Professional Documents
Culture Documents
Treatment Phase - Comprehensive Treatment Planning - 2 (Compatibility Mode)
Uploaded by
haneenee0 ratings0% found this document useful (0 votes)
34 views5 pagesTreatment_Phase-_Comprehensive_treatment_planning
Original Title
Treatment Phase- Comprehensive Treatment Planning -2 [Compatibility Mode]
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentTreatment_Phase-_Comprehensive_treatment_planning
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
34 views5 pagesTreatment Phase - Comprehensive Treatment Planning - 2 (Compatibility Mode)
Uploaded by
haneeneeTreatment_Phase-_Comprehensive_treatment_planning
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
111
Dr SUGHU MALAYIL KOSHY
BDS,MSc (Comm.Dent),DDPH RCS(England)
Patient recall guidelines &
Treatment Phase-
Comprehensive Treatment
planning -2
Recall intervals for scale and polish treatments
the prescription and timing of dental radiographs
Intervals between examinations that are not routine dental
recall, that is intervals between examinations relating to
ongoing courses of treatment
Emergency dental interventions or intervals between
episodes of specialist care
DENTAL RECALL GUIDELINES: Nice guideline UK ,
Clinical guideline 19,2004
This guideline does not cover:
The recommended interval between en oral health
reviews should be determined specifically for each patient
and tailored to meet his or her needs, on the basis of an
assessment of disease levels and risk of or from dental
disease.
This assessment should integrate the evidence presented in
this guideline with the clinical judgement and expertise of the
dental team, and should be discussed with the patient.
During an oral health review, the dental team (led by
the dentist) should ensure that comprehensive histories
are taken, examinations are conducted and initial
preventive advice is given.
This will allow the dental team and the patient (and/or
his or her parent, guardian or carer to discuss,where
appropriate:
The effects of oral hygiene, diet, fluoride use, tobacco and
alcohol on oral health
The risk factors that may influence the patients oral health,
and their implications for deciding the appropriate recall interval
The outcome of previous care episodes and the suitability of
previously recommended intervals
The patients ability or desire to visit the dentist at the
recommended interval
The financial costs to the patient of having the oral health
review and any subsequent treatments
The interval before the next oral health review should be
chosen, either at the end of an oral health review if no further
treatment is indicated, or on completion of a specific treatment
journey.
The recommended shortest and longest intervals between
oral health reviews are as follows:
The shortest interval between oral health reviews for all
patients should be 3 months.
The longest interval between oral health reviews for patients
younger than 18 years should be 12 months.
The longest interval between oral health reviews for patients
aged 18 years & older should be 24 months
For practical reasons, the patient should be assigned a
recall interval of 3, 6, 9 or 12 months if he or she is younger
than 18 years old, or 3, 6, 9, 12, 15,18, 21 or 24 months if he
or she is aged 18 years or older.
The dentist should discuss the recommended recall interval
with the patient and record this interval, and the patients
agreement or disagreement with it, in the current record-
keeping system.
The recall interval should be reviewed again at the next oral
health review, to learn from the patients responses to the oral
care provided and the health outcomes achieved.
This feedback and the findings of the oral health review
should be used to adjust the next recall interval chosen.
Patients should be informed that their recommended call
interval may vary over time.
222
RESTORATIVE TREATMENT:
Initial treatment:
Control etiology: Eg:Dental Caries
Advice on diet
Oral hygeine
Use of Fluorides
Oral prophylaxis
Dietary advice:
Should be personal, practical & positive
Adopt less cariogenic diet
- Eat less sugar & eat sugar less often
Reduce consumption of sugars & fats
Increase consumption of fiber rich starchy foods.
Fresh fruit & vegetables
Meals provide a better nutritional balance than
snacks, hence good eating/slash drinking at meal
times avoiding between meal snacking is healthy
Use of intense sweeteners Eg: Saccharin & aspartime are
non cariogenic, but to be used with caution due to the effect
on the gastrointestinal system.
Chewing gums- sugar free chewing gums (Xylitlol)
simulates saliva & thus increases salivary buffers & enhances
wash out of sugar.
Carbonated beverage have a 2-3 PH & can cause marked
loss of tooth structure via erosion.
Detersive food stuffs like carrots & apples etc. are of little or
benefit in removal of plaque
Effective plaque removal is dependent on tooth brushing
only
Diet & Dental caries:
Pre-requsite for dental caries is a carbohydrate form that can
be metobolised by oral bacteria.
Classification of sugars:
Intrinsic sugars: Sugars forming an integral part of certain
unprocessed food stuffs.
Called intrinsic because they are enclosed within a cell
Found in whole fruits & vegetable, mainly as fructose, sucrose
& glucose.
Contd.
Extrinsic Sugars:
Found in food outside the cellular structure
Further classifies as:
Milk extrinsic sugars- In milk & milk containing
products mainly lactose. This is of low cariogenicity
Non Milk extrinsic sugars: found in confectioneries,
soft drinks, biscuits & cakes. Includes sucrose, fructose
& glucose. These have the greatest cariogenic potential
Factors influencing the cariogenicity of food:
Consistency: Sticky retensive foods are more cariogenic than
liquid non retensive forms
Frequency of consumption: Snacking or grazing results in
lower PH, where net outflow of calcium & phosphate ions from
tooth surface occurs from prolonged period of time.
333
Oral Hygeine Refer Previous lecture on oral hygeine &
plaque control:
Fluorides:
Series of systematic reviews published by the cochrane
library have concluded that children who brush their teeth at
least one a day with fluoridated tooth paste will have less tooth
decay.
Has a caries prevention action when delivered in vehicles
other than tooth paste also.
Fluoride Mode of action
Systemic Pre-eruptive effect:
Fluoride ions are incorporated into the enamel structure in the
form of fluor appetite during the period of tooth formation
Topical -post eruptive effect:
Fluoride is either incorporated into the crystal lattice or by
binding to crystal surface.
Calcium Fluoride at the tooth surface not only reduces the
solubility of the appetite but also encourages re-mineralisation
Fluoride causes decrease acid production by cariogenic
bacteria
Topical effect at the tooth surface, post eruption is more
effective than systemic effect
Pain history:
Essential in diagnosing pulpal pain
Pain quality :
Sharpness - Sharp pain can indicate, exposed dentinal
tubules & fractured cusp
Dullness - May indicate pulpal hyperemia
Throbbing pain Particularly if constant may indicate an
irreversible pulpitis
Duration:
Short pain- Few seconds, can indicate reversible pulpitis but
may also indicate pain of non dental origin.
Eg: Trigeminal neuralgia
Constant pain- Often indicates irreversible pulpitis or one of its
sequelae
Stimuli:
Reaction to heat Irreversible pulpitis reacts to heat but not
cold
Reaction to cold - Reversible pulpitis
Reaction to pressure- May indicate periapical or periodontal
abcess.
Release of pressure- may indicate a cracked cusp
Reaction to sweet stimuli- Reversible pulpitis or exposed
dentin
Time of Pain:
Pain pattern day & night is important.
Pulpal pain is often worse at night
Conclusion:
A pain history gives the dentist a guide as to the source
of pulpal pain.
It does not produce a diagnosis on its own
444
Site & radiation:
History indicates primary site of pain & where it
radiates.
Pain in teeth adjacent to the tooth the patient
suspect as the cause of pain or the opposing arch is
common.
Referred pain from non dental causes- Eg:
Sinusitis
Pain localisation in difficult in low grade reversible
pulpitis & in children
Pulpal Diseases:
Reversible pulpitis:
Symptoms:
Pain of short duration as response to Hot, cold & sweet
Relieved by analgesics
Poor pain localisation
Irreversible pulpitis:
Pain of long duration
Throbbing, dull in nature
Worse with hot stimuli
Better localisation of pain
Not always relieved by analgesics
Periapical periodontitis:
Symptoms:
Dull, throbbing constant pain
Frequently keeps patient awake
Can localize pain to particular tooth
Tender to chew
Poor relief from analgesics
Stabilisation Phase:
Extract unrestorable teeth
Restore by simple means- Intra coronal
restorations. Amalgam composite restorations etc.
Simple endodontic treatment to key teeth
Stablisation phase restore by simple means
Removal of carious tissue
Minimize pulpal and /or periodontal damage
Cavity should be prepared such that the restorative
material to be used can restore function & appearance of the
tooth, & is retained in the tooth
Fundamental guiding principle of cavity preparation, is that
the preparation should only be as large as the carious lesion.
However follow the basic steps in the preparation of
cavities, like outline form, resistance & retension form,
management of remaining caries, enamel margin finishing &
cavity toilet.
Simple endodontic treatment for offending tooth:
Indirect pulp capping- Should be used for all cavities
where it is considered there may be a micro exposure or
where removing further remnants of caries is likely to cause
classic pulpal exposure
A layer of Calcium hydroxide (setting) is placed over the
dentine closest to the micro exposure. This is reinforced by a
structural lining.
555
2. Direct Pulp capping:
An exposed vital pulp may be pulp capped. This is
less sucessful than indirect pulp capping but most likely
to succeed in circumstances where:
pulpal exposure is small (less than 1-2 mm)
pulp is free of salivary contamination
carious exposure is not present
tooth was symptom free prior to cavity preparation
Patient is young (Better pulpal blood supply)
Reassess Response to treatment
Assess patients motivation
Oral hygiene
Diet
Reasess problem teeth
Reasess treatment plan in poorly motivated patient,
complex treatment will inevitably fail due to poor oral
hygeine
In some patients no further treatment is required
Definitive treatment:
Premolar Molar Endodontic treatment
Endodontic retreatment
Post-core restorations
Crown & Bridge
Removable prosthesis
Implants
CONCLUSION:
In the formulation & carrying out of treatment:
Keep treatment as simple as possible
Construct treatment plan where there is scope to
reassess & change plan
Know your own professional limitations
Know your patients limitations
When planning restorative treatment, the dentist
should take into account not just the teeth but the
individual patients total oral health & general health
needs
29
You might also like
- Emergency Equipment ChecklistDocument1 pageEmergency Equipment Checklisthaneenee100% (1)
- Behavioural Management in Children (Compatibility Mode)Document25 pagesBehavioural Management in Children (Compatibility Mode)haneeneeNo ratings yet
- 5.respiratory Distress Dental LectureDocument40 pages5.respiratory Distress Dental LecturehaneeneeNo ratings yet
- Areatha ResumeDocument2 pagesAreatha ResumehaneeneeNo ratings yet
- AhmadDocument3 pagesAhmadhaneeneeNo ratings yet
- Stainless Steel Crowns (SSCS)Document24 pagesStainless Steel Crowns (SSCS)haneenee0% (1)
- Ahmad 2Document6 pagesAhmad 2haneeneeNo ratings yet
- SurgeryDocument1 pageSurgeryhaneeneeNo ratings yet
- Rich Text Editor FileDocument1 pageRich Text Editor FilehaneeneeNo ratings yet
- 341PDSDocument12 pages341PDShaneeneeNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Profiles of Leading Neuro-OphthalmologistsDocument18 pagesProfiles of Leading Neuro-OphthalmologistsfaqihalifNo ratings yet
- Paper Cervical LenghtDocument30 pagesPaper Cervical LenghtDanTe D' WinchesterNo ratings yet
- The Word "Reiki" Means "Mysterious Atmosphere, Miraculous Sign." It Comes From The Japanese Words "Rei" (Universal) and Ki" (Life Energy)Document3 pagesThe Word "Reiki" Means "Mysterious Atmosphere, Miraculous Sign." It Comes From The Japanese Words "Rei" (Universal) and Ki" (Life Energy)Đặng Ngọc ThạchNo ratings yet
- CPM16TH Essential Newborn CareDocument11 pagesCPM16TH Essential Newborn CareKevin AgbonesNo ratings yet
- Anidula VS FluconDocument11 pagesAnidula VS FluconHarsha KuriNo ratings yet
- An Assessment of Knowledge On Newborn Care Practices Among Hospital Delivered Postnatal MothersDocument66 pagesAn Assessment of Knowledge On Newborn Care Practices Among Hospital Delivered Postnatal MothersAdersh Nair90% (21)
- PS01619 PDFDocument8 pagesPS01619 PDFEvelinaNo ratings yet
- RESPONDER Nitrile Exam GlovesDocument6 pagesRESPONDER Nitrile Exam Glovessandakelum AsankaNo ratings yet
- Policy and Procedure Manual: Diagnostic Services - Department of Radiology - Diagnostic DivisionDocument5 pagesPolicy and Procedure Manual: Diagnostic Services - Department of Radiology - Diagnostic DivisionFriends ForeverNo ratings yet
- HATADocument28 pagesHATAshyamchepurNo ratings yet
- Cardiac Arrest Circular AlgorithmDocument6 pagesCardiac Arrest Circular Algorithmno_spam_mang80% (5)
- Mei Penyakit UmumDocument1 pageMei Penyakit Umumghaniangga11No ratings yet
- AIIMS Case Study: India's Premier Medical InstituteDocument12 pagesAIIMS Case Study: India's Premier Medical InstituteShivangi SwarnkarNo ratings yet
- Orig 1 S 000 Other RDocument63 pagesOrig 1 S 000 Other RAsaad iqbalNo ratings yet
- BWC FAQs - Mental Health Policy - 170820Document6 pagesBWC FAQs - Mental Health Policy - 170820Jeremiah CarlosNo ratings yet
- Sympathetic OphthalmiaDocument4 pagesSympathetic Ophthalmiatiara_kusumaningtyasNo ratings yet
- Food Poisoning Final Print!Document3 pagesFood Poisoning Final Print!Joeven HilarioNo ratings yet
- Instructions For The COVID-19 Vaccination - ModernaDocument2 pagesInstructions For The COVID-19 Vaccination - ModernaMarc LiNo ratings yet
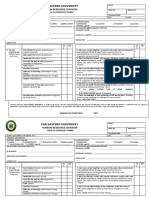
- City Health Services IPCR Performance ReviewDocument8 pagesCity Health Services IPCR Performance ReviewLiecel Valdez100% (2)
- USMLE Step 1 GuideDocument3 pagesUSMLE Step 1 GuideSofieNo ratings yet
- PRCDocument10 pagesPRCKatie TenebroNo ratings yet
- 4'Rs of Radiobiology: Nilesh Kumar PG Radiation Physics Deapartment of Radiation PhysicsDocument23 pages4'Rs of Radiobiology: Nilesh Kumar PG Radiation Physics Deapartment of Radiation Physicsnilesh kumarNo ratings yet
- Overview of The Mucopolysaccharidoses: RheumatologyDocument9 pagesOverview of The Mucopolysaccharidoses: RheumatologyLaura Orjuela MateusNo ratings yet
- SellersPaulineM 2018 SectionOneMaternalAnd SellersMidwiferyDocument1 pageSellersPaulineM 2018 SectionOneMaternalAnd SellersMidwiferyQedeniNo ratings yet
- Group 1 Members List for Politeknik Bhakti Asih PurwakartaDocument22 pagesGroup 1 Members List for Politeknik Bhakti Asih PurwakartateguhNo ratings yet
- MVP Silver Summary of Benefits and CoverageDocument6 pagesMVP Silver Summary of Benefits and Coverageksenos.ukNo ratings yet
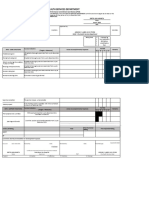
- FEU Health Checklist FormDocument2 pagesFEU Health Checklist FormDavid Antonio A. EscuetaNo ratings yet
- Expert review on soft-tissue plasmacytomas in multiple myeloma: definition, disease assessment and treatment considerationsDocument12 pagesExpert review on soft-tissue plasmacytomas in multiple myeloma: definition, disease assessment and treatment considerationsCeci AndradeNo ratings yet
- Care of The Chronically Ill and The Older PersonDocument8 pagesCare of The Chronically Ill and The Older PersonAnne Con100% (1)
- Claim Form - Group Health InsuranceDocument5 pagesClaim Form - Group Health Insurancevizag mdindiaNo ratings yet