Professional Documents
Culture Documents
Adverse Reactions
Uploaded by
Chrissie0 ratings0% found this document useful (0 votes)
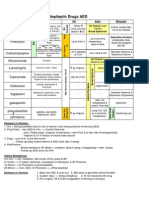
64 views1 pageThis document discusses various adverse drug reactions and effects related to different body systems and drug classes. It covers drugs that can induce lupus or autoimmune diseases, those causing extrapyramidal symptoms, endocrine effects like changes to thyroid and prolactin levels, hematological issues such as hemolytic anemia and effects on platelets or red blood cells, electrolyte imbalances, cardiac toxicities, organ toxicities, and other miscellaneous reactions. Multiple categories, acronyms and mnemonics are provided to help remember various drugs that can cause similar side effects.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses various adverse drug reactions and effects related to different body systems and drug classes. It covers drugs that can induce lupus or autoimmune diseases, those causing extrapyramidal symptoms, endocrine effects like changes to thyroid and prolactin levels, hematological issues such as hemolytic anemia and effects on platelets or red blood cells, electrolyte imbalances, cardiac toxicities, organ toxicities, and other miscellaneous reactions. Multiple categories, acronyms and mnemonics are provided to help remember various drugs that can cause similar side effects.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
64 views1 pageAdverse Reactions
Uploaded by
ChrissieThis document discusses various adverse drug reactions and effects related to different body systems and drug classes. It covers drugs that can induce lupus or autoimmune diseases, those causing extrapyramidal symptoms, endocrine effects like changes to thyroid and prolactin levels, hematological issues such as hemolytic anemia and effects on platelets or red blood cells, electrolyte imbalances, cardiac toxicities, organ toxicities, and other miscellaneous reactions. Multiple categories, acronyms and mnemonics are provided to help remember various drugs that can cause similar side effects.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
adverse reactions
autoimmune diseases lupus
Lupus: drugs inducing itHIP:
Hydralazine
INH
Procanimide
relating to neurotransmitter
antidopaminerg
extrapyramidal
tardive dyskinesa
may persist after withdrawal
involuntary movements of jaw, tongue and face
after long term use
acute dystonic reactons (slow, prolonged muscle spasms of tongue, neck and face)
parkinsonian syndrome (bradykinic rigidity, tremor)
akathisia (motor restlessness)
prolactin elevation endocrine alteration: galactorrhea, amenorrhea, infertility, decreased libido
alpha-blockade
reflex tachycardia
orthostatic hypotension
ani-serotoninerg weight gain
antihistaminic
weight gain
sedation
anticholinergic
tachycardia
dry mouth, constipation, urinary retention, blurry vision
CNS sedation cognitive impairment
GENERAL
Type A (Augmented) Type B (Bizarre) Predictable Unpredictable Dose-dependent Dose-independent
High incidence Low incidence (90% ADRs) Often serious May respond to Generally need dose
adjustment to stop drug
endocrinal effects
thyroid
hyperthyrodism
hypothyrodism
interferon
decreases absorption of T4
raloxifene
calcium
ciprofloxacin
lithium
amiodarone
medication can alter TSH levels
somatostatin and analogs minimal effect
dopamine
agonists and antagonists
minimal effect
corticosteroids minimal effect
insulin
hyperglycaemia
furosemide
thiazides
isoniazide
pentamidine (long-term effect)
nicotinic acid
protease inhibitors
phenytoin
oestrogen
diuretics
corticosteroids
ciclosporin
beta agonist, sympathomimetics
atypical antipsychotics
hypoglycaemia
pentamidine (initial effect)
fenfluramine
fluoxetine
MAO
salicylates (large doses)
sulphonamides
beta-blockers (prolonged hypo-and masking of symptoms)
alcohol
ACE inhibitors
endocrinal effects
prolactin levels
decreasing
ergot alkaloids
L-dopa
increasing
phenothiazines
haloperidol
methyldopa
syndrome of inappropriate antidiuretic hormone secretion (SIADH)
SIADH-inducing drugs ABCD:
Analgesics: opioids, NSAIDs
Barbiturates
Cyclophosphamide/ Chlorpromazine/ Carbamazepine
Diuretic (thiazide)
Gynaecomastia-causing drugs DISCOS:
Digoxin
Isoniazid
Spironolactone
Cimetidine
Oestrogens
Stilboestrol
relating to metabolism uric acid
hyperuricemia are renal dysfunction, metabolic acidosis, tumor lysis syndrome,
purine-rich diet, and use of furosemide, thiazide diuretics, and niacin.2,15
Hyperuricemia may be associated with the development of gouty arthri-
tis, nephrolithiasis, and gouty tophi.2
Decreased Uric Acid
Decreased uric acid levels (hypouricemia) are usually of little clinical signifi-
cance but may occur with a low-protein diet, deficiency of xanthine oxidase,
or use of allopurinol, probenecid, or high doses of aspirin or vitamin C.2,1
decrease
increase nateglinide
relating to blood
There are two types of the Coombs' test:
The indirect Coombs' test looks for free-flowing antibodies against certain red blood cells. It is is most
often done to determine if you may have a reaction to a blood transfusion.
The direct Coombs' test is used to detect antibodies that are stuck to the surface of red blood cells.
Many diseases and drugs (including quinidine, methyldopa, and procainamide) can cause this. These
antibodies sometimes destroy red blood cells and cause anemia. Your doctor may order this test if you
have signs or symptoms of anemia or jaundice.
decreased platelet count
acetazolamide, acetohexamide, antimony, antineoplastic drugs, brompheniramine maleate,
carbamazepine, chloramphenicol, furosemide, gold salts, isoniazid, mephentoin, methyldopa,
sulfonamides, thiazide, heparin, valproic acid and many others.
G6PD deficiency
Glucose-6-phosphate dehydrogenase deficiency is an X-linked recessive hereditary disease
characterized by abnormally low levels of glucose-6-phosphate dehydrogenase, a metabolic enzyme
involved in the pentose phosphate pathway, especially important in red blood cell metabolism. G6PD
deficiency is the most common human enzyme defect.Individuals with the disease may exhibit
nonimmune hemolytic anemia in response to a number of causes, most commonly infection or
exposure to certain medications or fava beans. G6PD deficiency is closely linked to favism, a disorder
characterized by a hemolytic reaction to consumption of fava or broad beans, with a name derived
from the Italian name of the broad bean (fava). The name favism is sometimes used to refer to the
enzyme deficiency as a whole, although this is misleading as not all people with G6PD deficiency or
Favism will manifest physically observable symptoms to the consumption of broad beans. Symptomatic
patient are all almost exclusively males.
G6PD: oxidant drugs inducing hemolytic anemia AAA: Antibiotic (eg: sufamethoxazole)
Antimalarial (eg: primaquine)
Antipyietics (eg: acetaniliu, but not aspiiin oi acetaminophen
hemolytic anemia
isosorbid dinitrate
quinidin
phenacetin
aspirin
primaquinine
nitrofurantoin
sulfonamide
quinine
Porphyrias: acute intermittent porphyria symptoms 5 P's:
Pain in abdomen
Polyneuropathy
Psychologial abnormalities
Pink urine
Precipitated by drugs (eg barbiturates, oral contraceptives, sulpha drugs)
relating to electrolytes
Cl-levels use of acid suppressants (H2 blockers and proton pump inhibitors [PPIs])
Na-level
decreasing
2,10 Sodium depletion
may also be seen in SIADH, cystic fibrosis, mineralocorticoid deficiency, or
fluid replacement with solutions that do not contain sodium.10
SIADH may be associated with disease states such as cancer or the use of
medications, including chlorpropamide, thiazide diuretics, and carbamazepine.2
increasing
Phosphat-level
decreasing
increasing
Ca-level
decreasing loop diuretics
increasing lithiium and thiazides
K-level
decreasing and use of amphotericin B or thiazide, loop, or osmotic diuretics
increasing
2,10 Medications such as angiotensin enzyme
converting (ACE) inhibitors, angiotensin receptor blockers (ARBs), potassium
supplements, potassium-sparing diuretics, and oral contraceptives containing
drospirenone are also contributing factors to hyperkalemia.1,10
K+ increasing agents K-BANK:
K-sparing diuretic
Beta blocker
ACEI
NSAID
K supplement
CNS reaction
seizures antibiotics penicillin G, imipenem, amphotericin B, metronidazole
disulfiram like reactions
sulfonylureas
metronidazole
depression
5 drugs causing it PROMS:
Propranolol
Reserpine
Oral contraceptives
Methyldopa
Steroids
delirium
Delerium-causing drugsACUTE CHANGE IN MS:
Antibiotics (biaxin, penicillin, ciprofloxacin)
Cardiac drugs (digoxin, lidocaine)
Urinary incontinence drugs (anticholinergics)
Theophylline
Ethanol
Corticosteroids
H2 blockers
Antiparkinsonian drugs
Narcotics (esp. mepridine)
Geriatric psychiatric drugs
ENT drugs
Insomnia drugs
NSAIBs (eg inuomethacin, napioxin
Muscle relaxants
Seizuie meuicines
medicine groups
Sulfonamide side effects:
Steven-Johnson syndrome
Skin rash
Solubility low (causes crystalluria)
Serum albumin displaced (causes newborn kernicterus and potentiation of other serum
albumin-binders like warfarin)
teratogenic drugs
Antibiotics contraindicated during pregnancy MCAT:
Metronidazole
Chloramphenicol
Aminoglycoside
Tetracycline
Teratogenic drugs"W/ TERATOgenic":
Warfarin
Thalidomide
Epileptic drugs: phenytoin, valproate, carbamazepine
Retinoid
ACE inhibitor
Third element: lithium
OCP and other hormones (eg danazol)
TAP CAP Thalidomide Androgens Progestins Corticosteroids Aspirin & indomethacinPhenytoin
organ toxicity
kidney
mouth taste disturbances
Other Antihistamines, antineoplastics, bronchodilators, anti-inflammatories, smoking cessation
aids, antifungals, antivirals
acetazolamide
clacitriol
phenindione
chlorhexidine
griseofulvin
metformin
gold salts
penicillamine
aspirin
Psychotropics Most tricyclic antidepressants, some antipsychotics, anxiolytics, mood stabilizers,
hypnotics
imipramine
Endocrine medications Most thyroid medications carbimazole
Cardiac medications Many antihypertensives, diuretics, statins, antiarrhythmics
clofibrate
captopril
Neurologic medications Antiparkinsonians, CNS stimulants, migraine medications, muscle relaxants
lithium carbonate
levodopa
Antibiotics Ampicillin, macrolides, quinolones, sulfamethoxazole, trimethoprim, tetracycline,
metronidazole
metronidazole
heart
BP influenced by drugs
decreased a1 blocker effect
neuroleptics
clozapin
thioridazine
TCA
increased
erythropoetin
immunosuppressiva: ciclosporin and tacrolismus
NSAIDs
decreased GFR
decreased synthesis of prostacyclin in afferent arteries to glomeruli
estrogens increased angiotensinogen synthesis in liver
glucocorticoids, hydrocortison+prednisolon over mineralocorticoid receptors
psychostimulans
ephedrin
cocain
amphetamin
methylphenidate
noradrenalin reuptake increases
appetit inhbitiors, amfepramon or sibutramin
duloxetin
venlafaxin
reboxetin
MAO A or B antagonists
a-agonisten
torsades de pointes
TEQ Tricyclic antidepressants, Erythromycin, Quinidine
APACHE A miodarone, Procainamide, Arsenium, Cisapride, Haloperidol, Eritromycin
eye ocular toxicity
corticosteroids
phenothiazines
chlorpromazine
amiodarone
chloroquine, hydroxy-
lungs
Respiratory depression inducing drugs"STOP breathing":
Sedatives and hypnotics
Trimethoprim
Opiates Polymyxins
pulmonary toxicity
"uo BAN Ne!":
Gold Bleomycin/ Busulphan/ BCNU
Amiodarone/ Acyclovir/ Azathioprine
Nitrofurantoin
Melphalan/ Methotrexate/ Methysergide
bromocriptine
nitrofurantoin
amiodarone
bleomycine
liver
Hepatic necrosis: drugs causing focal to massive necrosis
"Very Angry Hepatocytes":
Valproic acid
Acetaminophen
Halothane
cholestatic jaundice
methyldopa
sulindac
certain TCA
trazodone
chlorpropamide
erythromycin estolate
chlorpromazine
ear
ringing in the ear quinidine
ototoxicity
loop diuretics
minocycline
animoglycosides
salicylates
hypersensitivy reactions
Pseudoallergic reactions(anaphylactoid)
They are, however, mediated pharmacologically and not immunologically (e.g. aspirin and NSAIDs in
asthma). The fact that they do not occur in everyone indicates some predisposition (e.g. genetic). This
is why this type of reaction is considered to be type B rather than type A. Cross-sensitivity occurs with
drugs which have the same action, but not structure, cf. true allergy.
Most drugs have small molecular weights (often ~300 D) and are too small to be antigenic in
themselves. They act as haptens, binding to endogenous proteins to form antigenic complexes that
incite antibody production. This process usually takes 12 weeks. Reexposure to the chemical results
in an antigenantibody interaction that provokes the typical manifestations of allergy a release of
mediators (e.g. histamine) cell damage or cell death.
see under IMMUNOLOGY
type V
Grave's disease
autoimmune disorders ???
type IV cell mediated
e.g. contact dermatitisby poison ivy)
infections (tuberculosis, leprosis,listeria)
acute graf rejection
contact dermatitis
T-cells
type III immune complex
Serum sickness (urticaria, arthralgia, lymphadenopathy and fever), is a classical presentation (e.g.
serum sickness due to sulphonamides or penicillins). Extreme form a StevensJohnson syndrome
non-organic autoimmune diseases
sjogren syndrome
rheumatoid arthritis
SLE
type II cytotoxic
(e.g. penicillinhaemolytic anaemia, quinidine thrombocytopenia,sulphonamide neutropenia).
organic autoimmune diseases
thrombocytopenia
Hashimoto
myasthenia gravis
pencillin, cephalosporin, quinidine, methyldopa may result in hemolytic anemia
Rh disease
IgM and IgG
type I immediate/anaphylactic
(e.g. anaphylaxis,urticaria and bronchospasm due to penicillin
certain vaccines
hormones
penicillin, cephalosporin
pollens
IgE
URINE CHANGES red colour
vitamin B
chlorpromazine
daunomycin / daunorubicin
warfarin
rifampicin
prochlorperazine
senna (anthrachinone)
You might also like
- Drug ListsDocument10 pagesDrug ListsAmber Merritt100% (1)
- Top 300 Drugs Pocket Reference Guide (2021 Edition)From EverandTop 300 Drugs Pocket Reference Guide (2021 Edition)Rating: 5 out of 5 stars5/5 (1)
- Naplex MpjeDocument35 pagesNaplex MpjeAtlantis ManNo ratings yet
- Naplex NotesDocument226 pagesNaplex NotesløzanNo ratings yet
- Total Pharmacy Notes TPN For EEDocument1,601 pagesTotal Pharmacy Notes TPN For EEClaire Cura100% (2)
- 2006 Info For MpjeDocument28 pages2006 Info For Mpjemina75% (4)
- Antiepileptic Drugs AED: D' DI Disadv SE AdvDocument1 pageAntiepileptic Drugs AED: D' DI Disadv SE Advrayooona88No ratings yet
- Pharmacy Operations: Licensure, Registration and CertifiacationsDocument5 pagesPharmacy Operations: Licensure, Registration and CertifiacationsHitomi Shiroshita100% (1)
- R: K D, M, S T: Xprep EY Rugs Nemonics Tudy IPSDocument18 pagesR: K D, M, S T: Xprep EY Rugs Nemonics Tudy IPSKNo ratings yet
- Pharmacy Laws, Medicare, Medicaid and Business Management: Copy Right ProtectedDocument8 pagesPharmacy Laws, Medicare, Medicaid and Business Management: Copy Right Protectedasas100% (1)
- @ Drug Antibiotics AntifungalDocument57 pages@ Drug Antibiotics AntifungalDr. Anil Virani SurgeonNo ratings yet
- Pedia Stickers PDFDocument8 pagesPedia Stickers PDFAshNo ratings yet
- OTC Exam 2 Study GuideDocument32 pagesOTC Exam 2 Study GuideDave WinNo ratings yet
- All Other ClassificationsDocument6 pagesAll Other ClassificationsCorey100% (1)
- IV PO Conversion CAPDocument3 pagesIV PO Conversion CAPdamondouglasNo ratings yet
- Brand Generic Class Other: NAPLEX ReviewDocument72 pagesBrand Generic Class Other: NAPLEX Reviewbapimirab654No ratings yet
- Over The Counter Drug ListDocument5 pagesOver The Counter Drug Listpradip_26No ratings yet
- Infectious Diseases IDocument7 pagesInfectious Diseases ITiff VoNo ratings yet
- Top 200 Drug ExamDocument1 pageTop 200 Drug ExamUyen V. NguyenNo ratings yet
- RX Cheat Sheet Pharmacy CrackDocument1 pageRX Cheat Sheet Pharmacy Crackramesh kumar100% (1)
- Drug of Choice and First Line of TreatmentDocument2 pagesDrug of Choice and First Line of Treatmentprinz1mendezNo ratings yet
- Chapter 35 AsthmaDocument4 pagesChapter 35 AsthmaDrashtibahen PatelNo ratings yet
- RxprepDocument1 pageRxprepSandeep KannegantiNo ratings yet
- Top Drugs: 1. ACETAMINOPHEN (Tylenol)Document12 pagesTop Drugs: 1. ACETAMINOPHEN (Tylenol)epingNo ratings yet
- Math Formulas For NAPLEX CalculationsDocument1 pageMath Formulas For NAPLEX CalculationsNasru DiinNo ratings yet
- Antipsychotics Factsheet pg2Document1 pageAntipsychotics Factsheet pg2JUSASBNo ratings yet
- Comprehensive Pharmacology SummaryDocument25 pagesComprehensive Pharmacology Summarysubash p100% (1)
- Naplex StudyDocument1 pageNaplex StudyMaxwell Bentley LeeNo ratings yet
- Study GuideDocument6 pagesStudy GuideFidelis MusicGroupNo ratings yet
- Insulin Chart: Insulin Type Onset of Action Peak Duration of ActionDocument1 pageInsulin Chart: Insulin Type Onset of Action Peak Duration of ActionGeorge ZachariahNo ratings yet
- Brad Hinton CVDocument6 pagesBrad Hinton CVapi-486072801No ratings yet
- Chapter 28 Infections: Perioperative Antimicrobial PPXDocument10 pagesChapter 28 Infections: Perioperative Antimicrobial PPXDrashtibahen PatelNo ratings yet
- Confused Drug Names-IsMPDocument9 pagesConfused Drug Names-IsMPPria Utama100% (1)
- Pharmacy Law Final Exam ReviewDocument3 pagesPharmacy Law Final Exam Reviewtiffanievo05100% (1)
- OtcDocument9 pagesOtcChrissie100% (1)
- Hypertension Drugs Cheat Sheet: by ViaDocument3 pagesHypertension Drugs Cheat Sheet: by ViaGulzaib KhokharNo ratings yet
- Know Common Disease ManagementDocument14 pagesKnow Common Disease Managementcdx25No ratings yet
- Drug TerminologyDocument5 pagesDrug Terminologyimdaking123No ratings yet
- 2017 Comprehensive ReviewDocument26 pages2017 Comprehensive Reviewapi-364961432100% (2)
- TPN CalculationDocument3 pagesTPN CalculationSARANYANo ratings yet
- Pharm Drug ListDocument17 pagesPharm Drug Listanon_523534678No ratings yet
- What 2 StudyDocument2 pagesWhat 2 StudyWil Lester100% (1)
- NAPLEXDocument1 pageNAPLEXbaniyo100% (1)
- Drug Side EffectsDocument2 pagesDrug Side EffectsAngelic khanNo ratings yet
- Naplex 1Document7 pagesNaplex 1baniyoNo ratings yet
- Apc0271 V4 PDFDocument53 pagesApc0271 V4 PDFDrAnisha PatelNo ratings yet
- Naplex - Math FormulasDocument1 pageNaplex - Math FormulasbooseeyNo ratings yet
- NJ Mpje PDFDocument168 pagesNJ Mpje PDFPatrick Mata100% (3)
- PK Equations To Know For NaplexDocument1 pagePK Equations To Know For NaplexNasru DiinNo ratings yet
- Pharmacist ChartDocument17 pagesPharmacist Chartrajnar1962100% (1)
- 2017 April Exam CompilationDocument8 pages2017 April Exam CompilationabbasyaqobiNo ratings yet
- Quizlet PractiDocument21 pagesQuizlet Practitohomas100% (1)
- Pharmacology Drug ChartDocument50 pagesPharmacology Drug ChartEssentialForLivingNo ratings yet
- Multistate Pharmacy Jurisprudence Examination (MPJE) Study GuideDocument20 pagesMultistate Pharmacy Jurisprudence Examination (MPJE) Study GuideMcRee Learning Center100% (2)
- Antibiotic PrescribingDocument1 pageAntibiotic PrescribingJay KayNo ratings yet
- Comprehensive - Pharmacy Review For NAPLEX Practice Exams Cases and Test Prep.8thDocument63 pagesComprehensive - Pharmacy Review For NAPLEX Practice Exams Cases and Test Prep.8thRabie YahfoufiNo ratings yet
- MULTISTATE PHARMACY JURISPRUDENCE EXAMINATION (MPJE): Passbooks Study GuideFrom EverandMULTISTATE PHARMACY JURISPRUDENCE EXAMINATION (MPJE): Passbooks Study GuideNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Vitamin Toxicities: NeonatalDocument29 pagesVitamin Toxicities: NeonatalfarazNo ratings yet
- Preview of Pharmacist OSCE Review BookDocument45 pagesPreview of Pharmacist OSCE Review BookChrissie100% (3)
- Pharmacy CounsellingDocument8 pagesPharmacy CounsellingChrissieNo ratings yet
- Practice Osce Scenarios PDFDocument20 pagesPractice Osce Scenarios PDFa1docNo ratings yet
- OtcDocument9 pagesOtcChrissie100% (1)
- Pharmacy Service AgreementDocument164 pagesPharmacy Service AgreementChrissieNo ratings yet
- Look Under Drugs Affecting Nutritional and Metbolic FunctionDocument1 pageLook Under Drugs Affecting Nutritional and Metbolic FunctionChrissieNo ratings yet
- Drug InteractionDocument1 pageDrug InteractionChrissieNo ratings yet
- Writing Task 1Document9 pagesWriting Task 1ChrissieNo ratings yet
- Glyceryltrinitrate: Cardiovascular PharmacologyDocument1 pageGlyceryltrinitrate: Cardiovascular PharmacologyChrissieNo ratings yet
- Processing PrescriptionsDocument24 pagesProcessing PrescriptionsChrissieNo ratings yet
- MdsMgtModule Calculations FinalDocument35 pagesMdsMgtModule Calculations FinalChrissieNo ratings yet
- Differentiating Language Difference and Language Disorder - Information For Teachers Working With English Language Learners in The Schools PDFDocument23 pagesDifferentiating Language Difference and Language Disorder - Information For Teachers Working With English Language Learners in The Schools PDFIqra HassanNo ratings yet
- This Study Resource Was: MCV4U Exam ReviewDocument9 pagesThis Study Resource Was: MCV4U Exam ReviewNathan WaltonNo ratings yet
- Jo - Mc.Donough. ESP in Perspective A Practical Guide. London. Collin ELT. 1984. p.3Document6 pagesJo - Mc.Donough. ESP in Perspective A Practical Guide. London. Collin ELT. 1984. p.3Falihatul Kholidiyah100% (1)
- Device InfoDocument3 pagesDevice InfoGrig TeoNo ratings yet
- Ielts Reading Actual Tests With Suggested Answers Oct 2021 JDocument508 pagesIelts Reading Actual Tests With Suggested Answers Oct 2021 JHarpreet Singh JohalNo ratings yet
- GTAG-14 Edited With Ad 05-20-20101 PDFDocument32 pagesGTAG-14 Edited With Ad 05-20-20101 PDFpiornelNo ratings yet
- Month Puzzle Two VariableDocument6 pagesMonth Puzzle Two VariableNayan KaithwasNo ratings yet
- Lecture Planner - Chemistry - MANZIL For JEE 2024Document1 pageLecture Planner - Chemistry - MANZIL For JEE 2024Rishi NairNo ratings yet
- Bach Polonaise G Min BWV 119 A4Document1 pageBach Polonaise G Min BWV 119 A4vincenzovaiaNo ratings yet
- CIT 811 TMA 4 Quiz QuestionDocument3 pagesCIT 811 TMA 4 Quiz QuestionjohnNo ratings yet
- Structural Engineering Formulas Second EditionDocument224 pagesStructural Engineering Formulas Second Editionahmed_60709595194% (33)
- Cisco Nexus 7000 Introduction To NX-OS Lab GuideDocument38 pagesCisco Nexus 7000 Introduction To NX-OS Lab Guiderazzzzzzzzzzz100% (1)
- 2 TolentinoDocument12 pages2 TolentinoMA. ANGELINE GRANADANo ratings yet
- ADAPT-Builder 2019 GUI Quick Reference GuideDocument103 pagesADAPT-Builder 2019 GUI Quick Reference GuideephremNo ratings yet
- Ericsson AXE 810: Switch (ROTD)Document4 pagesEricsson AXE 810: Switch (ROTD)Kao Sun HoNo ratings yet
- Manual Daily Calorie Log: MyfitnesspalDocument4 pagesManual Daily Calorie Log: MyfitnesspalAzariah Burnside100% (2)
- STRESS HealthDocument40 pagesSTRESS HealthHajra KhanNo ratings yet
- Solow 5e Web SolutionsDocument58 pagesSolow 5e Web SolutionsOscar VelezNo ratings yet
- Week 1 Macro (DDR)Document49 pagesWeek 1 Macro (DDR)Stevie Sean100% (1)
- Dell Inspiron 5547 15Document7 pagesDell Inspiron 5547 15Kiti HowaitoNo ratings yet
- Algorithm Design: Figure 1. Architecture Diagram For Greykite Library's Main Forecasting Algorithm, SilverkiteDocument3 pagesAlgorithm Design: Figure 1. Architecture Diagram For Greykite Library's Main Forecasting Algorithm, Silverkitesiper34606No ratings yet
- 2 MercaptoEthanolDocument8 pages2 MercaptoEthanolMuhamad ZakyNo ratings yet
- MODULE 1 - Contemporary WorldDocument4 pagesMODULE 1 - Contemporary WorldaapNo ratings yet
- Soal PTS Vii BigDocument6 pagesSoal PTS Vii Bigdimas awe100% (1)
- KRPL Shahjahanpur Check List For Arc Welding MachineDocument1 pageKRPL Shahjahanpur Check List For Arc Welding MachineA S YadavNo ratings yet
- Liquid Process Piping - Part 1 General Piping Design PDFDocument33 pagesLiquid Process Piping - Part 1 General Piping Design PDFnitin guptaNo ratings yet
- Introduction of Woman Role in SocietyDocument12 pagesIntroduction of Woman Role in SocietyApple DogNo ratings yet
- English Lesson Plan Form 4 (Literature: "The Living Photograph")Document2 pagesEnglish Lesson Plan Form 4 (Literature: "The Living Photograph")Maisarah Mohamad100% (3)
- Test Bank Bank For Advanced Accounting 1 E by Bline 382235889 Test Bank Bank For Advanced Accounting 1 E by BlineDocument31 pagesTest Bank Bank For Advanced Accounting 1 E by Bline 382235889 Test Bank Bank For Advanced Accounting 1 E by BlineDe GuzmanNo ratings yet
- 32 Forms of God GaneshaDocument16 pages32 Forms of God Ganeshasudhakarpk2011100% (2)