Professional Documents
Culture Documents
A Case of Swine Flu Superinfected With Carbapenem Resistant Klebsiella
Uploaded by
rajdiphazraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Case of Swine Flu Superinfected With Carbapenem Resistant Klebsiella
Uploaded by
rajdiphazraCopyright:
Available Formats
120 Asian Journal of Medical Sciences | Jul-Sep 2014 | Vol 5 | Issue 3
INTRODUCTION
Swine fu is primarily a respiratory disease caused by a
reassortant virus. Though it is usually species specifc (pigs),
occasionally it crosses species barrier and infects humans.
1
First isolation of swine infuenza virus from a human
was done in 1974
2
. In the past, though cases of person to
person transmission have been reported, it resulted in small
outbreaks only.
2
Then in March and April 2009, there was
an outbreak of swine H1N1 infuenza A virus in Mexico
with subsequent cases being detected later in several other
countries including United States and India
3
(so called 2009
fu pandemic). The signs and symptoms of swine fu caused
by H1N1 infuenza A virus are similar to those in seasonal
infuenza virus.
4
However, secondary bacterial pneumonia
may complicate viral pneumonia, especially in pediatric age
group.
4
But among adults, bacterial coinfection is a rarity.
4
Here, we report a case of swine fu superinfected with
carbapenem resistant klebsiella.
CASE REPORT
A 65 years old female patient presented to us with
history of abrupt onset high grade fever along with
chill, headache, dry cough, sore throat, myalgia, malaise
and anorexia of one week duration. The patient was
disoriented, dehydrated and tachypneic. The cough was
nonproductive and nonpurulent. There was no history of
diarrhea or vomiting. Neck rigidity was absent. There was
diminished movement of right side of chest. Also, there
was impaired resonance on percussion. On auscultation
of right side of chest, bronchophony and tubular breath
sounds were found especially in the mid portion. On
routine investigations, neutrophilic leukocytosis (total
white blood cell [WBC] count 13,400 /cu mm with 84%
neutrophil) and moderate anemia (hemoglobin 8.95 g/dL)
were found. Liver function test (LFT) showed elevated
SGPT (serum glutamic pyruvic transaminase- 3706.0
U/L) level. Chest x-ray PA (posteroanterior) view showed
homogenous opacity involving right middle lobe of lung
with no mediastinal shift. Initially she was diagnosed as
a case of viral hepatitis with encephalopathy and chest
infection and treated symptomatically with empirical
antibiotics (co-amoxiclav 1.2 g and metronidazole 500 mg,
both thrice daily intravenously) and adequate hydration.
However on the very next day, the real-time reverse
transcriptase-polymerase chain reaction (rRT-PCR) swine
fu panel was done on throat swab specimen and it showed
a positive result for swine fu (as per report from National
Institute of Cholera and Enteric Diseases [NICED],
Kolkata). Subsequently, neuraminidase inhibitor oseltamivir
75 mg twice daily through Ryles tube (patient was
disoriented) was started without any delay. For initial couple
A case of swine fu superinfected with carbapenem
resistant Klebsiella
Rajdip Hazra
1
, Manjunatha S.M.
1
, Md Babrak Manuar
1
, Sisir Chakraborty
2
, Kaushik Ghosh
3
1
Department of Anesthesiology, Nilratan Sircar Medical College and Hospital, Kolkata, India,
2
Department of Medicine, College of Medicine
and Sagore Dutta Hospital, Kolkata, India,
3
Department of Medicine, Malda Medical College and Hospital, Malda, India
A B S T R A C T
CASE REPORT ASIAN JOURNAL OF MEDICAL SCIENCES
Access this article online
Website:
http://nepjol.info/index.php/AJMS
Submitted: 10-09-2013 Revised: 21-01-2014 Published: 10-03-2014
Address for Correspondence:
Dr. Rajdip Hazra, Department of Anesthesiology, Nilratan Sircar Medical College and Hospital, Kolkata, West Bengal, India.
E-mail: rajdiphazra_nrs@yahoo.co.in; Phone: +918013436607. Copyright AJMS
Swine fu is caused by antigenic shift of infuenza A virus with clinical features similar
to seasonal infuenza virus. Majority of the morbidity and mortality due to swine fu are
attributable to pneumonia and the acute respiratory distress syndrome (ARDS). Bacterial
superinfection can occur, though it is rare in adults. Here we report a case of swine fu
superinfected with carbapenem resistant Klebsiella, which is often coined as Klebsiella
superbug.
Key words: Swine fu, Bacterial superinfection, Carbapenem resistant Klebsiella
Hazra, et al.: Swine fu with carbapenem resistant Klebsiella
Asian Journal of Medical Sciences | Jul-Sep 2014 | Vol 5 | Issue 3 121
of days, the patient responded with reduced total leukocyte
count (12,200 /cu mm) and SGPT level (402.8 U/L). On
5
th
day of admission, the patient became unconscious,
dyspneic with peripheral desaturation (oxygen saturation
of peripheral arterial blood [SpO
2
] <85%) and crepitations
throughout both lung felds. Arterial blood gas analysis
showed mild respiratory alkalosis (pH) with PaO
2
(partial
pressure of oxygen in blood) of 55 mm Hg. The patient
was immediately intubated and put on mechanical ventilator
on volume control mode (with tidal volume 6 ml/kg of
predicted body weight and positive end expiratory pressure
[PEEP] of 10 cm H
2
O maintaining plateau airway pressure
below 30 cm H
2
O). Antibiotic regimes were changed to
linezolid (600 mg twice daily intravenously) and ceftazidime
(2 g thrice daily intravenously). Chest x-ray PA view revealed
diffuse, bilateral, interstitial and alveolar infltrates. Steroids
(hydrocortisone 100 mg twice daily on intravenous route
and budesonide respules 0.5 mg/2 ml, 4 times a day
through nebulisation) and bronchodilator (salbutamol
respules 5 mg/2.5 ml, 4 times a day through nebulisation)
were added. With these measures, vital hemodynamic
parameters (pulse, respiratory rate, non-invasive blood
pressure and oxygen saturation) became stable. Acute
respiratory distress syndrome (ARDS) was suspected.
Graveness of the situation was explained to patient party.
Suction material from endotracheal tube was sent for
bacteriological culture and sensitivity maintaining adequate
sterility. Next day, the culture and sensitivity reports were
received. The VITEK 2 Advanced Expert System
TM
(AES) phenotypically identifed the organism as Klebsiella
spp. with ESBL (extended spectrum beta lactamase) +
Carbapenemase (Metallo- or KPC i.e., Klebsiella pneumonia
Carbapenemase) resistance mechanism sensitive only to
colistin (minimal inhibitory concentration [MIC] <0.5
mcg/ml) and intermediate sensitivity to tigecycline (MIC
4 mcg/ml). Then, the patient was started on tigecycline
(100 mg bolus followed by 50 mg every 12 hours through
intravenous route). The rRT-PCR was repeated on throat
swab specimen and it was negative for swine fu virus (as per
report from NICED). Inspite of the treatment, the patient
gradually developed hypoxia followed by type I respiratory
failure. Over next two days, she developed shock and
azotemia. Vasopressor was added (noradrenaline infusion
started initially at 12 mcg/min and later titrated as per blood
pressure). The patient experienced a rapid and progressive
downhill course over the next four days by developing multi
organ dysfunction syndrome. Subsequently, the patient died
on the thirteenth day of admission.
DISCUSSION
Infuenza occurs in seasonal epidemics affecting mainly
those with extremes of ages (<6 months or >65 years) or
with comorbid medical illness. About 80% of infuenza
deaths and most severe disease are attributable to H3N2
strains of infuenza A.
5
In early months of 2009, a novel
H1N1 infuenza A virus descendent of the 1918 pandemic
strain, appeared in Mexico.
3
It was suffciently different
from previously circulating seasonal H1N1 viruses to
qualify as an antigenic shift and its resultant spread
around the world has been classifed as 2009 fu pandemic.
This new strain of H1N1 infuenza A virus is known as
pandemic H1N1 or pH1N1, novel H1N1, SOIV (swine
origin infuenza virus) or swine fu.
Infuenza epidemics due to seasonal strain used to occur
as a result of minor changes in the antigenic characteristics
of the hemaglutinin and neuraminidase glycoproteins
of the infuenza viruses (antigenic drift).
6
Morbidity and
mortality associated with seasonal infuenza outbreaks are
signifcant, especially in older patients.
5
However, infuenza
pandemics like that of swine fu, occur less frequently due
to major changes of surface glycoproteins of the viruses
(antigenic shift). Groups at risk of getting affected with
swine fu include those with underlying cardio-pulmonary
disease, having immunosuppression, pregnancy, lactation,
diabetes, obesity or neurological disabilities.
7
The clinical
features of uncomplicated infuenza are that of other
respiratory viral infections.
Majority of the morbidity and mortality due to swine fu are
attributable to pneumonia and the acute respiratory distress
syndrome (ARDS).
8
Pneumonia may be primary viral or
mixed viral and secondary bacterial. Those progressing
to ARDS have the worst prognosis.
8
Secondary bacterial
infection is much more prevalent in swine fu affected
patients than their seasonal counterpart. A study on
lung specimens from 77 fatal cases of pH1N1 infection
found 29% prevalence of bacterial superinfection and
Pneumococcus, Staphyococcus aureus, and Streptococcus
pyogenes being the commonest.
4
However, Klebsiella superinfection in a swine fu patient is a
rare fnding. To the best of our present knowledge, it is the
frst case report of swine fu superinfected with carbapenem
resistant Klebsiella. Carbapenemase producing bacteria are
often referred to as superbugs because infections caused
by them are diffcult to treat. Sometimes, such bacteria
are sensitive to polymyxins or tigecycline
9
(in our case,
it was sensitive to colistin and intermediately sensitive
to tigecycline). In 2009, a Swedish national travelling
India, developed UTI (urinary tract infection) caused by
carbapenem resistant Klebsiella sensitive to tigecycline
and colistin. After genotypic analysis of the isolate, a new
strain was found which is known today as NDM-1 or New
Delhi metallo-beta-lactamase-1.
10
Unfortunately in our
case, genotypic analysis could not be done.
Hazra, et al.: Swine fu with carbapenem resistant Klebsiella
122 Asian Journal of Medical Sciences | Jul-Sep 2014 | Vol 5 | Issue 3
ACKNOWLEDGEMENTS
The authors like to acknowledge Infectious Disease and
Beliaghata General (ID & BG) Hospital, Kolkata, India
for providing necessary support. None of the authors has
any confict of interest.
REFERENCES
1. Jafri SSI, Ilyas M and Idrees M. Swine fu: A threat to human
health. Biotechnology and Mol Biol 2010; 5(3):46-50.
2. Myers KP, Olsen CW and Gray GC. Cases of swine infuenza
in humans: a review of the literature. Clin Infect Dis 2007;
44(8):1084-1088.
3. Zimmer SM and Burke DS. Historical perspective Emergence
of infuenza A (H1N1) Viruses. N Engl J Med 2009; 361:
279-285.
4. Bacterial coinfections in lung tissue specimens from fatal
cases of 2009 pandemic infuenza A (H1N1) - United
States, May-August 2009. MMWR Morb Mortal Wkly Rep
2009;58:1071-1074.
Authors Contribution:
RH & MSM Prepared the initial draft. RH, MBM, SC, KG Contributed to the manuscript. RH Reviewed and helped in fnal preparation
of the manuscript.
Source of Support: Nil, Confict of Interest: None declared.
5. Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges
CB, Cox NJ, et al. Infuenza-associated hospitalizations in the
United States. JAMA 2004; 292:13331340.
6. Lai CJ, Markoff LJ, Sveda MM, Lamb RA, Dhar R and Chanock
RM. Genetic variation of infuenza A viruses as studied by
recombinant DNA techniques. Ann N Y Acad Sci 1980; 354:162-
171.
7. Hospitalized patients with novel infuenza A (H1N1) virus
infection - California, April-May 2009. MMWR Morb Mortal Wkly
Rep 2009; 58:536-541.
8. Rello J, Rodrguez A, Ibaez P, Socias L, Cebrian J, Marques
A, et al. H1N1 SEMICYUC Working Group. Intensive care adult
patients with severe respiratory failure caused by Infuenza A
(H1N1)v in Spain. Crit Care Med 2009;13:148.
9. Health Protection Agency. Multi-resistant hospital bacteria
linked to India and Pakistan. Health Protection Report 2009;
3. Available from: http://www.hpa.org.uk/hpr/archives/2009/
news2609.htm.
10. Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee
K and Walsh TR. Characterization of a new metallo-beta-
lactamase gene, bla(NDM-1), and a novel erythromycin
esterase gene carried on a unique genetic structure in Klebsiella
pneumoniae sequence type 14 from India. Antimicrob Agents
Chemother 2009; 53(12):50465054.
You might also like
- Assignment 7Document2 pagesAssignment 7rajdiphazraNo ratings yet
- Assignment 3: Literature Review: 1 PointDocument3 pagesAssignment 3: Literature Review: 1 Pointrajdiphazra0% (1)
- Assignment 5Document2 pagesAssignment 5rajdiphazraNo ratings yet
- Assignment 2: Formulating Research Question: 1 PointDocument2 pagesAssignment 2: Formulating Research Question: 1 PointrajdiphazraNo ratings yet
- Assignment 4Document3 pagesAssignment 4rajdiphazraNo ratings yet
- Assignment 1Document2 pagesAssignment 1rajdiphazraNo ratings yet
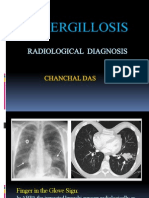
- Aspergillosis: Radiological DiagnosisDocument12 pagesAspergillosis: Radiological DiagnosisrajdiphazraNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Defence Mechanism of Oral CavityDocument15 pagesDefence Mechanism of Oral CavityANUBHANo ratings yet
- Diuretics: Dr. Sadat MemonDocument28 pagesDiuretics: Dr. Sadat MemonCham PianoNo ratings yet
- The Current Strategy in Hormonal and Non-HormonalDocument25 pagesThe Current Strategy in Hormonal and Non-HormonalJulio YulitaNo ratings yet
- PneumoniaDocument41 pagesPneumoniapaanar100% (2)
- Daftar Pustaka: Universitas Sumatera UtaraDocument3 pagesDaftar Pustaka: Universitas Sumatera UtaraYuliana WiralestariNo ratings yet
- Case Study MiDocument23 pagesCase Study Mianamika sharma100% (6)
- Pediatric Mechanical VentilationDocument36 pagesPediatric Mechanical VentilationrizalNo ratings yet
- Head To Toe Exam: ChestDocument2 pagesHead To Toe Exam: Chestnicolas lastreNo ratings yet
- AvantGen Awarded Contract From NIH To Expedite The Commercialization of Its AccuRate COVID-19 SelfCheck OTC TestDocument3 pagesAvantGen Awarded Contract From NIH To Expedite The Commercialization of Its AccuRate COVID-19 SelfCheck OTC TestPR.comNo ratings yet
- Hem OccultDocument2 pagesHem OccultfidofidzNo ratings yet
- Rectum: Malueth AbrahamDocument19 pagesRectum: Malueth AbrahamMalueth AnguiNo ratings yet
- Phacoemulsification Versus Small Incision Cataract Surgery (SICS) A Surgical Option For Immature Cataract in Developing Countries.Document5 pagesPhacoemulsification Versus Small Incision Cataract Surgery (SICS) A Surgical Option For Immature Cataract in Developing Countries.Ragni MishraNo ratings yet
- Facial Feminization Surgery FFS Surgeon ListingsDocument46 pagesFacial Feminization Surgery FFS Surgeon ListingsTrinity Rose Transsexual100% (2)
- 1 - Pharmaceutical Dosage FormsDocument41 pages1 - Pharmaceutical Dosage Formspanwar_brossNo ratings yet
- Disorders of The Eye LidsDocument33 pagesDisorders of The Eye Lidsc/risaaq yuusuf ColoowNo ratings yet
- Acute Otitis Media: Jama Patient PageDocument1 pageAcute Otitis Media: Jama Patient PageS. JohnNo ratings yet
- Physiotherapy in Shoulder Impigement SyndromeDocument181 pagesPhysiotherapy in Shoulder Impigement SyndromePraneeth KumarNo ratings yet
- MDI Major Depression Inventory - English PDFDocument3 pagesMDI Major Depression Inventory - English PDFcmenikarachchiNo ratings yet
- Test Preparation & ReviewDocument4 pagesTest Preparation & Reviewhelamahjoubmounirdmo100% (1)
- NICU 2021clinical Reference Manual For Advanced Neonatal Care FINALDocument254 pagesNICU 2021clinical Reference Manual For Advanced Neonatal Care FINALTewodros Demeke100% (7)
- Orthopaedic vs Orthodontic TherapyDocument3 pagesOrthopaedic vs Orthodontic Therapyاسراء فاضل مصطفى100% (1)
- Tool Box Talk - Snake BitesDocument1 pageTool Box Talk - Snake BitesNicole AnthonyNo ratings yet
- Bip03051f UgDocument2 pagesBip03051f UgdellalalaNo ratings yet
- CKHA 2013 Salary DisclosureDocument2 pagesCKHA 2013 Salary DisclosureChatham VoiceNo ratings yet
- Cardiovascular System Lecture 1 2020 2021Document5 pagesCardiovascular System Lecture 1 2020 2021olawandeilo123No ratings yet
- Circulation Case Study Week 4Document10 pagesCirculation Case Study Week 4Caroline GamboneNo ratings yet
- Free TOEFL Practice Questions About The TOEFLDocument39 pagesFree TOEFL Practice Questions About The TOEFLDieu-Donné NoukounwouiNo ratings yet
- EFM Teaching Didactic FINALDocument81 pagesEFM Teaching Didactic FINALNadia RestyNo ratings yet
- St. Paul College of Ilocos Sur Nursing Department Clinical CourseDocument3 pagesSt. Paul College of Ilocos Sur Nursing Department Clinical CourseMarie Kelsey Acena Macaraig100% (1)
- Antibodies To Watch in 2020 PDFDocument25 pagesAntibodies To Watch in 2020 PDFFranciscoNo ratings yet