Professional Documents
Culture Documents
Metabolic Alkalosis
Uploaded by
Lee June LyngOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Metabolic Alkalosis
Uploaded by
Lee June LyngCopyright:
Available Formats
General - Potassium depletion occurs with situations of mineralocorticoid excess.
Bicarbonate reabsorption in both the proximal and distal tubules is increased in the presence of potassium depletion. Potassium depletion decreases aldosterone release by the adrenal cortex. Primary Hyperaldosteronism - This condition is one cause of 'saline-resistant' metabolic alkalosis. The increased aldosterone levels lead to increased distal tubular Na+ reabsorption and increased K+ & H+ losses. The increased H+ loss is matched by increased amounts of renal HCO3leaving in the renal vein. The net result is metabolic alkalosis with hypochloraemia and hypokalaemia, often with an expanded ECF volume. Cushing's Syndrome - The excess corticosteroids have some mineralocorticoid effects and because of this can produce a metabolic alkalosis. The alkalosis is most severe with the syndrome of ectopic ACTH production. Severe K+ depletion - Cases have been reported of patients with metabolic alkalosis and severe hypokalaemia ([K+] < 2 mmol/l) due to severe total body potassium depletion. Investigation has not shown increased mineralocorticoid activity. The aetiology in these patients is not understood but correction of the alkalosis requires correction of the potassium deficit. These patients do not respond to saline loading unless K+ replacement is sufficient to correct the deficit. Urinary chloride losses are high (>20mmol/l). Bartter's syndrome - This is a syndrome of increased renin and aldosterone levels due to hyperplasia of the juxtaglomerular apparatus. It is inherited as an autosomal recessive disorder. The increased aldosterone levels usually result in a metabolic alkalosis. The condition is usually found in children. Patients who present with hypokalaemic alkalosis of uncertain cause are often suspected of having this condition but other causes which may be denied by the patient should be considered eg surreptitious vomiting and/or use of diuretics for weight loss or psychological problems. Rare genetic disorders such as Gitelmann's syndrome should also be considered. Adverse Effects of Alkalosis (i) decreased myocardial contractility (ii) arrhythmias (iii) decreased cerebral blood flow (iv) confusion (v) mental obtundation (vi) neuromuscular excitability (vii) impaired peripheral oxygen unloading (due shift of oxygen dissociation curve to left). - Hypoxaemia may occur and oxygen delivery to the tissues may be reduced. - Factors involved in impaired arterial oxygen content are: (i) Hypoventilation (due respiratory response to metabolic alkalosis) (ii) Pulmonary microatelectasis (consequent to hypoventilation) (iii) Increased ventilation-perfusion mismatch (as alkalosis inhibits hypoxic pulmonary vasoconstriction) - Peripheral oxygen unloading may be impaired because of the alkalotic shift of the haemoglobin oxygen dissociation curve to the left. The body's major compensatory response to impaired tissue oxygen delivery is to increase cardiac output but this ability is impaired if hypovolaemia and decreased myocardial contractility are present. - The hypoventilation causes a compensatory rise in arterial pCO2 but the magnitude of the response has generally been found to be quite variable. - Failure of hypoventilation may be attributed (i) Hyperventilation due to pain (ii)Hyperventilation due to pulmonary congestion. - Some patients with metabolic alkalosis due to diuretic use have subclinical pulmonary congestion sufficient to stimulate intrapulmonary receptors and cause tachypnoea and give a sensation of dyspnoea. This slight hyperventilation is sufficient to negate the rise in arterial pCO2. (iii) Hyperventilation due to hypoxaemia. - An associated hypoxaemia will stimulate the peripheral chemoreceptors and cause hyperventilation if the arterial pO2 is below 50 to 55mmHg. - The expected pCO2 due to appropriate hypoventilation in simple metabolic alkalosis can be estimated from the following formula: Expected pCO2 = 0.7 [HCO3] + 20 mmHg (range: +/- 5) - While it is widely believed that the maximum value of arterial pCO2 due to compensatory hypoventilation is 55 to 60mmHg arterial pCO2 can rise higher than this and values up to 86mmHg have been reported in severe cases of metabolic alkalosis
definition
- A metabolic alkalosis is a primary acid-base disorder which causes the plasma bicarbonate to rise to a level higher than expected. The severity of a metabolic alkalosis is determined by the difference between the actual [HCO3] and the expected [HCO3]. general: - The kidney rapidly excretes bicarbonate if the plasma level is elevated - This ability of the kidney to rapidly excrete bicarbonate if its level is high is in complete contrast to its powerful ability to reabsorb all of the filtered load if plasma [HCO3] is low or normal. - The persistence of a metabolic alkalosis requires an additional process which acts to impair renal bicarbonate excretion. - This means that two issues must to be considered when analysing a metabolic alkalosis: (i) Initiation: What process is initiating the disorder? (ii) Maintenance: What process is maintaining the disorder? The Initiating Process - Classification of Initiating Processes for Metabolic Alkalosis 1. Gain of alkali in the ECF (i) from an exogenous source (eg IV NaHCO3 infusion, citrate in transfused blood) (ii) from an endogenous source (eg metabolism of ketoanions to produce bicarbonate) 2. Loss of H+ from ECF (i) via kidneys (eg use of diuretics) (ii) via gut (eg vomiting, NG suction) - Excessive intravenous administration of alkali alone will cause a metabolic alkalosis which is only short-lived because of rapid renal excretion of bicarbonate - Hepatic metabolism of citrate, lactate, acetate or certain other organic acid anions to bicarbonate can cause a brief metabolic alkalosis. This may occur after a massive blood transfusion because of the metabolism of the administered citrate. The kidneys excrete the bicarbonate and the urine will be relatively alkaline. Maintenance of Alkalosis - Maintenance of the alkalosis requires a process which greatly impairs the kidney's ability to excrete bicarbonate and prevent the return of the elevated plasma level to normal. - The four factors that cause maintenance of the alkalosis (by increasing bicarbonate reabsorption in the tubules or decreasing bicarbonate filtration at the glomerulus) are: (i) Chloride depletion (ii) Reduced glomerular filtration rate (GFR) (iii) Potassium depletion (iv) ECF volume depletion Metabolic Alkalosis Classification Based on Urinary Chloride 1. Urine Cl- < 10 mmol/l - Often associated with volume depletion (increased proximal tubular reabsorption of HCO3) - Respond to saline infusion (replaces chloride and volume) - Causes: previous diuretic therapy, vomiting 2. Urine Cl- > 20 mmol/l - Often associated with volume expansion and hypokalaemia - Resistant to therapy with saline infusion - Cause: Excess aldosterone, severe K+ deficiency - Other causes: diuretic therapy (current), Bartter's syndrome - Recent diuretic use can acutely elevate the urinary chloride level but as the diuretic effect passes the urinary chloride level will fall to low levels. So seek information on the timing of diuretic use. (This variability in urine chloride levels has been used as an indicator of surreptious diuretic use) - A 'spot' urine chloride may be misleading if bladder urine contains a mixture of urine from during and after diuretic effect. - A high urinary chloride in association with hypokalaemia suggests mineralocorticoid excess. - The urinary chloride/creatinine ratio may occasionally be useful as it is elevated if there is an extra-renal cause of alkalosis.
potassium depletion
causes
effects of metabolic alkalosis
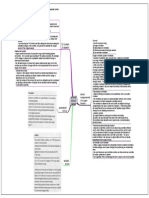
metabolic alkalosis [created by Paul Young 14/12/07]
urinary chloride measurements
compensation
1. Correct cause if possible (eg correct pyloric obstruction, cease diuretics) 2. Correct the deficiency which is impairing renal bicarbonate excretion (ie give chloride, water and K+) - chloride administration is essential for correction of chloride depletion metabolic alkalosis 3. Expand ECF Volume with N/saline (and KCl if K+ deficiency) - Mineralocorticoid excess causes renal potassium wasting. This can maintain a metabolic alkalosis even in the absence of chloride depletion. 4. If the diagnosis is not obvious, spot urine chloride is useful: low levels suggest Cl- depletion and need for replacement; high levels suggest adrenocortical excess and need for K+ replacement 5. Rarely ancillary measures such as: - HCl infusion - Acetazolamide (one or two doses only) - Oral lysine hydrochloride 6. Supportive measures (eg give O2 in view of hypoventilation; appropriate monitoring and observation) Avoid hyperventilation as this worsens the alkalaemia
chloride depletion
treatment
General - The commonest causes in clinical practice are those causing chloride depletion - Administration of chloride is necessary to correct these disorders. The two commonest causes of chronic metabolic alkalosis accounting for 90% of cases are loss of gastric juice and diuretic therapy. (i) Gastric alkalosis - most marked with vomiting due to pyloric stenosis or obstruction because the vomitus is acidic gastric juice only. Vomiting in other conditions may involve a mixture of acid gastric loss and alkaline duodenal contents and the acid-base situation that results is more variable. Histamine H2-blockers also decrease gastric H+ losses despite continued vomiting or nasogastric drainage and alkalosis will not occur if the fluid lost is not particularly acidic - indeed loss of alkaline small intestinal contents can even result in an acidosis if gasric acid secretion is suppressed. (ii) Diuretics -diuretics such as frusemide and thiazides interfere with reabsorption of chloride and sodium in the renal tubules. Urinary losses of chloride exceed those of bicarbonate. The patients on diuretics who develop an alkalosis are those who are also volume depleted (increasing aldosterone levels) and have a low dietary chloride intake ('salt restricted' diet). Hypokalaemia is common in these patients. - The effect of diuretic use on urinary chloride levels depends on the relationship of the time of urine collection to diuretic effect: it is high while the diuretic is acting, but drops to low levels afterwards. (iii) other causes - Villous adenomas typically excrete bicarbonate and can cause a hyperchloraemic metabolic acidosis. Sometimes they excrete chloride predominantly and the result is then a metabolic alkalosis. - Chloride diarrhoea is a rare congenital condition due to an intestinal transport defect, where the chronic faecal chloride loss can (if associated with volume depletion and K+ loss as maintenance factors) result in a metabolic alkalosis.
You might also like
- DKA ScenarioDocument21 pagesDKA ScenarioLee June LyngNo ratings yet
- FinalfrcaDocument68 pagesFinalfrcaLee June LyngNo ratings yet
- Fast Track SurgeryDocument39 pagesFast Track SurgeryLee June LyngNo ratings yet
- Respiratory AcidosisDocument1 pageRespiratory AcidosisLee June LyngNo ratings yet
- Normal Anion Gap Acidoses1Document1 pageNormal Anion Gap Acidoses1Lee June LyngNo ratings yet
- Stress Response in Surgery and TraumaDocument9 pagesStress Response in Surgery and TraumaLee June LyngNo ratings yet
- Aorta Cross ClampingDocument10 pagesAorta Cross ClampingLee June LyngNo ratings yet
- SuxamethoniumDocument34 pagesSuxamethoniumLee June LyngNo ratings yet
- Cvs PharmacologyDocument4 pagesCvs PharmacologyLee June LyngNo ratings yet
- 221 Smoking and AnaesthesiaDocument4 pages221 Smoking and AnaesthesiaLee June Lyng100% (1)
- Use of BicarbonateDocument1 pageUse of BicarbonateLee June LyngNo ratings yet
- Respiratory AlkalosisDocument1 pageRespiratory AlkalosisLee June LyngNo ratings yet
- Stress Response in Surgery and TraumaDocument9 pagesStress Response in Surgery and TraumaLee June LyngNo ratings yet
- KetoacidosisDocument1 pageKetoacidosisLee June LyngNo ratings yet
- Metabolic AcidosisDocument1 pageMetabolic AcidosisLee June LyngNo ratings yet
- Neurophys.... Membrane PotentialDocument49 pagesNeurophys.... Membrane PotentialLee June LyngNo ratings yet
- Lactic AcidosisDocument1 pageLactic AcidosisLee June LyngNo ratings yet
- Arterial Blood GasesDocument1 pageArterial Blood GasesLee June LyngNo ratings yet
- Phar of Inhalational AnaesDocument6 pagesPhar of Inhalational AnaesLee June LyngNo ratings yet
- Acidosis in Kidney DiseasesDocument1 pageAcidosis in Kidney DiseasesLee June LyngNo ratings yet
- Spinal Anaesthesia2Document15 pagesSpinal Anaesthesia2Lee June LyngNo ratings yet
- Approach To Abg AnalysisDocument1 pageApproach To Abg AnalysisLee June LyngNo ratings yet
- Pharmacology of ParecoxibDocument8 pagesPharmacology of ParecoxibLee June LyngNo ratings yet
- Cvs PharmacologyDocument4 pagesCvs PharmacologyLee June LyngNo ratings yet
- Obesity and AnaesDocument6 pagesObesity and AnaesLee June LyngNo ratings yet
- Renal Replacement Therapy JunelyngDocument87 pagesRenal Replacement Therapy JunelyngLee June LyngNo ratings yet
- Pharmacology of IV InductionDocument6 pagesPharmacology of IV InductionLee June LyngNo ratings yet
- Intrathecal OpiodsDocument5 pagesIntrathecal OpiodsLee June LyngNo ratings yet
- Lactate PhysiologyDocument5 pagesLactate PhysiologyLee June LyngNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Pdev 111 Week 1 20 1st SemesterDocument123 pagesPdev 111 Week 1 20 1st SemesterReyn TabelismaNo ratings yet
- Teardrop by Lauren KateDocument47 pagesTeardrop by Lauren KateRandom House Teens88% (16)
- Communicating Across AgesDocument35 pagesCommunicating Across AgesConrad TarihoranNo ratings yet
- Written Work Instruction (Sheet Piles Installation)Document14 pagesWritten Work Instruction (Sheet Piles Installation)cynthia100% (1)
- Low Back Pain Anatomy of Thoracolumbar SpineDocument10 pagesLow Back Pain Anatomy of Thoracolumbar SpineMNo ratings yet
- Comparative Analysis of Mineral Constituents of Ethanol Leaf and SeedDocument9 pagesComparative Analysis of Mineral Constituents of Ethanol Leaf and SeedKIU PUBLICATION AND EXTENSIONNo ratings yet
- Handout2 Fischer CarbeneDocument5 pagesHandout2 Fischer CarbeneMuhammad ShimaNo ratings yet
- Chapter Test A: Teacher Notes and Answers 17Document5 pagesChapter Test A: Teacher Notes and Answers 17Mmf 123 JanNo ratings yet
- BOS II SlickDocument2 pagesBOS II SlickDineu OliveiraNo ratings yet
- Medical Student Assessment Form in PDFDocument4 pagesMedical Student Assessment Form in PDFDanial S. SaktiNo ratings yet
- Viscometer Toki Sangyo - TV25 - 35Document12 pagesViscometer Toki Sangyo - TV25 - 35Eddy CurrentNo ratings yet
- Ravi ProjectDocument92 pagesRavi ProjectAvinash Avii100% (1)
- Unit 1 Organic Questions Q1Document5 pagesUnit 1 Organic Questions Q1Hadeel DossaNo ratings yet
- (UNISIM (BEHAS) - Introduction To Aerospace) EAS105 - Lab4Document33 pages(UNISIM (BEHAS) - Introduction To Aerospace) EAS105 - Lab4Mohd Ashraf Mohd IsmailNo ratings yet
- Work Family Conflict Dengan KinerjaDocument11 pagesWork Family Conflict Dengan KinerjaNinaerizaNo ratings yet
- ABS and Air Conditioner Wiring DiagramDocument207 pagesABS and Air Conditioner Wiring Diagramservice_00783% (30)
- STRATEGIC MANAGEMENT FRAMEWORKDocument19 pagesSTRATEGIC MANAGEMENT FRAMEWORKCharles CagaananNo ratings yet
- NCL ReportDocument20 pagesNCL ReportSwati Tripathi33% (3)
- Basseri TribeDocument3 pagesBasseri TribeMaddah HussainNo ratings yet
- The Positive and Negative Syndrome Scale PANSS ForDocument5 pagesThe Positive and Negative Syndrome Scale PANSS ForditeABCNo ratings yet
- PreparationDocument2 pagesPreparationmghaffarzadehNo ratings yet
- New Accreditation ToolsDocument52 pagesNew Accreditation ToolsLyle Guion Paguio100% (1)
- 2008 Annual Debt StatementDocument12 pages2008 Annual Debt StatementEwing Township, NJNo ratings yet
- Environmental Clearance CertificateDocument4 pagesEnvironmental Clearance CertificateAra Jane T. PiniliNo ratings yet
- JMPR 2010 ContentsDocument55 pagesJMPR 2010 ContentsTÙNGNo ratings yet
- Deutz-Fahr Workshop Manual for AGROTRON MK3 ModelsDocument50 pagesDeutz-Fahr Workshop Manual for AGROTRON MK3 Modelstukasai100% (1)
- Inspection and Repair of Aircraft Integral Tanks AND Fuel CellsDocument222 pagesInspection and Repair of Aircraft Integral Tanks AND Fuel CellsgnanasekarNo ratings yet
- Lesson Plan The Food: TH THDocument8 pagesLesson Plan The Food: TH THFeraru FlorinNo ratings yet
- Do We Still Need Formocresol in Pediatric DentistryDocument3 pagesDo We Still Need Formocresol in Pediatric DentistryAlexanderDetorakisNo ratings yet
- The Dukan Diet by Dr. Pierre Dukan - ExcerptDocument8 pagesThe Dukan Diet by Dr. Pierre Dukan - ExcerptCrown Publishing Group15% (20)