Professional Documents
Culture Documents
Azoospermia No Obstructiva
Uploaded by
César EscalanteOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Azoospermia No Obstructiva
Uploaded by
César EscalanteCopyright:
Available Formats
Medical management of non-obstructive azoospermia
Rajeev Kumar
All India Institute of Medical Sciences, Department of Urology, New Delhi, India.
Non-obstructive azoospermia is diagnosed in approximately 10% of infertile men. It represents a failure of
spermatogenesis within the testis and, from a management standpoint, is due to either a lack of appropriate
stimulation by gonadotropins or an intrinsic testicular impairment. The former category of patients has
hypogonadotropic hypogonadism and benefits from specific hormonal therapy. These men show a remarkable
recovery of spermatogenic function with exogenously administered gonadotropins or gonadotropin-releasing
hormone. This category of patients also includes some individuals whose spermatogenic potential has been
suppressed by excess androgens or steroids, and they also benefit from medical management. The other, larger
category of non-obstructive azoospermia consists of men with an intrinsic testicular impairment where
empirical medical therapy yields little benefit. The primary role of medical management in these men is to
improve the quantity and quality of sperm retrieved from their testis for in vitro fertilization. Gonadotropins
and aromatase inhibitors show promise in achieving this end point.
KEYWORDS: Infertility; Drug Therapy; Gonadotropins; Hypogonadism; Aromatase Inhibitors.
Kumar R. Medical management of non-obstructive azoospermia. Clinics. 2013;68(S1):75-79.
Received for publication on February 29, 2012; Accepted for publication on March 2, 2012
E-mail: rajeev02@gmail.com
Tel.: +91-11-26594884
& INTRODUCTION
Non-obstructive azoospermia (NOA) is generally consid-
ered a non-medically manageable cause of male infertility.
These patients, who constitute up to 10% of all infertile men,
have abnormal spermatogenesis as the cause of their
azoospermia. The establishment of in vitro fertilization
using intracytoplasmic sperm injection (ICSI) as a standard
treatment modality has resulted in a number of these men
successfully fathering a child through surgically retrieved
sperm from the testis. The challenge, however, is to improve
their spermatogenic function to enable the appearance of
sperm in their ejaculate or to improve the chances of a
successful retrieval from the testis for ICSI.
The initial evaluation aims at resolving the following
issues: (1) confirming azoospermia, (2) differentiating
obstructive from non-obstructive etiology, (3) assessing for
the presence of reversible factors and (4) evaluating for the
presence of genetic abnormalities. An elevated follicle-
stimulating hormone (FSH) level or an absence of normal
spermatogenesis by testicular histology in the presence of
azoospermia is generally considered sufficient evidence of a
non-obstructive etiology. The most common reversible
factors that need to be ruled out include recent exogenous
hormone administration, severe febrile illnesses, chemother-
apy/radiation or prolonged antibiotic use.
Hormone analysis forms the cornerstone of the further
evaluation and management of NOA and serves two
important functions. The first function is to identify a
distinct subset of men who have hypogonadotropism (low
FSH), in which azoospermia results from an inadequate
stimulation of the testis by gonadotropins. The inherent
spermatogenic potential of the testis may be partially
recoverable, and the management and prognosis of inferti-
lity in these men differ from all other subsets. The second
function is to predict the success of medical therapy and of
surgical sperm retrieval. Based on these initial hormone
studies, the two broad categories are hypogonadotropic
hypogonadism and hypergonadotropic hypogonadism or
eugonadism (Table 1). There is considerable overlap in the
hormone statuses of men who do not have hypogonado-
tropism, with similar etiologies producing a spectrum of
hormonal changes. The American Urological Association
recommends an estimation of serum FSH and testosterone
as the initial hormonal assessment (1). However, endocrine
abnormalities are a rare cause of male infertility and account
for less than 3% of all cases. Additional hormone analysis,
including luteinizing hormone (LH), estradiol and prolactin
evaluations, is performed based on the likelihood of their
abnormality and potential impact on management.
& HYPOGONADOTROPIC HYPOGONADISM
Hypogonadotropic hypogonadism (HH) is a condition of
low serum testosterone due to a decrease in the secretion of
FSH and LH from the pituitary gland. HH may be
congenital, acquired or idiopathic. The congenital forms
Copyright 2013 CLINICS This is an Open Access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License (http://
creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-
commercial use, distribution, and reproduction in any medium, provided the
original work is properly cited.
No potential conflict of interest was reported.
DOI: 10.6061/clinics/2013(Sup01)08
REVIEW
75
are classically syndromic, such as Kallmann syndrome,
Prader-Willi syndrome and Laurence-Moon syndrome.
Acquired HH usually results from the destruction of normal
pituitary function following radiotherapy, trauma or a
pituitary tumor. Another form of acquired HH is due to
excess exogenous steroids or androgens. Hyperprolactinemia
may also cause infertility by inhibiting the hypothalamic
secretion of gonadotropin-releasing hormone (GnRH) and
also through a direct inhibition of the binding of LH to the
Leydig cells in the testis.
Congenital hypogonadotropic hypogonadism typically
occurs in association with anosmia and is known as
Kallmann syndrome. It has varying genetic modes of
transmission, including via both sex chromosomal (X-
linked) and autosomal abnormalities. Hypogonadism
results in abnormal secondary sexual characteristics, includ-
ing gynecomastia, cryptorchidism and micropenis. The
primary abnormality is decreased GnRH secretion from
the hypothalamus with consequent low levels of gonado-
tropins (FSH and LH) from the pituitary.
Hypogonadotropic hypogonadism is one of the fewcauses
of NOA that have shown a consistent response to medical
management (2,3). Gonadotropin therapy is begun at the
time the patient wishes to father a child, and three to six
months of treatment are usually sufficient to induce
spermatogenesis (4,5). Therapy is initiated with human
chorionic gonadotropin (hCG) at 2,000 IU subcutaneously
three times per week or 2,500 IU twice a week and
supplemented with FSH (menopausal, purified or recombi-
nant) at 37.5-150 IU three times a week after three to six
months. hCG is sufficient to initiate spermatogenesis, but
FSH is required to complete the spermiogenesis, particularly
in patients with congenital abnormalities. In one of the largest
reported series, Burgues et al. (6) evaluated self-administered
highly purified follicle-stimulating hormone in 60 men with
hypogonadotropic hypogonadism who showed an adequate
response to an initial hCGtherapy. Subjects self-administered
150 IU of FSH three times per week and 2,500 IU of hCG
twice a week for at least six months, with non-responders
continuing treatment for a further period. By the end of the
treatment, 80% of these azoospermic/aspermic men had
sperm in their ejaculate, with a median time to sperm
presence of five months. Similar data reported from other
studies support the specific role of hormone replacement
therapy in these men (7,8).
An alternative method for treating hypogonadotropic
hypogonadism is with a pulsatile injection of GnRH in
patients with intact pituitary glands. GnRH can be
administered subcutaneously, intravenously or intranasally,
but the 2-hour dosing regimen makes the intravenous and
intranasal routes impractical. The standard method is 5-20
micrograms administered every 2 hours subcutaneously. In
a large cohort of men with idiopathic hypogonadotropic
hypogonadism (IHH), a bihourly pulsatile administration of
GnRH subcutaneously through an infusion pump for 12-24
months resulted in the induction of spermatogenesis in 77%
of initially azoospermic men (9). The authors reported a
more rapid return of spermatogenesis in men who had
achieved at least partial puberty at the time of initiating
GnRH therapy, with all such subjects responding within six
months. GnRH therapy reliably corrected the hypogonad-
ism, with a reversal of azoospermia in a majority of the men,
but a subset of men may exhibit pituitary resistance or
atypical response (10). Other studies have also reported the
successful initiation of pregnancy using GnRH therapy
(11,12). Pulsatile GnRH therapy is more cumbersome and
expensive than gonadotropin therapy, and this precludes its
routine use. However, in men with IHH who fail to respond
to gonadotropin therapy, GnRH therapy may be an option.
GnRH therapy is also not possible in men who do not have
functional pituitary glands.
Congenital abnormalities are likely to have been noticed
early during adolescence, and a number of these men would
have received testosterone therapy near the onset of puberty
to induce the development of secondary sexual character-
istics. This prior treatment with testosterone at the time of
puberty does not interfere with the response to gonado-
tropins when attempting a pregnancy. A number of these
men will produce sperm in their ejaculate but with total
counts below the reference range. However, these men are
often able to initiate a pregnancy with these low counts (13).
Therapeutic interventions may be associated with a sig-
nificant delay in the appearance of sperm or achieving a
sufficient quantity or quality to imitate a spontaneous
pregnancy, and some men may benefit from assisted
reproduction techniques if an adequate response is not
observed at the end of one year (14,15).
Androgen and steroid excess
Androgen excess through exogenous administration or
pituitary/adrenal or testicular tumors can also lead to the
suppression of spermatogenesis and NOA that is amenable
to medical management. This is a form of hypogonadotropic
hypogonadism, where the excess androgens produce feed-
back inhibition on normal pulsatile gonadotropin secretion,
and suppression of excess steroids results in the recovery of
spermatogenesis.
Congenital adrenal hyperplasia is a diagnosis of child-
hood. However, a number of these men will present as adults
with infertility. Infertility is particularly common in the
presence of associated testicular adrenal rest tumors
(TARTs). Exogenous steroid administration results in sup-
pression of adrenocorticotropic hormone (ACTH) with a
consequent decrease in the size of the TARTs and the possible
return of fertility (16,17). Devoto et al. (18) reported a 29-year-
old male with azoospermia and congenital adrenal hyper-
plasia with a 21-hydroxylase deficiency who had normal
serum hormones but a testicular biopsy suggesting hypogo-
nadism. The patient was treated with exogenous corticoster-
oids that resulted in normal testicular development,
improvement in sperm counts and spontaneous paternity
Table 1 - Non-obstructive azoospermia classification
Hypogonadotropic hypogonadism
N
Low FSH, Low LH, Low testosterone
N
Congenital: Kallmann syndrome (hypothalamic GnRH deficiency)
N
Acquired: Pituitary tumors
Hypergonadotropic hypogonadism/eugonadism
N
High/normal FSH, Normal/high LH, Normal/low testosterone
N
Congenital: Genetic abnormalities (Chromosomal)
N
Acquired:
N
Varicocele
N
Orchitis
N
Gonadotoxins (chemotherapy/radiation)
N
Trauma/torsion
N
Idiopathic
Drug therapy for NOA
Kumar R
CLINICS 2013;68(S1):75-79
76
on two occasions. The authors cautioned that hormone
analysis in these men might not suggest hypogonadism
because the excess testosterone production from the adrenals
masks the intra-testicular hypogonadism. A reversal of
azoospermia may depend on the type of steroid used and
its dose. Claahsen-van der Grinten (19) noted inadequate
suppression with 30 mg of hydrocortisone but a significant
improvement after changing to an equivalent dose of
dexamethasone in a patient who had azoospermia but went
on to father two children through spontaneous conception
after this change. These outcomes have been supported by
other reports on the reversal of azoospermia with exogenous
dexamethasone treatment (20,21).
Excess androgens present in anabolic steroids or testos-
terone itself are potent causes for the suppression of
endogenous hormone production. The initial step in the
management of these men is the cessation of the use of all
such hormones. It may take a year or longer for endogenous
production to return to normal after the cessation of
exogenous therapy. Spermatogenesis may then be sponta-
neously restored, or there may then be evidence of
additional endocrine abnormalities that will need to be
addressed.
& HYPERGONADOTROPIC HYPOGONADISM/
EUGONADISM
Aromatase inhibitors
High intra-testicular levels of testosterone are necessary
for spermatogenesis. An imbalance between the circulating
testosterone and estrogen levels has been investigated as a
potential therapeutic target in men with NOA. The enzyme
aromatase, which is present in the adipose tissue, liver,
testis and skin, is responsible for converting testosterone
and other androgens to estradiol in men. Estradiol sup-
presses pituitary LH and FSH secretion and also directly
inhibits testosterone biosynthesis. This results in an imbal-
ance in the testosterone and estradiol (T/E) ratio, which
may be reversible. Aromatase inhibitors have the potential
to block the conversion of androgens to estradiol. The two
types of aromatase inhibitors are steroidal (testolactone) and
non-steroidal (anastrozole, letrozole). Both of these groups
of agents have been studied for potential therapeutic roles in
NOA.
In 2001, Pavlovich et al. reported one of the first studies
on the potential role of low-dose oral testolactone in men
with NOA or severe oligospermia (22), in which 63 men
(NOA or sperm density below 10 million/mL) were
evaluated. This study included 43 men with NOA that
was documented by a testis biopsy. Data from these men
were compared with those from 40 age-matched fertile
controls. All men underwent a baseline hormone profile,
and 45 out of 63 men had a testosterone-to-estradiol ratio
below the 20
th
percentile of normal, as determined from the
healthy controls. These 45 men included patients with
Klinefelters syndrome, chromosomal anomalies, varico-
celes, etc. as the cause for NOA. Subjects received 50 to
100 mg of oral testolactone twice a day for a mean of five
months. Hormone profiles were obtained at one month of
therapy, and the dose of testolactone was increased from 50
to 100 mg if the ratios remained low. A semen analysis was
performed after at least three months of stable drug therapy.
The authors reported a decline in estradiol or an increase
in testosterone with drug therapy in all patients, with
significant improvements in T/E ratios. However, while the
oligospermic men demonstrated significant improvements
in total sperm counts and motility, none of the 12
azoospermic men who completed three months of treatment
showed any return of sperm in the ejaculate.
In a direct comparison between testolactone and anastro-
zole, Raman and Schlegel treated 140 men with low T/E
ratios with testolactone and/or anastrozole (23). Some men
received both therapies sequentially; they overlapped in the
study population. Ultimately, 74 men received 50 to 100 mg
of testolactone twice daily for a mean of six months, and 104
men received 1 mg of anastrozole daily for a mean of 4.7
months. The 12 azoospermic men did not exhibit any
improvement. Similar to their experience with testolactone,
while the T/E ratios improved in all men, none of the 14
azoospermic men experienced a return of sperm to the
ejaculate.
These studies argue against the use of aromatase
inhibitors in NOA men. However, there may be a potential
role in improving the quality or quantity of testicular sperm,
thus improving the outcomes of sperm retrieval using
testicular sperm extraction (TESE) and ICSI. Schiff et al.
reported their experience with pretreatment with testolac-
tone, hCG and anastrozole in men with non-mosaic
Klinefelters syndrome prior to TESE/ICSI (24). Among
their cohort of 42 men, 36 had low pre-treatment levels of
testosterone. These men received either an aromatase
inhibitor alone or in combination with hCG until the
testosterone or T/E ratio normalized. TESE was successful
in all men who received either anastrozole alone or in
combination with hCG, while it succeeded in 74% of those
receiving only testolactone and 54% of those receiving
testolactone and hCG. The authors did not have a control
group, and it is difficult to assess the contribution of the
pretreatment on the successful outcomes, particularly
because all six men who did not require pretreatment had
successful outcomes. However, the success rates in these
men were higher than historical controls. In a more recent
update of their data, this group identified no significant
impact of the pretreatment on a successful outcome (25).
However, they did note an improved outcome if the
pretreatment resulted in an improved serum testosterone
level prior to performing the TESE.
Antiestrogens
Clomiphene citrate and tamoxifen are non-steroidal anti-
estrogens that have long been used as empirical options in the
management of idiopathic oligospermia. Clomiphene blocks
the feedback inhibition of estrogen on the pituitary, resulting
in increased FSH and LH secretion and a consequent rise in
testosterone. There is little scientific evidence in favor of using
clomiphene empirically. However, it continues to be a popular
choice and has been used in men with NOA. Hussein et al.
treated 42 men with NOA and either hypospermatogenesis or
maturation arrest based on a biopsy with clomiphene citrate,
which was initially 50 mg every alternate day for two weeks
and then increased serially until the testosterone levels
reached between 600-800 ng/dL (26). Semen analysis was
performed at regular intervals, and if azoospermia persisted
beyond six months of treatment, a testis biopsy was
performed. The results revealed that 64% of the men
experienced a return of sperm in their ejaculate, with sperm
density ranging from 1-16 million/mL. Among those who
remainedazoospermic, spermretrieval for ICSI was successful
CLINICS 2013;68(S1):75-79 Drug therapy for NOA
Kumar R
77
in all cases. Of note, the authors excluded all men with Sertoli
cell-only syndrome or a lowtesticular volume anda mean FSH
at baseline of 7.21 mIU/mL. Further, this remains the only
series on the successful use of clomiphene in azoospermic
men, and its results have not been replicated by other
investigators.
Gonadotropins
The use of gonadotropins to induce the appearance of
sperm in the ejaculate or to increase the success rates of
TESE in men with NOA has been based on the rationale
that high levels of exogenous gonadotropins decrease the
endogenous gonadotropin secretion. This in turn allows a
resetting of the FSH and LH receptors in the Leydig and
Sertoli cells, whose functions then improve (27).
Selman et al. reported a 32-year-old man with Y
chromosome microdeletions who received recombinant
FSH and hCG before a successful ICSI procedure with
ejaculated sperm that numbered in the few thousands (28).
Similarly, Efesoy et al. reported sperm in the ejaculate of 2
of 11 azoospermic men with maturation arrest who were
treated with recombinant FSH (29).
Shiraishi et al. reviewed their data on repeat TESE in men
with NOA who had no sperm retrieved during the first
TESE (30). Of 48 such men with no chromosomal anomalies
and normal serum testosterone levels, 28 received 5,000 IU
of hCG three times a week for three months. The men whose
FSH declined significantly received additional recombinant
FSH of 150 IU three times a week for two months, while the
other men continued to receive hCG until the repeat TESE.
Another 20 men in this cohort refused hormonal therapy
and underwent a second TESE at a mean of 17 months after
the first surgery. None of the 48 men experienced a return of
sperm in their ejaculate. However, the second TESE was
successful in 21% of men who received hormonal therapy,
while it failed in all those who did not. By evaluating a more
select group of men with normal baseline hormone profiles,
testicular volumes and genetic analyses, Selman et al.
treated 49 men with rFSH, which was initially at 75 IU on
alternate days for two months, followed by 150 IU for two
months and then an additional 2,000 IU of hCG for two
months (31). All men remained azoospermic at the end of
treatment; however, while none had mature sperm in the
pre-treatment testis biopsy, sperm were found in the
biopsies of 22% men after treatment. Similarly, Ramasamy
et al. reported improved outcomes of primary TESE
following gonadotropin therapy in men with NOA and
Klinefelters syndrome (25).
Antioxidants
The role of antioxidant therapy in male subfertility
continues to be debated. While there is a significant amount
of data documenting raised oxidative stress and low
antioxidant capacity in the seminal plasma of infertile men
with abnormal semen parameters, including azoospermia,
there is little high-quality evidence in support of using
antioxidants in the treatment of these men (32). This is
primarily because such therapy has not resulted in significant
improvements in pregnancy rates, although statistically
significant changes in anti-oxidant capacity and improve-
ments in measured seminal parameters have occurred.
Furthermore, most of the existing literature involves men
with oligo/asthenospermia and not azoospermia. One of the
fewstudies using antioxidants on azoospermic men reported
a remarkable improvement in all subjects but was hampered
by a poorly documented methodology (33).
Among men with NOA, gonadotropin therapy for
hypogonadotropic hypogonadism is the only specific
indication that has universally shown an improvement in
semen analysis and pregnancy rates. Gonadotropins (hCG
and rFSH) in combination constitute a standard therapy,
with GnRH therapy reserved for non-responders. The
medical management of other forms of NOA remains
empirical. Drug therapy with aromatase inhibitors and
gonadotropins shows potential promise in improving out-
comes in men requiring surgical sperm retrieval, but there is
lack of level I clinical evidence for this indication.
& REFERENCES
1. American Urological Association. The optimal evaluation of the infertile
male. Accessed February 22, 2012. Available from: http://www.auanet.
org/content/media/optimalevaluation2010.pdf.
2. Hoffman AR, Crowley WF. Induction of Puberty in Men by Long-Term
Pulsatile Administration of Low-Dose Gonadotropin-Releasing Hormone.
New Engl J Med. 1982;307(20):1237-41, http://dx.doi.org/10.1056/
NEJM198211113072003.
3. Belchetz PE, Plant TM, Nakai Y, Keogh EJ, Knobil E. Hypophysial
responses to continuous and intermittent delivery of hypopthalamic
gonadotropin-releasing hormone. Science. 1978;202(4368):631-3, http://
dx.doi.org/10.1126/science.100883.
4. Vicari E, Mongioi A, Calogero AE, Moncada ML, Sidoti G, Polosa P, et al.
Therapy with human chorionic gonadotrophin alone induces spermato-
genesis in men with isolated hypogonadotrophic hypogonadismlong-
term follow-up. International journal of andrology. 1992;15(4):320-9,
http://dx.doi.org/10.1111/j.1365-2605.1992.tb01131.x.
5. Finkel DM, Phillips JL, Snyder PJ. Stimulation of spermatogenesis by
gonadotropins in men with hypogonadotropic hypogonadism.
N Engl J Med. 1985;313(11):651-5.
6. Burgues S, Calderon MD. Subcutaneous self-administration of highly
purified follicle stimulating hormone and human chorionic gonadotrophin
for the treatment of male hypogonadotrophic hypogonadism. Spanish
Collaborative Group on Male Hypogonadotropic Hypogonadism. Hum
Reprod. 1997;12(5):980-6, http://dx.doi.org/10.1093/humrep/12.5.980.
7. Liu PY, Gebski VJ, Turner L, Conway AJ, Wishart SM, Handelsman DJ.
Predicting pregnancy and spermatogenesis by survival analysis during
gonadotrophin treatment of gonadotrophin-deficient infertile men. Hum
Reprod. 2002;17(3):625-33, http://dx.doi.org/10.1093/humrep/17.3.625.
8. Efficacy and safety of highly purified urinary follicle-stimulating
hormone with human chorionic gonadotropin for treating men with
isolated hypogonadotropic hypogonadism. European Metrodin HP
Study Group. Fertil Steril. 1998;70(2):256-62.
9. Pitteloud N, Hayes FJ, Dwyer A, Boepple PA, Lee H, Crowley WF, Jr.
Predictors of outcome of long-term GnRH therapy in men with
idiopathic hypogonadotropic hypogonadism. The Journal of clinical
endocrinology and metabolism. 2002;87(9):4128-36, http://dx.doi.org/
10.1210/jc.2002-020518.
10. Sykiotis GP, Hoang XH, Avbelj M, Hayes FJ, Thambundit A, Dwyer A,
et al. Congenital idiopathic hypogonadotropic hypogonadism: evidence
of defects in the hypothalamus, pituitary, and testes. J Clin Endocrinol
Metab. 2010;95(6):3019-27, http://dx.doi.org/10.1210/jc.2009-2582.
11. Buchter D, Behre HM, Kliesch S, Nieschlag E. Pulsatile GnRH or human
chorionic gonadotropin human menopausal gonadotropin as effective
treatment for men with hypogonadotropic hypogonadism: a review of 42
cases. Eur J Endocrinol. 1998;139(3):298-303.
12. Delemarre-Van de Waal HA. Induction of testicular growth and spermato-
genesis by pulsatile, intravenous administration of gonadotrophin-releasing
hormone in patients with hypogonadotrophic hypogonadism. Clin
Endocrinol (Oxf). 1993;38(5):473-80.
13. Burris AS, Clark RV, Vantman DJ, Sherins RJ. A Low Sperm
Concentration Does Not Preclude Fertility in Men with Isolated
Hypogonadotropic Hypogonadism after Gonadotropin Therapy.
Fertility and sterility. 1988;50(2):343-7.
14. Tachiki H, Ito N, Maruta H, Kumamoto Y, Tsukamoto T. Testicular
findings, endocrine features and therapeutic responses of men with
acquired hypogonadotropic hypogonadism. International journal of
urology : official journal of the Japanese Urological Association.
1998;5(1):80-5, http://dx.doi.org/10.1111/j.1442-2042.1998.tb00244.x.
15. Liu PY, Handelsman DJ. The present and future state of hormonal
treatment for male infertility. Human reproduction update. 2003;9(1):9-
23, http://dx.doi.org/10.1093/humupd/dmg002.
Drug therapy for NOA
Kumar R
CLINICS 2013;68(S1):75-79
78
16. Augarten A, Weissenberg R, Pariente C, Sack J. Reversible male
infertility in late onset congenital adrenal hyperplasia. J Endocrinol
Invest. 1991;14(3):237-40.
17. Tiitinen A, Valimaki M. Primary infertility in 45-year-old man with
untreated 21-hydroxylase deficiency: successful outcome with glucocor-
ticoid therapy. The Journal of clinical endocrinology and metabolism.
2002;87(6):2442-5, http://dx.doi.org/10.1210/jc.87.6.2442.
18. Devoto CE, Madariaga AM, Fernandez W. [Congenital adrenal hyperpla-
sia causing male infertility. Report of one case]. Revista medica de Chile.
2011;139(8):1060-5, http://dx.doi.org/10.4067/S0034-98872011000800012.
19. Claahsen-van der Grinten HL, Otten BJ, Sweep FC, Hermus AR.
Repeated successful induction of fertility after replacing hydrocortisone
with dexamethasone in a patient with congenital adrenal hyperplasia
and testicular adrenal rest tumors. Fertility and sterility. 2007;88(3):705
e5-8.
20. Nicopoullos JD, Ramsay JW, Cassar J. From zero to one hundred million
in six months: the treatment of azoospermia in congenital adrenal
hyperplasia. Archives of andrology. 2003;49(4):257-63, http://dx.doi.
org/10.1080/713828165.
21. Iwamoto T, Yajima M, Tanaka H, Minagawa N, Osada T. [A case report:
reversible male infertility due to congenital adrenal hyperplasia]. Nihon
Hinyokika Gakkai zasshi The japanese journal of urology. 1993;84(11):
2031-4.
22. Pavlovich CP, King P, Goldstein M, Schlegel PN. Evidence of a treatable
endocrinopathy in infertile men. J Urol. 2001;165(3):837-41.
23. Raman JD, Schlegel PN. Aromatase inhibitors for male infertility. J Urol.
2002;167(2 Pt 1):624-9.
24. Schiff JD, Palermo GD, Veeck LL, Goldstein M, Rosenwaks Z, Schlegel
PN. Success of testicular sperm extraction [corrected] and intracytoplas-
mic sperm injection in men with Klinefelter syndrome. J Clin Endocrinol
Metab. 2005;90(11):6263-7, http://dx.doi.org/10.1210/jc.2004-2322.
25. Ramasamy R, Ricci JA, Palermo GD, Gosden LV, Rosenwaks Z, Schlegel
PN. Successful fertility treatment for Klinefelters syndrome. J Urol.
2009;182(3):1108-13.
26. Hussein A, Ozgok Y, Ross L, Niederberger C. Clomiphene administra-
tion for cases of nonobstructive azoospermia: a multicenter study.
J Androl. 2005;26(6):787-91; discussion 92-3.
27. Foresta C, Bettella A, Spolaore D, Merico M, Rossato M, Ferlin A.
Suppression of the high endogenous levels of plasma FSH in infertile
men are associated with improved Sertoli cell function as reflected by
elevated levels of plasma inhibin B. Hum Reprod. 2004;19(6):1431-7,
http://dx.doi.org/10.1093/humrep/deh255.
28. Selman HA, Cipollone G, Stuppia L, De Santo M, Sterzik K, El-Danasouri
I. Gonadotropin treatment of an azoospermic patient with a Y-
chromosome microdeletion. Fertility and sterility. 2004;82(1):218-9,
http://dx.doi.org/10.1016/j.fertnstert.2003.11.055.
29. Efesoy O, Cayan S, Akbay E. The efficacy of recombinant human follicle-
stimulating hormone in the treatment of various types of male-factor
infertility at a single university hospital. J Androl. 2009;30(6):679-84.
30. Shiraishi K, Ohmi C, Shimabukuro T, Matsuyama H. Human chorionic
gonadotrophin treatment prior to microdissection testicular sperm
extraction in non-obstructive azoospermia. Hum Reprod. 2012;27(2):331-
9, http://dx.doi.org/10.1093/humrep/der404.
31. Selman H, De Santo M, Sterzik K, Cipollone G, Aragona C, El-Danasouri
I. Rescue of spermatogenesis arrest in azoospermic men after long-term
gonadotropin treatment. Fertil Steril. 2006;86(2):466-8, http://dx.doi.
org/10.1016/j.fertnstert.2005.12.055.
32. Esteves SC, Agarwal A. Novel concepts in male infertility. Int Braz J Urol.
2011;37(1):5-15.
33. Singh AK, Tiwari AK, Singh PB, Dwivedi US, Trivedi S, Singh SK, et al.
Multivitamin and micronutrient treatment improves semen parameters
of azoospermic patients with maturation arrest. Indian J Physiol
Pharmacol. 2010;54(2):157-63.
CLINICS 2013;68(S1):75-79 Drug therapy for NOA
Kumar R
79
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Lubchenco Curve PDFDocument1 pageLubchenco Curve PDFWarren Lie25% (4)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Week 8 - Powerpoint Issues On Artificial Reproduction, Its Morality andDocument13 pagesWeek 8 - Powerpoint Issues On Artificial Reproduction, Its Morality andArlynn Faith Cabrera75% (4)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Columbia Sexuality and Gender Law Clinic - Surrogacy Law and Policy Report - June 2016 PDFDocument90 pagesColumbia Sexuality and Gender Law Clinic - Surrogacy Law and Policy Report - June 2016 PDFShantanu AgnihotriNo ratings yet
- Five Elements Tai Chi Chuan Theory In-DepthDocument10 pagesFive Elements Tai Chi Chuan Theory In-DepthCésar EscalanteNo ratings yet
- Model Systems in SDHx-related Pheochromocytoma/paragangliomaDocument25 pagesModel Systems in SDHx-related Pheochromocytoma/paragangliomaCésar EscalanteNo ratings yet
- Latent Adrenal Insufficiency: From Concept To DiagnosisDocument12 pagesLatent Adrenal Insufficiency: From Concept To DiagnosisCésar EscalanteNo ratings yet
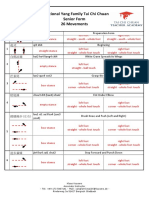
- Traditional Yang Family Tai Chi Chuan Tai Chi Kung 10 MovementsDocument3 pagesTraditional Yang Family Tai Chi Chuan Tai Chi Kung 10 MovementsCésar EscalanteNo ratings yet
- 2020 Article 1793Document13 pages2020 Article 1793César EscalanteNo ratings yet
- iPSC Technology-Based Regenerative Therapy For DiabetesDocument10 pagesiPSC Technology-Based Regenerative Therapy For DiabetesCésar EscalanteNo ratings yet
- Steps: Liraglutide (Saxenda) For Weight LossDocument2 pagesSteps: Liraglutide (Saxenda) For Weight LossCésar EscalanteNo ratings yet
- Liraglutide and Cardiovascular Outcomes in Type 2 DiabetesDocument17 pagesLiraglutide and Cardiovascular Outcomes in Type 2 DiabetesCésar EscalanteNo ratings yet
- Treatment of Peripheral Precocious Puberty in McCune-Albright SyndromeDocument12 pagesTreatment of Peripheral Precocious Puberty in McCune-Albright SyndromeCésar EscalanteNo ratings yet
- Guidelines For The Management of Glucocorticoids During The Peri OperativeDocument10 pagesGuidelines For The Management of Glucocorticoids During The Peri OperativeCésar EscalanteNo ratings yet
- Traditional Yang Family Tai Chi Chuan Senior Form 26 MovementsDocument5 pagesTraditional Yang Family Tai Chi Chuan Senior Form 26 MovementsCésar EscalanteNo ratings yet
- Traditional Yang Family Tai Chi Chuan Essential Form 22 MovementDocument5 pagesTraditional Yang Family Tai Chi Chuan Essential Form 22 MovementCésar EscalanteNo ratings yet
- HHS Public AccessDocument35 pagesHHS Public AccessBudi PutraNo ratings yet
- Diagnosis and Management of Adrenal InsufficiencyDocument29 pagesDiagnosis and Management of Adrenal InsufficiencyCésar EscalanteNo ratings yet
- The Effects Induced by Spinal Manipulative Therapy On The Immune and Endocrine SystemDocument12 pagesThe Effects Induced by Spinal Manipulative Therapy On The Immune and Endocrine SystemCésar EscalanteNo ratings yet
- COVID-19 and The Endocrine System Exploring The Unexplored PDFDocument5 pagesCOVID-19 and The Endocrine System Exploring The Unexplored PDFDiego CoronelNo ratings yet
- AmenorrheaDocument11 pagesAmenorrheaisaNo ratings yet
- The Physiology of Endocrine Systems With AgeingDocument24 pagesThe Physiology of Endocrine Systems With AgeingCésar EscalanteNo ratings yet
- Hypothalamic Amenorrhea and The Long-Term Health ConsequencesDocument12 pagesHypothalamic Amenorrhea and The Long-Term Health ConsequencesCésar EscalanteNo ratings yet
- Polycystic Ovary SyndromeDocument17 pagesPolycystic Ovary SyndromeCésar EscalanteNo ratings yet
- Drugs That May Worsen Myasthenia GravisDocument1 pageDrugs That May Worsen Myasthenia GravisyulianitadewiNo ratings yet
- Hypertension and AcromegalyDocument26 pagesHypertension and AcromegalyCésar EscalanteNo ratings yet
- 2 PDFDocument6 pages2 PDFCésar EscalanteNo ratings yet
- A Consensus Statement On Acromegaly Therapeutic OutcomesDocument10 pagesA Consensus Statement On Acromegaly Therapeutic OutcomesCésar EscalanteNo ratings yet
- Traditional Chinese Medicine Combined With Conventional Therapy For Female Kidney Stone: A Protocol For Systematic Review.Document5 pagesTraditional Chinese Medicine Combined With Conventional Therapy For Female Kidney Stone: A Protocol For Systematic Review.César EscalanteNo ratings yet
- The Effect of High-Dose Vitamin C On Biochemical Markers of Myocardial Injury in Coronary Artery Bypass SurgeryDocument8 pagesThe Effect of High-Dose Vitamin C On Biochemical Markers of Myocardial Injury in Coronary Artery Bypass SurgeryCésar EscalanteNo ratings yet
- The Tailgate Study: Differing Metabolic Effects of A Bout of Excessive Eating and DrinkingDocument36 pagesThe Tailgate Study: Differing Metabolic Effects of A Bout of Excessive Eating and DrinkingCésar EscalanteNo ratings yet
- 2 PDFDocument6 pages2 PDFCésar EscalanteNo ratings yet
- Correspondence on COVID-19 cytokine storm syndromes and immunosuppressionDocument2 pagesCorrespondence on COVID-19 cytokine storm syndromes and immunosuppressionCésar EscalanteNo ratings yet
- Correspondence on COVID-19 cytokine storm syndromes and immunosuppressionDocument2 pagesCorrespondence on COVID-19 cytokine storm syndromes and immunosuppressionCésar EscalanteNo ratings yet
- 3 - Human Sexuality and ReproductionDocument15 pages3 - Human Sexuality and ReproductionLucas JelmarNo ratings yet
- Uterine Fibroid - Viva VoceDocument77 pagesUterine Fibroid - Viva VoceK Haynes Raja100% (1)
- 40 Mistakes Men Make While Having Sex With WomenDocument3 pages40 Mistakes Men Make While Having Sex With WomenJill Camacho100% (2)
- Portofolio Dr. Irwin Fitriansyah Maret-April 2019Document18 pagesPortofolio Dr. Irwin Fitriansyah Maret-April 2019Irwin FitriansyahNo ratings yet
- Virginity Test Corruption PresentationDocument8 pagesVirginity Test Corruption PresentationNovita AinunNo ratings yet
- Curriculum VitaeDocument12 pagesCurriculum VitaeAnonymous 3FCoQaTukNo ratings yet
- Pelvic Examination: Liezel B. Cauilan MSN, MSTDocument25 pagesPelvic Examination: Liezel B. Cauilan MSN, MSTSIR ONENo ratings yet
- Ob10 Abnormal LabourDocument76 pagesOb10 Abnormal LabourFazzril HasmiNo ratings yet
- 4-. Revision Notes of Lecture OneDocument104 pages4-. Revision Notes of Lecture OneHasan DahamshehNo ratings yet
- Fhsis 1ST Quarter 2018Document29 pagesFhsis 1ST Quarter 2018Josette Mae AtanacioNo ratings yet
- ASRH in Emergencies - SlidesDocument30 pagesASRH in Emergencies - Slidesꓰꓡꓡꓰꓠ ꓓꓖꓰꓠꓰꓣꓰꓢꓢNo ratings yet
- The Gynaecological ExaminationDocument3 pagesThe Gynaecological ExaminationpogimudaNo ratings yet
- Childless MarriageDocument3 pagesChildless MarriageJeremy YoungNo ratings yet
- Yoshino, K. (2000) - The Epistemic Contract of Bisexual Erasure. Stanford Law Review, 52 (2), 353-461.Document110 pagesYoshino, K. (2000) - The Epistemic Contract of Bisexual Erasure. Stanford Law Review, 52 (2), 353-461.thinkofanumberNo ratings yet
- Reflection Essay For 2Document2 pagesReflection Essay For 2api-640132814No ratings yet
- Medad Andrology Special Note NMT13 PDFDocument70 pagesMedad Andrology Special Note NMT13 PDFSelim TarekNo ratings yet
- Multiple Choice Questions on Androgen Production and EffectsDocument4 pagesMultiple Choice Questions on Androgen Production and EffectsDrFarah Emad AliNo ratings yet
- Promotion OBGYNDocument30 pagesPromotion OBGYNAloah122346No ratings yet
- Sex, Marriage & ParenthoodDocument63 pagesSex, Marriage & ParenthoodAnselm JimohNo ratings yet
- S1 IS 2nd Term - Mid Term Test (U4 Cells and Human Reproduction) - 2020-2021 - AnswersDocument4 pagesS1 IS 2nd Term - Mid Term Test (U4 Cells and Human Reproduction) - 2020-2021 - Answerscody cheungNo ratings yet
- A Case Report of HELLP SyndromeDocument4 pagesA Case Report of HELLP SyndromeEditor_IAIMNo ratings yet
- Polyhydramnios CASE STUDY: Download NowDocument14 pagesPolyhydramnios CASE STUDY: Download NowJv LalparaNo ratings yet
- On The Sexual Intercourse Drawings of Leonardo Da VinciDocument4 pagesOn The Sexual Intercourse Drawings of Leonardo Da VinciCarlo Bugli Restauri100% (1)
- DystociaDocument8 pagesDystociaCylin Dadural100% (1)
- Spanish InsultsDocument5 pagesSpanish InsultsAlex D.50% (2)
- Practical Apporoach To UttarbastiDocument19 pagesPractical Apporoach To UttarbastiMadhura PhadtareNo ratings yet
- HysterosDocument17 pagesHysterosAnto PopaNo ratings yet