Professional Documents
Culture Documents
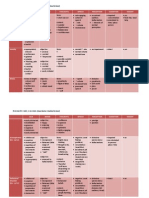
DSM 5 Chart
Uploaded by
Jose Luis Gonzalez Celis100%(1)100% found this document useful (1 vote)
795 views7 pagesDSM-5 diagnostic criteria do not reflect significance of language content and form. Diagnostic features indicate that nonverbal communication should be assessed "relative to cultural norms" individual will be given a diagnosis of "autism spectrum disorder" with three levels of severity.
Original Description:
Original Title
DSM-5-Chart
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDSM-5 diagnostic criteria do not reflect significance of language content and form. Diagnostic features indicate that nonverbal communication should be assessed "relative to cultural norms" individual will be given a diagnosis of "autism spectrum disorder" with three levels of severity.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
100%(1)100% found this document useful (1 vote)
795 views7 pagesDSM 5 Chart
Uploaded by
Jose Luis Gonzalez CelisDSM-5 diagnostic criteria do not reflect significance of language content and form. Diagnostic features indicate that nonverbal communication should be assessed "relative to cultural norms" individual will be given a diagnosis of "autism spectrum disorder" with three levels of severity.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 7
DSM-5
(Criteria and Major Changes for SLP-Related
Conditions)
ASHA Comments*
(ASHA Recommendations Compared to
DSM-5 Criteria)
Potential Practice Implications
Austism Spectrum Disorder (ASD)
Individuals meeting the criteria will be given a
diagnosis of autism spectrum disorder with
three levels of severity based on degree of
support needed.
Diagnostic criteria include deficits in social
communication and social interaction; and
restricted, repetitive patterns of behavior,
interest or activities, which cause significant
impairments in daily functioning.
Eliminates pervasive developmental disorder
and its subcategories (autistic disorder, Retts
disorder, childhood disintegrative disorder,
Aspergers disorder, pervasive developmental
disorder-not otherwise specified [PDD-NOS]).
Rett syndrome, a genetic disorder, is not
included in DSM-5, although girls with Rett
syndrome often have ASD symptoms and may
be diagnosed with ASD if they meet the criteria.
Omits criterion related to delay in or lack of
development of spoken language. Rather, the
evaluator is to specify whether the ASD occurs
with or without accompanying language
impairment.
Changes the age of onset from prior to age 3
years in DSM-IV to symptoms present in the
early developmental period.
DSM-5 consolidated subcategories in ASD.
ASHA supported this change due to lack of
evidence for discrete categories.
ASHA recommended including disorders of
language content (semantics), form (phonology,
syntax) and use (pragmatics, social
communication) in the diagnostic criteria for
ASD. DSM-5 diagnostic criteria do not reflect
the significance of language content and form in
defining ASD. However, the severity specifiers
and diagnostic features capture language
deficits in more detail.
ASHA suggested that DSM-5 criteria indicate
that nonverbal communication behaviors vary
within and across cultures. Although the ASD
diagnostic criteria in DSM-5 do not mention
cultural variation, the diagnostic features, which
describe the criteria in greater detail, indicate
that nonverbal communication should be
assessed relative to cultural norms. Sections
detailing culture and gender-related diagnostic
issues also were added in DSM-5.
Under new DSM-5 criteria, individuals will
receive a diagnosis of ASD, rather than
previous subcategories. There is concern that
those who are higher functioning may not
receive an ASD diagnosis and may not get the
services they need.
Social (pragmatic) communication disorder is
a more appropriate diagnosis than ASD for a
client who has difficulties with social skills but
doesnt show restricted or repetitive patterns of
behavior. SLPs will be instrumental in making
this differential diagnosis.
Because the language component is
downplayed in the ASD criteria, SLPs will need
to advocate for the inclusion of language in
intervention plans for those with ASD.
SLPs will need to ensure that people with
ASD receive a comorbid diagnosis of language
disorder (a component of communication
disorders) when they meet the criteria for both
conditions.
There is a need to ensure that services arent
limited to those with higher severity levels.
The more descriptive and clear DSM-5
criteria for ASD may benefit children by
leading to earlier diagnosis and intervention.
Communication Disorders
Diagnostic categories for communication
disorders include Language Disorder,
Speech Sound Disorder, Childhood-Onset
Fluency Disorder (Stuttering), Social
(Pragmatic) Communication Disorder, and
Unspecified Communication Disorder. This
represents a change from the DSM-IV
categories of Expressive Language Disorder
and Mixed Receptive-Expressive Language
Disorder.
Language Disorder. The diagnostic criteria
for language disorder include persistent
difficulties in the acquisition and use of
language across modalities (i.e., spoken,
written, sign language, or other) due to deficits
in comprehension or production, language
abilities that are substantially and quantifiably
below age expectations.
Social (Pragmatic) Communication
Disorder. The diagnostic criteria for social
(pragmatic) communication disorder are
persistent difficulties in the social use of verbal
and nonverbal communication, which include
deficits in using communication for social
purposes , impairment in the ability to
change communication to match context or the
needs of the listener, difficulties following
rules for conversation and storytelling, and
difficulties understanding what is not explicitly
statedand nonliteral or ambiguous meaning of
language.
Speech Sound Disorder. The key diagnostic
criterion for speech sound disorder includes
persistent difficulty with speech sound
production that interferes with speech
intelligibility or prevents verbal communication
ASHA recommended including a statement that
a regional, social, or cultural or linguistic
variation (e.g., dialect) of language is not a
language disorder. DSM-5 indicates that
regional, social, or cultural/ethnic variations of
speech should be considered before making the
diagnosis. DSM-5 also states in the
introduction to this section that speech,
language, and communication assessments
must take into account the individuals cultural
and language context, particularly for
individuals growing up in bilingual
environments. Also indicated is that
standardized measures must be relevant for the
cultural and linguistic group.
ASHA did not recommend having a separate
category for social communication disorder.
ASHA indicated that difficulties in use of
language (e.g., impairments in discourse) were
already part of the criteria for a language
disorder. However, the criteria for Language
Disorder were reframed and were defined
primarily around vocabulary and grammar.
Social (Pragmatic) Communication Disorder
includes verbal and nonverbal communication
in a social context.
ASHA recommended indicating that speech
sound disorder may co-occur with a language
disorder. DSM-5 accepted this
recommendation.
ASHA asked that diagnostic criteria for
cluttering be added. However, cluttering is not
included.
ASHA recommended that motor speech
disorders, voice disorders and resonance
disorders not be included in DSM-5 because
It is essential that individuals with other
conditions, particularly ASD, specific learning
disorder, ADHD and intellectual disability, also
be diagnosed with a communication disorder
when they meet the diagnostic criteria for both.
SLPs will need to make sure to that individuals
with ASD be assessed for a language disorder.
Individuals with social (pragmatic)
communication disorder, however, cannot be
dually diagnosed as having ASD.
ASD must be ruled out before a diagnosis of
social (pragmatic) communication can be made.
SLPs will be key team players in making these
diagnoses.
Diagnosis of social communication, including
pragmatics, has been and will continue to be a
challenge, and we clearly need more research in
this area. Assessment needs to be contextually
based and involve multiple settings and
communication partners. Social communication
skills do not fit easily within a single
assessment tool. Multiple observations,
checklists, structured tasks, and assessment
measures are needed. Recognition of cultural
and linguistic variations is paramount,
particularly for this area of assessment.
Some may be concerned that individuals
diagnosed with social (pragmatic)
communication disorder may be given a lower
priority with respect to workload than
individuals diagnosed with ASD. However,
services should be based on need, not on
diagnostic labels or severity levels.
of messages.
Childhood-Onset Fluency Disorder
(Stuttering). The diagnostic criteria for
childhood-onset fluency disorder (stuttering) are
disturbances in the normal fluency and time
patterning of speech and the disturbance
causes anxiety about speaking.
The onset of symptoms for communication
disorders is in the early developmental
period. However, social communication
deficits may continue to unfold with increasing
social communication demands. Adult-onset
fluency disorders are not included in DSM-5.
they are physiological problems rather than
mental or developmental disorders. DSM-5
does not include these disorders.
ASHA suggested refraining from using
developmental in the description of
childhood-onset fluency disorder because this
disorder is not developmental in nature, but
rather is applicable to individuals whose
stuttering has an observed onset during
childhood. DSM-5 indicates that the onset of
symptoms is in the early developmental period
and indicates that childhood-onset fluency
disorder is also called developmental
stuttering, but does not use the term
developmental as a diagnostic criterion or in
the description of the diagnostic features.
Intellectual Disability (Intellectual Developmental Disorder)
Change in terminology from Mental
Retardation to Intellectual Disability
(Intellectual Developmental Disorder).
Diagnostic criteria include deficits in
intellectual functions confirmed by both
clinical assessment and individualized,
standardized intelligence testing and deficits
in adaptive functioning. This represents a
move away from a specific IQ level and
expands the role of clinical assessment.
Onset is in the developmental period. In
DSM-IV, onset was indicated as before 18
years.
DSM-IV had distinct classifications of mild,
ASHA supported the change from Mental
Retardation to Intellectual Disability.
ASHA agreed with the need for alignment
with the American Association of
Intellectual and Developmental Disabilities
(AAIDD) terminology and other
professionals and consumers who use this
more contemporary terminology.
ASHA recommended the elimination of
classification by IQ and severity level.
ASHA recommended use of the AAIDD
definition, which characterizes intellectual
disability by significant limitations both in
intellectual functioning (reasoning,
learning, problem solving) and in adaptive
Individuals with intellectual disabilities
may have a co-occurring condition such as
communication disorder, specific learning
disorder, or ASD when all of the diagnostic
criteria are met. SLPs will play a pivotal
role in making these differential diagnoses.
SLPs will be critical members of a
diagnostic and intervention team to ensure
that individuals receive ongoing support,
AAC systems, and involvement of
communication partners.
More individuals may be diagnosed with
intellectual disability because the diagnosis
does not require a specific IQ score.
moderate, severe, and profound mental
retardation based on IQ level. DSM-5 has a
single category of intellectual disability rather
than divisions by severity level. There are
specifiers now for various levels of severity
that are defined by adaptive functioning
across conceptual, social, and practical
domains.
The category of Global Developmental
Delay may apply for children under the age
of 5 years when severity level cannot be
assessed reliably. Unspecified Intellectual
Disability (Intellectual Developmental
Disorder) is limited to individuals older than
5 years when assessment is difficult or
impossible due to associated sensory,
physical, or other conditions.
The need for assessment tools for intellectual
and adaptive functioning that are culturally
appropriate is mentioned in the section on
diagnostic features.
behaviors. (www.aaidd.org).
ASHA recommended including assessment
of support needs such as augmentative and
alternative communication systems (AAC)
and involvement of communication
partners. DSM-5 recognizes the need for
ongoing support to address limits in
adaptive functioning. The diagnostic
features indicate that standardized measures
should be used with knowledgeable
informants.
Major and Mild Neurocognitive Disorders
Dementia is no longer a separate diagnostic
category; replaced by major and mild
neurocognitive disorders (NCD).
Dementia as described in DSM-IV is
classified under major NCD.
Mild cognitive impairment can now be
diagnosed and coded under the new mild
NCD sub-category.
The term dementia can be used to reflect
ASHA supported the change of diagnostic
category from Delirium, Dementia,
Amnestic, and Other Geriatric Cognitive
Disorders to Neurocognitive Disorders
because it is broader in scope and includes
cognitive deficits related to traumatic brain
injury.
ASHA did not support the differentiation
between major and mild
neurocognitive because the differences
between the categories appear to be
May increase referrals of individuals with
mild NCD disorders for cognitive services.
Clinicians and consumers may be confused
when the severity markers are applied to a
major NCD. For example, it is now
possible to receive a diagnosis of a mild
major NCD.
etiological subtypes (e.g., Alzheimers
dementia).
Diagnostic criteria for different etiological
subtypes are either elaborated (vascular &
Alzheimers disease) or revised and
separately delineated (frontotemporal NCD,
Lewy bodies, traumatic brain injury (TBI),
Parkinsons disease, HIV infection,
Huntingtons disease, prion disease,
substance/medication-induced NCD, another
medical condition, multiple etiologies and
unspecified).
Cognitive domains (deficits in), which are the
basis of the NCD diagnosis, are clearly
specified.
arbitrary.
ASHA recommended that the severity
specifiers be excluded for neurocognitive
disorders since a diagnosis such as severe
mild NCD would be confusing. As per
these recommendations, the severity
specifiers for mild NCD have been
excluded. However, the severity markers of
mild, moderate and severe are included as
specifiers for major NCD.
ASHA did not support describing deficits in
mild NCD as insufficient to interfere with
independence. ASHAs recommended
revisions were accepted.
ASHA recommended retaining the explicit
description of symptoms of mild TBI
provided in DSM-IV, and adding
difficulty concentrating as a feature of
mild TBI. Both of these recommendations
were accepted.
Selective Mutism
Now classified as an anxiety disorder (rather
than Other Disorder of Infancy, Childhood ,
or Adolescence in DSM-IV)
No change in the diagnostic criteria.
ASHA did not make recommendations
pertaining to the diagnostic criteria for
selective mutism.
SLPs will continue to be involved as team
members in the diagnosis and treatment of
selective mutism.
Specific Learning Disorder
Characterized as difficulties learning and
using academic skills. Diagnostic criteria
include difficulty with word reading,
understanding the meaning of what is read,
word meaning, spelling, written expression,
ASHA expressed concern about the
omission of oral language as a diagnostic
criterion for specific learning disorder.
DSM-5 indicates that a specific learning
disorder is frequently, but not invariably
Omission of reference to oral language
significantly misrepresents the constellation
of learning disabilities. As a consequence,
individuals may be excluded from receiving
the services they need and research
number use and calculation, and
mathematical reasoning. Combines
diagnoses, which were separate in DSM-IV,
of reading disorder, disorder of written
expression, mathematics disorder, and
learning disorder not otherwise specified.
Determines academic performance through
standardized achievement measures and
comprehensive clinical assessment. Notes
that clinical synthesis should occur based
on the individuals developmental, medical,
family, and educational histories, school
reports, and psycho-educational assessment.
Affected academic skills must be
substantially and quantifiably below those
expected based on chronological age (or
average achievement that is sustainable only
by extraordinary high levels of effort or
support).
Deficits must cause significant interference
with academic or occupational performance,
or with activities of daily living.
Severity levels are specified separately for
impairments in reading, written expression,
and mathematics.
Does not include disorders of spoken
language (speaking and listening) as a
diagnostic criterion.
preceded, in preschool years, by delays in
attention, language or motor skills that may
persist and co-occur with specific learning
disorder.
ASHA argued against the use of
standardized measures as the sole basis for
diagnosis of specific learning disorder.
DSM-5 recognizes the need to include
multiple sources of data to make an
accurate diagnosis. ASHA supports the use,
when available, of culturally and
linguistically appropriate, age-appropriate,
and psychometrically sound standardized
measures as part of an assessment battery
in which assessments are conducted with
fidelity and repeated over time. Use of
inappropriate measures can lead to an
increase in false positives and false
negatives in diagnosing any disorder.
ASHA stressed the need to use culturally
and linguistically appropriate measures.
DSM-5 includes a section on culture-
related diagnostic issues for a specific
learning disorder. This section includes
assessment considerations for English
language learners and the need to consider
cultural and linguistic contextual factors for
assessment.
ASHA preferred the term specific learning
disability, well-established clinical and
research term, rather than specific learning
disorder. Disability addresses the impact of
a disorder and represents a lifelong
problem. However, DSM-5 recognizes that
a specific learning disorder can have
populations may be identified inaccurately.
SLPs will need to be vigilant about
ensuring that individuals with a specific
learning disorder, who also meet the
diagnostic criteria for a language disorder,
receive both diagnoses.
SLPs who are part of the diagnostic team
should emphasize that language can be in
any modality, such as spoken, manually
coded (e.g., signing, cued speech), or other
type of augmentative and alternative
communication system.
Because a specific learning disorder
comprises multiple disorders, it is
important that SLPs and other professionals
recognize that need for comprehensive
assessment and multiple intervention
strategies, which may change over time.
negative functional consequences across
the lifespan.
*Note: ASHA provided comments during the three public comment periods.
References and Resources
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, Fifth Edition.
Arlington, VA: American Psychiatric Association.
American Psychiatric Association, DSM-5 Resources, www.dsm5.org
Highlights of Changes from DSM-IV-TR to DSM-5 http://www.dsm5.org/Documents/changes%20from%20dsm-iv-tr%20to%20dsm-5.pdf
Frequently Asked Questions on the DSM-5 http://www.dsm5.org/about/Pages/faq.aspx
Fact Sheets on Whats New http://www.dsm5.org/
You might also like
- The Dsm-5 Survival Guide: a Navigational Tool for Mental Health ProfessionalsFrom EverandThe Dsm-5 Survival Guide: a Navigational Tool for Mental Health ProfessionalsRating: 3 out of 5 stars3/5 (2)
- DSM 5 OverviewDocument78 pagesDSM 5 Overviewoyehello23No ratings yet
- ASWB EXAMINATION IN SOCIAL WORK [ASWB] (1 VOL.): Passbooks Study GuideFrom EverandASWB EXAMINATION IN SOCIAL WORK [ASWB] (1 VOL.): Passbooks Study GuideNo ratings yet
- Writing DSM 5 DiagnosisDocument2 pagesWriting DSM 5 Diagnosiscristina83% (6)
- LMSW Exam Prep Pocket Study Guide: Intervention Methods and TheoriesFrom EverandLMSW Exam Prep Pocket Study Guide: Intervention Methods and TheoriesNo ratings yet
- A Survival Guide to Understanding the DSM-5Document73 pagesA Survival Guide to Understanding the DSM-5Luke Bacon100% (2)
- Foundations of Clinical Psychiatry Fourth EditionFrom EverandFoundations of Clinical Psychiatry Fourth EditionRating: 5 out of 5 stars5/5 (1)
- DSM 5 EssentialsDocument8 pagesDSM 5 EssentialsAlyssa Gervacio100% (2)
- Psychotherapist'S Guide To Psychopharmacology: Second EditionFrom EverandPsychotherapist'S Guide To Psychopharmacology: Second EditionRating: 5 out of 5 stars5/5 (6)
- DSM 5 DiagnosesDocument1 pageDSM 5 DiagnosesGen Feliciano100% (4)
- Joel Paris-The Intelligent Clinician's Guide To The DSM-5®-Oxford University Press (2013)Document265 pagesJoel Paris-The Intelligent Clinician's Guide To The DSM-5®-Oxford University Press (2013)JC Barrientos100% (7)
- DSM 5 ChartDocument2 pagesDSM 5 ChartJanie VandeBerg93% (27)
- What's New With DSM 5? (Formerly Known As DSM V) : 1 Credit Continuing Education CourseDocument15 pagesWhat's New With DSM 5? (Formerly Known As DSM V) : 1 Credit Continuing Education CourseTodd Finnerty44% (9)
- DSM VDocument9 pagesDSM VAddie Espiritu100% (4)
- More Than Just Words and Numbers:: The Top 15 Fundamental Changes To The Dsm-5 & The Transition To Icd-10Document107 pagesMore Than Just Words and Numbers:: The Top 15 Fundamental Changes To The Dsm-5 & The Transition To Icd-10Hilma Harry'sNo ratings yet
- DSM-5 List of Mental DisordersDocument2 pagesDSM-5 List of Mental DisordersIqbal Baryar100% (1)
- DSM 5 SummaryDocument61 pagesDSM 5 Summaryroxxifoxxi87% (15)
- Case of JessicaDocument2 pagesCase of JessicaElaine Joyce PasiaNo ratings yet
- Psychiatric Rating Scales-RRFINALDocument45 pagesPsychiatric Rating Scales-RRFINALnkivc100% (1)
- Mental Health NotesDocument21 pagesMental Health Notesbazahoor97% (33)
- DSM-5 Diagnosis Reference GuideDocument2 pagesDSM-5 Diagnosis Reference GuideDeAn White100% (1)
- Changes From Dsm-IV-tr To Dsm-5Document19 pagesChanges From Dsm-IV-tr To Dsm-5Sofia Cabezas Ordóñez100% (1)
- Misophonia assessment toolsDocument12 pagesMisophonia assessment toolsSoraia RomanelliNo ratings yet
- DSM 5 Update 2016Document33 pagesDSM 5 Update 2016Monica Putri Damayanti100% (1)
- DSM-5 Personality DisordersDocument2 pagesDSM-5 Personality DisordersIqbal BaryarNo ratings yet
- DSM 5 Cross Cutting Over ViewDocument9 pagesDSM 5 Cross Cutting Over Viewapi-4201886000% (1)
- Common Psychiatric MedicationsDocument1 pageCommon Psychiatric MedicationsDan Kiarie92% (12)
- Intellectual DisabilitiesDocument4 pagesIntellectual Disabilitieslevs rivers100% (1)
- DSM 5 Clinicalcases SoftDocument226 pagesDSM 5 Clinicalcases SoftSophie100% (5)
- Resident's Guide To Clinical PsychiatryDocument412 pagesResident's Guide To Clinical PsychiatryJP Rajendran88% (16)
- PSYCHIATRY Course NotesDocument43 pagesPSYCHIATRY Course NotesNisha PillaiNo ratings yet
- Psychiatry: Mental State ExaminationDocument3 pagesPsychiatry: Mental State ExaminationSok-Moi Chok100% (3)
- Charles Scott-DSM-5® and The Law - Changes and Challenges-Oxford University Press (2015) PDFDocument305 pagesCharles Scott-DSM-5® and The Law - Changes and Challenges-Oxford University Press (2015) PDFfpsearhiva personala100% (3)
- Clinical Psych NotesDocument9 pagesClinical Psych Notesky knmt100% (1)
- Psych CardsDocument10 pagesPsych CardsJennifer Rodriguez96% (23)
- DSM 5 - DSM 5Document7 pagesDSM 5 - DSM 5Roxana ClsNo ratings yet
- The Biopsychosocial Formulation Manual A Guide For Mental Health Professionals PDFDocument178 pagesThe Biopsychosocial Formulation Manual A Guide For Mental Health Professionals PDFLeidy Yiseth Cárdenas100% (4)
- PTSD Clinical Case ExampleDocument10 pagesPTSD Clinical Case Exampleapi-552282470No ratings yet
- DSM 5 CriteriaDocument6 pagesDSM 5 CriteriaCarmela ArcillaNo ratings yet
- DSM-5 Survival Guide Formatted FinalDocument73 pagesDSM-5 Survival Guide Formatted FinalrobajonesincNo ratings yet
- DSM-5 Insanely Simplified: Unlocking The Spectrums Within DSM-5 and ICD-10 - PsychiatryDocument5 pagesDSM-5 Insanely Simplified: Unlocking The Spectrums Within DSM-5 and ICD-10 - Psychiatrylucebycu0% (1)
- DSM 5 TR What's NewDocument2 pagesDSM 5 TR What's NewRafael Gaede Carrillo100% (1)
- DSM-5 LCA Case Formulation Rev.Document31 pagesDSM-5 LCA Case Formulation Rev.Khadeeja Rana100% (3)
- Screening For Personality Disorders Among PDFDocument14 pagesScreening For Personality Disorders Among PDFDrMartens AGNo ratings yet
- Minnesota Multiphasic Personality Inventory TestDocument26 pagesMinnesota Multiphasic Personality Inventory TestGicu BelicuNo ratings yet
- Antidepressant Comparison ChartDocument3 pagesAntidepressant Comparison Chartiggyputtty100% (29)
- Biopsychosocial Formulation PocketmodDocument1 pageBiopsychosocial Formulation Pocketmodluming7100% (1)
- Example Dap NoteDocument5 pagesExample Dap NoteLindsey Jo Townsend80% (5)
- 1001 Biopsychosocial Assessment (PIHP) (Handwritten)Document26 pages1001 Biopsychosocial Assessment (PIHP) (Handwritten)Sharon Price-James100% (3)
- The Mental Status Exam: A Systematic ApproachDocument35 pagesThe Mental Status Exam: A Systematic ApproachMohamad Faizul Abu HanifaNo ratings yet
- Notes On Mood DisordersDocument21 pagesNotes On Mood DisordersPrince Rener Velasco Pera67% (3)
- Behavioral Guide To Personality Disorders - (DSM-5) (2015) by Douglas H. RubenDocument275 pagesBehavioral Guide To Personality Disorders - (DSM-5) (2015) by Douglas H. RubenCristianBale100% (6)
- DSM5 Workshop PresentationsDocument185 pagesDSM5 Workshop PresentationsMichel Haddad100% (2)
- DSM 5 DiagnosingDocument107 pagesDSM 5 DiagnosingMichel Haddad100% (1)
- HTTP WWW - Nami.org Template - CFM Section Borderline Personality Disorder (BPD) &template ContentManagement ContentDisplayDocument20 pagesHTTP WWW - Nami.org Template - CFM Section Borderline Personality Disorder (BPD) &template ContentManagement ContentDisplayCorina MihaelaNo ratings yet
- Psychiatric Clinical SkillsDocument376 pagesPsychiatric Clinical SkillsSamuel Agunbiade100% (5)
- Case FormulationDocument22 pagesCase FormulationELvine Gunawan100% (5)
- The Master Disorder Document SPR 2015Document6 pagesThe Master Disorder Document SPR 2015api-261267976100% (1)
- Suicide Risk Assessment Summary.08Document1 pageSuicide Risk Assessment Summary.08Pintiliciuc-aga MihaiNo ratings yet
- Psychiatric Assessment ToolDocument53 pagesPsychiatric Assessment ToolLori100% (4)
- Utility of BAI Factors in Screening Anxiety DisordersDocument15 pagesUtility of BAI Factors in Screening Anxiety DisordersMilos Beba Ristic100% (1)
- Management Guidelines For Anxiety Disorders in Children and AdolescentsDocument23 pagesManagement Guidelines For Anxiety Disorders in Children and AdolescentsHari HaranNo ratings yet
- Brief Psychiatric Rating ScaleDocument1 pageBrief Psychiatric Rating ScalesilmarestuNo ratings yet
- 21 - Smith2014Document33 pages21 - Smith2014stupidshitNo ratings yet
- Psychological Disorders Chapter 13: Defining and Diagnosing Mental Disorders/TITLEDocument34 pagesPsychological Disorders Chapter 13: Defining and Diagnosing Mental Disorders/TITLEannaNo ratings yet
- Psych 1 Phobia ProjectDocument3 pagesPsych 1 Phobia ProjectalexlaneNo ratings yet
- The Effectiveness of Psychodynamic Psychotherapies - An Update (2015) PDFDocument14 pagesThe Effectiveness of Psychodynamic Psychotherapies - An Update (2015) PDFmysticmdNo ratings yet
- A Different Approach To Rising Rates of ADHD DiagnosisDocument1 pageA Different Approach To Rising Rates of ADHD DiagnosisPaul AsturbiarisNo ratings yet
- Child Depression Inventory Cdi InterpretationDocument2 pagesChild Depression Inventory Cdi InterpretationGerlinde M Schmidt75% (4)
- Ab Psych Exam by Sir ThanksDocument15 pagesAb Psych Exam by Sir ThanksSteffiNo ratings yet
- Borderline Personality DisorderDocument368 pagesBorderline Personality Disordercarlesavila224678% (9)
- Child and Adolescent DisorderDocument38 pagesChild and Adolescent DisorderZeref KakarotNo ratings yet
- Letter For Wayne McGuinness' Ride For Mental HealthDocument2 pagesLetter For Wayne McGuinness' Ride For Mental Healthscribd-jNo ratings yet
- Libro The Oxford Handbook of Depression and Comorbidity PDFDocument673 pagesLibro The Oxford Handbook of Depression and Comorbidity PDFToñitoo H. Skelter100% (2)
- Mania & ADHDDocument47 pagesMania & ADHDbabarsaggu100% (1)
- CBT Reading ListDocument6 pagesCBT Reading ListrzeczywistoscgryzieNo ratings yet
- You Probably Have AdhdDocument3 pagesYou Probably Have AdhdNur Amaleena GafarNo ratings yet
- Kleptomania and HomoeopathyDocument7 pagesKleptomania and HomoeopathyDr. Rajneesh Kumar Sharma MD HomNo ratings yet
- Catatonia: FeaturesDocument6 pagesCatatonia: FeaturesfirehuNo ratings yet
- Test Bank For Foundations of Mental Health Care 3rd Edition Morrison ValfreDocument11 pagesTest Bank For Foundations of Mental Health Care 3rd Edition Morrison ValfreAnthonyRiveraqion100% (43)
- Ocd in dsm-5 2014Document15 pagesOcd in dsm-5 2014Dilan RasyidNo ratings yet
- Delusion and HallucinationDocument4 pagesDelusion and HallucinationRiezky FebriyantiNo ratings yet
- Psychiatry SamsonDocument12 pagesPsychiatry Samsonamina100% (1)
- Parental Substance AbuseDocument8 pagesParental Substance Abuseapi-458338612No ratings yet
- Child Psychiatry - Introduction PDFDocument7 pagesChild Psychiatry - Introduction PDFRafli Nur FebriNo ratings yet
- Don'T Hide Behind Happiness, Live in ItDocument3 pagesDon'T Hide Behind Happiness, Live in ItChacha D. LoñozaNo ratings yet
- Social Anxiety Disorder PDFDocument14 pagesSocial Anxiety Disorder PDFhamoNo ratings yet
- Anxiety DisordersDocument18 pagesAnxiety DisordersAzahed ArturoNo ratings yet
- Adhd - David JesselsonDocument12 pagesAdhd - David Jesselsonapi-311051259100% (1)
- Psychiatry 1 Dr. Anastasia Ratnawati Biromo, SPKJ - Identifying Anxiety and Somatization and Its Treatment in General PracticeDocument23 pagesPsychiatry 1 Dr. Anastasia Ratnawati Biromo, SPKJ - Identifying Anxiety and Somatization and Its Treatment in General PracticeThomas KweeNo ratings yet


![ASWB EXAMINATION IN SOCIAL WORK [ASWB] (1 VOL.): Passbooks Study Guide](https://imgv2-1-f.scribdassets.com/img/word_document/402068986/149x198/afec08b5ad/1617230405?v=1)