Professional Documents
Culture Documents
Spinal Anaesthesia2
Uploaded by
Lee June LyngOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Spinal Anaesthesia2
Uploaded by
Lee June LyngCopyright:
Available Formats
Best Practice & Research Clinical Anaesthesiology Vol. 17, No. 3, pp.
289 303, 2003
doi:10.1016/S1521-6896(02)00114-3, www.elsevier.com/locate/jnlabr/ybean
1 Physiology of spinal anaesthesia and practical suggestions for successful spinal anaesthesia
Francis V. Salinas*
Staff Anaesthesiologist
MD
Lila A. Sueda
MD
Staff Anaesthesiologist
Spencer S. Liu
MD
Clinical Professor of Anaesthesiology and Staff Anaesthesiologist Department of Anaesthesiology, Virginia Mason Medical Center, 1100 Ninth Avenue B2-AN, Seattle, WA 98111, USA
There are numerous physiological effects of spinal anaesthesia. This chapter focuses on the physiological effects that are of clinical relevance to the anaesthesiologist, and provides suggestions for successful management of this simple and popular technique. The mechanisms and clinical signicance of spinal-anaesthesia-induced hypotension, bradycardia and cardiac arrest are reviewed. The increasing popularity of ambulatory spinal anaesthesia requires knowledge that long-acting local anaesthetics, such as bupivacaine, impair the ability to void far longer than short-acting local anaesthetics, such as lidocaine. The importance of thermoregulation during spinal anaesthesia, and the clinical consequences of spinalanaesthesia-induced hypothermia are reviewed. Effects of spinal anaesthesia on ventilatory mechanics are also highlighted. Lastly, the sedative and minimum-alveolar-concentration-sparing effects of spinal anaesthesia are discussed to reinforce the need for the judicious use of sedation in the perioperative setting. Key words: hypotension; bradycardia; asystole; volume kinetics; urinary retention; hypothermia; sedation.
A thorough understanding of the numerous physiological effects of spinal anaesthesia is essential for successful perioperative management of patients undergoing this commonly used anaesthetic technique. The degree to which these physiological effects impact on the surgical patient and lead to adverse outcomes is dependent on patient co-morbidity, surgical operation, clinical setting (inpatient versus ambulatory) and spinal anaesthetic technique. Awareness of, and attention to, the factors that potentially cause these physiological effects to become complications is important to ensure proper patient selection and preparation prior to induction of spinal anaesthesia.
* Corresponding author. Tel. 1-206-223-6980; Fax: 1-206-223-6982. E-mail address: anefvs@vmmc.org (F. V. Salinas). 1521-6896/$ - see front matter Q 2003 Elsevier Ltd. All rights reserved.
290 F. V. Salinas, L. A. Sudea and S. S. Liu
CARDIOVASCULAR PHYSIOLOGY Hypotension and bradycardia are both well-recognized side effects of spinal anaesthesia, although their clinical presentations are usually mild and respond rapidly to treatment.1 However, asystole and cardiac arrest can occur suddenly and may lead to signicant morbidity or even mortality.2 The following section reviews the physiology, associated risk factors and clinical signicance of spinal-anaesthesia-induced hypotension (SIH), bradycardia and asystole/cardiac arrest. A pragmatic approach is then offered for the prevention and treatment of these cardiovascular effects associated with spinal anaesthesia. Hypotension Experimental studies in both animals and humans indicate that reduction in both cardiac output (CO) and systemic vascular resistance (SVR) contributes signicantly to SIH.3,4 Approximately 60 70% of the blood volume is contained within the venous capacitance vessels, which retain minimal vasomotor tone following local-anaesthetic-induced sympathetic denervation.5 The decrease in venous return occurs owing to re-distribution of the central blood volume, primarily to the splanchnic vasculature and, to a lesser extent, the lower extremities.4,6,7 Therefore, vasomotor tone largely determines venous return and consequently CO. In contrast to the venous vasculature, the arterioles retain a signicant degree of vasomotor tone during sympathetic blockade. In young healthy subjects, SVR decreases only moderately (15 18%) even with signicant sympathetic blockade.5 With the cephalad extent of spinal anaesthesia limited to lower or midthoracic levels, lower extremity vasodilatation can be compensated for by upper extremity vasoconstriction. However, with high thoracic levels of spinal anaesthesia, both upper extremity and splanchnic vasoconstriction is abolished and may lead to signicant haemodynamic compromise. It is generally believed that the decrease in SVR is only moderate and that the major determinant of SIH is decreased venous return.5 However, the physiology of SIH in elderly patients is likely to be different from that of younger patients.4,8 In elderly patients (average age 68 72) with T4 T6 sensory levels of spinal anaesthesia, SVR decreased by 23 26%, CVP decreased by 2 3 mmHg, and left ventricular end diastolic volume decreased by 20%. The higher degree of resting sympathetic tone exhibited by elderly patients may explain the exaggerated decrease in SVR to sympathetic blockade compared with younger patients.5,8 Bradycardia and asystole Supraspinal control of heart rate is co-ordinated within the vasomotor centre, located in the oor of the fourth ventricle within the medulla oblongata.9,10 The cardioinhibitory centre has efferent connections mainly to the dorsal nucleus of the vagus, and the cardio-accelerator centre has efferent outow to the thoracic sympathetic bres.9,10 The overall incidence of moderate bradycardia (dened as a heart rate , 50 beats/min) from prospective studies is 8.9 13%, with almost 75% of the episodes of moderate bradycardia occurring when peak sensory block height was $ T5.11 13 Spinal anaesthesia that blocks the sympathetic cardio-accelerator bres from T1 to T5 leaves vagal parasympathetic tone unopposed and will normally result in mild to moderate decreases in heart rate.
Physiology and suggestions for successful spinal anaesthesia 291
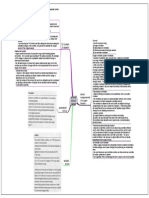
A more signicant effect of the sympathectomy induced by spinal anaesthesia is the potential for a marked decrease in venous return to the heart that, paradoxically, further enhances vagal tone, leading to marked bradycardia and possibly asystole.9,14 The signicant decrease in pre-load that may accompany spinal anaesthesia may initiate the following three reexes that mediate this response that can eventually lead to an abrupt onset of cardiovascular collapse and syncope.9,10,14 The rst reex involves direct stretching of the pacemaker cells in the sinoatrial node. The rate of spontaneous depolarization of these cells is proportional to the degree of stretch. Thus, a decrease in venous return produces less stretch and a lower heart rate. The second reex involves baroreceptors located within the walls of the right atrium and the vena-cava atrial junction. Stimulation of these receptors brought on by an increase in venous return sends afferent signals via the vagus nerve to the vasomotor centre. The efferent pathway is mediated through the cardio-accelerator bres leading to an increase in heart rate. There is no vagal efferent pathway in this reex, and decreases in venous return result in decreased efferent outow to the cardio-accelerator bres, inducing a decrease in heart rate. The third reex is mediated by cardiac baroreceptors located in the inferoposterior wall of the left ventricle. The Bezold Jarisch reex can be viewed as a pathophysiological perturbation of the normal physiological response whereby a decrease in central blood volume results in bradycardia and vasodilatation (instead of the normal physiological compensatory responses of vasoconstriction and tachycardia).15 The Bezold Jarisch reex is initially provoked by a decrease in central blood volume, with resulting decreases in ventricular volume and an increase in ventricular contractility. The increase in contractility and wall tension is sensed as a stretch by the sensory baroreceptors located in the inferoposterior portions of the left ventricle, paradoxically increasing afferent output via the vagus nerve to the vasomotor centre. This, in turn, leads to a combination of a marked increase in vagal efferent activity from the vasomotor centre, leading to varying degrees of bradycardia, and a decrease in efferent sympathetic output to the primary sympathetic neurons in the thoracolumbar spinal cord, thus leading to marked vasodilatation (Figure 1). Other proposed mechanisms for sudden bradycardia include a shift in the cardiac autonomic balance, as evidenced by spectral analysis of heart rate variability, and increases in baroreex activity.16,17 Utilizing continuous assessment of spontaneous baroreex activity as a measure of sympathetic parasympathetic balance, a study of patients undergoing spinal anaesthesia was not able to demonstrate any signicant variable in autonomic balance.17 In three of these patients, severe episodes of unexpected SIH and bradycardia could not be prospectively identied by the parameters used to assess sympathetic parasympathetic balance, reinforcing the clinical observation that sudden episodes of severe SIH and bradycardia are difcult to predict.2,17 Clinical signicance Due to the expected physiological changes associated with spinal anaesthesia, hypotension and bradycardia are relatively common side effects, even if they are not always clinically relevant. The incidence of hypotension and bradycardia will depend on
292 F. V. Salinas, L. A. Sudea and S. S. Liu
Substrate
Situational (haemorrhage, exercise, micturition) Outflow obstruction (aortic stenosis, hypertrophic obstructive cardiomyopathy) Drugs (afterload and pre-load agents, adenosine) Hypovolaemia Upright position Humoral peptides pre-load reduction/hypotension + Sympathetic afferents (adenosine) Baroreceptor afferents (stretch) Thalamus Emotion + Sympathetic activation + Vagal afferents + Vagal efferents (bradycardia) _ Sympathetic efferents (vasodilatation)
Anxiety Pain
Modulators
Common pathways
Hypothalamus
Fright Fear
Mechanoreceptors Chemoreceptors
Medulla Vasomotor
Figure 1. The Bezold Jarisch reex is initially provoked by a decreases in central blood volume, with resulting decreases in ventricular volume and an increase in cardiac contractility. The increase in contractility and wall tension is sensed as a stretch by the sensory baroreceptors, paradoxically increasing afferent output via the vagus nerve to the vasomotor centre. This in turn leads to a marked increase in parasympathetic activity, leading to bradycardia, and an inhibition of efferent sympathetic output, leading to marked vasodilation. Modied with permission from Fenton AM. Annals of Internal Medicine, 2000.10
the criteria used; the criteria used in large prospective studies include a systolic blood pressure below 85 90 mmHg or a decrease from baseline levels of greater than 30% to dene hypotension. A heart rate below 50 beats/min is used to dene bradycardia. The overall incidence of hypotension is reported to be 8.2 33% and the overall incidence of bradycardia is reported to be 9 16%.11 13,18 81% of the episodes of hypotension and 74% of the episodes of bradycardia occur when the peak sensory block height is $ T5.13 Despite the expected moderate decrease in venous return, SVR and mean arterial pressure associated with sensory block level to T4, CO has been shown to decrease minimally, with preservation of left ventricular function.4 Preservation of CO during spinal anaesthesia allows maintenance of oxygen delivery to vital organs such as the brain, as demonstrated by lack of change in jugular venous oxygen saturation.19 Additionally, the sympathetic block and muscle paralysis associated with spinal anaesthesia has been shown to decrease total body oxygen consumption by up to 25% in diabetic patients presenting for vascular surgery.20 Despite the frequency of mild to moderate decreases in blood pressure and heart rate, severe hypotension, bradycardia and asystole are uncommon but not rare. The two largest prospective surveys designed to evaluate the incidence of serious complications during spinal anaesthesia reported a total of 28 cardiac arrests in 42, 521 patients for an overall incidence of 0.07%, with a reported mortality rate of 21% of those patients suffering a cardiac arrest.12,21 This compares with the risk of 0.03% of cardiac
Physiology and suggestions for successful spinal anaesthesia 293
arrest from any cause in patients presenting for non-cardiac surgery.22 When cardiac arrest does occur, serious morbidity and mortality may result. In the largest single prospective study of serious complications related to spinal anaesthesia, cardiac arrest was associated with a 23% mortality rate.21 Risk factors for hypotension and bradycardia In two large prospective studies, the most predictive variable for developing SIH is peak sensory block height at or above T5 [odds ratio (OR) of 3.8].12,13 Other risk factors identied, in order of predictive strength, include age greater than 40 years (OR, 2.5), baseline systolic blood pressure less than 120 mmHg (OR, 2.4), combined spinal/ general anaesthesia (OR, 1.9), spinal puncture at or above the L2 L3 interspace (OR, 1.8) and addition of phenylephrine to the local anaesthetic (OR, 1.6). A recent prospective survey utilizing automated data analysis again conrmed that peak block height at or above T5 (OR, 2.3) is highly predictive for hypotension.18 Additional risk factors identied, in order of predictive strength, were chronic alcohol consumption (OR, 3.1), emergency surgery (OR, 2.8) and a history of hypertension (OR, 2.2). Patients with a history of alcohol abuse are more likely to have SIH based on underlying autonomic dysfunction and a higher basal sympathetic tone.18 Hypertensive patients typically exhibit mild intravascular volume depletion so they are more vulnerable to the re-distribution of the central blood volume to the capacitance vessels. In addition, the arterioles of hypertensive patients possess medial hyperplasia and hypertrophy. Thus, they are capable of greater degrees of vasodilatation for any given level of sympathetic blockade.23 The risk factors for developing moderate bradycardia (heart rate , 50 beats/min), in order of predictive strength, are baseline heart rate of less than 60 beats/min (OR, 4.9), ASA physical status I versus III/IV (OR, 3.5), prolonged PR interval (OR, 3.2), use of beta-blockers (OR, 2.9) and block height T5 or greater (OR, 1.7).12,13 In contrast to the common misconception that bradycardia is related to high sensory block, a sensory block level above T5 is a weak predictor of bradycardia and does not correlate with the severity of bradycardia.13 The presence of one risk factor does not make it certain that a given patient will develop severe bradycardia or asystole. However, when two or more risk factors are present, the risk for severe bradycardia or asystole may signicantly increase.24 Prophylactic volume loading Numerous studies of prophylactic volume loading to prevent SIH have provided inconsistent results, largely due to different denitions of hypotension and different patient populations (surgical, elderly, obstetric), as well as confounding inuences from the concomitant use of prophylactic or rescue vasopressor therapy included in the study design. Administration of crystalloid prior to induction of spinal anaesthesia in earlier studies failed to demonstrate sustained and predictable maintenance of blood pressure. The pharmacokinetics of crystalloid solution explains its poor efcacy as even large volumes of infused crystalloid quickly re-distribute from the intravascular to the extravascular compartment.25 27 Two recent studies compared the efcacy of a largevolume crystalloid infusion [12 ml/kg and 20 ml/kg lactated Ringers (LR) over 20 min] within 20 min prior to induction of spinal anaesthesia with crystalloid infusion at the time of induction of spinal anaesthesia, these studies demonstrated no signicant difference in the incidence of hypotension between the two groups.28,29 However,
294 F. V. Salinas, L. A. Sudea and S. S. Liu
patients who received crystalloid infusion immediately after spinal injection had signicantly higher COs 30 min after the onset of anaesthesia compared with patients who received crystalloid infusion 20 min prior to spinal injection.28 In addition, crystalloid infusion at the time of induction of spinal anaesthesia compared with crystalloid infusion before the induction of spinal anaesthesia, resulted in a signicant reduction in the incidence of cardiovascular side effects (dened as nausea, vomiting and faintness) from 9.2 to 2.3%.29 Thus, a more rational approach to crystalloid administration based on pharmacokinetic analysis may indeed provide more consistent results in preventing adverse haemodynamic sequelae to spinal anaesthesia. In contrast to crystalloid solutions, prophylactic volume loading with colloid solutions (500 1000 ml) prior to spinal injection has consistently maintained blood pressure and volume expansion in both surgical and obstetric patients.27,30 32 Colloid infusion results in a sustained increase of intravascular volume due to slower redistribution from the intravascular to the extravascular compartment.26,27 In contrast to prophylactic volume loading with either crystalloid or colloid, treatment of hypotension during spinal anaesthesia will be more effective because of changes in pharmacokinetics induced by spinal anaesthesia or intravascular hypovolaemia.33 35 Either absolute hypovolaemia (from uid losses) or central hypovolaemia (induced by spinal anaesthesia) alter volume kinetics to allow enhanced retention of infused uids within the intravascular space. Given the lack of consistent evidence to support the use of prophylactic crystalloid loading prior to spinal anesthesia, it appears more prudent to infuse crystalloid infusion either at the time of induction of spinal anaesthetic or to treat hypotension with rapid infusions. The improved efcacy of colloid therapy must be weighed against its increased cost and small but signicant risk of anaphylaxis. Additionally, there is little evidence that prophylactic volume loading improves either maternal or fetal outcome, as long as clinically signicant hypotension is recognized early and treated appropriately.30 Prophylactic vasopressors As with prophylactic volume loading, studies of prophylactic vasopressors are difcult to interpret owing to different denitions of hypotension, different patient populations and different study designs. A recent meta-analysis concluded that prophylactic ephedrine is more effective than placebo for preventing SIH for Caesarean section, but that clinically relevant positive effects on neonatal outcome were not demonstrated.36 In addition, the use of ephedrine has traditionally been advocated as the drug of choice for either prevention or management of SIH for the parturient due to concerns about the potential adverse effects of pure a agonists (such as phenylephrine or metaraminol) on uterine blood ow. However, a recent meta-analysis did not nd any clinically signicant differences between phenylephrine and ephedrine in either maternal or neonatal outcome when used for the management of SIH.36 Treatment of hypotension The treatment of SIH should be directed towards the underlying mechanisms of decreased venous return, SVR and CO. The haemodynamic effects of spinal anaesthesia may be signicantly enhanced in the presence of hypovolaemia. Thus, the correction of hypovolaemia prior to induction of spinal anaesthesia is mandatory. The use of either crystalloid or colloid, as well as appropriate patient positioning, appear to be effective in
Physiology and suggestions for successful spinal anaesthesia 295
attenuating and treating SIH.26 29 Experimental studies have demonstrated that optimal pharmacological correction of the circulatory effects of spinal anaesthesia is achieved by utilizing ephedrine.2 Ephedrine is also preferable in patients with hypotension and mild to moderate bradycardia, and may be administered intravenously in 5 10 mg boluses or as a continuous infusion (50 mg/250 1000 ml crystalloid) titrated to desired effect. Phenylephrine is a directly acting selective a1-adrenergic agonist (with weak b-adrenergic effects at clinically used concentrations) that results in vasoconstriction at the level of the arterioles. Intravenous administration of phenylephrine results in dose-dependent increases in systolic, diastolic and mean arterial pressures that are accompanied by decreases in heart rate and CO. Decreases in CO may reect increased arteriolar resistance but are more likely due to baroreceptor-mediated reex bradycardia in response to an increase in diastolic blood pressures.37,38 Thus, phenylephrine is best suited for the hypotensive, tachycardic patient in whom the potential chronotropic effects of ephedrine are not desired. Epinephrine, when given in low doses (0.05 mg/kg/min), has been shown to restore baseline systolic blood pressure and increase heart rate, stroke volume and CO in the setting of hypotension from sympathetic blockade.39 At these low doses, diastolic blood pressure is not restored and probably reects b2-mediated peripheral vasodilatation.39 Bolus doses of adrenaline (epinephrine) (5 20 mg) should be used for hypotension unresponsive to either ephedrine or phenylephrine, especially in the setting of severe bradycardia.2,24 Treatment of bradycardia and asystole Moderate bradycardia may be treated with either intravenous atropine (0.4 1.0 mg) or intravenous ephedrine (5 20 mg). In the case of severe bradycardia, particularly if unresponsive to either ephedrine or atropine or in the setting of a precipitous decrease in heart rate, epinephrine (5 20 mg) should be administered and may require higher doses (0.2 0.3 mg) to achieve an appropriate response. For cardiac arrest, full resuscitation doses of intravenous epinephrine (1 mg intravenous bolus) should be promptly administered to increase coronary and cerebral perfusion pressure.40
SPINAL ANAESTHESIA AND BLADDER FUNCTION The act of micturition is co-ordinated by the opposing functions of the urinary bladder and the urethra. The bladder possesses the dual function of storing and eliminating urine, and involves the co-ordinated actions within the central nervous, somatic and autonomic nervous systems. The detrusor muscle, composed primarily of smooth muscle, is largely responsible for actions of urine storage and micturition. The smooth muscle of the internal urethral sphincter, the urethra, and the striated muscle of the external urethral sphincter also serve the dual function of remaining closed during collection of urine to maintain continence and opening during micturition to allow a conduit for the urinary stream.41 The second, third and fourth sacral spinal nerves (S2 S4) contain the afferent and efferent pathways responsible for control of the bladder and urethral sphincters. Distention of the bladder sends afferent signals (via the pelvic nerve to the sacral segments of the spinal cord) that are transmitted to the frontal lobe. Voluntary micturition is initiated by efferent impulses from the higher cortical centres to the pontine micturition centre, which then activate pre-ganglionic motor neurones
296 F. V. Salinas, L. A. Sudea and S. S. Liu
in the sacral (S2 S4) spinal cord that initiate contraction of the detrusor muscle. Concomitantly, supraspinal efferent impulses temporarily inhibit sympathetic impulses, which promote opening of the internal urethral sphincter and external urethral sphincter, and an increase in detrusor tone, to allow micturition.41,42 After the induction of spinal anaesthesia, the urge to void (normal detrusor function) is abolished within 60 s.42,43 Recovery of the ability to void normally does not return until sensory anaesthesia has regressed to the S3 sacral segment.42 Prolonged inhibition of normal detrusor function with the use of long-acting local anaesthetics, such as bupivacaine, may allow bladder over-distension and urinary retention. In a study of healthy male patients undergoing non-urological surgery after spinal anaesthesia comparing 100 mg lidocaine with 10 mg bupivacaine, the time to return of normal detrusor function (dened as return of urge to void at cystometric capacity together with the ability to empty the bladder completely without abdominal straining) after spinal injection was signicantly longer in the bupivacaine group (233 ^ 31 versus 462 ^ 61 min).42 The cystometric capacity (the bladder volume at which patients feel an urge to void prior to spinal anaesthesia) in this study was between 500 and 600 ml for both groups. The patients in the bupivacaine group generated an average of 875 ml urine by the time they regained normal detrusor function (462 min), far exceeding the cystometric capacity. In contrast, the patients in the lidocaine group had generated an average of 498 ml urine by the time they regained normal detrusor function (233 min). Thus, the use of long-acting local anaesthetics may lead to bladder overdistention before normal bladder function resumes and may result in acute postoperative urinary retention. Postoperative urinary retention can have signicant immediate and long-term consequences. Painful overdistension of the bladder can lead to hypertension, but may also cause hypotension and bradycardia. Overdistension of the bladder can potentially result in permanent, irreversible damage to the detrusor, leading to incomplete emptying of the bladder and an increased long-term risk of urinary tract infections.44 In treating spinal anaesthesia-induced hypotension, patients may potentially be administered large volumes of intravenous uids, possibly increasing the risk of urinary retention.14,42 Due to this potential complication, it has been customary to insert bladder catheters in patients undergoing prolonged spinal anaesthesia. This concern is especially important in the ambulatory setting, where the traditional requirement to void after spinal anaesthesia often leads to prolonged delays in discharge.45 However, the use of short-acting local anaesthetics for ambulatory spinal anaesthesia has not been associated with urinary retention.46 A recent study of ambulatory surgery patients (considered at low risk of urinary retention) discharged prior to voiding after shortacting spinal anaesthesia demonstrated signicantly shorter discharge times with no reports of urinary retention.47 Thus, the risk of urinary retention appears to be low after short-acting spinal anaesthesia, and further prospective study is needed to conrm this practice (discharging low-risk patients prior to voiding after short-acting spinal anaesthesia) in a large population.
THERMOREGULATION Mild perioperative hypothermia is a frequent complication of anaesthesia and surgery because of impaired thermoregulation as well as exposure to a cool environment. While the risk of hypothermia is greater with general anaesthesia, the risk of hypothermia increases with larger cases performed under spinal anaesthesia and can
Physiology and suggestions for successful spinal anaesthesia 297
approach the same magnitude as with general anaesthesia.48 This hypothermia is of no small consequence. Perioperative hypothermia has been shown to affect adversely the incidence of myocardial ischaemia, cardiac morbidity49, wound infection50, surgical bleeding51 and patient discomfort.52,53 However, a recent survey of American Society of Anesthesiologists members revealed that only 33% of anaesthesiologists routinely monitored temperature during regional anaesthesia.54 Reasons for this lack of routine temperature monitoring include the belief that regional anaesthesia is not associated with thermoregulatory abnormalities, lack of a convenient site for temperature monitoring, and the absence of associated malignant hyperthermia with spinal anaesthesia. Additionally, it has been shown that anaesthesiologists are unable to estimate the patients thermal status reliably.55 Due to the lack of temperature monitoring, inability to estimate the patients thermal status reliably, and often a lack of perception by the patient of hypothermia, intraoperative hypothermia goes unrecognized and untreated. Core hypothermia with spinal anaesthesia develops primarily from a re-distribution of heat from core tissues, which are well-perfused tissues such as the head and trunk, to the peripheral tissues, or arms and legs.56,57 This re-distribution of heat is a direct result of the vasodilatation that occurs as a result of the accompanying sympathetic blockade with spinal anaesthesia. This inhibition of tonic vasoconstriction results in a decrease in the core temperature and a proportionate increase in the peripheral tissue temperature.56,57 During the rst hour of anaesthesia, core temperatures have been shown to decrease 0.8 ^ 0.3 8C, with re-distribution contributing 89% to the decrease.58 This is the most important cause of core hypothermia during the rst hour of anaesthesia and remains important even after 3 h of surgery.58 Subsequent hypothermia occurs slowly at a rate linear to heat loss and heat production, in which heat loss exceeds the metabolic production of heat.56,57 Therefore, progressive hypothermia can occur in patients undergoing large operations under spinal anaesthesia as the sympathetic block persists, preventing vasoconstriction and shivering, unlike general anaesthesia in which an active core temperature plateau develops. Vasoconstriction and shivering in unblocked regions (i.e. arms) are triggered by core hypothermia; however, these thermoregulatory responses are largely ineffective56 and are inuenced by age59, sedative medications60, and height of the block, with extensive spinal block impairing thermoregulatory control more than less extensive blocks.61 Spinal anaesthesia has been shown to decrease the thresholds for vasoconstriction and shivering signicantly (i.e. approximately 0.5 8C).62 As mentioned previously, perioperative hypothermia is associated with adverse clinical outcomes; therefore the identication of risks factors for the development of hypothermia during spinal anaesthesia is important. As with general anaesthesia, advanced age is a predictor of hypothermia with spinal anaesthesia. High levels of spinal blockade (i.e. peak sensory block height $ T8) have also been shown to be predictive of hypothermia as vasomotor tone and shivering is inhibited below the level of spinal blockade.63 A recent survey-based study prioritized risk factors for the development of intraoperative hypothermia. They include age , 1 month, low ambient operating-room temperature, second- or third-degree burns, general anaesthesia combined with spinal anaesthesia, age . 70 years, low patient temperature before induction, thin body habitus, and large blood loss, in that order.64 While this study has its limitations, it does suggest risk factors that can be further evaluated in clinical trials. Therefore, to minimize the risk of intraoperative hypothermia during spinal anaesthesia, the following strategies are recommended. First, core temperature should be monitored. Acceptable monitoring sites during spinal anaesthesia include
298 F. V. Salinas, L. A. Sudea and S. S. Liu
the tympanic membrane, axilla, mouth or forehead skin surface. Second, active warming with forced air warmers should be used if core hypothermia occursor its prophylactic use considered in extended operations or high-risk patients. Third, intravenous uids should be warmed to approximately 37 8C if large volumes are to be administered. Fourth, ambient operating room temperature should be greater than 25 8C. Fifth, skin should be covered to decrease cutaneous heat loss.56 Lastly, excessive spinal block height should be avoided when possible.63 This may be accomplished by careful attention to the total dose administered or by utilizing the effect of local anaesthetic baricity and patient positioning to achieve a unilateral block. However, the effect of unilateral block on the degree of intraoperative hypothermia has not been studied.
PULMONARY EFFECTS Clinically signicant alterations in respiratory function are minimal, and most studies show that mid-thoracic levels of spinal anaesthesia produce either small or no changes in respiratory function.65 In 1991, Steinbrook and Concepcion66 demonstrated no change in minute ventilation, tidal volume, respiratory rate or mean inspiratory ow rate with high- to mid-thoracic blocks with spinal anaesthesia. Spinal anaesthesia has been associated with little, if any, change in respiratory rate and tidal volumeeven with a high level of blockadewhereas vital capacity decreases slightly.67,68 This preservation of inspiratory muscle function is logical as the cervical plexus innervates the diaphragm, the primary muscle of ventilation, thereby preserving its function even with a high thoracic block. On the other hand, active expiratory muscle function is decreased in proportion to the level of spinal anaesthesia, demonstrated by reductions in maximal expiratory pressure and ow rates. An 11% decrease in peak expiratory ow with an anaesthetic level at T8 versus a 17% reduction when the anaesthetic level was at T4 has been reported previously.69 This results from the paralysis of abdominal muscles necessary for forced exhalation. As active expiratory efforts are necessary for effective cough, the ability to clear secretions may be impaired after spinal anaesthesia.70 Healthy patients tolerate these effects; however, they mayin theoryhave deleterious effects in patients with severe chronic obstructive pulmonary disease (COPD). Older studies demonstrated that patients with chronic lung disease usually tolerated the altered respiratory mechanics associated with spinal anaesthesia without change in vital capacity while FEV1 increased (probably due to improved diaphragmatic contraction).71 Studies have shown that spinal anaesthesia in the absence of sedation has little effect on pulmonary gas exchange.70 Most authors have demonstrated no signicant changes in minute ventilation, dead-space ventilation, arterial oxygen or carbon dioxide tensions after spinal anaesthesia.69 When hypoxaemia occurs during spinal anaesthesia, it usually results from the effects of sedative drugs. However, it is important to remember that the intrathecal administration of opioids can cause respiratory depression and subsequent alterations in pulmonary gas exchange. Monitoring ventilatory status, pulse oximetry, and careful sedation during spinal anaesthesia and into the postoperative period are warranted, especially in the presence of intrathecal opioids. Control of breathing during spinal anaesthesia is not altered signicantly, although earlier studies demonstrated a small decrease in resting end-tidal PCO2.70 While hyperventilation due to anxiety may cause lowering of the PCO2, it has been speculated that the hypocapnia results from a lack of proprioceptive input from the abdomen and
Physiology and suggestions for successful spinal anaesthesia 299
chest wall during spinal anaesthesia, thereby resulting in an increased drive to breathe.70 It has been reported that spinal anaesthesia with bupivacaine in unpremedicated patients increased ventilatory responsiveness to CO2.72 The rare respiratory arrest after spinal anaesthesia is thought to result from brainstem hypoperfusion secondary to decreased CO rather than from the direct effects of local anaesthetics on the brainstem as the concentration of local anaesthetic in the ventricular uid is not high enough to result in medullary depression.
CENTRAL NERVOUS SYSTEM EFFECTS OF SPINAL ANAESTHESIA While high levels of spinal anaesthesia have been associated with decreased levels of consciousness, this was presumably the result of hypotension and a subsequent decrease in cerebral blood ow rather than the direct effects of local anaesthetics.73 Since then, this view has been challenged, and studies have looked at whether or not spinal anaesthesia may have direct effects on consciousness. Spinal anaesthesia with bupivacaine has been shown to decrease the hypnotic requirements of midazolam and thiopental.74 Increased sensitivity to the sedating effects of midazolam has been reported with spinal anaesthesia in unpremedicated patients, the degree of sedation corresponding to level of sensory block.75,76 While the exact mechanism for this marked sensitivity is unknown, several theories have been postulated for this effect. The rst is a de-afferentation phenomenon in which decreased cerebral arousal is thought to result from decreased afferent input from the spinal cord rendering the reticular activating system more susceptible to the sedative actions of drugs.77 Other possible explanations include the rostral spread of local anaesthetic within the cerebrospinal uid, and increased systemic levels of local anaesthetics.76 Recently Pollock et al78 reported that spinal anaesthesia is accompanied by signicant sedation when compared with controls. However, unlike earlier studies, this effect was unrelated to block height, and interestingly, the sedative effects appeared to be most pronounced at 60 min, possibly favouring direct rostral spread of local anaesthetics to the central nervous system with direct action on the brain, or re-distribution of blood ow and increasing cerebral concentrations of local anaesthetics. These theories are speculative and have not been proven in human models. While the mechanism of sedation with spinal anaesthesia is speculative, the ndings of the aforementioned studies have clinical signicance. Sedative drugs should be administered cautiously in patients with central neuraxial anaesthesia, and it should be remembered that central neuraxial anaesthesia has minimum alveolar concentration (MAC)-sparing properties when combined with general anaesthesia. After spinal anaesthesia, high-risk patients with compromised cardiopulmonary or central nervous
Practice points the main mechanisms for SIH are a re-distribution of the central blood volume to the splanchnic and lower extremity venous capacitance vessels, and mild to moderate decreases in SVR although sympathetic denervation of the cardio-accelerator bres will lead to mild to moderate bradycardia, the decrease in venous return may play a more
300 F. V. Salinas, L. A. Sudea and S. S. Liu
prominent role (presumably via the Bezold Jarisch reex) in the aetiology of asystole/cardiac arrest there are factors that may place patients at higher risk for bradycardia, but it is difcult prospectively to identify patients at risk for asystole/cardiac arrest knowledge of the volume kinetics of crystalloid and colloid should provide a more rational choice of intravenous uid therapy for treating SIH severe bradycardia/asystole unresponsive to either intravenous ephedrine and/or atropine should be treated early and aggressively with intravenous adrenaline (epinephrine) and volume loading, perhaps favouring colloid solutions over crystalloid solutions the use of long-acting local anaesthetics for spinal anaesthesia is associated with a prolonged recovery in the ability to void normally and may potentially lead to bladder overdistention and postoperative urinary retention failure to recognize impaired thermoregulation during spinal anaesthesia can lead to signicant clinical consequences core temperature should be monitored during spinal anaesthesia (preferably at the tympanic membrane or axilla) and forced air warmers should be instituted prophylactically to minimize heat loss in select clinical situations (high-risk patients and extended operations, i.e. greater than 2 h duration) spinal anaesthesia has minimal clinically relevant effects on ventilatory mechanics, and in the absence of sedation, it has little effect on pulmonary gas exchange spinal anaesthesia has been demonstrated to decrease both intravenous sedative/hypnotic requirements and the MAC of inhalation anaesthetics, suggesting that sedative drugs should be administered cautiously during the perioperative period
Research agenda additional studies of the efcacy of intravenous uid therapy guided by volume kinetics to treat and prevent SIH improved prospective identication of patients at high risk for asystole during spinal anaesthesia a large prospective study to validate the practice of discharging low-risk ambulatory surgery patients prior to voiding
system function may require monitoring for up to 60 min after the initial injection of local anaesthetic. SUMMARY This chapter reviewed the clinically relevant physiological effects of spinal anaesthesia on the major organ systems. Knowledge of mechanisms, clinical relevance, risk factors and treatment strategies for some of the more common side effects of spinal anaesthesia should provide a framework for instituting a rational perioperative plan for conducting a successful spinal anaesthetic.
Physiology and suggestions for successful spinal anaesthesia 301
REFERENCES
1. McCrae AF & Wildsmith JA. Prevention and treatment of hypotension during central neural block. British Journal of Anaesthesia 1993; 70: 672680. * 2. Caplan RA, Ward RJ, Posner K & Cheney FW. Unexpected cardiac arrest during spinal anesthesia: a closed claims analysis of predisposing risk factors. Anesthesiology 1988; 68: 126133. 3. Butterworth JF, Piccione W, Berrizbeitia LD et al. Augmentation of venous return by adrenergic agonists during spinal anesthesia. Anesthesia and Analgesia 1986; 65: 612616. 4. Rooke GA, Freun PR & Jacobson AF. Hemodynamic response and change in organ blood volume during spinal anesthesia in elderly men with cardiac disease. Anesthesia and Analgesia 1997; 85: 99105. 5. Bridenbaugh PO, Greene NM & Brull SJ. Spinal (subarachnoid) neural blockade. In Cousins MJ & Bridenbaugh PO (eds) Neural Blockade in Clinical Anesthesia and Management of Pain, 3rd edn. Philadelphia: Lippincott-Raven, 1998, pp 221 226. 6. Arndt JO, Hock A, Stanton-Hicks M & Stuehmeier KD. Peridural anesthesia and the distribution of blood in supine humans. Anesthesiology 1985; 63: 616623. 7. Hogan QA. Venous capacitance changes in the lower extremities during spinal anesthesia. Regional Anesthesia 1996; 21: 376. 8. Critchley LAH, Stuart JC, Short TG & Gin T. Haemodynamic effects of subarachnoid block in elderly patients. British Journal of Anaesthesia 1994; 73: 464 470. 9. Evans RG, Ventura S, Dampney RAL & Ludbrook J. Neural mechanisms in the cardiovascular responses to acute central hypovolaemia. Clinical and Experimental Pharmacology and Physiology 2001; 28: 479 487. 10. Fenton AM, Hammill SC, Rea RF et al. Vasovagal syncope. Annals of Internal Medicine 2000; 133: 714725. 11. Tarkkila PJ & Isola J. A regression model for identifying patients at high risk of hypotension, bradycardia, and nausea during spinal anesthesia. Acta Anaesthesiologica Scandinavica 1992; 36: 554 558. 12. Tarkkila PJ & Kaukinen S. Complications during spinal anesthesia. Regional Anesthesia 1991; 16: 101 106. * 13. Carpenter RL, Caplan RA, Brown DL et al. Incidence and risk factors for side effects of spinal anesthesia. Anesthesiology 1992; 76: 916 922. 14. Stienstra R. Mechanisms behind and treatment of sudden, unexpected circulatory collapse during central neuraxis blockade. Acta Anaesthesiologica Scandinavica 2000; 44: 965 971. 15. Kinsella SM & Tuckey JP. Perioperative bradycardia and asystole: relationship to vasovagal syncope and the BezoldJarisch reex. British Journal of Anaesthesia 2001; 86: 859 868. 16. Critchley LA, Chan S & Tam YH. Spectral analysis of sudden bradycardia during intrathecal meperidine anesthesia. Regional Anesthesia and Pain Medicine 1998; 23: 506510. 17. Gratador P, Viale JP, Parlow J et al. Sympathovagal effects of spinal anesthesia assessed by the spontaneous cardiac baroreex. Anesthesiology 1997; 87: 13591367. * 18. Hartmann B, Junger A, Klasen J et al. The incidence and risk factors for hypotension after spinal anesthesia induction: an analysis with automated data collection. Anesthesia and Analgesia 2002; 94: 15211529. 19. Atallah MM, Hoeft A, El-Ghorouri MA et al. Does spinal anesthesia affect cerebral oxygenation during transurethral prostatectomy? Regional Anesthesia and Pain Medicine 1998; 23: 119 125. 20. Stanley GD, Pierce ET, Moore WJ et al. Spinal anesthesia reduces oxygen consumption in diabetic patients prior to peripheral vascular surgery. Regional Anesthesia 1997; 22: 5358. 21. Auroy Y, Narchi P, Messiah A et al. Serious complications related to regional anesthesia. Anesthesiology 1997; 87: 479 486. 22. Chopra V, Bovill JG & Spierdijk J. Accidents, near accidents and complications during anaesthesia: a retrospective analysis of a 10-year period in a teaching hospital. Anaesthesia 1990; 45: 36. 23. Racle JP, Poy JY, Haberer JP & Benkhadra A. A comparison of cardiovascular responses of normotensive and hypertensive elderly patients following bupivacaine spinal anesthesia. Regional Anesthesia 1989; 14: 6671. 24. Pollard JB. Cardiac arrest during spinal anesthesia: common mechanisms and strategies for prevention. Anesthesia and Analgesia 2001; 92: 252256. * 25. Svensen C & Hahn RG. Volume kinetics of ringer solution, dextran 70, and hypertonic saline in male volunteers. Anesthesiology 1997; 87: 204212. 26. Ueyama H, He YL, Tanigamia H et al. Effects of crystalloid and colloid preload on blood volume in the parturient undergoing spinal anesthesia for elective cesarean section. Anesthesiology 1999; 91: 1571 1576. 27. Kamenik M & Paver-Erzen V. The effects of lactated ringers solution on cardiac output changes after spinal anesthesia. Anesthesia and Analgesia 2001; 92: 71 714. 28. Mojica JL, Melendez HJ & Bautista LE. The timing of intravenous crystalloid administration and incidence of cardiovascular side effects during spinal anesthesia; the results from a randomized controlled trial. Anesthesia and Analgesia 2002; 94: 432437.
302 F. V. Salinas, L. A. Sudea and S. S. Liu 29. Morgan PJ, Halpern SH & Tarshis J. The effects of an increase in central blood volume before spinal anesthesia for cesarean delivery: a qualitative systematic review. Anesthesia and Analgesia 2001; 92: 9971005. 30. Sharma SK, Gajraj NM & Sidawi ES. Prevention of hypotension during spinal anesthesia: a comparison of intravascular administration of hetastarch versus lactated ringers solution. Anesthesia and Analgesia 1997; 84: 111114. 31. Marhofer P, Faryniak B, Oismuller C et al. Cardiovascular effects of 6% hetastarch and lactated ringers solution during spinal anesthesia. Regional Anesthesia and Pain Medicine 1999; 24: 399 404. * 32. Ewaldsson CA & Hahn RG. Volume kinetics of ringers solution during induction of spinal and general anaesthesia. British Journal of Anaesthesia 2001; 87: 406414. 33. Drobin D & Hahn RG. Volume kinetics of ringers solution in hypovolemic volunteers. Anesthesiology 1999; 90: 8191. 34. Hahn RG & Resby M. Volume kinetics of ringers solution and dextran 3% during induction of spinal anaesthesia for cesarean section. Canadian Journal of Anaesthesia 1998; 45: 443 451. 35. Lee A, Ngan Kee WD & Gin T. Prophylactic ephedrine prevents hypotension during spinal anaesthesia for cesarean delivery but does not improve neonatal outcome: a quantitative systematic review. Canadian Journal of Anaesthesia 2002; 49: 588 599. * 36 Lee A, Ngan Kee WD & Gin T. A quantitative, systematic review of randomized controlled trials of ephedrine versus phenylephrine for the management of hypotension during spinal anesthesia for cesarean delivery. Anesthesia and Analgesia 2002; 94: 920926. 37. Morgan P. The role of vasopressors in the management of hypotension induced by spinal and epidural anaesthesia. Canadian Journal of Anaesthesia 1994; 41: 404413. 38. Stoelting RK. Sympathomimetics. In Stoelting RK (ed.) Pharmacology and Physiology in Anesthetic Practice, 3rd edn. Philadelphia: Lippincott-Raven, 1999, pp 272273. 39. Brooker RF, Butterworth JF, Kitzman DW et al. Treatment of hypotension after hyperbaric tetracaine spinal anaesthesia. A randomized, double-blind, cross-over comparison of phenylephrine and epinephrine. Anesthesiology 1997; 86: 797805. 40. Rosenberg JM, Wahr JA, Sung CH et al. Coronary perfusion pressure during cardiopulmonary resuscitation after spinal anesthesia in dogs. Anesthesia and Analgesia 1996; 82: 8487. 41. Elbadawi A. Functional anatomy of the organs of micturation. Urologic Clinics of North America 1996; 23: 177210. * 42. Kamphius ET, Ionescu TI, Kuipers PWG et al. Recovery of storage and emptying functions of the urinary bladder after spinal anesthesia with lidocaine and with bupivacaine in men. Anesthesiology 1998; 88: 310 316. 43. Axelsson K, Mollefors K, Olsson JO et al. Bladder function in spinal anaesthesia. Acta Anaesthesiologica Scandinavica 1985; 29: 315321. 44. Hinman F. Postoperative overdistension of the bladder. Surgery, Gynecology, and Obstetrics 1976; 142: 901902. 45. Pavlin DJ, Rapp SE, Polissar NL et al. Factors affecting discharge time in adult outpatients. Anesthesia and Analgesia 1998; 87: 816 826. 46. Mulroy MF, Larkin KL, Hodgson PH et al. A comparison of spinal, epidural, and general anesthesia for outpatient knee arthroscopy. Anesthesia and Analgesia 2000; 91: 860 864. 47. Mulroy MF, Salinas FV, Larkin KL & Polissar NL. Ambulatory surgery patients may be discharged before voiding after short-acting spinal and epidural anesthesia. Anesthesiology 2002; 97: 315 319. 48. Frank SM, Shi RY, Raja SN et al. Core hypothermia and skin-surface temperature gradients: epidural vs general anesthesia and the effects of age. Anesthesiology 1994; 80: 502508. 49. Frank SM, Fleisher LA, Breslow MJ et al. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events; a randomized trial. Journal of the American Medical Association 1977; 87: 11271134. 50. Kurz A, Sessler DI & Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization: study of wound infection and temperature group. New England Journal of Medicine 1996; 334: 12091215. 51. Winkler M, Akca O, Birkenberg B et al. Aggressive warming reduces blood loss during hip arthroplasty. Anesthesia and Analgesia 2000; 91: 978984. 52. Macario A, Weinger MS, Carney S et al. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesthesia and Analgesia 1999; 89: 652 658. 53. Macario A, Weinger M, Truong P et al. Which clinical anesthesia outcomes are both common and important to avoid? The perspective of a panel of expert anesthesiologists. Anesthesia and Analgesia 1999; 88: 10851091. 54. Frank SM, Nguyen JM, Garcia CM & Barnes RA. Temperature monitoring practices during regional anesthesia. Anesthesia Analgesia 1999; 88: 373377.
Physiology and suggestions for successful spinal anaesthesia 303 55. Arkilic CF, Akca O, Taguchi A et al. Temperature monitoring and management during neuraxial anesthesia: an observational study. Anesthesia and Analgesia 2000; 91: 662666. 56. Sessler DI. Mild perioperative hypothermia. New England Journal of Medicine 1997; 336: 17301737. 57. Sessler DI. Perioperative heat balance. Anesthesiology 2000; 92: 578596. 58. Matsukawa T, Sessler DI, Christensen R et al. Heat ow and distribution during epidural anesthesia. Anesthesiology 1995; 83: 961967. 59. Vassilieff N, Rosencher N, Sessler DI et al. Shivering threshold during spinal anesthesia is reduced in elderly patients. Anesthesiology 1995; 83: 11621166. 60. Matsukawa T, Kurz A, Sessler DI et al. Propofol linearly reduces the vasoconstriction and shivering thresholds. Anesthesiology 1995; 82: 11691180. 61. Leslie K & Sessler DI. Reduction in shivering threshold is proportional to spinal block height. Anesthesiology 1996; 84: 13271331. * 62. Kurz A, Sessler DI, Schroeder M & Kurz M. Thermoregulatory response thresholds during spinal anesthesia. Anesthesia and Analgesia 1993; 77: 721726. * 63. Frank SM, El-Rahmany HK, Cattaneo CG & Barnes RA. Predictors of hypothermia during spinal anesthesia. Anesthesiology 2000; 92: 13301334. * 64. Macario A & Dexter F. What are the most important risk factors for a patients developing intraoperative hypothermia? Anesthesia and Analgesia 2002; 94: 215220. 65. Butterworth J. Physiology of spinal anesthesia: what are the implications for management? Regional Anesthesia and Pain Management 1998; 23: 370373. 66. Steinbrook RA & Concepcion M. Respiratory effects of spinal anesthesia: resting ventilation and singlebreath CO2 response. Anesthesia and Analgesia 1991; 72: 182186. 67. Egbert LD, Tamersoy K & Deas TC. Pulmonary function during spinal anesthesia: the mechanism of cough depression. Anesthesiology 1961; 22: 822. 68. Hasrrop-Grifths AW, Ravalia A, Browne DA & Robinson PN. Regional anesthesia and cough effectiveness. Anaesthesia 1991; 46: 11 13. 69. Pitkanen MT. Body mass and spread of spinal anesthesia with bupivacaine. Anesthesia and Analgesia 1987; 66: 127131. 70. Steinbrook RA. Respiratory effects of spinal anesthesia. International Anesthesiology Clinics 1989; 27: 4045. 71. Giesecke Jr AH, Cale JO & Jenkins MT. The prostate, ventilation, and anesthesia. Journal of the American Medical Association 1968; 203: 389 391. 72. Steinbrook RA, Concepcion M & Topulos GP. Ventilatory responses to hypercapnia during bupivacaine spinal anesthesia. Anesthesia and Analgesia 1988; 67: 247252. 73. Greene NM & Brull SJ. The central nervous system. In Grayson TH (ed.) Physiology of Spinal Anesthesia, 4th edn. Baltimore: Williams and Wilkins, 1993, pp 183. 74. Tverskoy M, Shagal M, Finger J & Kissin I. Subarachnoid bupivacaine blockade decreased midazolam and thiopental hypnotic requirements. Journal of Clinical Anesthesia 1994; 6: 487490. 75. Ben-David B, Vaida S & Gaitini L. The inuence of high spinal anesthesia on sensitivity to midazolam sedation. Anesthesia and Analgesia 1995; 81: 525528. 76. Gentili M, Chau HP, Enel D et al. Sedation depends on the level of sensory block induced by spinal anaesthesia. British Journal of Anaesthesia 1998; 81: 970 971. 77. Hodgson PS, Liu SS & Gras TW. Does epidural anesthesia have general anesthetic effects? Anesthesiology 1999; 91: 16871692. * 78. Pollock JE, Neal JM, Liu SS et al. Sedation during spinal anesthesia. Anesthesiology 2000; 93: 728734.
You might also like
- DKA ScenarioDocument21 pagesDKA ScenarioLee June LyngNo ratings yet
- FinalfrcaDocument68 pagesFinalfrcaLee June LyngNo ratings yet
- Fast Track SurgeryDocument39 pagesFast Track SurgeryLee June LyngNo ratings yet
- Respiratory AcidosisDocument1 pageRespiratory AcidosisLee June LyngNo ratings yet
- Normal Anion Gap Acidoses1Document1 pageNormal Anion Gap Acidoses1Lee June LyngNo ratings yet
- Stress Response in Surgery and TraumaDocument9 pagesStress Response in Surgery and TraumaLee June LyngNo ratings yet
- Aorta Cross ClampingDocument10 pagesAorta Cross ClampingLee June LyngNo ratings yet
- SuxamethoniumDocument34 pagesSuxamethoniumLee June LyngNo ratings yet
- Cvs PharmacologyDocument4 pagesCvs PharmacologyLee June LyngNo ratings yet
- 221 Smoking and AnaesthesiaDocument4 pages221 Smoking and AnaesthesiaLee June Lyng100% (1)
- Use of BicarbonateDocument1 pageUse of BicarbonateLee June LyngNo ratings yet
- Respiratory AlkalosisDocument1 pageRespiratory AlkalosisLee June LyngNo ratings yet
- Acidosis in Kidney DiseasesDocument1 pageAcidosis in Kidney DiseasesLee June LyngNo ratings yet
- Lactic AcidosisDocument1 pageLactic AcidosisLee June LyngNo ratings yet
- Metabolic AlkalosisDocument1 pageMetabolic AlkalosisLee June LyngNo ratings yet
- Neurophys.... Membrane PotentialDocument49 pagesNeurophys.... Membrane PotentialLee June LyngNo ratings yet
- Metabolic AcidosisDocument1 pageMetabolic AcidosisLee June LyngNo ratings yet
- KetoacidosisDocument1 pageKetoacidosisLee June LyngNo ratings yet
- Phar of Inhalational AnaesDocument6 pagesPhar of Inhalational AnaesLee June LyngNo ratings yet
- Approach To Abg AnalysisDocument1 pageApproach To Abg AnalysisLee June LyngNo ratings yet
- Stress Response in Surgery and TraumaDocument9 pagesStress Response in Surgery and TraumaLee June LyngNo ratings yet
- Arterial Blood GasesDocument1 pageArterial Blood GasesLee June LyngNo ratings yet
- Pharmacology of ParecoxibDocument8 pagesPharmacology of ParecoxibLee June LyngNo ratings yet
- Cvs PharmacologyDocument4 pagesCvs PharmacologyLee June LyngNo ratings yet
- Obesity and AnaesDocument6 pagesObesity and AnaesLee June LyngNo ratings yet
- Renal Replacement Therapy JunelyngDocument87 pagesRenal Replacement Therapy JunelyngLee June LyngNo ratings yet
- Pharmacology of IV InductionDocument6 pagesPharmacology of IV InductionLee June LyngNo ratings yet
- Intrathecal OpiodsDocument5 pagesIntrathecal OpiodsLee June LyngNo ratings yet
- Lactate PhysiologyDocument5 pagesLactate PhysiologyLee June LyngNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Recent Advances in Endodontic SurgeryDocument29 pagesRecent Advances in Endodontic Surgeryhenavns50% (2)
- Local AnesthesiaDocument4 pagesLocal AnesthesiawowoNo ratings yet
- Local Anesthesia Techniques in Oral and Maxillofacial SurgeryDocument102 pagesLocal Anesthesia Techniques in Oral and Maxillofacial Surgerydr_jamal1983No ratings yet
- Unit 11 Arterial PunctureDocument34 pagesUnit 11 Arterial PunctureZoe Rodriguez100% (1)
- Oral Serguary MCQDocument9 pagesOral Serguary MCQmohamed saadNo ratings yet
- Local Anesthesia - Definition of Local Anesthesia in The Medical Dictionary - by The Free Online Medical Dictionary, Thesaurus and EncyclopediaDocument10 pagesLocal Anesthesia - Definition of Local Anesthesia in The Medical Dictionary - by The Free Online Medical Dictionary, Thesaurus and EncyclopediaAkhilesh PipadaNo ratings yet
- Percutaneous Imaging-Guided Spinal Facet Joint InjectionsDocument6 pagesPercutaneous Imaging-Guided Spinal Facet Joint InjectionsAlvaro Perez HenriquezNo ratings yet
- 75 Medicinal Chemistry IIDocument9 pages75 Medicinal Chemistry IISalman SkNo ratings yet
- Dwnload Full Applied Pharmacology For The Dental Hygienist 7th Edition Haveles Solutions Manual PDFDocument35 pagesDwnload Full Applied Pharmacology For The Dental Hygienist 7th Edition Haveles Solutions Manual PDFmanganicidealityfy9rc1100% (12)
- Anesthprog00276-0033-Summary of The Scientific Literature For Pain and Anxiety Control in Dentistry-Journal Literature, January 1986-December 1987Document19 pagesAnesthprog00276-0033-Summary of The Scientific Literature For Pain and Anxiety Control in Dentistry-Journal Literature, January 1986-December 1987skyclad_21No ratings yet
- Efficacy of Adductor Canal Block in Total Knee Arthroplasty: A Systematic ReviewDocument10 pagesEfficacy of Adductor Canal Block in Total Knee Arthroplasty: A Systematic ReviewHalim SudonoNo ratings yet
- PPP Reading Test 6 Parts BC Question PaperDocument16 pagesPPP Reading Test 6 Parts BC Question PaperJaisy Martin100% (3)
- Sural Nerve BiopsyDocument2 pagesSural Nerve BiopsyArindam MukherjeeNo ratings yet
- Saudi J Anaesth 2013 7 1 57 60-TerkunciDocument4 pagesSaudi J Anaesth 2013 7 1 57 60-TerkunciRafael BagusNo ratings yet
- Understanding Craniotomy: Types, Procedure, Risks & RecoveryDocument21 pagesUnderstanding Craniotomy: Types, Procedure, Risks & RecoveryEshel Juliene100% (1)
- NCM 112 - Drug StudyDocument35 pagesNCM 112 - Drug StudyZoe WsetNo ratings yet
- Management of Local Anesthetic Complications: Ross Camiel, Samuel Roh, and Christy LottingerDocument10 pagesManagement of Local Anesthetic Complications: Ross Camiel, Samuel Roh, and Christy LottingerErryskaNo ratings yet
- Drugs SevofluraneDocument9 pagesDrugs Sevofluranequincym75% (4)
- Acute Wound CareDocument73 pagesAcute Wound CareDikaNo ratings yet
- Institutional Research Guidelines A.Y. 2018-2019: Pines City CollegesDocument18 pagesInstitutional Research Guidelines A.Y. 2018-2019: Pines City CollegesPau CastilloNo ratings yet
- ADC HandbookDocument16 pagesADC HandbookJats_Fru_1741No ratings yet
- Benzydamine HCL Drug StudyDocument1 pageBenzydamine HCL Drug StudyKrissy JavaNo ratings yet
- Biers BlockDocument4 pagesBiers Blockemkay1234No ratings yet
- DrugsDocument81 pagesDrugsrevathidadam55555100% (1)
- Local anesthetic bupivacaine nursing considerationsDocument2 pagesLocal anesthetic bupivacaine nursing considerationsPutuNo ratings yet
- Local Anesthesia Manual GuideDocument81 pagesLocal Anesthesia Manual GuideRichiene Bartolome CustorioNo ratings yet
- How To Perform A Digital Finger Block PDFDocument3 pagesHow To Perform A Digital Finger Block PDFsuasponte2100% (1)
- 2017 Book You Are Wrong, I Am RightDocument404 pages2017 Book You Are Wrong, I Am RightPaulo HibernonNo ratings yet
- (Contemporary Perspectives in Rehabilitation) Charles D. Ciccone - Melissa Duffield (Editor) - Dean DeChambeau (Editor) - Pharmacology in Rehabilitation-F.a. Davis Company (2016)Document737 pages(Contemporary Perspectives in Rehabilitation) Charles D. Ciccone - Melissa Duffield (Editor) - Dean DeChambeau (Editor) - Pharmacology in Rehabilitation-F.a. Davis Company (2016)Kathy LawrenceNo ratings yet
- Why Does Inferior Alveolar Nerve Block Fail - A ReviewDocument15 pagesWhy Does Inferior Alveolar Nerve Block Fail - A ReviewSetu KatyalNo ratings yet