Professional Documents
Culture Documents
Articulo Sesiones 3 Bueno
Uploaded by
Moy VillanuevaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Articulo Sesiones 3 Bueno
Uploaded by
Moy VillanuevaCopyright:
Available Formats
Effects of a selective vasopressin V
2
receptor antagonist, satavaptan,
on ascites recurrence after paracentesis in patients with cirrhosis
q
Florence Wong
1,
*
, Pere Gines
2
, Hugh Watson
3
, Yves Horsmans
4
, Paolo Angeli
5
, Paul Gow
6
,
Pascal Minini
3
, Mauro Bernardi
7
1
Department of Medicine, University of Toronto, Canada;
2
Hospital Clinic, University of Barcelona, Institut dInvestigacions Biomdiques
August Pi-Sunyer (IDIBAPS), CIBER de Enfermedades Hepticas y Digestivas (CIBEREHD), Barcelona, Catalunya, Spain;
3
Internal
Medicine, Clinical Development, Sano-Aventis R&D, Chilly-Mazarin, France;
4
Saint-Luc University Hospital, Brussels, Belgium;
5
University of
Padova, Italy;
6
Austin Hospital, University of Melbourne, Australia;
7
Department of Internal Medicine, University of Bologna, Italy
See Editorial, pages 225227
Background & Aims: Cirrhotic patients with recurrent ascites
frequently require paracentesis despite diuretic therapy. Vaso-
pressin receptor antagonists, by increasing free water clearance,
may reduce the recurrence of ascites. To investigate the effects
of the addition of a vasopressin V
2
receptor antagonist, satavap-
tan, to 100 mg spironolactone on ascites recurrence after a large
volume paracentesis in patients with liver cirrhosis irrespective
of the presence of hyponatraemia.
Methods: One hundred and fty one cirrhotic patients with
recurrent ascites with or without hyponatraemia, and normal
to mildly abnormal renal function were randomised in a dou-
ble-blind study to receive either 5 mg (n = 39), 12.5 mg (n = 36),
25 mg (n = 40) of satavaptan or placebo (n = 36) for 12 weeks.
Their ChildPugh scores were 9.2 1.3, 8.7 1.7, 8.8 1.3, and
9.0 1.5, respectively.
Results: Median time to rst paracentesis was 23, 26, and
17 days with satavaptan 5, 12.5, and 25 mg, respectively, versus
14 days with placebo (ns for all doses). The frequency of para-
centeses was decreased signicantly (p < 0.05) in all satavaptan
groups versus placebo. Mean increase in ascites was
2.82 0.48 L/week for placebo versus 2.12 0.40, 2.14 0.33,
and 2.06 0.40 L/week for the 5, 12.5, and 25 mg of satavaptan,
respectively (ns for all doses). Similar numbers of patients expe-
rienced major adverse events in all groups. Increases in serum
creatinine, orthostatic changes in systolic pressure and thirst
were more common with satavaptan.
Conclusions: Satavaptan has the potential to reduce recurrence
of ascites after a large volume paracentesis at doses from 5 to
25 mg in cirrhotic patients with ascites.
2010 European Association for the Study of the Liver. Published
by Elsevier B.V. All rights reserved.
Introduction
The development of ascites in the natural history of cirrhosis
heralds a worsening of the prognosis to 50% survival at 2 years
[1], and this deteriorates to 3050% at 1 year when the ascites
becomes refractory to medical therapy [2,3]. Traditionally,
the management of ascites consists of dietary sodium restric-
tion, judicious use of diuretics, and large volume paracentesis
(LVP) [4]. Although repeated LVPs have been shown to be safe
[5,6], frequent LVPs involve signicant medical manpower and
inconvenience to the patients. Other treatment options, includ-
ing the insertion of a transjugular intrahepatic portosystemic
stent shunt, are only suitable for carefully selected patients [7].
Vasopressin V
2
receptor antagonists are aquaretic agents. By
antagonising the antidiuretic effects of vasopressin at the V
2
receptor located in the renal collecting duct, they increase free
water clearance, and thus may be helpful in mobilising excess
water in conditions associated with water retention including cir-
rhosis [810]. The use of V
2
receptor antagonists in cirrhosis with
ascites has be shown to be safe and efcacious, with a dose-
dependent increase in urinary volume and a reduction in urinary
osmolality [8,9]. Furthermore, while cirrhotic patients with asci-
tes on placebo gained weight, those on aquaretic agents main-
tained their weight with the lower doses, and clearly lost
weight with the higher doses [8,9].
Satavaptan is a selective V
2
receptor antagonist, which
increased urine output when administered with spironolactone in
cirrhotic patients with ascites and hyponatraemia [11], associated
Journal of Hepatology 2010 vol. 53
j
283290
Keywords: Cirrhosis; Ascites; V
2
receptor antagonist; Large volume paracentesis.
Received 17 January 2010; received in revised form 22 February 2010; accepted 23
February 2010; available online 24 May 2010
DOI of original article: 10.1016/j.jhep.2010.04.003.
q
The study was registered on a public clinical trial registry website, www.Clin-
icalTrials.org, number NCT 00501384.
*
Corresponding author. Address: 9th oor, North Wing, Room 983, Toronto
General Hospital, 200 Elizabeth Street, Toronto, Ontario, Canada M5G2C4. Tel.: +1
416 340 3834; fax: +1 416 340 5019.
E-mail address: orence.wong@utoronto.ca (F. Wong).
Abbreviations: AST, aspartate transaminase; ALT, alanine transaminases; ALP,
alkaline phosphatase; CI, condence interval; dDAVP, 1-desamino-8-D-arginine
vasopressin; INR, international normalized ratio; ITT, intention to treat; LVP, large
volume paracentesis; MELD, model for end-stage liver disease; QTcF, QT interval
corrected by the Fridericia formula; TIPS, transjugular intrahepatic portosystemic
stent shunt.
Research Article
with improved ascites control over a 14-day period [11]. It is pos-
tulated that satavaptan, together with spironolactone, is able to
enhance ascites reduction by increasing free water excretion in
patients with cirrhosis irrespective of the presence of hyponatra-
emia over a longer time period.
Therefore, the aim of this study was to assess the efcacy of
satavaptan at three xed doses on ascites recurrence after an
LVP in cirrhotic patients with recurrent ascites being treated with
spironolactone over a 12-week period.
Patients and methods
Patients
Cirrhotic patients with ascites, with or without hyponatraemia, who had at least
one LVP in the previous 3 months, as well as undergoing a LVP on the day of
entry, each of P4 L, were assessed for enrolment.
Exclusion criteria were serum bilirubin >135 lmol/L, international normal-
ized ratio (INR) >3.0, serum creatinine >175 lmol/L, serum sodium >142 mmol/
L, serum potassium P5.5 mmol/L, or systolic arterial pressure of <80 mmHg.
Clinical exclusion criteria were signicant cardiac diseases such as recent myo-
cardial infarction (61 month), or prolonged QT interval corrected by the Frider-
icia formula (QTcF) of P500 ms; complications of liver cirrhosis such as recent
infection including spontaneous bacterial peritonitis, or gastrointestinal bleed
(610 days from randomisation), or ongoing hepatic encephalopathy of >grade
1 [12], or known hepatocellular carcinoma of >5 cm in maximal diameter for
1 lesion or <3 cm for each of 63 lesions. Patients who had a liver transplant,
or a portosystemic shunt were not eligible, as were patients with non-cirrhotic
ascites.
Methods
The study was designed and developed by the Internal Medicine team at Sano-
Aventis, together with Drs. Wong and Gines. Dr. Wong prepared the rst and sub-
sequent drafts of the manuscript with Dr. Bernardi. The data are held and ana-
lyzed by Sano-Aventis, but accessible to Drs. Wong and Gines. Decisions
relating to the nal draft were made by Drs. Wong and Watson.
Ethics approval was obtained from all participating institutions. All patients
gave written informed consent. The study was registered on a public clinical trial
registry website, www.ClinicalTrials.org, number NCT 00501384.
This was a double-blind, randomised, placebo-controlled, parallel-group
study assessing the efcacy of three xed doses of satavaptan, 5, 12.5, and
25 mg versus placebo, plus low-dose spironolactone, in the prevention of ascites
recurrence after a LVP of P4 L. On day 1, whilst inpatients, all patients under-
went a complete physical examination, and a LVP of P4 L, plus albumin infusion
at 68 g/L of ascitic uid removed [4], together with complete biochemistry, a
complete blood count and an electrocardiograph to exclude prolonged QTc. A
24-h urine collection was done to determine urinary volume, osmolality and elec-
trolyte excretion. The following day (day 1), eligible patients were randomised to
receive a single daily dose of either 5, 12.5 or 25 mg of satavaptan or placebo, plus
100 mg spironolactone per day for a total of 12 weeks. A central randomisation
list was generated electronically at Sano-Aventis with each site receiving a block
of equally distributed sealed treatment groups. At randomization, the lowest
available treatment number at that particular site was selected for the patient,
thus ensuring a random allocation of patients to each treatment group.
On days 13, patients were assessed clinically daily, as well as for serum elec-
trolytes, renal function, serum and urinary osmolality, urinary volume and uri-
nary electrolyte excretion. Patients were discharged on day 3, if possible.
Outpatient visits occurred on days 7, 14, 28, 56, and 84, when the same laboratory
parameters that were assessed during the rst 3 days were repeated. 24-h urine
collections were only done on days 28 and 84. Plasma vasopressin, supine aldo-
sterone and supine plasma renin levels were measured on day 1 prior to study
medication, and again on days 7 and 84. An electrocardiograph was repeated
on days 2, 7, 28, and 84 of the study. LVP was permitted, plus albumin infusion
at a dose of 68 g/L of ascitic uid removed if patients had gained P4 kg in
weight, accompanied by tense ascites. Patients were maintained on a sodium
restriction of 688 mmol/day and were instructed to drink water as required by
thirst. Throughout the study, patients were assessed for electrolyte abnormalities,
renal dysfunction, dehydration and thirst.
The co-primary endpoints were time to the rst paracentesis, and increase in
ascites as assessed by the increase in body weight and cumulative volume of asci-
tes removed during the 12-week study period. Secondary endpoint was frequency
of paracentesis. Subgroup analysis of patients with refractory ascites was
performed.
Laboratory assays
Serumand urinary electrolytes, complete blood count, INR, and liver function tests
were performed using standard automated laboratory techniques. Blood samples
for vasopressin, plasma renin, and aldosterone concentrations were collected on
ice. Plasma was separated by refrigerated centrifugation and stored at 70 C until
assay. Serumand urinary osmolality were measured with a freezing point osmom-
eter. Plasma renin was measured using an immuno-chemiluminometric assay
(Nichols Kit & Instrument, San Clemente, CA). Plasma aldosterone (Coat-A-Count
Aldosterone kit, Diagnostic Products Corporation, Los Angeles, CA), and vasopres-
sin (Quest Diagnostics, Madison, NJ) were assayed by radioimmunoassay.
Sample size calculation and statistical analysis
Sample size calculations were based on the two co-primary endpoints. For the
rst primary endpoint, it was assumed that the time to rst paracentesis was
>12 weeks in 20% of placebo patients, versus 60% of satavaptan patients, the num-
ber required for each group would be 33 patients, or 132 patients for the four
study groups. For the second primary endpoint, it was assumed that placebo
patients would gain 4 kg more ascites over the 12-week period versus satavaptan
patients. The number required for each group would be 35 patients, or 140
patients for the four study groups. The primary analysis was conducted on the
intent-to-treat (ITT) population. Cumulative mean number of paracenteses as a
function of time was estimated using the NelsonAalen estimator (an extension
of the KaplanMeier estimator for recurrent events). Comparisons between treat-
ment groups were performed using a Cox model for recurrent events with robust
estimate of the variance (sandwich estimate) [13]. Change from baseline in 24-h
urine volume was analysed using an analysis of covariance with treatment group
as main factor and baseline value as covariate. Categorical variables were com-
pared using the Fishers exact test. Calculations were performed with the statis-
tical program SAS 8.2 (Cary, NC, USA). Results are presented as mean SD.
Median values with ranges were presented for nonparametric variables.
p < 0.05 was considered statistically signicant.
Results
Of 173 potentially suitable patients who were consented and
screened between April 2004 and February 2005, 20 patients did
not meet inclusion/exclusion criteria. One patient withdrew con-
sent, and one patient did not return for randomisation. Therefore,
151 patients were entered into the study, randomised to receive
placebo (n = 36), 5 mg (n = 39), 12.5 mg (n = 36) or 25 mg
(n = 40) of satavaptan (Fig. 1). Patient demographics, baseline lab-
oratory parameters are presented in Tables 1 and 2, respectively.
Control of ascites
Ascites was previously present in all patients for a mean period of
>1 year (placebo: 16.7 17.3 months, satavaptan 5 mg: 19.5
20.2 months, 12.5 mg: 27.6 30.9 months, 25 mg: 33.1 36.0
months), witha previous medianfrequencyof LVPof every15 days
(Table 1). The mediantime tothe rst LVPwas increasedto23 days
[95% condence interval (CI): 16, 31 days], 26 days [95% CI, 16,
56 days] and 17 days [95% CI: 14, 28 days] with 5, 12.5, and
25 mg of satavaptan, respectively, versus 14 days with placebo
[95% CI: 8, 29 days] (NS for all doses). The mean increase in ascites
was 2.82 0.48 L/week for placebo versus 2.12 0.40, 2.14 0.33,
and 2.06 0.40 L/week for the 5, 12.5, and 25 mg of satavaptan
respectively (NS for all doses), with respective relative risks for a
rst repeat LVPof 0.69, 0.60, and0.63for thethreesatavaptandoses.
Over the 12-week study period, the total number of LVPs,
adjusted for the duration of assessment, was signicantly
reduced at each dose of satavaptan: 3.11 LVPs (p = 0.026), 2.95
LVPs (p = 0.018) and 2.72 LVPs (p = 0.017) for 5, 12.5, and
Research Article
284 Journal of Hepatology 2010 vol. 53
j
283290
Screened patients
n = 173
Screened failures
n = 22
Randomized patients
n = 151
Patients who received
double blind treatment
n=151
Placebo
n = 36
Satavaptan
(5 mg/day)
n = 39
Satavaptan
(12.5 mg/day)
n = 36
Satavaptan
(25 mg/day)
n = 40
Completed
20 (56%)
Completed
19 (49%)
Completed
27 (75%)
Completed
28 (70%)
Discontinued = 16
: Lack of efficacy = 3
: Adverse event = 5
: Poor compliance = 2
: Subject's request = 4
: Other reasons = 2
Discontinued = 12
: Lack of efficacy = 2
: Adverse event = 9
: Poor compliance = 0
: Subject's request = 1
: Other reason = 0
Discontinued = 20
: Lack of efficacy = 4
: Adverse event = 13
: Poor compliance = 1
: Subject's request = 0
: Other reason = 2
Discontinued = 9
: Lack of efficacy = 3
: Adverse event = 3
: Poor compliance = 1
: Subject's request = 1
: Other reason = 1
Fig. 1. Distribution of patients who were screened for enrollment into the study.
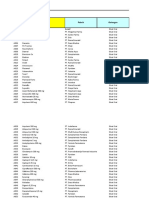
Table 1. Patient demographics.
Satavaptan
Placebo 5 mg 12.5 mg 25 mg
n 36 39 36 40
Age (y) 60 9 59 9 59 9 60 11
M/F 26/10 32/7 28/8 29/11
Aetiology of cirrhosis
Alcohol 26 30 29 26
Hepatitis B 2 4 4 2
Hepatitis C 9 8 6 9
Others 4 2 2 5
ChildPugh score 9.0 1.5 9.2 1.3 8.7 1.7 8.8 1.3
MELD score 14.2 4.3 15.6 4.2 14.0 3.9 14.2 3.2
Ascites classication
Refractory [4] 22 24 26 22
Recidivant 13 14 10 17
Neither 1 1 0 1
Median interval between paracenteses (days) 15 13 15 16
Recidivant ascites: recurrent ascites requiring large volume paracentesis for >3 times per year.
JOURNAL OF HEPATOLOGY
Journal of Hepatology 2010 vol. 53
j
283290 285
25 mg, respectively versus 4.32 LVPs for placebo. The relative
risks for any paracentesis were 0.69, 0.66, and 0.63, respectively
for the three satavaptan doses (Fig. 2). Allowing for drop-outs, the
KaplanMeier analysis estimated that 2025% of satavaptan
patients versus 11% of placebo patients had no further paracent-
eses during the 12-week study period.
For the subpopulation of patients with refractory ascites, the
mean number of paracenteses over the 12-week period was also
signicantly reduced for the 5 mg (p = 0.015) and for the 12.5 mg
group (p = 0.017), though not for the 25 mg group (p = 0.103). In
addition, the relative risks for requiring a rst paracentesis in this
subpopulation of patients were 0.51 (p = 0.049), 0.47 (p = 0.023),
and 0.70 (ns) for the three satavaptan doses, respectively, when
compared with placebo.
Renal function and sodium and water homeostasis
Throughout the study, there were no signicant changes in the
mean serum creatinine, serum sodium or urinary sodium excre-
tion (Table 3). At entry, there were 61 patients who had hypona-
traemia (Placebo: 14, 5 mg: 17, 12.5 mg: 11, 25 mg: 19 patients).
All hyponatraemic patients on satavaptan, irrespective of dose,
had a signicant increase in serum sodium by day 7 compared
to the placebo group. Since the majority of patients in this study
Table 2. Baseline laboratory data of study patients.
Satavaptan
Placebo 5 mg 12.5 mg 25 mg
n 36 39 36 40
Serum sodium (N = 135145 mmol/L) 136 4 133 6 135 5 134 5
Serum potassium (N = 3.54.5 mmol/L) 4.2 0.7 4.1 0.6 4.2 0.6 4.5 0.6
Serum creatinine (N <100 lmol/L) 97 30 94 28 100 27 100 28
Haemoglobin (N = 8.111.2 mmol/L for men 7.49.9 mmol/L for women) 6.9 1.3 6.7 1.4 7.2 1.0 6.9 3.7
INR (N = 1.01.2) 1.5 0.4 1.5 0.3 1.4 0.3 1.4 0.3
AST (N <35 IU/L) 49 31 53 24 44 22 54 38
ALT (N <40 IU/L) 29 17 33 24 24 11 33 30
ALP (N <110 IU/L) 149 98 166 96 195 189 184 174
Serum albumin (N = 3550 g/L) 30 6 29 6 30 5 30 5
Serum bilirubin (N <17 lmol/L) 39 28 49 30 35 21 33 20
Urinary volume (ml) 1015 455 1214 784 1202 713 1283 749
QTcF (ms) 412 31 417 27 420 27 420 26
INR: international normalized ratio; AST: aspartate transaminase; ALT: alanine transaminase; ALP: alkaline phosphatase; QTcF: QT interval corrected by Fridericias
formula.
Table 3. Systemic haemodynamics, renal function, and sodium and water homeostasis in all study patients.
Satavaptan
Placebo 5 mg 12.5 mg 25 mg
n 36 39 36 40
Systolic blood pressure (N = 110140 mm Hg)
Baseline 116 14 116 16 119 17 119 19
Month 1 116 14 122 10 118 14 121 18
Month 3 117 13 126 18 121 15 119 14
Diastolic blood pressure (N = 6090 mm Hg)
Baseline 69 10 68 11 73 11 71 13
Month 1 71 9 72 7 72 12 71 10
Month 3 71 9 73 10 75 13 73 9
Serum [Na] (N = 135145 mmol/L)
Baseline 136 4 133 6 135 5 134 5
Month 1 136 4 134 5 136 6 137 4
Month 3 135 5 136 4 136 4 137 4
Urinary [Na] (mmol/hr)
Baseline 2.2 2.3 2.6 3.5 2.7 2.9 2.4 2.8
Month 1 3.7 5.5 3.2 3.1 3.2 3.1 3.2 3.4
Month 3 2.9 3.2 2.8 3.2 4.2 3.1 3.3 3.1
Serum osmolality (N = 285298 mOsmol/kg of H
2
O)
Baseline 291 9 287 18 289 11 283 11
Month 1 290 14 289 17 288 12 294 14
Month 3 285 23 290 12 292 12 297 14
Urinary osmolality (mOsmol/kg of H
2
O)
Baseline 522 215 544 184 461 185 420 175
Month 1 533 188 364 158
a
285 138
a
203 101
a
Month 3 519 198 452 201 299 134
a
227 106
a
Serum creatinine (N <110 lmol/L)
Baseline 97 30 94 28 100 27 100 28
Month 1 93 29 93 36 101 27 102 35
Month 3 94 32 95 36 99 38 98 37
a
p <0.01 compared to baseline.
Research Article
286 Journal of Hepatology 2010 vol. 53
j
283290
were normonatraemic at entry, there was no signicant increase
in serum sodium overall (Table 3).
However, renal failure, when dened by a rise in serum creat-
inine of >50% from baseline with a value P133 lmol/L, occurred
at least once in 14.8% of satavaptan patients versus 2.7% for pla-
cebo. These patients, especially in the 25 mg satavaptan group,
generally had poorer baseline renal function as indicated by
serum creatinine and estimated GFR compared with those not
experiencing such an event. The peak serum creatinine exceeded
200 lmol/L in two patients on satavaptan 5 mg, two patients on
12.5 mg and four patients on 25 mg.
There was a signicant dose-dependent increase in urinary
volume at the end of the study compared with baseline in
patients receiving satavaptan (Fig. 3), associated with a
signicant reduction in urinary osmolality. The serum osmolality,
however, did not rise signicantly throughout the study (Table 3).
Hormonal levels
At baseline, plasma renin and aldosterone concentrations were
signicantly elevated, but these levels did not change signi-
cantly throughout the study. Plasma vasopressin levels decreased
in the placebo group, but signicant increases were observed in
all satavaptan groups, and appeared to be dose-related (Table 4).
Other adverse events
The overall incidence of adverse events did not differ markedly
between placebo and the satavaptan groups (Table 5).
Orthostatic hypotension (20 mm Hg), although more fre-
quent (16.7%) (Table 5) in satavaptan patients, were mostly
asymptomatic. Two symptomatic patients (one each in the
12.5 mg and 25 mg groups) recovered spontaneously without
being reported as adverse events. One of these patients was tak-
ing nadolol concomitantly. All patients with orthostatic hypoten-
sion completed the 12-week study without further hypotensive
episodes. Thirst was also a frequently reported adverse event in
satavaptan patients (13.9%), but in none of the placebo patients.
Other common adverse events included hyperkalaemia, the
development of hepatic encephalopathy and muscle cramps
(Table 5). The majority of patients, except 1 patient in the
12.5 mg group, recovered from their hyperkalaemia following
withdrawal of spironolactone, and withholding study medica-
tions with or without the administration of sodium polystyrene
sulfonate, or insulin or albumin. He had concomitant renal fail-
N at risk
M
e
a
n
c
u
m
u
l
a
t
i
v
e
n
u
m
b
e
r
o
f
p
a
r
a
c
e
n
t
e
s
i
s
5
4
3
2
1
0
36
39
36
40
Placebo
5 mg
12.5 mg
25 mg
36
39
36
38
31
34
36
36
31
32
34
33
28
29
34
33
24
26
33
30
23
24
32
29
22
22
32
28
22
21
32
28
22
20
28
28
22
19
28
28
20
19
28
28
17
15
25
24
0 7 14 21 28 35 42 49 56 63 70 77 84
p <0.05
Time since treatment start (days)
Placebo
5 mg
12.5 mg
25 mg
Fig. 2. Cumulative number of large volume paracentesis required per patient
with time. p <0.05 for all satavaptan groups compared with placebo.
25 mg Placebo 5 mg 12.5 mg
2
4
h
r
u
r
i
n
a
r
y
v
o
l
u
m
e
i
n
m
l
5000
4000
3000
2000
1000
0
End of Treatment
Baseline
Fig. 3. Twenty-four hour urinary volume at the beginning and at the end of
the study.
Table 4. Hormonal levels in all study patients.
Satavaptan
Placebo 5 mg 12.5 mg 25 mg
n 36 39 36 40
Plasma vasopressin (N = 0.912.3 pmol/L)
Baseline 2.7 (1.94, 3.35) 2.2 (1.84, 2.81) 2.2 (1.51, 3.13) 2.1 (1.51, 3.02)
Day 7 2.2 (1.51, 3.08)
a
3.3 (2.38, 4.54)
a
3.5 (2.38, 4.54)
a
4.0 (3.02, 5.94)
a
Month 3 1.9 (1.57, 2.33)
a
2.9 (2.27, 3.24)
a
3.8 (2.05, 5.83)
a
3.7 (2.70, 7.88)
a
Plasma renin (N = 229 mU/L)
Baseline 229 (81, 553) 298 (62, 582) 169 (72, 456) 201 (88, 489)
Day 7 322 (101, 530) 322 (77, 843) 230 (57, 575) 239 (68, 645)
Month 3 177 (92, 501) 301 (112, 697) 178 (72, 734) 211 (96, 554)
Plasma aldosterone (N = <0.440 nmol/L)
Baseline 1.29 (0.75, 3.41) 1.02 (0.45, 4.22) 1.11 (0.58, 2.22) 1.80 (0.89, 4.69)
Day 7 1.91 (1.00, 4.72) 1.94 (0.86, 4.94) 1.83 (1.14, 2.30) 2.05 (1.08, 6.05)
Month 3 1.52 (1.00, 2.33) 1.80 (0.92, 3.33) 1.36 (0.97, 2.03) 1.97 (1.14, 4.33)
Results are expressed as median and 25th and 75th percentiles.
a
p <0.05 compared with baseline.
JOURNAL OF HEPATOLOGY
Journal of Hepatology 2010 vol. 53
j
283290 287
ure. Hyperkalaemia led to the discontinuation of study medica-
tion in three patients (placebo: 2, 25 mg satavaptan: 1) Three
cases of hepatic encephalopathy were associated with other com-
plications of liver cirrhosis, and they all succumbed to their
advanced liver disease. Otherwise, the majority of patients recov-
ered with the administration of lactulose. Patients with muscle
cramps all recovered with symptomatic treatment. There was
no clear evidence of a dose-relationship in the frequency of any
events.
There were no QTcF values of >500 ms observed either in the
placebo or the satavaptan groups throughout the study.
Several patients (placebo: 2; satavaptan 5 mg: 1; 12.5 mg: 2;
25 mg: 2) had their study medication withheld for 1 day because
of a >8 mmol/L rise in serum sodium, which quickly returned to
normal following temporary discontinuation of study medica-
tion. All patients were able to resume study medication without
further problems. No withdrawal from the study occurred
because of persistent hypernatraemia.
Patient outcome
Overall, 57 patients discontinued the study early, for reasons
listed in Fig. 1. The median duration of study was 81, 68, 84,
and 84 days for placebo, 5, 12.5, and 25 mg satavaptan groups,
respectively.
Twelve patients died during the study period (placebo: 3,
5 mg: 2, 12.5 mg: 3 and 25 mg: 4) from sepsis (n = 3), liver failure
(n = 2), hepatorenal syndrome (n = 2), gastrointestinal hemor-
rhage (n = 1), cerebral vascular accident (n = 1), pancreatic carci-
noma (n = 1), biliary carcinoma (n = 1) and refractory anemia
(n = 1). There was no increase in mortality in the satavaptan ver-
sus placebo patients in this study.
Discussion
This study, in cirrhotic patients with recurrent ascites with or
without hyponatraemia, found that satavaptan, a vasopressin
V
2
receptor antagonist, in conjunction with low-dose spironolac-
tone, reduced the frequency of LVP over a 3-month period. The
two co-primary endpoints of time to rst LVP and accumulated
volume of ascites did not achieve statistical signicance, but
the relative risks for rst LVP were very consistent with those
for all LVPs over 3 months, and all were within the range of
0.600.69. The difference in statistical signicance is explained
by the greater statistical power achieved by counting all LVPs
instead of only the rst event. It might also be argued that the
reduction of all LVPs over 3 months is of greater clinical signi-
cance than the delay of only the rst LVP.
Excess sodium and water retention is pivotal in the patho-
physiology of ascites formation in cirrhosis [14]. The binding
of satavaptan, a selective vasopressin V
2
receptor antagonist,
to the V
2
receptor at the renal collecting tubule, blocks the ser-
ies of reactions that ultimately make the collecting tubule
impermeable to water [15], thereby inducing a diuresis. Intui-
tively, it seems unlikely that an aquaretic agent such as satavap-
tan, could effect a reduction in ascites accumulation. However,
the loss of a signicant volume of water induced by satavaptan
could lead to reduction in the intravascular volume. This could
be compensated for by an increase in oral uid intake and/or
activation of various physiological mechanisms to replenish
the effective intravascular volume. The fact that we did not
observe any signicant change in the systemic haemodynamics,
in serum osmolality, nor in plasma renin levels, suggests that
the intravascular volume was maintained despite large diuresis,
even with the 25 mg dose of satavaptan. We postulate that this
was achieved partly through an increased reabsorption of ascitic
uid, hence the reduction in ascites accumulation and a
decrease in the frequency of paracentesis in the satavaptan
groups, and partly through an increased movement of water
from the interstitial and/or intracellular compartment to the
vascular compartment. It should be noted that despite higher
doses of satavaptan inducing a higher urine output, and pre-
sumably a greater degree of intravascular volume contraction,
there was not a dose response in the reduction in ascites. This
may be related to the fact that reabsorption of ascitic uid is
relatively xed [16], maximally at approximately 400 mL/day.
Since these patients had free access to uid intake, the decit
in the intravascular volume induced by satavaptan presumably
was replenished by increasing oral uid intake. The corollary
is that increasing aquaretic doses may not yield a greater reduc-
tion of ascites despite a greater urinary water excretion. Fur-
thermore, patients receiving aquaretic agents should not be
placed on uid restriction.
It is possible that satavaptan was able to effect a reduction in
ascites by inuencing other pathogenetic mechanisms of ascites
formation. Circulating vasopressin stimulates sodium reabsorp-
tion in the collecting duct by increasing the activity of the amil-
oride-sensitive epithelial sodium channel. 1-Desamino-8-D-
arginine vasopressin, a potent vasopressin receptor agonist, has
been shown to markedly reduce urine ow rate and sodium
excretion in healthy individuals [17], and the use of satavaptan
in normal Wistar rats was associated with an increase in urinary
sodium excretion [18]. The urinary sodium excretion in our study
cohort remained relatively unchanged throughout the study.
Table 5. Adverse events overview and incidence of selected types of adverse events reported 67 days after last dose of study medication.
Satavaptan
Placebo 5 mg 12.5 mg 25 mg
n 36 39 36 40
Any adverse event 28 34 26 28
Any serious adverse event 13 18 13 16
Death 3 2 3 4
Episodes of hepatic encephalopathy 3 7 4 4
Bacterial peritonitis 3 0 1 2
Esophageal variceal bleeding 1 3 2 0
Muscle cramps 1 4 2 6
Thirst 0 5 6 5
Hyperkalaemia (serum [K] >5.5 mmol/L) 7 10 11 7
Orthostatic hypotension (>20 mmHg) 1 9 7 3
Research Article
288 Journal of Hepatology 2010 vol. 53
j
283290
However, the increased sodium excretion with satavaptan is
transient [18], and therefore may not have been captured by
intermittent urinary collections. It remains a possibility that the
sodium excretory effects of satavaptan may have contributed to
the reduction in ascites in these patients.
Irrespective of which mechanisms are involved, the fact that
satavaptan, when added to low-dose spironolactone over a 3-
month period, was able to effect a reduction in ascites accumula-
tion as measured by LVP frequency, suggests that it could be used
as adjunctive therapy for the management of ascites in cirrhosis,
including patients with refractory ascites [4]. This has signicant
clinical implications, as cirrhotic patients with ascites of varying
severity may potentially have their ascites better managed with
the addition of an aquaretic agent irrespective of serum sodium
concentration. It should be noted that the xed low-dose of spiro-
nolactone, which was necessary to run a controlled clinical trial
without introducing potentially confounding effects related to
the administration of various types and doses of diuretics, does
not represent the most appropriate approach to the treatment of
cirrhotic ascites. Thus, future studies will need to test whether
the addition of satavaptan to individually optimised regimens of
natriuretic agents will yield the same results.
The safety prole of satavaptan in this study also suggests that
it may be an attractive adjunctive therapy. Although a signicant
number of patients died during the study period, most of these
patients died from complications of cirrhosis, with mortality rate
not signicantly different from what has been observed in
patients with advanced cirrhosis [1]. Furthermore, patients on
various doses of satavaptan did not have signicantly more major
adverse events compared with placebo. Thirst was clearly treat-
ment related. However, as reported above, despite increased
urine volume with excess water, none of the patients taking
satavaptan experienced dehydration, or hypovolaemia. This is
because all patients had free access to water, and were advised
to drink when thirsty. Therefore, only a few patients had their
satavaptan dose temporarily withheld because of hypernatra-
emia, unlike another aquaretic [9], thereby improving patient
compliance. However, one must be cognizant of the fact that
there is a potential for dehydration with satavaptan, as the
proportion of patients with increased serum creatinine was
higher in the satavaptan patients than in the placebo group.
Therefore, careful monitoring of renal function is required with
aquaretic therapy.
There were several episodes of hyperkalaemia with the com-
bination of spironolactone and satavaptan, although this was not
signicantly higher than in the placebo group. This may be
related to the fact that vasopressin regulates the NaKATPase
and NaKCl cotransporter activity [19], which is crucial for
sodium reabsorption and potassium excretion in the distal neph-
ron [20]. The use of a V
2
receptor antagonist has been shown to
decrease NaKATPase expression and activity in experimental
animals [19]. Since potassium excretion in the collecting duct
usually occurs by active uptake across the basolateral membrane
by NaKATPase, and passive diffusion across the apical mem-
brane into the lumen [21], decreasing NaKATPase expression
by satavaptan would effectively reduce potassium secretion and
have the same clinical effects as aldosterone blockade. Therefore,
patients on a combination of aldosterone antagonist and V
2
receptor antagonist should have their electrolytes monitored reg-
ularly. However, in the doses studied, the combination appears to
be safe. There was an increased incidence of muscle cramps or
hepatic encephalopathy, unrelated to hyperkalaemia, in the sat-
avaptan patients. It would be prudent to monitor for these
adverse events and administer prompt corrective therapies.
In summary, the addition of xed doses of a V
2
receptor antago-
nist, satavaptan, to low-dose spironolactone in cirrhotic patients
with ascites requiring frequent LVPs may improve the control of
ascites, as the total number of LVPs over 3 months was signicantly
decreased at all doses tested. The safety of satavaptan appeared
acceptable at all of the doses tested and any increase in renal dys-
function appeared to be mild. Careful and regular monitoring of
electrolytes and renal function is advisable. In conclusion, the V
2
receptor antagonist, satavaptan, added to low-dose spironolactone,
has thepotential toreducerecurrenceof ascites at doses intherange
of 525 mg in cirrhotic patients withrecurrent or refractory ascites.
Competing interests
Florence Wong and Pere Gines are consultants for Sano-Aventis,
Hugh Watson and Pascal Minini are employees of Sano-Aventis,
Yves Horsmans, Paolo Angeli, Paul Gow and Mauro Bernardi
report no conict of interest.
Funding
The study was sponsored by Sano-Aventis.
Acknowledgment
CIBEREHD is supported by the Instituto de Salud Carlos III, Spain.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in
the online version, at doi:10.1016/j.jhep.2010.02.036.
References
[1] DAmico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic
indicators of survival in cirrhosis: a systematic review of 118 studies. J
Hepatol 2006;44:217231.
[2] Planas R, Montoliu S, Balleste B, Rivera M, Miquel M, Masnou H, et al. Natural
history of patients hospitalized for management of cirrhotic ascites. Clin
Gastroenterol Hepatol 2006;4:13851394.
[3] Moreau R, Delegue P, Pessione F, Hillaire S, Durand F, Lebrec D, et al. Clinical
characteristics and outcome of patients with cirrhosis and refractory ascites.
Liver Int 2004;24:457464.
[4] Moore KP, Wong F, Gines P, Ochs A, Bernardi M, Salerno F, et al. The
management of ascites report on the consensus conference of the
International Ascites Club. Hepatology 2003;38:258266.
[5] Gines P, Arroyo V, Quintero E, Planas R, Bory F, Cabrera J, et al. Comparison of
paracentesis and diuretics in the treatment of cirrhotics with tense ascites.
Results of a randomized study. Gastroenterology 1987;93:234241.
[6] Salerno F, Badalamenti S, Incerti P, Tempini S, Restelli B, Bruno S, et al.
Repeated paracentesis and i.v. albumin infusion to treat tense ascites in
cirrhotic patients. A safe alternative therapy. J Hepatol 1987;5:102108.
[7] Wong F. The use of TIPS in chronic liver disease. Ann Hepatol 2006;5:515.
[8] Gerbes AL, Gulberg V, Gines P, Decaux G, Gross P, Gandjini H, et al. Therapy
of hyponatremia in cirrhosis with a vasopressin receptor antagonist: a
randomized double-blind multicenter trial. Gastroenterology 2003;124:
933939.
[9] Wong F, Blei AT, Blendis LM, Thuluvath PJ. A vasopressin receptor antagonist
(VPA-985) improves serum sodium concentration in patients with hypona-
JOURNAL OF HEPATOLOGY
Journal of Hepatology 2010 vol. 53
j
283290 289
tremia: a multicenter, randomized, placebo-controlled trial. Hepatology
2003;37:182191.
[10] Udelson JE, McGrew FA, Flores E, Ibrahim H, Katz S, Koshkarian G, et al.
Multicenter, randomized, double-blind, placebo-controlled study on the
effect of oral tolvaptan on left ventricular dilation and function in patients
with heart failure and systolic dysfunction. J Am Coll Cardiol
2007;49:21512159.
[11] Gins P, Wong F, Watson H, Milutinovic S, Ruiz del Arbol L, Olteanu D, et al.
Effects of satavaptan, a selective vasopressin V
2
receptor antagonist, on
ascites and serum sodium concentration in patients with cirrhosis and
hyponatremia. Hepatology 2008;48:204213.
[12] Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT, et al.
Hepatic encephalopathy-denition, nomenclature, diagnosis, and quanti-
cation: nal report of the working party at the 11th World Congresses of
Gastroenterology, Vienna, 1998. Hepatology 2002;35:716721.
[13] Lawless JF, Nadeau C. Some simple robust method for the analysis of
recurrent events. Technometrics 1995;37:158168.
[14] Crdenas A, Arroyo V. Mechanisms of water and sodium retention in
cirrhosis and the pathogenesis of ascites. Best Pract Res Clin Endocrinol
Metab 2003;17:607622.
[15] Bonilla-Felix M. The development of water transport in the collecting duct.
Am J Physiol 2004;287:F1093F1101.
[16] Shear L, Ching S, Gabuzda GJ. Compartmentalization of ascites and edema in
patients with hepatic cirrhosis. N Engl J Med 1970;282:13911396.
[17] Bankir L, Fernandes S, Bardoux P, Bouby N, Bichet DG. Vasopressin-V
2
receptor stimulation reduces sodium excretion in healthy humans. J Am Soc
Nephrol 2005;16:19201928.
[18] Perucca J, Bichet DG, Bardoux P, Bouby N, Bankir L. Sodium excretion in
response to vasopressin and selective vasopressin receptor antagonists. J Am
Soc Nephrol 2008;19:17211731.
[19] Bertuccio CA, Ibarra FR, Toledo JE, Arrizurieta EE, Martin RS. Endogenous
vasopressin regulates NaKATPase and Na(+)K(+)Cl() cotransport-
er rbsc-1 in rat outer medulla. Am J Physiol Renal Physiol 2002;282:
F265F270.
[20] Rozansky DJ. The role of aldosterone in renal sodium transport. Semin
Nephrol 2006;26:173181.
[21] Giebisch G. Renal potassium transport: mechanisms and regulations. Am J
Physiol 1998;274:F817F833.
Research Article
290 Journal of Hepatology 2010 vol. 53
j
283290
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Way Out of Alcoholism by Jack BolandDocument38 pagesThe Way Out of Alcoholism by Jack BolandIma AardvarkNo ratings yet
- DDEV SPICES PVT LTD (Product List)Document1 pageDDEV SPICES PVT LTD (Product List)jaymin zalaNo ratings yet
- Injection Analyzer Electronic Unit enDocument67 pagesInjection Analyzer Electronic Unit enmayralizbethbustosNo ratings yet
- PYMS Is A Reliable Malnutrition Screening ToolsDocument8 pagesPYMS Is A Reliable Malnutrition Screening ToolsRika LedyNo ratings yet
- People Vs CacayanDocument2 pagesPeople Vs CacayanAshley CandiceNo ratings yet
- Nephrotic SyndromeDocument56 pagesNephrotic SyndromeMurugesan100% (1)
- Report Text: General ClassificationDocument7 pagesReport Text: General Classificationrisky armala syahraniNo ratings yet
- Implementation of 5G - IoT Communication System 1 - RB - LAB EQUIPMENTDocument32 pagesImplementation of 5G - IoT Communication System 1 - RB - LAB EQUIPMENTMaitrayee PragyaNo ratings yet
- Ne XT ProtDocument2 pagesNe XT Protwilliam919No ratings yet
- Chef Basics Favorite RecipesDocument58 pagesChef Basics Favorite Recipesbillymac303a100% (2)
- Jurnal Gerd PDFDocument6 pagesJurnal Gerd PDFdilaNo ratings yet
- Data Obat VMedisDocument53 pagesData Obat VMedismica faradillaNo ratings yet
- The Lion and The AntDocument4 pagesThe Lion and The AntDebby Jean ChavezNo ratings yet
- Philips Healthcare: Field Change Order ServiceDocument5 pagesPhilips Healthcare: Field Change Order ServiceJimNo ratings yet
- 2015 4-H Show & Sale CatalogDocument53 pages2015 4-H Show & Sale CatalogFauquier NowNo ratings yet
- URICA TestDocument3 pagesURICA TestCristy PagalanNo ratings yet
- Jinko 570 Mono Facial Jkm570m-7rl4-VDocument2 pagesJinko 570 Mono Facial Jkm570m-7rl4-VShahneela AnsariNo ratings yet
- Dual Laminate Piping HandbookDocument46 pagesDual Laminate Piping HandbookA.Subin DasNo ratings yet
- Low Voltage Fixed and Automatic Power Factor Correction SystemsDocument6 pagesLow Voltage Fixed and Automatic Power Factor Correction Systemszabiruddin786No ratings yet
- Sepsis Management UCLA HealthDocument23 pagesSepsis Management UCLA HealthKomang_JananuragaNo ratings yet
- Preservative MaterialsDocument2 pagesPreservative MaterialsmtcengineeringNo ratings yet
- Silly VersesDocument29 pagesSilly Verseskevin daleNo ratings yet
- Cariprazine PDFDocument162 pagesCariprazine PDFige zaharaNo ratings yet
- Child Case History FDocument6 pagesChild Case History FSubhas RoyNo ratings yet
- Marketing ProjectDocument82 pagesMarketing ProjectSumit GuptaNo ratings yet
- 03 Secondary School Student's Academic Performance Self Esteem and School Environment An Empirical Assessment From NigeriaDocument10 pages03 Secondary School Student's Academic Performance Self Esteem and School Environment An Empirical Assessment From NigeriaKienstel GigantoNo ratings yet
- Market Pulse Q4 Report - Nielsen Viet Nam: Prepared by Nielsen Vietnam February 2017Document8 pagesMarket Pulse Q4 Report - Nielsen Viet Nam: Prepared by Nielsen Vietnam February 2017K57.CTTT BUI NGUYEN HUONG LYNo ratings yet
- R. Nishanth K. VigneswaranDocument20 pagesR. Nishanth K. VigneswaranAbishaTeslinNo ratings yet
- Cataloge ICARDocument66 pagesCataloge ICARAgoess Oetomo100% (1)
- 15 UrinalysisDocument9 pages15 UrinalysisJaney Ceniza تNo ratings yet