recommend primary prophylaxis with pegfilgrastim 6mg 24hrs post chemotherapy.
Secondary Prophylaxis
In other situations where the risk of neutropenic events is lower we do not routinely recommend primary prophylaxis with GCSF and CCC policy is that secondary prophylaxis is reserved for the following situations:
(1) To maintain dose intensity in potentially curable malignancies where the dose limiting toxicity is neutropenia eg
Germ cell tumours Intermediate / high grade lymphomas Hodgkins disease Sarcomas prior to potentially curative surgery Adjuvant chemotherapy
Thus if chemotherapy is delayed due to a neutropenic episode defined as either:
9
Infection associated with neutropenia (neutrophil count < 1.0x10 /l) or
9 9
Total wbc < 3.0x10 /l and neutrophil count < 1.0 x10 /l on the day the chemotherapy cycle was due.
Then prophylaxis with pegfilgrastim 6mg s/c administered 24hrs post chemotherapy.
(2) Infection associated with protracted neutropenia > 7 days
There is no evidence that giving GCSF to patients with neutropenic sepsis improves outcomes in terms of survival or reduced incidence of medical sequelae. However for febrile patients with neutropenia lasting more than 7 days GCSF may be considered.
Issue Date:
30th October 2012
Page 130 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Palliative Chemotherapy Patients who are receiving palliative chemotherapy should be managed with appropriate dose reductions if problems with neutropenia arise.
Prophylactic antibiotics The use of prophylactic antibiotics following cyctotoxic chemotherapy can result in a small reduction in febrile episodes but at the expense of side effects and the potential risk of inducing antibiotic resistance and increasing the risk of clostridium difficile infection. The use of prophylactic antibiotics is not therefore recommended routinely but should be reserved for patients thought to be at particularly high risk of infection. The current CCC protocol is:
Ciprofloxacin 500mg oral BD days 9 20 post chemotherapy dependent on nadir
Issue Date:
30th October 2012
Page 131 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Erythropoietin
Erythropoietin may be used to maintain haemoglobin levels during chemotherapy in patients where transfusion is contra-indicated e.g.
Religious grounds Cardiac failure
In addition erythrpoietin may be considered in patients who have required two or more transfusions and who are due to receive further chemotherapy.
Erythropoietin may also be used to maintain haemoglobin levels during combined modality therapy for cervical cancer.
Protocol Hb > 12 no treatment required
Hb < 12
darbepoetin 150micrograms / sc weekly
If Hb rises to > 14 stop until Hb < 12 then restart at 100micrograms / week
If Hb rises by > 2g/dl / month reduce dose to 100micrograms / week
If Hb does not rise after 4 weeks treatment increase to 300micrograms / week
If no response after a further weeks then stop treatment.
Issue Date:
30th October 2012
Page 132 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Intrathecal (IT) Chemotherapy
Department of Health regulations now dictate that intra-thecal chemotherapy may only be prepared and administered by specific named individuals.
Prescriptions must be written on the intra-thecal prescription form Patients must receive any IV chemotherapy prior to IT treatment The doctor administering the IT drugs must collect them in person from pharmacy. The drugs must be checked by the doctor and a qualified chemotherapy nurse prior to administration All staff members involved (doctor, nurse, pharmacist) must be on the current IT chemotherapy register.
Methotrexate is the only drug we use as intrathecal therapy at a flat dose of 12.5mg.
Cytosine, thiotepa and hydrocortisone may also be given intrathecally.
All other chemotherapy drugs are potentially lethal when administered intrathecally
In addition any diluent used to prepare an intrathecal drug must be aqueous based and not alcohol based.
Intrathecal chemotherapy must always be given under the direction of a consultant and administered by one of the doctors on the CCC approved list.
Issue Date:
30th October 2012
Page 133 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Creatinine Clearance
Wright Creatinine Clearance Formula
Women ((6580 (38.8 x age)) x bsa x 0.832) /creatinine
Men
((6580 (38.8 x age)) x bsa ) /creatinine
NB
Weight in kg Creatinine in umol/l
Calvert formula for Carboplatin dosage
Carboplatin dose in mg = AUC x (Creatinine clearance + 25)
Desired area under the curve (AUC) normally 4-6 depending on protocol and clinical situation
Cisplatin dose guidelines
Cisplatin is nephrotoxic and thus patients must have their renal function measured prior to each cycle.
Creatinine clearance > 50mls /min
Cisplatin dose 100%
40 50 mls / min
75%
< 40mls / min
no further cisplatin
Patients should only commence cisplatin chemotherapy if they have an adequate performance status ie 0-2. The only exception to this is patients with advanced germ cell tumours with poor PS who may commence treatment with low dose etoposide / platinum.
Patients should only receive second and subsequent cycles of cisplatin if they are well and have suffered no deterioration in performance status.
Issue Date:
30th October 2012
Page 134 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Cisplatin Hydration Policy
Cisplatin doses 20 40mg/m2 (Outpatients) Cisplatin in 1000mL Sodium Chloride 0.9% Cisplatin doses 20 40mg/m2 (Inpatients) Prehydration Sodium Chloride 0.9% 500mL Monitor urine Output Cisplatin in 1000mL Sodium Chloride 0.9% Sodium Chloride 0.9% 500mL IV over 1 hour IV over 1 hour IV over 1 hour IV over 1 hour
Post-hydration
Cisplatin doses 41 - 80mg/m2 (Inpatients/Daycase) Furosemide Sodium Chloride 0.9% 1000mL (+ 20mmol Potassium Chloride) Monitor Urine Output Cisplatin in 1000mL Sodium Chloride 0.9% Sodium Chloride 0.9% 1000mL (+ 20mmol Potassium Chloride ) PO 20mg IV over 90 minutes
Prehydration
Post-hydration
IV over 90 minutes IV over 90 minutes
Cisplatin doses >81mg/m2 (Inpatients) Furosemide Sodium Chloride 0.9% 1000mL (+ 20mmol Potassium Chloride) Monitor Urine Output Cisplatin in 1000mL Sodium Chloride 0.9% Sodium Chloride 0.9% 1000mL (+ 20mmol Potassium Chloride) Sodium Chloride 0.9% 1000mL PO 20mg IV over 2 hour
Prehydration
Post-hydration
IV over 4 hours IV over 4 hour IV over 4 hour
n.b. Where Urine Output is of concern, please contact a clinician for advice.
Issue Date:
30th October 2012
Page 135 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Haematological Indices Guidelines for the administration of chemotherapy
(1) Platelets > 100x10 /l + Total WBC > 3 x10 /l + Neutrophils >1.0x10 /l
9 9 9
administer
administer
administer
(2) Platelets <100x10 /l or Total WBC < 2.9 x10 /l or Neutrophils < 1.0x10 /l
9 9 9
physician discretion
physician discretion
physician discretion
These guidelines assume that patients are well with good performance status, that other acute toxicities have resolved and the patient has not had a previous episode of neutropenic sepsis.
In some situations chemotherapy is given despite lower blood count values than those noted above. These include patients receiving adjuvant chemotherapy, those with curable metastatic malignancies such as germ cell tumours and lymphomas and also patients with bone marrow infiltration. These situations will be dealt with on a case by case basis.
Capecitabine-Renal function recommendations
Prior to starting treatment: CrCl > 50 full dose
CrCl 30 49 75% dose
CrCl <30
omit
During treatment if there was a rise in serum creatinine the CrCl should be re-calculated and further treatment adjusted according to the above
Issue Date:
30th October 2012
Page 136 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Neutropenic Sepsis Policy
Patients admitted with a fever associated with neutropenia (N < 1x10 /l) are scored according to the presence or absence of risk factors.
9
Age
> 60yrs < 60
=0 =2
Dehydrated requiring iv fluids
No Yes
=3 =0
Hypotensive
Systolic <90 >90
=0 =5
Presence of COPD
Yes No
=0 =4
Symptoms related to infection
None Mild Moderate Severe
=5 =5 =3 =0
Was the patient already in hospital Yes No
=0 =3
Score
17 + = low risk <17= high risk
Low risk: Co-amoxiclav 625mg tds + ciprofloxaxin 750mg bd or
Oral doxycycline 200mg bd + ciprofloxaxin 750mg bd If penicillin allergy or Ceftazidime iv 1g bolus then 2g / 24 hours continuous infusion If unable to take oral medication or already on antibiotics at home or Ceftazidime iv 1g bolus then 2g / 24 hours continuous infusion + vancomycin If evidence of central line infection
Issue Date:
30th October 2012
Page 137 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
High risk: Gentamicin + piperacillin/tazobactam (Tazocin) 4.5g tds
Gentamicin + iv ciprofloxacin 400mg bd if penicillin allergy
Add vancomycin if central line infection suspected
Other pathogens Anaerobic infection suspected: metronidazole 500mgtds
Atypical respiratory infection suspected: Clarithromycin 500mg bd
Platelet Transfusion Policy
Platelets required if:
9
Platelets < 10x10 /l
9
Platelets < 100x10 /l and significant bleeding
Hypocalcaemia
Calcium gluconate 10% 10mls given by slow IV injection tds then orally if needed ECG and calcium monitoring required
Hypomagnesaemia
Patients who present with symptoms suggestive of hypomagnesaemia Patients who have previously had hypomagnesaemia and who are due to have further platinum chemotherapy.
Symptomatic patients with Mg <0.5 or <0.4 regardless of symptoms.
Consider urgent replacement if Mg <0.4 and cardiac history (IHD, AF, AVF).
If normal renal function: 40 mmol in 250 mls Sodium chloride 0.9% over 2 hours.
If suspected abnormal renal function (Cr >125umol/l) or already an inpatient: 40 mmol in 1L Sodium chloride 0.9% over 8 hours.
Give 40 mmol and re-assess symptoms.
Issue Date: 30th October 2012 Page 138 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Re-check Mg if symptoms persist or if indicated for other reasons
Do not give more than 40 mmol in one day.
Ifosfamide Encephalopathy and Methylene Blue
Most mild cases of ifosfamide encephalopathy will spontaneously resolve within 24-72 hours. However, consider use of methylene blue if Grade 3/ Grade 4 neurotoxicity (i.e. somnolence >30% of time, disorientation/ hallucination/ echolalia/ perseveration/ coma, or seizures on which consciousness is altered, or which are prolonged, repetitive or difficult to control).
Methylene Blue 50mg IV every 6 hours.
For future infusions, methylene blue 50 mg prior to infusion of ifosfamide and 50mg every 6 hours during infusion
Ifosfamide Renal Toxicity
Pre-treatment: Serum Na, K, Ca, PO4, Cl, total CO2/HCO3, AP PO4 Creatinine, Osmolarity
Early morning urine
Tp/Creat = PO4 serum PO4 urine x Creat serum umol/l Creat urine
GFR > 60 40-59 < 40
Tp/Creat >1.0 0.8-0.99 <0.8
HCO3 >17.0 14.0-16.9 >14.0
Action Ifosfamide 100% Ifosfamide 70% Switch to cyclophosphamide 1500mg/m2 IV Day 1
Issue Date:
30th October 2012
Page 139 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Folinic acid rescue for High Dose Methotrexate
Time after starting methotrexate Methotrexate Plasma concentration in micromol/L If serum creatinine is greater that 50% of normal limit, double the folinic Acid dose Start folinic acid 15mg/m2 IV every 6 hours, then follow table below < 0.1M 48 hrs Stop rescue 0.5 5M 15mg-30mg 6 hourly 72 hrs Stop rescue 15mg-30mg 6 hourly 96 hrs Stop rescue 15mg-30mg 6 hourly 120 hrs Stop rescue 15mg-30mg 6 hourly 5 50M 200mg/m
2
24 HRS
>50M 1000mg/m 6 hourly 1000mg/m 6 hourly 1000mg/m 6 hourly 1000mg/m 6 hourly
2 2 2 2
6 hourly 200mg/m
2
6 hourly 200mg/m
2
6 hourly 200mg/m 6 hourly
2
CCC Dose Banding Policy
Rationale It is widely recognised that using body surface areas (BSA) is not the most accurate method of calculating chemotherapy doses. Dose banding does not result in a significant dose variation from the traditional method as the maximum variation between the standard dose and the dose comprising each band is 5% or less. A range of pre-filled syringes may be used to administer the dose. This system has worked successfully in Cancer Centres in the UK
1, 2
For all intravenous chemotherapy agents there is a threshold below which it is not possible for pharmacy to guarantee the accuracy of a given dose. This usually corresponds to approximately 5% of a standard dose e.g. 10mg of Docetaxel.
Given that the calculation of chemotherapy doses on the basis of surface area is at best an educated guess, treatment is unlikely to be compromised by rounding the dose to the nearest 5% increment.
Oral agents have to be dose rounded often to a much larger tolerance e.g. Etoposide 10-16%.
Dose banding has been defined as a system whereby, through agreement between prescribers and pharmacists, doses of intravenous cytotoxics calculated on an individual basis, which are within defined
Issue Date: 30th October 2012 Page 140 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0 Author: Dr. D.B. Smith Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
ranges or bands are rounded up or down to predetermined standard doses. The initial step is to decide on the bands and how best to arrive there from the calculated dose. Taking BSA to 2 decimal place and rounding the dose to the nearest 1ml volume (taking concentration into account) appears to be the simplest way forward. All cytotoxic doses are rounded up/down, which allows easier manipulation within pharmacy.
For the following drugs the doses prescribed should be rounded or banded to the indicated pharmacy tolerance level. For drugs not on this list clinicians should round the dose to the nearest figure that approximates to 5% of the total dose.
Drugs dispensed at CCC
Dactinomycin (Actinomycin-D) Doses rounded to nearest 0.1mg dose
6
Aldesleukin (Proleukin) 18 *10 IU /1ml Doses rounded to nearest 1MU (*10 ) dose
6
Alemtuzumab (30mg/1ml Vial) Used for TBI patients at CCC Usual dose 10mg
Bevacizumab (400mg /16ml and 100mg / 4ml) Doses rounded to nearest 25mg dose
Bleomycin (15000 IU Vial) Usual dose either 15,000IU or 30,000IU
Liposomal Doxorubicin (Caelyx) 20mg /10ml Liposomal Doxorubicin 45mg/m2 (Do not dose band trials)
BSA
1.3 -1.49 1.5- 1.69 1.7-1.89 >1.9
60mg 70mg 80mg 90mg
Calcium Folinate 300mg /30ml vial Folinic acid syringes for 5FU/FA regime dispensed as 50mg flat dose DeGramont type regimes dose dispensed at 350mg flat dose
Carboplatin 10mg/ 1ml (60ml Vial) Doses rounded to nearest 50mg dose
Issue Date: 30th October 2012 Page 141 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Cetuximab (100mg /50ml Vial) Doses rounded to nearest 2mg dose
CMF Regimes BSA (m ) < 1.39 1.40 - 1.59 1.60 -1.74 1.75 - 1.84 > 1.85
2
5FU Dose 800mg 900mg 1000mg 1100mg 1200mg
Methotrexate Dose 55mg 60mg 65mg 70mg 80mg
Cyclophosphamide Dose 50mg TDS14/7 50mg TDS 14/7 50mg TDS 14/7 50mg TDS 14/7 50mg QDS 14/7
If Cyclophosphamide 50mg BD 14/7 or 50mg QDS 14/7 required, Dr to specify on script.
Cisplatin (100mg /100ml) Doses rounded to nearest 10mg dose
Cyclophosphamide (1gram Vial) Doses rounded to nearest 20mg dose
Doses >800mg should be rounded to the nearest 100mg dose.
Dacarbazine (1gram Vial) Doses >1000mg should be rounded to the nearest 100mg dose.
Docetaxel (80mg Vial) BSA (m ) 1.40 1.59 1.60 1.79 1.80 2.00 Doxorubicin (200mg / 100ml Vial) Doses should be rounded to nearest 2mg dose
2
Docetaxel Dose (100mg/m ) 150mg 170mg 190mg
Doses > 80mg should be supplied in presentations corresponding to the nearest 10mg
Etoposide (500mg /25ml) Doses rounded to nearest 20mg dose
Etopophos (Etoposide Phosphate) 100mg Vial Doses rounded to nearest 10mg dose
Epirubicin (50mg /25ml Vial) Doses > 80mg should be supplied in presentations corresponding to the nearest 10mg
Issue Date: 30th October 2012 Page 142 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Epirubicin 50mg/m
DOSE (mg) 70 80 90 100
2
1.54 1.69 1.70 1.89 >1.90 Epirubicin 100mg/m
DOSE (mg) 1.31 1.34 1.35 1.44 1.45 1.54 1.55 1.64 1.65 1.74 1.75 1.84 1.85 1.92 >1.93 130 140 150 160 170 180 190 200
Epirubicin and Doxorubicin doses > 80mg should be dose banded to the nearest 10mg dose
Epirubicin and Doxorubicin doses < 80mg should be rounded to nearest 2mg dose
Fluorouracil (500mg / 100ml Vial)
Doses < 1000mg should be rounded to nearest 50mg dose
Fluorouracil doses >1000mg should be rounded to the nearest 100mg dose.
Fluorouracil LV5 Pumps For DeGramont type regimes should be banded as below:
2
2400mg/m
BSA 1.45 1.51 1.52 1.61 1.62 1.71 1.72 1.82 1.83 1.92 >1.93 2800mg/m
2
Dose 3500mg 3750mg 4000mg 4250mg 4500mg 4750mg
BSA 1.45 1.47 1.48 1.56 1.57 1.65 1.66 1.72 1.73 1.86 1.87 2.00
Issue Date:
Dose 4000mg 4250mg 4500mg 4750mg 5000mg 5500mg
30th October 2012 Page 143 of 148 Filename: MCHACPROTO Issue No: Copy No: 10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Fluorouracil doses at 1000mg /m BSA 1.26 1.35 1.36 1.45 1.46 1.55 1.56 1.65 1.66 1.75 1.76 1.85 1.86 1.95 >1.96 Gemcitabine (1gram Vial)
Dose 1300mg 1400mg 1500mg 1600mg 1700mg 1800mg 1900mg 2000mg
Doses dispensed to nearest 38mg dose BSA (m ) 1.40 1.49 1.50 1.69 1.70 1.89 1.90 2.00
2
Gemcitabine Dose (1000 mg/m ) 1400mg 1600mg 1800mg 2000mg
2
BSA (m ) 1.40 1.49 1.50 1.69 1.70 1.89 1.90 2.00 Irinotecan (100mg / 5ml) BSA (m ) 1.40 1.59 1.60 1.79 1.80 2.00
2
Gemcitabine Dose (1250 mg/m ) 1800mg 2000mg 2300mg 2500mg
Irinotecan Dose (180mg/m ) 260mg 300mg 340mg
Ifosfamide (2gram Vial) Doses rounded to nearest 80mg dose
Methotrexate (500mg / 20ml) Doses rounded to nearest 5mg dose
Mesna (1000mg / 10ml) Doses rounded to nearest 100mg dose
Mitomycin (10mg Vial) Doses rounded to nearest 1mg dose
Issue Date:
30th October 2012
Page 144 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Mitoxantrone (20mg /10 ml) Doses rounded to nearest 2mg dose
Oxaliplatin (100mg and 50mg Vial) BSA (m ) 1.40 1.59 1.60 1.79 1.80 2.00
2
Oxaliplatin Dose (85mg/m ) 130mg 150mg 170mg
Paclitaxel (300mg / 50m, 100mg / 16.7ml, 30mg / 5ml) Doses < 230mg rounded to nearest 6mg dose
2
Paclitaxel 175mg/m should be banded to the strengths below: BSA 1.30 1.34 1.35 1.42 1.43 1.46 1.47 1.62 1.63 1.79 1.80 1.94 1.94 2.00 Pemetrexed (500mg / 20ml) Doses rounded to nearest 50mg dose Dose 230mg 240mg 250mg 270mg 300mg 330mg 350mg
Rituximab (100mg and 500mg Vial) Doses rounded to nearest 10mg dose
Topotecan (4mg Vial) Doses rounded to nearest 0.1mg dose
Trastuzumab (150mg Vial) Doses rounded to nearest 21mg dose Treosulfan (1gram and 5 gram Vial) Doses rounded to nearest 100mg dose
Vinblastine (10mg / 10ml Vial) Doses rounded to nearest 1mg dose
Vincristine ( 2mg / 2ml) Doses rounded to nearest 0.1mg dose
Issue Date:
30th October 2012
Page 145 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Vindesine (5mg /5ml) Doses rounded to nearest 1mg dose
Vinorelbine (50mg / 5ml) Doses rounded to nearest 5mg dose as below IV dose 2 25 mg/m Dose (mg) 30 30 35 40 40 45 45 50 Oral dose 2 60 mg/m Dose (mg) 80 80 90 100 100 110 110 120 IV dose 2 30 mg/m Dose (mg) 40 45 50 50 55 55 55 60 Oral dose 2 80 mg/m Dose (mg) 100 110 120 130 140 140 150 160
BSA (m ) 1.25 to 1.34 1.35 to 1.44 1.45 to 1.54 1.55 to 1.64 1.65 to 1.74 1.75 to 1.84 1.85 to 1.94 1.95
Oral Vinorelbine is available in 20mg and 30mg Capsules
25mg IV Vinorelbine = 60mg Oral Vinorelbine dose 30mg IV Vinorelbine = 80mg Oral Vinorelbine dose
The dose of oral Vinorelbine is approx 2.5 times that of IV Vinorelbine
References
1.
Plumridge R, Sewell G. Dose banding of cytotoxic drugs: A new concept in cancer chemotherapy. Am J Health Syst Pharm 2001; 58: 1760 4.
2.
Baker J P, Jones S E. Rationalisation of chemotherapy services at the University Hospital Birmingham NHS Trust. J Oncol Pharm Prac 1998; 4: 10 14.
Issue Date:
30th October 2012
Page 146 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
THE CLATTERBRIDGE CANCER CENTRE NHS FOUNDATION TRUST
Surface Area Nomogram
Issue Date:
30th October 2012
Page 147 of 148
Filename:
MCHACPROTO
Issue No: Copy No:
10.0
Author: Dr. D.B. Smith
Authorised by: Dr. D.B. Smith
You might also like
- Hiponatremia Predicts Length of Hospital Stay in ADHF PatientsDocument4 pagesHiponatremia Predicts Length of Hospital Stay in ADHF PatientsMayang Sri WulandNo ratings yet
- Peresepan OlahragaDocument7 pagesPeresepan OlahragaAngga Julyananda PradanaNo ratings yet
- Deresuscitation ARDSDocument28 pagesDeresuscitation ARDSSudaryadiNo ratings yet
- Anestesi Mimang PDFDocument67 pagesAnestesi Mimang PDFJhoeDjiplakNo ratings yet
- Modul 2 - 3 PDFDocument70 pagesModul 2 - 3 PDFTarmidi MidziNo ratings yet
- Adult Questionnaire Self-CompletionDocument39 pagesAdult Questionnaire Self-CompletionAnnisa Ratna DNo ratings yet
- Kurva Disosiasi HB OksigenDocument6 pagesKurva Disosiasi HB Oksigenhendra_darmawan_4No ratings yet
- Calculator Dosis Obat Support Dan Vasoactive: Masukkan 55Document4 pagesCalculator Dosis Obat Support Dan Vasoactive: Masukkan 55Kaharudin KaharudinNo ratings yet
- Komplikasi Stroke PDFDocument7 pagesKomplikasi Stroke PDFJose Hady PuteraNo ratings yet
- Kardio SoalDocument90 pagesKardio SoalSiti Abdillah MuliadiNo ratings yet
- Askep MCI - AchirmanDocument53 pagesAskep MCI - AchirmanmarthaNo ratings yet
- DapusDocument2 pagesDapusrahmadNo ratings yet
- Pengwas Sitasi VancouverDocument27 pagesPengwas Sitasi VancouverPrameswari ZahraNo ratings yet
- Pelatihan USGDocument53 pagesPelatihan USGEkoWayanNo ratings yet
- Soal Ujian Praktikum Faal Kardio 2021Document2 pagesSoal Ujian Praktikum Faal Kardio 2021Audry RachmaniarsyNo ratings yet
- Burat-Buret Echo Romi Revised PDFDocument2 pagesBurat-Buret Echo Romi Revised PDFAsma.denmiNo ratings yet
- PEDIATRICS VITAL SIGNS CHARTDocument33 pagesPEDIATRICS VITAL SIGNS CHARTMelinda Marianni100% (1)
- Scanned With CamscannerDocument53 pagesScanned With CamscannerdefiNo ratings yet
- REVISI 1st Announcement Book 27th ASMIHA 2018 - 12des2017Document21 pagesREVISI 1st Announcement Book 27th ASMIHA 2018 - 12des2017Jimmy Oi SantosoNo ratings yet
- JURNAL STROKE (Andrew Regar)Document15 pagesJURNAL STROKE (Andrew Regar)drew Regar100% (1)
- Interpreting ABG ResultsDocument28 pagesInterpreting ABG Resultsmafoel39No ratings yet
- ArthritisDocument8 pagesArthritissdorji72No ratings yet
- Lutembacher's Syndrome at KolonodaleDocument7 pagesLutembacher's Syndrome at KolonodaleWayan GunawanNo ratings yet
- SSTi Diabetic PETRI 2019Document36 pagesSSTi Diabetic PETRI 2019intermoska soloNo ratings yet
- Hubungan Kepatuhan Terapi Kelasi Dengan Kadar Feritin Seum Pasien Beta-Talasemia Di RSUP DR M Djamil PadangDocument55 pagesHubungan Kepatuhan Terapi Kelasi Dengan Kadar Feritin Seum Pasien Beta-Talasemia Di RSUP DR M Djamil PadangSilvania Maisya100% (1)
- Tatalaksana Hipertensi EmergensiDocument31 pagesTatalaksana Hipertensi EmergensiSitiMaghfirahHafizNo ratings yet
- Head circumference growth chart for baby girlsDocument1 pageHead circumference growth chart for baby girlsNia Tri Mulyani100% (1)
- Pengaruh Aromaterapi Inhalasi Terhadap Penurunan Nilai Kecemasan Pasien Gagal Ginjal Kronik Yang Menjalani HemodialisaDocument6 pagesPengaruh Aromaterapi Inhalasi Terhadap Penurunan Nilai Kecemasan Pasien Gagal Ginjal Kronik Yang Menjalani HemodialisaevangelineNo ratings yet
- Final 2nd Announcement Konas Perdatin Perdici 2019 - WebsiteDocument65 pagesFinal 2nd Announcement Konas Perdatin Perdici 2019 - Websitetia_drNo ratings yet
- DAFTAR CAIRAN TONISITAS DAN KOMPOSISI UTAMADocument6 pagesDAFTAR CAIRAN TONISITAS DAN KOMPOSISI UTAMAagung permanaNo ratings yet
- Evaluation of causes and initial testing for ascitesDocument16 pagesEvaluation of causes and initial testing for ascitesMaricruz BracamonteNo ratings yet
- Trombosis Vena Dalam: Pendidikan Kedokteran Berkelanjutan (PKB) XXI 2013Document13 pagesTrombosis Vena Dalam: Pendidikan Kedokteran Berkelanjutan (PKB) XXI 2013IkaNo ratings yet
- Pemasangan Dan Interpretasi EKGDocument117 pagesPemasangan Dan Interpretasi EKGaulianadanisya100% (2)
- (F) Chi-Square 3 X 3Document6 pages(F) Chi-Square 3 X 3Rendy FirmansyahNo ratings yet
- Kul Sem 4 Heat Stroke N Fever UHT 2016Document63 pagesKul Sem 4 Heat Stroke N Fever UHT 2016NandaSuryaWijayaNo ratings yet
- Hepatorenal SyndromeDocument6 pagesHepatorenal SyndromeEveline YNo ratings yet
- Clinical Pathways SMF PARU 2016Document12 pagesClinical Pathways SMF PARU 2016Ricky TaufiqurrohmanNo ratings yet
- CASE REPORT: 75-YEAR-OLD WOMAN WITH 25% BODY SURFACE AREA BURNSDocument64 pagesCASE REPORT: 75-YEAR-OLD WOMAN WITH 25% BODY SURFACE AREA BURNSabdul100% (1)
- Aspek Medikolegal Gawat DaruratDocument33 pagesAspek Medikolegal Gawat Daruratlinda rahayu ningsihNo ratings yet
- BGA Acid Base Stepwise PradikDocument43 pagesBGA Acid Base Stepwise PradikZulfadly NuralimNo ratings yet
- PEMBERIAN OBAT VIA SYRINGE PUMPDocument5 pagesPEMBERIAN OBAT VIA SYRINGE PUMPNasRah Nurdin ARNo ratings yet
- NSTEMI Refarat Cardio 2016Document48 pagesNSTEMI Refarat Cardio 2016Anonymous IOkNvM8VbtNo ratings yet
- Makalah Bahasa Inggris (Jantung)Document12 pagesMakalah Bahasa Inggris (Jantung)Nia Mldyni100% (1)
- TN73-2 Electromagnetic Disturbance Troubleshooting HelpDocument6 pagesTN73-2 Electromagnetic Disturbance Troubleshooting HelpCharls GuevaraNo ratings yet
- COMFORT ScaleDocument7 pagesCOMFORT ScaleALDO STEFANUZ (STIK)No ratings yet
- EKG Interpretation Guide by Dr. AritantriDocument64 pagesEKG Interpretation Guide by Dr. Aritantriaandaku100% (1)
- Slamet Hidayat - Peran Perawat Igd Cardiac Arrest Webinar ReadyDocument34 pagesSlamet Hidayat - Peran Perawat Igd Cardiac Arrest Webinar Readynova hapsariNo ratings yet
- Death Case II DizaDocument29 pagesDeath Case II DizaJayarasti KusumanegaraNo ratings yet
- PHB Semester Ganjil 2018 - 2019 XI MIPA - IPSDocument15 pagesPHB Semester Ganjil 2018 - 2019 XI MIPA - IPSkanyaNo ratings yet
- Differential Diagnosis of Microcytic Anemia PDFDocument5 pagesDifferential Diagnosis of Microcytic Anemia PDFayms99No ratings yet
- Dasar-Dasar Radiologi Musculoskeletal - 2Document75 pagesDasar-Dasar Radiologi Musculoskeletal - 2qumanNo ratings yet
- Clinical Pathway Hiperbilirubinemia Rumah Sakit Kelas C: Hari Penyakit Keterangan 1 2 3 4 5 6 7 Hari Rawat 1 2 3 4 5 6 7Document5 pagesClinical Pathway Hiperbilirubinemia Rumah Sakit Kelas C: Hari Penyakit Keterangan 1 2 3 4 5 6 7 Hari Rawat 1 2 3 4 5 6 7Anonymous BiWytIXFjNo ratings yet
- Risiko: Layanan Penunjang LainnyaDocument2 pagesRisiko: Layanan Penunjang Lainnyagode100% (1)
- Gold 2019Document43 pagesGold 2019Hayatillah Natasya100% (1)
- Cardiac Arrhythmias: Abnormal of Cardiac RhythmDocument39 pagesCardiac Arrhythmias: Abnormal of Cardiac Rhythmemoyandhy100% (1)
- Gap Co2 Cocc 2018Document9 pagesGap Co2 Cocc 2018Cesar Rivas CamposNo ratings yet
- Soal MAYO Yg KeluarDocument8 pagesSoal MAYO Yg KeluardoktersaktiNo ratings yet
- Soac 2021 First AnnouncementDocument13 pagesSoac 2021 First AnnouncementHendi PrihatnaNo ratings yet
- Merck Interest AreasDocument40 pagesMerck Interest AreasPhil MurrayNo ratings yet
- Apr 79 ADocument4 pagesApr 79 ADala VWNo ratings yet
- A Review ofDocument9 pagesA Review ofDala VWNo ratings yet
- 1477 7819 7 61Document9 pages1477 7819 7 61Deni Andre AtmadinataNo ratings yet
- PasswordDocument1 pagePasswordDala VWNo ratings yet
- Clinicopathological Profile and Surgical Treatment of Abdominal Tuberculosis: A Single Centre Experience in Northwestern TanzaniaDocument9 pagesClinicopathological Profile and Surgical Treatment of Abdominal Tuberculosis: A Single Centre Experience in Northwestern TanzaniaDala VWNo ratings yet
- Clinicopathological Profile and Surgical Treatment of Abdominal Tuberculosis: A Single Centre Experience in Northwestern TanzaniaDocument9 pagesClinicopathological Profile and Surgical Treatment of Abdominal Tuberculosis: A Single Centre Experience in Northwestern TanzaniaDala VWNo ratings yet
- In Room Dining MenuDocument8 pagesIn Room Dining MenuDala VWNo ratings yet
- Intra Abdominal InfectionDocument13 pagesIntra Abdominal InfectionDala VWNo ratings yet
- 23 02 14Document15 pages23 02 14Dala VWNo ratings yet
- Surgical Treatment of Primary Hyperparathyroidism: Clinical StudyDocument4 pagesSurgical Treatment of Primary Hyperparathyroidism: Clinical StudyDala VWNo ratings yet
- Chemo Stability Chart AtoK 1jun2016Document46 pagesChemo Stability Chart AtoK 1jun2016arfitaaaaNo ratings yet
- BCCA CHOP Protocol for Lymphoma TreatmentDocument3 pagesBCCA CHOP Protocol for Lymphoma TreatmentNararto PrijogoNo ratings yet
- OCN Study GuideDocument10 pagesOCN Study GuideYadile D BenoitNo ratings yet
- MOH BluebookDocument210 pagesMOH BluebookSay LeeNo ratings yet
- Ewing's Sarcoma Case StudyDocument24 pagesEwing's Sarcoma Case StudyMary Justine Nuyad-Africa100% (1)
- PHD222, Oncology Pharmacy (IQHWAN C2)Document8 pagesPHD222, Oncology Pharmacy (IQHWAN C2)Danial IqhwanNo ratings yet
- Biological Properties of Essential OilsDocument20 pagesBiological Properties of Essential OilsDébora MarchesineNo ratings yet
- Acute Leukemia ProtocolDocument13 pagesAcute Leukemia ProtocolBol Dhalbeny MalualNo ratings yet
- 3236249339Document197 pages3236249339Mohamed Abd El-Fattah GalalNo ratings yet
- Breast Cancer ChemotherapyDocument7 pagesBreast Cancer Chemotherapydini kusmaharaniNo ratings yet
- Immunology & Oncology Review 2Document99 pagesImmunology & Oncology Review 2Melchor Felipe SalvosaNo ratings yet
- Stabilis-Monographie-Doxorubicin Hydrochloride Liposome PegDocument9 pagesStabilis-Monographie-Doxorubicin Hydrochloride Liposome PegSepti Marta SariNo ratings yet
- Barabadi 2019 - Emerging Theranostic Biogenic Silver Nanoparticles For Breast Cancer PDFDocument21 pagesBarabadi 2019 - Emerging Theranostic Biogenic Silver Nanoparticles For Breast Cancer PDFayiedNo ratings yet
- ESMO Handbook Oncological Emergencies PDFDocument303 pagesESMO Handbook Oncological Emergencies PDFJuan C. Calderón León100% (5)
- NCM-112-RLE-LEARNING-PACKET-BREAST-CANCER 1st SEM-SY2021-2022Document8 pagesNCM-112-RLE-LEARNING-PACKET-BREAST-CANCER 1st SEM-SY2021-2022Gallannalyn Sanchez100% (1)
- Recent Updates On Nanomedicine Based Products: Current Sce-Nario and Future OpportunitiesDocument13 pagesRecent Updates On Nanomedicine Based Products: Current Sce-Nario and Future OpportunitiesvijuNo ratings yet
- ESCDocument34 pagesESCDIANNo ratings yet
- Consumer Chemistry: Quarter 4 - Module 4: Anticancer DrugsDocument24 pagesConsumer Chemistry: Quarter 4 - Module 4: Anticancer DrugsShekina Joy SungaNo ratings yet
- Advanced Drug Delivery Reviews: Vladimir TorchilinDocument5 pagesAdvanced Drug Delivery Reviews: Vladimir Torchilinvishal makadiaNo ratings yet
- Antibiotic (Bacteriostatic) DrugsDocument15 pagesAntibiotic (Bacteriostatic) DrugsVictor LeeNo ratings yet
- Norton Simon HypothesisDocument2 pagesNorton Simon HypothesissusdoctorNo ratings yet
- Quiz Chapter 28Document23 pagesQuiz Chapter 28Amelie AvenidoNo ratings yet
- Gao 2016Document15 pagesGao 2016kevin gelaudeNo ratings yet
- Seminar Obgyn Chemotheraphy in GynaecologyDocument38 pagesSeminar Obgyn Chemotheraphy in GynaecologyRoshandiep GillNo ratings yet
- Liposomes: A Novel Drug Delivery System: Review ArticleDocument9 pagesLiposomes: A Novel Drug Delivery System: Review ArticleVera WatiNo ratings yet
- Drug Study: Cotrimoxazole: Cotrimoxazole 500mg Tab PO TID X 7 DaysDocument6 pagesDrug Study: Cotrimoxazole: Cotrimoxazole 500mg Tab PO TID X 7 Daysbobo gamingNo ratings yet
- Laboratory and Diagnostic Findings: Small Cell CarcinomaDocument4 pagesLaboratory and Diagnostic Findings: Small Cell CarcinomaTheresa Sombilla FacunlaNo ratings yet
- REVERSING MDR" Reversal of multidrug resistance in vitro and in vivo by 5-N-formylardeemin, a new ardeemin derivativeDocument8 pagesREVERSING MDR" Reversal of multidrug resistance in vitro and in vivo by 5-N-formylardeemin, a new ardeemin derivativeali99No ratings yet
- Growing Portfolio of Complex InjectablesDocument4 pagesGrowing Portfolio of Complex InjectablesTathagata DuttaNo ratings yet
- Medical Management For Cervical CancerDocument8 pagesMedical Management For Cervical CancerMark Anthony MalicseNo ratings yet