Professional Documents
Culture Documents
How To Get Your Cholesterol Tested
Uploaded by
m_pergastegui_mOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
How To Get Your Cholesterol Tested
Uploaded by
m_pergastegui_mCopyright:
Available Formats
How To Get Your Cholesterol Tested
Cholesterol plays a major role in a person's heart health. High blood cholesterol is a major
risk factor for coronary heart disease and stroke. That's why it's important for all people to
know their cholesterol levels. They should also learn about their other risk factors for heart
disease and stroke.
How is cholesterol tested?
A small sample of blood will be drawn from your arm. If your doctor has ordered other
tests to be run at the same time as your cholesterol test, all the samples will usually be taken
at the same time. Your blood sample is then analyzed by a laboratory.
Your doctor will tell you if you should fast (avoid consuming food, beverages and
medications, usually for nine to 12 hours) before your blood test. If you aren't fasting when
the blood sample is drawn, only the values for total cholesterol and HDL cholesterol will be
usable. That's because the amount of LDL (bad) cholesterol level and triglycerides can be
affected by what you've recently consumed.
Your test report will show your cholesterol level in milligrams per deciliter of blood
(mg/dL). Your doctor must interpret your cholesterol numbers based on other risk factors
such as age, family history, smoking and high blood pressure.
Your LDL (bad) cholesterol levels will be needed to determine your treatment plan if your
total cholesterol is 200 mg/dL or greater, or if your HDL is less than 40 mg/dL. If you
weren't fasting for your first test, your doctor may need to send you for another test.
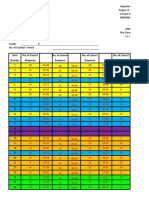
What do your cholesterol levels mean?m
How often should I have my cholesterol checked?
The American Heart Association endorses the National Cholesterol Education Program
(NCEP) guidelines for detection of high cholesterol: All adults age 20 or older should have
a fasting lipoprotein profile which measures total cholesterol, LDL (bad) cholesterol,
HDL (good) cholesterol and triglycerides once every five years. The Third Report of the
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults
(Adult Treatment Panel III or ATP III) was released in 2001. It recommends that everyone
age 20 and older have a fasting "lipoprotein profile" every five years. This test is done after
a 912-hour fast without food, liquids or pills. It gives information about total cholesterol,
LDL cholesterol, HDL cholesterol and triglycerides.
You may need to have your cholesterol checked more often than every five years if one or
more of these situations applies to you:
Your total cholesterol is 200 mg/dL or more.
You are a man over age 45 or a woman over age 50.
Your HDL (good) cholesterol is less than 40 mg/dL.
You have other risk factors for heart disease and stroke.
If a fasting lipoprotein profile isn't possible, the values for total cholesterol and HDL
cholesterol are still useful. If your total cholesterol is 200 mg/dL or more, or your HDL
cholesterol is less than 40 mg/dL (for men) or less than 50 mg/dL (for women), you need to
have a follow-up lipoprotein profile done to determine your LDL cholesterol and
triglyceride levels. Your healthcare provider will set appropriate management goals based
on your LDL cholesterol level and your other risk factors. See What Your Cholesterol
Levels Mean for information on what your levels should be.
Where should I have my cholesterol checked?
It's best to have your regular doctor run your cholesterol test. Overall risk factors such as
your age, family history, smoking history and high blood pressure must be considered when
interpreting your results and your regular doctor is most likely to have all that
information. Once you know your numbers, your doctor should recommend a treatment and
prevention plan, as well as follow-up testing to make sure the plan is getting you to your
cholesterol goals.
If you're admitted to the hospital for a major coronary event, your LDL cholesterol should
be measured on admission or within 24 hours. However, it may take four to six weeks
before your fasting lipid profile stabilizes and you can get accurate results. Your doctor will
determine whether to start drug treatment at discharge.
If you have your cholesterol checked at public screenings, make sure a reputable company
does the screening. Remember that your cholesterol level is just part of your overall
cardiovascular risk profile, and your other risk factors must be considered. You should
share the screening results with your healthcare professional so your tests can be properly
interpreted, and an appropriate treatment and prevention plan developed.
Be sure to review your test results with your doctor so you can understand and follow your
treatment plan.
The American Heart Association hasn't taken a position on cholesterol home testing
devices. Several devices are on the market. Some measure only total cholesterol. Others
measure total cholesterol and high-density lipoprotein (HDL) or "good" cholesterol. One
measures low-density lipoprotein (LDL) or "bad" cholesterol, HDL cholesterol and
triglycerides (blood fats).
This content was last reviewed on 12/10/2012.
A total cholesterol blood test is a blood test to check the cholesterol and triglyceride in the
blood. Total cholesterol testing is necessary to check the level of cholesterol in the blood.
This test is especially essential for anyone who is at a risk of getting heart disease or suffers
from heart disease. A total cholesterol home test is essential for anyone who believes in
remaining fit and wants to keep his cholesterol level under check.
Cholesterol
Cholesterol attaches itself to a protein and travels through blood. This package is known as
a lipoprotein. A Lipid profile test is done to check the level of total cholesterol,
triglycerides, HDL cholesterol, and LDL cholesterol.
Cholesterol - Cholesterol is used by the body to produce hormones and build cells.
Excess cholesterol in the blood can clog artery walls and form plaque. Too much of
plaque can increase the risk of heart disease.
HDL cholesterol - This is good cholesterol that binds with fat in the blood and helps
to remove it from the body.
LDL cholesterol - Known as 'bad cholesterol', LDL cholesterol can increase the risk
of heart disease.
VLDL - This lipoprotein distributes the triglyceride that is created by the liver.
Excessive VLDL can increase the chances of a stroke and heart disease.
Triglycerides - Triglycerides are fat that is stored in the body as energy.
Reasons Why It is Conducted
This is done to screen for a lipid disorder.
This test is done to check how a person is responding to treatment for lipid
disorders.
A test like this can determine if you are at a risk of getting heart disease.
This test might be done to screen for diseases that cause high cholesterol in people.
Preparation
You need to speak with your doctor about the preparations that you need to make for the
test. For a total cholesterol test, you can get the test done even if you've eaten a meal before
going in for the test.
For some of the other tests you may have to abstain from food and drink for nine to twelve
hours before the blood test. In general, it is advisable not to eat high-fat foods before you
go in for the test. Some medicines may affect the test results. You should not drink alcohol
before the test.
Procedure
The total cholesterol test is done by following a simple blood test procedure. The health
care expert will tie an elastic band around your upper arm and clean the area with alcohol,
before inserting a needle.
Lipid tests are routinely performed on plasma, which is the liquid part of blood without the
blood cells. Lipids themselves are a group of organic compounds that are greasy and cannot
be dissolved in water, although they can be dissolved in alcohol. Lipid tests include
measurements of total cholesterol, triglycerides, high-density lipoprotein (HDL)
cholesterol, and low-density lipoprotein (LDL) cholesterol. Lipid tests may also be
performed on amniotic fluid, which is the fluid that surrounds the fetus during pregnancy.
Prenatal lipid tests include tests for lecithin and other pulmonary (lung) surfactants that
cover the air spaces in the lungs with a thin film.
Purpose
Blood tests
The purpose of blood lipid testing is to determine whether abnormally high or low
concentrations of a specific lipid are present. Low levels of cholesterol are associated with
liver failure and inherited disorders of cholesterol production. Cholesterol is a primary
component of the plaques that form in atherosclerosis and is therefore the major risk factor
for the rapid progression of coronary artery disease (CAD). High blood cholesterol may be
inherited or result from such other conditions as biliary obstruction, diabetes mellitus,
hypothyroidism, and nephrotic syndrome. In addition, cholesterol levels may be increased
in persons who eat foods that are rich in saturated fats and cholesterol, and who lead a
sedentary lifestyle.
Low levels of triglyceride are seen in persons with malnutrition or malabsorption. Increased
levels are associated with diabetes mellitus, hypothyroidism, pancreatitis, glycogen storage
diseases, and estrogens. Diets rich in either carbohydrates or fats may cause elevated
triglyceride levels in some persons. Although triglycerides are not a component of the
plaque associated with atherosclerosis, they increase the viscosity (thickness) of the blood
and promote obesity, which can contribute to coronary disease. The majority of cholesterol
and triglyceride testing is performed to screen persons at increased risk of coronary artery
disease.
Amniotic fluid tests
Lipid tests are performed on amniotic fluid to determine the maturity of the fetal lungs.
These tests are performed prior to delivery to ensure that there is sufficient pulmonary
surfactant to prevent collapse of the lungs when the baby exhales (breathes out).
Description
Cholesterol screening can be performed with or without fasting, but it should include tests
of total and HDL cholesterol levels. The frequency of cholesterol testing depends on the
patient's risk of developing CAD. Adults over 20 with total cholesterol levels below 200
mg/dL should be tested once every five years. People with higher levels should be tested
for LDL cholesterol levels, and tested at least once per year thereafter if their LDL
cholesterol is 130 mg/dL or higher. The National Cholesterol Education Program (NCEP)
suggests further evaluation when the patient has any of the symptoms of CAD, or if she or
he has two or more of the following risk factors for CAD:
high blood pressure
history of cigarette smoking
diabetes
low HDL levels
family history of CAD
age over 45 years (men) or 55 years (women)
Measurements of cholesterol and triglyceride levels are routinely performed in all patients.
Measurement of pulmonary surfactants
Lecithin is the principal pulmonary surfactant secreted by the alveolar cells of the lung.
Lecithin and the other surfactants prevent collapse of the air sacs when the baby exhales.
During the first half of gestation, the levels of lecithin and another lipid known as
sphingomyelin in the amniotic fluid are approximately equal. During the second half of
pregnancy, however, lecithin production increases while the sphingomyelin level remains
constant. Infants born prematurely may suffer from respiratory distress syndrome (RDS)
because the levels of pulmonary surfactant in their lungs are insufficient to prevent collapse
of the air sacs. Tests for RDS are called fetal lung maturity (FLM) tests. The reference
method for determining fetal lung maturity is the ratio between lecithin and sphingomyelin
in the amniotic fluid, or the L/S ratio.
Precautions
Tests for triglycerides and LDL cholesterol must be performed following a 12-hour fast.
Acute illness, high fever, starvation, or recent surgery lowers the blood cholesterol and
triglyceride levels. If possible, patients should also stop taking any medications that may
affect the accuracy of the test.
Amniotic fluid is collected by a process called amniocentesis . This procedure is usually
performed after the 30th week of gestation to evaluate the maturity of the baby's lungs. A
miscarriage (spontaneous abortion) may occur as a consequence of this procedure, although
its overall incidence following amniocentesis is less than 1%. Possible complications of
amniocentesis include premature labor and placental bleeding. The fluid that is withdrawn
may be contaminated with blood or meconium (a dark-green material in the intestines of a
fetus), which may interfere with some fetal lung maturity tests.
Preparation
Patients who are scheduled for a lipid profile test should fast (except for water) for 12 to 14
hours before the blood sample is drawn. If the patient's LDL cholesterol is to be measured,
he or she should also avoid alcohol for 24 hours before the test. When possible, patients
should also stop taking any medications that may affect the accuracy of the test results.
These drugs include corticosteroids ; estrogen or androgens; oral contraceptives; some
diuretics ; antipsychotic medications, including haloperidol; some antibiotics ; and niacin.
Antilipemics are drugs that lower the concentration of fatty substances in the blood. When
these medications are taken by the patient, blood testing may be done frequently to evaluate
liver function as well as lipid levels.
Aftercare
Aftercare following blood lipid tests includes routine care of the skin around the needle
puncture. Most patients have no aftereffects, but some may have a small bruise or swelling.
A washcloth soaked in warm water usually relieves any discomfort. In addition, the patient
can resume taking any prescription medications that were discontinued before the test.
Care after amniocentesis requires that the clinician monitor the patient for any signs of
infection or possible injury to the fetus. Some things to look for are fever, vaginal bleeding,
or vaginal discharge. The patient may feel sick and there may be some cramping. She
should be advised to rest and avoid strenuous activity. If the mother appears to be going
into labor, she should be given supportive care. She may be given medications known as
tocolytic agents to prevent the premature birth of the baby.
Risks
The primary risk to the patient from blood tests of lipid levels is a mild stinging or burning
sensation during the venipuncture, with minor swelling or bruising afterward.
Although amniocentesis is much safer in the third trimester, and is less risky when it is
performed with the guidance of ultrasound technology, does present a risk of miscarriage
and fetal injury. The mother should be monitored for any signs of bleeding, infection, or
impending labor.
Results
The normal values for serum lipids depend on the patient's age, sex, and race. Normal
values for people in Western countries are usually given as 140220 mg/dL for total
cholesterol in adults, although as many as 5% of the population have a total cholesterol
higher than 300 mg/dL. Among Asians, the figures are about 20% lower. As a rule, both
total and LDL cholesterol levels rise as people get older. Normal values for HDL
cholesterol are also age- and sex-dependent. The range for males between 20 and 29 years
is approximately 3063 mg/dL; for females of the same age group it is 3383 mg/dL.
Normal values for fasting triglycerides are also age- and sex-dependent. The reference
range for adult males 20 to 29 years is 45200 mg/dL; for females of the same age group it
is 37144 mg/dL. As with cholesterol, the normal range rises with age.
Since a person's diet and lifestyle affect normal values, which are determined by the
interval between the 5th and 95th percentile of the group, it is more helpful to evaluate
cholesterol and triglycerides from the perspective of desirable plasma levels. The desirable
values defined by the Nation Cholesterol Education Program (NCEP) in 2001 are as
follows:
Total cholesterol: Less than 200 mg/dL; 200239 mg/dL is considered borderline
high and greater than 240 mg/dL is high.
HDL cholesterol: Less than 40mg/dL is low.
LDL cholesterol: Less than 100 mg/dL is optimal; near-optimal is 100129 mg/dL;
borderline high is 130-159 mg/dL; high is 160189 mg/dL; and very high is any
value over 190 mg/dL.
Total cholesterol: HDL ratio: Under 4.0 in males; 3.8 in females.
Fetal lung maturity tests
Low levels of surfactant in amniotic fluid are denoted by an L/S ratio lower than 2.0 or a
lecithin level lower than or equal to 0.10 mg/dL. Lung development can be delayed in
premature births and in babies whose mothers have diabetes.
Patient education
Nurses should explain the results of abnormal blood lipid tests to patients and advise them
on lifestyle changes. Patient education is important in fetal lung maturity testing. The
situation faced by the expectant parents may be very critical; the more information they are
given, the better choices they can make.
Resources
BOOKS
Henry, J. B. Clinical Diagnosis and Management by Laboratory Methods , 20th ed.
Philadelphia, PA: W. B. Saunders Company, 2001.
"Hyperlipidemia." Section 2, Chapter 15 in The Merck Manual of Diagnosis and Therapy ,
edited by Mark H. Beers, MD, and Robert Berkow, MD. Whitehouse Station, NJ: Merck
Research Laboratories, 1999.
"Prenatal Diagnostic Techniques: Amniocentesis." Section 18, Chapter 247 in The Merck
Manual of Diagnosis and Therapy , edited by Mark H. Beers, MD, and Robert Berkow,
MD. Whitehouse Station, NJ: Merck Research Laboratories, 1999.
Wallach, Jacques. Interpretation of Diagnostic Tests , 7th ed. Philadelphia, PA: Lippincott
Williams & Wilkens, 2000.
ORGANIZATIONS
American Dietetic Association. (800) 877-1600. http://www.eatright.org. .
National Cholesterol Education Program. National Heart, Lung, and Blood Institute
(NHLBI), National Institutes of Health. PO Box 30105, Bethesda, MD, 20824-0105. (301)
251-1222. May 2001 [cited April 4, 2003].
http://www.nhlbi.nih.gov/guidelines/cholesterol/atglance.pdf .
OTHER
National Institutes of Health. [cited April 5, 2003].
http://www.nlm.nih.gov/medlineplus/encyclopedia.html .
Jane E. Phillips
Mark A. Best
User Contributions:
Read more: http://www.surgeryencyclopedia.com/La-Pa/Lipid-Tests.html#ixzz30PLwylGx
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 4-Page 7 Ways TM 20Document4 pages4-Page 7 Ways TM 20Jose EstradaNo ratings yet
- Slides 99 Netslicing Georg Mayer 3gpp Network Slicing 04Document13 pagesSlides 99 Netslicing Georg Mayer 3gpp Network Slicing 04malli gaduNo ratings yet
- Seangio Vs ReyesDocument2 pagesSeangio Vs Reyespja_14No ratings yet
- 5g-core-guide-building-a-new-world Переход от лте к 5г английскийDocument13 pages5g-core-guide-building-a-new-world Переход от лте к 5г английскийmashaNo ratings yet
- Annual Report Aneka Tambang Antam 2015Document670 pagesAnnual Report Aneka Tambang Antam 2015Yustiar GunawanNo ratings yet
- Kipor Diesel Generator KDE23SS3 CatalogueDocument32 pagesKipor Diesel Generator KDE23SS3 CatalogueAbbasNo ratings yet
- Kutune ShirkaDocument11 pagesKutune ShirkaAnonymous CabWGmQwNo ratings yet
- Lifeline® Specialty: Fire Resistant QFCI Cable: Fire Resistant, Flame Retardant Halogen-Free Loose Tube - QFCI/O/RM-JMDocument2 pagesLifeline® Specialty: Fire Resistant QFCI Cable: Fire Resistant, Flame Retardant Halogen-Free Loose Tube - QFCI/O/RM-JMkevinwz1989No ratings yet
- Holophane Denver Elite Bollard - Spec Sheet - AUG2022Document3 pagesHolophane Denver Elite Bollard - Spec Sheet - AUG2022anamarieNo ratings yet
- English HL P1 Nov 2019Document12 pagesEnglish HL P1 Nov 2019Khathutshelo KharivheNo ratings yet
- Positive Accounting TheoryDocument47 pagesPositive Accounting TheoryAshraf Uz ZamanNo ratings yet
- Ahts Ulysse-Dp2Document2 pagesAhts Ulysse-Dp2IgorNo ratings yet
- The Eaglet - Vol. 31, No. 3 - September 2019Document8 pagesThe Eaglet - Vol. 31, No. 3 - September 2019Rebecca LovettNo ratings yet
- A - Persuasive TextDocument15 pagesA - Persuasive TextMA. MERCELITA LABUYONo ratings yet
- National Rural Employment Guarantee Act, 2005Document17 pagesNational Rural Employment Guarantee Act, 2005praharshithaNo ratings yet
- Zoonotic Diseases From HorsesDocument12 pagesZoonotic Diseases From HorsesSandra Ximena Herreño MikánNo ratings yet
- ICTSAS601 Student Assessment Tasks 2020Document30 pagesICTSAS601 Student Assessment Tasks 2020Lok SewaNo ratings yet
- Kolehiyo NG Lungsod NG Lipa: College of Teacher EducationDocument3 pagesKolehiyo NG Lungsod NG Lipa: College of Teacher EducationPrincess LopezNo ratings yet
- Item AnalysisDocument7 pagesItem AnalysisJeff LestinoNo ratings yet
- Sabbir 47MDocument25 pagesSabbir 47MMd.sabbir Hossen875No ratings yet
- Book Review On PandeymoniumDocument2 pagesBook Review On PandeymoniumJanhavi ThakkerNo ratings yet
- Applications of Tensor Functions in Solid MechanicsDocument303 pagesApplications of Tensor Functions in Solid Mechanicsking sunNo ratings yet
- Simplified Electronic Design of The Function : ARMTH Start & Stop SystemDocument6 pagesSimplified Electronic Design of The Function : ARMTH Start & Stop SystembadrNo ratings yet
- Dye-Sensitized Solar CellDocument7 pagesDye-Sensitized Solar CellFaez Ahammad MazumderNo ratings yet
- Thomas HobbesDocument3 pagesThomas HobbesatlizanNo ratings yet
- Damodaram Sanjivayya National Law University VisakhapatnamDocument6 pagesDamodaram Sanjivayya National Law University VisakhapatnamSuvedhya ReddyNo ratings yet
- Frbiblio PDFDocument16 pagesFrbiblio PDFreolox100% (1)
- Imc Case - Group 3Document5 pagesImc Case - Group 3Shubham Jakhmola100% (3)
- Qafqaz UniversityDocument3 pagesQafqaz UniversityQafqazlife QUNo ratings yet
- Img - Oriental Magic by Idries Shah ImageDocument119 pagesImg - Oriental Magic by Idries Shah ImageCarolos Strangeness Eaves100% (2)