Professional Documents
Culture Documents
Health-Related Quality of Life After Ischemic Stroke: The Impact of Pharmaceutical Interventions On Drug Therapy (Pharmaceutical Care Concept)
Uploaded by
Dhila- Nailatul Fadhilah0 ratings0% found this document useful (0 votes)
14 views7 pagesjnjnjmn
Original Title
1477-7525-8-59
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentjnjnjmn
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
14 views7 pagesHealth-Related Quality of Life After Ischemic Stroke: The Impact of Pharmaceutical Interventions On Drug Therapy (Pharmaceutical Care Concept)
Uploaded by
Dhila- Nailatul Fadhilahjnjnjmn
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 7
Hohmann et al.
Health and Quality of Life Outcomes 2010, 8:59
http://www.hqlo.com/content/8/1/59
Open Access RESEARCH
2010 Hohmann et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
Research
Health-Related Quality of Life after Ischemic Stroke:
The Impact of Pharmaceutical Interventions on
Drug Therapy (Pharmaceutical Care Concept)
Carina Hohmann*
1,2
, Roland Radziwill
2
, Juergen MKlotz
1
and Andreas H Jacobs
3
Abstract
Background: Health-related quality of life (HRQoL) after stroke is an important healthcare measure. Pharmaceutical
Care (PC) is an evolving concept to optimize drug-therapy, minimize drug-related problems, and improve HRQoL of
patients. The purpose of this study was to evaluate the impact of PC on HRQoL, as determined by Short Form 36 (SF-
36) among patients after TIA or ischemic stroke one-year following their initial entry in hospital.
Methods: Patients were assigned to either an intervention (IG) or a control group (CG). The individual assignment of
the patient to IG or CG depended on the community pharmacy to which the patients were assigned for care.
Community pharmacies either delivered standard care (CG) or provided intensified PC (IG). Pharmacists who are
members of the "Quality Assurance Working Group" (QAWG) provided PC for patients in IG.
Results: 255 patients were recruited (IG: n = 90; CG: n = 165) between 06/2004 to 01/2007. During the study, the
HRQoL of the patients in IG did not change significantly. In the CG, a significant decrease in the HRQoL was observed in
7/8 subscales and in both summary measures of SF-36.
Conclusions: This is the first follow-up study in Germany involving a major community hospital, rehabilitation
hospitals, community pharmacies and general practitioners investigating the impact of PC on HRQoL of patients after
ischemic stroke. Our findings indicate that an intensified education and care of patients after ischemic stroke by
dedicated pharmacists based on a concept of PC may maintain the HRQoL of IG patients.
Background
Stroke is one of the leading causes of death in Europe and
the major cause of disability in the elderly [1,2]. Health-
related quality of life (HRQoL) related to stroke and life
satisfaction after stroke are important healthcare out-
comes that have not received sufficient attention in the
literature. HRQoL assessment includes at least 4 dimen-
sions: physical, functional, psychological, and social
health [3,4]. The physical health dimension refers to dis-
ease-related symptoms. The functional health comprises
self-care, mobility, and the capacity to perform various
familiar and work roles. The psychological dimension
includes cognitive and emotional functions and subjec-
tive perceptions of health and life satisfaction. The social
dimension includes social and familiar contacts [3]. Short
Form 36 is a widely and frequently used, generic, patient-
report instrument for measuring quality of life [5]. It has
also been validated in patients with stroke [5,6].
Pharmaceutical Care (PC), first outlined by Hepler and
Strand in 1990, has been the subject of intensive research
in Germany for several years. PC is the provision of drug
therapy by a responsible pharmacist for the purpose of
achieving a definite outcome to improve the patients'
quality of life [7]. PC is a patient-tailored, outcome ori-
ented pharmacy practice that requires that the pharma-
cist work in concert with the patient and the patient's
other healthcare providers to promote health, to prevent
disease, and to assess, monitor, initiate, and modify medi-
cation use to assure that drug therapy regimens are safe
and effective. Thus, PC is a concept to optimize drug
therapy, minimize drug-related problems, and improves
self-management; it can directly affect the HRQoL of
patients. The pharmacist is a part of the health care team,
* Correspondence: carina.hohmann@klinikum-fulda.de
1
Klinikum Fulda gAG, Department of Neurology, Pacelliallee 4, 36043 Fulda,
Germany
Full list of author information is available at the end of the article
Hohmann et al. Health and Quality of Life Outcomes 2010, 8:59
http://www.hqlo.com/content/8/1/59
Page 2 of 7
and extensive communication between pharmacist, phy-
sician, and the patient is necessary to achieve a defined
health care outcome [7]. The goal of Pharmaceutical Care
is to optimize the patient's HRQoL, and achieve positive
clinical outcomes, within realistic economic expendi-
tures. The positive influence of PC on HRQoL has been
demonstrated in several trials [8,9].
The main objective of this study was to evaluate the
impact of PC on the HRQoL, as determined by Short
Form 36 (SF-36) among patients after TIA or ischemic
stroke one-year following their initial entry into the hos-
pital.
Methods
Setting
A major community hospital in Germany (Klinikum
Fulda gAG), several rehabilitation hospitals, community
pharmacies and general practitioners were involved in
this study. The Stroke Unit of the Klinikum Fulda gAG
serves diagnosis and treatment of over 700 patients with
acute stroke each year.
Patients
Patients with TIA or ischemic stroke with a Barthel index
of over 30 points at the time of discharge from the hospi-
tal and living at home were included between June 2004
and January 2007. The follow-up-period for the patients
was 12 months. Demographic and clinical data were col-
lected from medical records and by interview.
The patients were assigned either to an intervention
group (IG) or a control group (CG). The individual
assignment of the patient to the IG or CG depended on
the community pharmacy to which patients were
assigned for care. Pharmacists (n = 23) who are members
of the "Quality Assurance Working Group" (QAWG) pro-
vided PC for patients in the IG. Pharmacists of the
QAWG met on a regular basis (once a month) to discuss
specific drug-related issues and to ensure proper imple-
mentation of PC in their pharmacies. The PC process in
this study comprises medication reviews and counselling
interviews with regards to medicines, especially those for
secondary prevention, and to specific actions, side
effects, and drug-interactions as well as cardiovascular
risk factors such as hypertension, diabetes mellitus, and
hyperlipidemia. Hypertension remains a major modifiable
risk factor for cardiovascular diseases. The diagnosis of
hypertension is made when the average of two or more
diastolic blood pressure (BP) measurements on at least
two subsequent visits is more than 90 mm Hg or when
the average of multiple systolic BP readings on two or
more subsequent visits is consistently more than 140 mm
Hg [10]. Diabetes mellitus is a group of metabolic dis-
eases characterised by chronic hyperglycemia resulting
from defects in insulin secretion, insulin action, or both
[11]. Hyperlipidemia is defined as an abnormal plasma
lipid status. Common lipid abnormalities include ele-
vated levels of total cholesterol, low-density lipoprotein
(LDL) cholesterol, lipoprotein (a), and triglyceride; as well
as low levels of high-density lipoprotein (HDL) choles-
terol. These abnormalities can be found alone or in com-
bination [12]. Furthermore, the pharmacists had to detect
and solve drug-related problems (DRPs). The community
pharmacists received education and training in PC with
respect to patients with stroke in several workshops. Top-
ics included causes of stroke, risk factors, symptoms, def-
inition of PC, identifying and solving DRPs and designing
a PC plan. Risk factors such as hypertension, diabetes
mellitus, hyperlipidemia, and atrial fibrillation as well as
secondary prevention and individual patient problems
were discussed. The other community (control) pharma-
cists (n = 39) delivered standard care for the patients
within the CG.
Pharmaceutical Care
The PC process for the patients in the IG consists of three
sections:
(i) At hospital: Patients and their relatives received a
counselling interview from the clinical pharmacist
about the current medication, their effects, the dos-
age and important side effects as well as administra-
tion advice. A medication record with detailed
information about the drug name, the dosage and
administration advice was provided.
(ii) Seamless care: At the time of discharge from hos-
pital, the general practitioner, the rehabilitation hos-
pital, and the community pharmacist received a
detailed care plan for the patient from the clinical
pharmacist.
(iii) In the ambulatory setting: PC was continued by
the attending pharmacist for 12 months during this
study. At least one counselling interview between the
pharmacist and the patient every three months was
obligatory. The attending pharmacist was required to
document the medication, the DRPs and the counsel-
ling interview.
Standard Care
Patients of the CG received a medication record at the
time of discharge from hospital and received standard
care from their community pharmacy. There is no
defined standard care process for the community phar-
macy and it depends on each pharmacist. General issues
are for example dispensing medicine, giving advice on
medicine, and information about side effects and drug-
interactions.
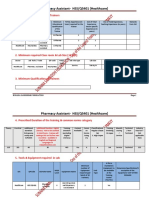
The steps taken over 12 months of the study are sum-
marized in Figure 1.
Hohmann et al. Health and Quality of Life Outcomes 2010, 8:59
http://www.hqlo.com/content/8/1/59
Page 3 of 7
Health-related quality of life
To evaluate the patient's HRQoL, the SF-36 was used
upon entry into the hospital and after 12 months. It pro-
vides a valid, subjective measure of physical and mental
health after stroke. Two types of SF-36 scores can be gen-
erated: the 8 SF-36 scales provide a comprehensive profile
of health status, and the two summary measures have fea-
tures that make them more advantageous for clinical tri-
als [5]. The SF-36 consists of 8 subscales: physical
functioning (PF), physical role (RP), bodily pain (BP),
general health (GH), vitality (VT), social functioning
(SF), emotional role (RE), and mental health (MH), and
the 2 summary measures are the Physical Component
Summary (PCS) and the Mental Component Summary
score (MCS).
Subscales and the summary scores range from 0 to 100,
with higher values representing better quality of life.
Different sociodemographic and medical variables were
recorded, including age, sex, cerebrovascular risk factors,
the type of cerebral ischemia (transient ischemic attack
(TIA), or ischemic stroke), and the Barthel Index.
The study was conducted in compliance with the
requirements of the institutional review board, Philipps
University, Marburg (Germany). All patients signed the
informed consent.
Statistical Analysis
All statistical analyses were performed by SPSS version
12.0 for Windows. Sample size calculations targeting a
power of 80% (2-sided test of = 5%) to improve the
patient's HRQoL after stroke on the basis of PC demon-
strated that 116 patients were needed for each group.
The evaluation of the HRQoL was based on a "per-pro-
tocol" analysis; only those patients were analyzed who
completed the entire trial.
Data are shown as means. The chi-squared test was
used for assessing differences in proportions. The stu-
dents t-test was used to compare the means of both
groups. In order to determine the normal distribution of
the variables the Kolmogorov-Smirnov-test was used.
The non-parametric rank-sum test according to Mann
and Whitney was used to compare the distribution of
ranks between the groups. The Wilcoxon Rank sum test
was chosen to identify differences in each group at base-
line and after 12 months. A two-tailed probability value
of <0.05 was considered to be statistically significant.
Results
Over the entire period of enrolment (20 months), 1316
patients were admitted to the Stroke Unit. In total, 911
patients (69.2%) were excluded from the study due to
intracranial haemorrhage or other diagnoses, for example
migrainous aura, seizures, Barthel index < 30 points at
discharge from hospital, fatal ischemic stroke or living in
a nursing home. A total of 405 patients met the inclusion
criteria, 150 patients of these (37.0%) declined participa-
tion in the study. Reasons for refusal were an excellent
support by the family or general practitioner, no need for
further information or intensive care, or the patient was
not familiar with PC. Of the remaining 255 patients, n =
90 were recruited into IG and n = 165 into CG (Figure 2).
Patients' baseline characteristics are summarized in
Table 1. Between IG and CG, there were no significant
differences with regards to age (p = 0.952), sex (p = 0.554)
or subtype of cerebral ischemia (p = 0.814), and Barthel
Index (p = 0.101). The most frequent cardiovascular risk
factor in both groups was arterial hypertension (37%); the
second most frequent was a combination of hypertension
and hyperlipidemia.
During the study period 17 patients (18.9%) in the IG
and 8 patients (4.9%) in the CG were lost during follow-
up. Reasons for patients' drop-out were withdrawal from
informed consent, moving of the patient to another town,
transfer to a nursing home or no specific reasons. One
patient in the IG and five patients in the CG died (Figure
2). No differences in sex, ages, and diagnosis were found
in both groups at time of discharge from hospital.
Figure 1 The sequence and structure in the intervention and con-
trol group for 12 months.
Intervention group (IG) Control group (CG)
Individual assignment to IG or CG depended on the community
pharmacy to which the patients were assigned for care
medication review process
patients health-related quality of life (SF-36)
medication record
Stroke Unit /
neurological
ward
counselling interview
Seamless
care
Care plan for the community
pharmacy, rehabilitation hospi-
tal and general practitioner from
the clinical pharmacist
Community
pharmacy
Pharmaceutical Care
medication review process
counselling interview (secon-
dary prevention, cardiovascular
risk factors and their medicines)
Detecting and solving drug-
related problems
Standard Care (it depends on
the pharmacist in the commu-
nity pharmacy
After 12
months
patients health-related quality of life (SF-36)
Hohmann et al. Health and Quality of Life Outcomes 2010, 8:59
http://www.hqlo.com/content/8/1/59
Page 4 of 7
Health-related quality of life
Eight subscales
The distribution of SF-36 scores in the IG (n = 64) and in
the CG (n = 119) is shown in Figure 3, 4, 5, 6. Upon
admission patients of both, IG and CG, groups showed
no significant differences in the 8 subscales (Figure 3).
After 12 months, the subscale vitality was significantly
lower in CG patients than in IG patients (p = 0.027) (Fig-
ure 4).
The HRQoL of patients in IG remained stable over the
entire observation period. Only the subscale bodily pain
decreased significantly over time (p = 0.001) (Figure 5). In
contrast, HRQoL parameter of patients in CG deterio-
rated significantly in 7 of the 8 subscales over time (Fig-
ure 6).
Two summary measures
The mean scores of both summary measures, PCS and
MCS, are shown in Table 2. Upon entry into the study
Figure 3 Score distribution of the SF-36 (8 subscales) IG and CG at
hospital (mean and standard deviation).
0
10
20
30
40
50
60
70
80
90
100
110
120
PF RP BP GH VT SF RE MH
m
e
a
n
IG (hospital) CG (hospital)
Figure 4 Score distribution of the SF-36 (8 subscales) IG and CG
after 12 months (mean and standard deviation).
0
10
20
30
40
50
60
70
80
90
100
110
120
PF RP BP GH VT SF RE MH
m
e
a
n
IG (12 months) CG (12 months)
*
Figure 2 Flow chart for patients' inclusion and exclusion criteria
and their participation.
A total of 1316 patients were admitted to the stroke unit
Excluded (n=1061)
- inclusion criteria not met
(n=911)
- declined the participation
(n=150)
Included (n=255)
Intervention group (n=90) Control group (n=165)
Lost to follow-up (n=17):
- withdraw from informed-consent
(n=12)
- moving to another town (n=1)
- transfer to a nursing home (n=2)
- no specific reason (n=2)
death (n=1)
Lost to follow up (n=8):
- withdraw from informed consent
(n=1)
- moving to another town (n=1)
- transfer to a nursing home (n=2)
- no specific reason (n=4)
death (n=5)
Outcome data Outcome data
Table 1: Baseline characteristics
Characteristics Interventio
n Group
n = 90
Control
Group
n = 165
Age, mean SD (years) 68.2 ( 9.7) 68.1 ( 10.8)
Min 45 23
Max 85 85
Sex, n (%)
female 35 (38.9%) 58 (35.2%)
male 55 (61.1%) 107 (64.8%)
subtype of cerebral ischemia, n (%)
TIA 28 (31.1%) 49 (29.7%)
Ischemic stroke 62 (68.9%) 116 (70.3%)
Barthel Index, mean SD 92,8 ( 7,5) 89,4 ( 14,3)
cardiovascular risk factors
hypertension 33 (36.7%) 61 (37.0%)
hyperlipidemia 6 (6.7%) 5 (3.0%)
diabetes mellitus 1 (1.1%) 2 (1.2%)
hypertension+hyperlipidemia 31 (34.4%) 46 (27.9%)
hypertension+diabetes mellitus 4 (4.4%) 20 (12.1%)
diabetes
mellitus+hyperlipidemia
-- 2 (1.2%)
hypertension+diabetes
mellitus+hyperlipidemia 7 (7.8%) 15 (9.1%)
None 8 (8.9%) 14 (8.5%)
SD = Standard deviation
Hohmann et al. Health and Quality of Life Outcomes 2010, 8:59
http://www.hqlo.com/content/8/1/59
Page 5 of 7
there was no significant difference in the two summary
measures in either group. At follow-up, there were also
no significant differences in HRQoL between the groups
(Table 2). For the CG, a significant decline in PCS and
MCS was observed between baseline and at follow-up
(PCS: p = 0.023; MCS: p = 0.001). For the IG, changes in
PCS and MCS between study entry and at follow-up were
not statistically significant.
Discussion
This is the first study in Germany to investigate the
impact of intensive pharmaceutical care (PC) versus stan-
dard care in a larger patient population with ischemic
stroke. This study demonstrates that PC is able to prevent
deterioration of most HRQoL parameters over a 12
months period. Our findings indicate that PC as per-
formed in the hospital and in the community setting is
feasible and has a clear benefit and positive impact on
patient's HRQoL. Moreover, this study is a step forward
towards monitoring the implementation of PC within
hospitals and within the community setting and towards
evaluating the role of pharmacists within a specific thera-
peutic team. We found that a PC concept stabilizes the
HRQoL in several scales as a result of an intensified
involvement by pharmacists.
In a comparison of the subscales and the summary
measures in both groups upon study entry there were no
significant differences, thus providing an optimal starting
point for measuring the impact of PC on HRQoL. After
12 months the comparison of the HRQoL of the patients
who received intensified PC with those who received
standard care showed that the vitality of the patients in
CG was significantly lower than of patients in IG. The
other subscales and the summary measures showed
lower, but not significant, HRQoL scores in CG indicat-
ing inferior HRQoL as compared with the patients in IG.
Due to ethical considerations community pharmacies
were not restricted from delivering PC as it did not seem
appropriate to keep the control pharmacists from provid-
ing PC in the case that DRP became apparent. For this
reason the comparison may not to be statistically signifi-
cant.
Most importantly, there was a significant deterioration
of 7 of 8 subscales as well as both summary measures of
the HRQoL over the 12 months period in the CG. That
means that patients who do not receive intensified PC
have a higher chance of deteriorating HRQoL. For the IG,
there was only a significant deterioration in bodily pain at
follow up. The deterioration of the HRQoL in patients
with cerebrovascular diseases has been reported in previ-
ous trials in several parameters [3,13,14]. The quality of
the patient's recovery can be evaluated on the basis of the
activity of daily living (ADL), social activities, and return
to work. Independently of ADL significant deleterious
effects in HRQoL result from continuing loss of function
due to the stroke. The deterioration in the HRQoL can be
caused by the presence of anomalous perception and dis-
satisfaction in patients with minor disability levels that
were incompletely restored after the stroke. Thus, the
consequences of mild to moderate stroke can affect all
dimensions of HRQoL despite the patient achieving full
independence as measured in ADL [3].
By participating in this study the HRQoL of the patients
in the IG was stable in several subscales and both sum-
mary measures indicating that the HRQoL can be main-
tained by intensified PC. Several studies have also
demonstrated that PC may have a positive impact on the
patients' HRQoL for example in patients with asthma or
hypertension [8,15,16]. Graesel et al. investigated the
impact of an intensified transition concept between inpa-
tient neurological rehabilitation and home care of
patients with stroke. The intensified transition concept
included four additional elements: a psycho-educational
seminar for family carers; an individual training course
for carers; therapeutic weekend care at home before dis-
charge; and finally, telephone counselling three months
Figure 5 Score distribution of the SF-36 (8 subscales) IG in hospi-
tal and after 12 months (mean and standard deviation).
0
10
20
30
40
50
60
70
80
90
100
110
120
PF RP BP GH VT SF RE MH
m
e
a
n
IG (hospital) IG (12 months)
***
Figure 6 Score distribution of the SF-36 (8 subscales) CG in hospi-
tal and after 12 months (mean and standard deviation). PF: physi-
cal functioning. RP: physical role. BP: bodily pain. GH: general health. VT:
vitality. SF: social functioning. RE: emotional role. MH: mental health. *
= p < 0.05. ** = p < 0.01. *** = p < 0.001.
0
10
20
30
40
50
60
70
80
90
100
110
120
PF RP BP GH VT SF RE MH
m
e
a
n
CG (hospital) CG (12 months)
***
***
*
***
*** **
**
Hohmann et al. Health and Quality of Life Outcomes 2010, 8:59
http://www.hqlo.com/content/8/1/59
Page 6 of 7
after discharge. The results show that this concept did
not lead to any significant benefit, neither to functional
status nor to HRQoL [17]. This finding may indicate that
the standard transition already contains effective ele-
ments of preparation for home care and that therefore no
further decisive advantage can be attained. Otherwise the
number of patients (n = 62) as well as the observation
period (n = 6 months) in the study was limited, thus
excluding long-term effects.
The HRQoL of the patients in the CG decreased signif-
icantly in the subscales and in both summary measures.
The deterioration of the physical role was significant
while physical functioning did not significantly deterio-
rate, which may indicate that patients perceived a decline
in their physical conditions.
There is a large difference in the frequency of diabetes
mellitus in both groups (IG: n = 12 (= 13.3%); CG: n = 39
(= 23.6%)). Diabetes mellitus has detrimental effects on a
range of health outcomes including HRQoL; for example
people with diabetes have lower scores at the SF-36 [18].
Thus, the higher proportion of patients with diabetes in
the CG may possibly cause the deterioration of HRQoL.
It should be pointed out that a considerably higher pro-
portion of subjects in the IG than in the CG refused to
participate. Those patients who refused to participate had
comparable demographic data, but may have had more
medical, social or psychological problems which could
have affected the HRQoL. The difference in HRQoL after
one year could be due to selection bias.
The mortality rate in both groups seems to be remark-
ably low (IG: n = 1; CG: n = 5); which is due to the fact
that patients with a Barthel index of less than 30 points at
discharge from hospital and/or who live in a nursing
home were excluded from this study. These exclusion cri-
teria were defined because only patients mobile enough
to go the pharmacy can be given PC.
An important difficulty in the analysis of HRQoL in
stroke patients is that few studies use the same measure-
ment tools and the same period of follow up. Further-
more, there are no data in the literature from the patients'
HRQoL from before the cerebrovascular event.
Limitations
The limitations of the present study include the fact that
no blinding or randomization could be performed. A tar-
get number of 116 participants were calculated for each
group. However, only 90 patients could be recruited for
the IG, as many patients refused to participate. The time
of enrolment was extended from 12 to 20 months and
then stopped. Moreover, patients who were lost to follow-
up were not evaluated for HRQoL, because no follow-up
data were available. It should be pointed out that, due to
ethical considerations, it did not seem to be appropriate
to keep the control pharmacists from caring in the case
that DRP became apparent. Furthermore, we did not have
any information on socioeconomic status, financial
resources or caregiver support in patients of either group,
which could have influenced the outcome of the patients.
Conclusions
In conclusion, this is the first follow-up study in Germany
involving a major community hospital, rehabilitation hos-
pitals, community pharmacies and general practitioners
demonstrating the potential impact of intensified phar-
maceutical care for patients with ischemic stroke on
HRQoL. Our findings indicate that an intensified educa-
tion and care of patients after ischemic stroke by dedi-
Table 2: Score distribution of the SF-36 (2 summary measures) at hospital and after 12 months (per-protocol-analysis)
IG (n = 64) CG (n = 119) After 12 months
Between group comparison
SF-36 Scales time mean
( SD)
mean
( SD)
p-Value
PCS Hospital 41.8 ( 9.8) 41.2 ( 10.8)
After 12 months 41.5 ( 11.0) 38.1 ( 11.6) 0.090
p-Value Differences between baseline and after
12 months
0.313 0.023*
MCS Hospital 49.5 ( 10.6) 49.6 ( 11.7)
After 12 months 48.1 ( 11.3) 45.0 ( 10.9) 0.077
p-Value Differences between baseline and after
12 months
0.831 0.001***
SD = Standard deviation.
= The Mann-Whitney U test was used to compare the distribution of ranks between the groups.
= The Wilcoxon Rank sum test was chosen to identify differences in each group at baseline and after 12 months.
Hohmann et al. Health and Quality of Life Outcomes 2010, 8:59
http://www.hqlo.com/content/8/1/59
Page 7 of 7
cated pharmacists based on a concept of PC may have a
positive impact on HRQoL.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
CH has made substantial contributions to conception and design, acquisition
of data, analysis and interpretation of data. RR, and JMK have made substantial
contributions to conception and design. All authors have been involved in
interpretation of data, drafting the manuscript or revising it critically for impor-
tant intellectual content and have given final approval of the version to be
published.
Acknowledgements
We would like to thank the participating patients, community pharmacists and
physicans who supported our study. We would also like to thank the Foerderini-
tiative Pharmazeutische Betreuung e.V., Berlin, Germany and the Dr. August und Dr.
Anni Lesmueller Stiftung, Munich, Germany for funding this project.
Author Details
1
Klinikum Fulda gAG, Department of Neurology, Pacelliallee 4, 36043 Fulda,
Germany,
2
Klinikum Fulda gAG, Department of Pharmacy and Patient
Counselling, Pacelliallee 4, 36043 Fulda, Germany and
3
European Institute for
Molecular Imaging - EIMI, University of Muenster, Technologiehof L1,
Mendelstrasse 11, 48149 Muenster, Germany
References
1. Kolominsky-Rabas P, Sarti C, Heuschmann PU, Graf C, Siemonsen S,
Neundoerfer B, Katalinic A, Lang E, Gassmann KG, Ritter von Stockert T: A
prospective community-based study of stroke in Germany - The
Erlangen stroke project (ESPro) - Incidence and case fatality at 1, 3, and
12 months. Stroke 1998, 29:2501-2506.
2. Manolio TA, Kronmal RA, Burke GL, O'Leary DH, Price TH: Short-term
predictors of incident stroke in older adults: The Cardiovascular Health
study. Stroke 1996, 27:1479-1486.
3. Carod-Artal J, Egido JA, Gonzlez JL, de Seijas EV: Quality of life among
stroke survivors evaluated 1 year after stroke: Experience of a stroke
unit. Stroke 2000, 31:2995-3000.
4. de Haan R: Measuring quality of life after stroke using the SF-36. Stroke
2002, 33:1176-1177.
5. Hobart JC, Williams LS, Moran K, Thompson AJ: Quality of life
measurement after stroke: uses and abuses of the SF-36. Stroke 2002,
33:1348-1356.
6. Anderson C, Laubscher S, Burns R: Validation of the Short Form 36 (SF-
36) Health Survey questionnaire among stroke patients. Stroke 1996,
27:1812-1816.
7. Hepler CD, Strand LM: Opportunities and responsibilities in
pharmaceutical care. Am J Hosp Pharm 1990, 47:533-543.
8. Schulz M, Verheyen F, Mhlig S, Mller JM, Mhlbauer K, Knop-
Schneickert E, Petermann F, Bergmann KC: Pharmaceutical Care Services
for Asthma patients: a controlled intervention study. J Clin Pharmaol
2001, 41:668-676.
9. Paulos CP, Nygren CEA, Celedon C, Carcamo CA: Impact of a
Pharmaceutical Care Program in a Community Pharmacy on Patients
with Dyslipidemia. Ann Pharmacother 2005, 39:939-943.
10. Carretero OA, Oparil S: Essential Hypertension: Part I: Definition and
Etiology. Circulation 2000, 101:329-335.
11. Craig ME, Hattersley A, Donaghue KC: Definition, epidemiology and
classification of diabetes in children and adolescents. Pediatric Diabetes
2009, 10(Suppl 12):3-12.
12. Ballantyne CM, O'Keefe JH, Gotto AM: Overview of Atherosclerosis and
Dyslipidemia. In Dyslipidemia & Atherosclerosis Essentials Volume Chapter
1. Fourth edition. Physicians's Press. Sudbury, MA: Jones and Bartlett;
2009:5.
13. Suenkeler IH, Nowak M, Misselwitz B, Kugler C, Schreiber W, Oertel W, Back
T: Timecourse of health-related quality of life as determined 3, 6 and 12
months after stroke. Relationship to neurological deficit, disability and
depression. J Neurol 2002, 249:1160-1167.
14. Hackett ML, Duncan JR, Anderson CS, Broad JB, Bonita R: Health-related
quality of life among long-term survivors of stroke: results from the
Auckland Stroke Study, 1991-1992. Stroke 2000, 31:440-447.
15. Mangiapane S, Schulz M, Muhlig S, Ihle P, Schubert I, Waldmann H:
Community pharmacy-based pharmaceutical care for asthma patients.
Ann Pharmacother 2005, 39:1817-1822.
16. Cote I, Moisan J, Chabot I, Gregoire J-P: Health-related quality of life in
hypertension: impact of a pharmacy intervention programme. Journal
of Clinical Pharmacy and Therapeutics 2005, 30:355-362.
17. Graesel E, Biehler J, Schmidt R, Schupp W: Intensification of the transition
between inpatient neurological rehabilitation and home care of stroke
patients. Controlled clinical trial with follow-up assessment six months
after discharge. Clinical Rehabilitation 2005, 19:725-736.
18. Wee HL, Cheung YB, Li SC, Fong KY, Thumboo J: The impact of diabetes
mellitus and other chronic medical conditions on health-related
Quality of Life: Is the whole greater than the sum of its parts? Health
and Quality of Life Outcomes 2005, 3:2.
doi: 10.1186/1477-7525-8-59
Cite this article as: Hohmann et al., Health-Related Quality of Life after Isch-
emic Stroke: The Impact of Pharmaceutical Interventions on Drug Therapy
(Pharmaceutical Care Concept) Health and Quality of Life Outcomes 2010, 8:59
Received: 8 March 2010 Accepted: 18 June 2010
Published: 18 June 2010
This article is available from: http://www.hqlo.com/content/8/1/59 2010 Hohmann et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Health and Quality of Life Outcomes 2010, 8:59
You might also like
- MSC1551 NAC Asthma COPD Medications Chart 2018 HR InternalDocument1 pageMSC1551 NAC Asthma COPD Medications Chart 2018 HR InternalDisha Jalan100% (1)
- Bangladesh National Formulary (BDNF) 5th Version 2019 PDFDocument924 pagesBangladesh National Formulary (BDNF) 5th Version 2019 PDFMSKC78% (9)
- Reduce Modifiable Cardiac Risk Factors in AdultsDocument4 pagesReduce Modifiable Cardiac Risk Factors in AdultsevangelinaNo ratings yet
- Impact of PharmacistDocument5 pagesImpact of PharmacistLeny MeiriyanaNo ratings yet
- A Descriptive Study of Adherence To Lifestyle Modification Factors Among Hypertensive PatientsDocument23 pagesA Descriptive Study of Adherence To Lifestyle Modification Factors Among Hypertensive PatientsSt. KhodijahNo ratings yet
- 2 Effects of A Pharmaceutical Care Intervention Coronary Heart DiseaseDocument16 pages2 Effects of A Pharmaceutical Care Intervention Coronary Heart DiseaseRosalinda Marquez VegaNo ratings yet
- Patterns of Antihypertensive Drug Utilization in Primary CareDocument11 pagesPatterns of Antihypertensive Drug Utilization in Primary CareIvan LiandoNo ratings yet
- Evaluation of A Pharmaceutical Care Program For Hypertensive Patients in Rural PortugalDocument7 pagesEvaluation of A Pharmaceutical Care Program For Hypertensive Patients in Rural PortugalNOorulain HyderNo ratings yet
- Antihypertension Non AdherenceDocument16 pagesAntihypertension Non AdherencebezieNo ratings yet
- Annals of General PsychiatryDocument9 pagesAnnals of General PsychiatryPutu Agus GrantikaNo ratings yet
- Makalah KesehatanDocument9 pagesMakalah KesehatanNini RahmiNo ratings yet
- Approach by Health Professionals To The Side Effects of Antihypertensive Therapy: Strategies For Improvement of AdherenceDocument10 pagesApproach by Health Professionals To The Side Effects of Antihypertensive Therapy: Strategies For Improvement of AdherenceSabrina JonesNo ratings yet
- DeJonge P 2003Document6 pagesDeJonge P 2003Camila AlmeidaNo ratings yet
- Science 6Document12 pagesScience 6Shinta Dian YustianaNo ratings yet
- Relationship Between Patients' Knowledge and Medication Adherence Among Patients With HypertensionDocument8 pagesRelationship Between Patients' Knowledge and Medication Adherence Among Patients With HypertensionWina MariaNo ratings yet
- Effect On Blood Pressure of A Continued Nursing Intervention Using Chronotherapeutics For Adult Chinese Hypertensive PatientsDocument9 pagesEffect On Blood Pressure of A Continued Nursing Intervention Using Chronotherapeutics For Adult Chinese Hypertensive PatientsadeliadeliaNo ratings yet
- Impact of A Designed Self-Care Program On Selected Outcomes Among Patients Undergoing HemodialysisDocument18 pagesImpact of A Designed Self-Care Program On Selected Outcomes Among Patients Undergoing HemodialysisImpact JournalsNo ratings yet
- Determinants of Hypertension Treatment Adherence ADocument7 pagesDeterminants of Hypertension Treatment Adherence ADr YusufNo ratings yet
- Complementary and Alternative Medicine As Part of Primary Health Care in GermanyDocument8 pagesComplementary and Alternative Medicine As Part of Primary Health Care in GermanyNancy KawilarangNo ratings yet
- JHH 20168Document8 pagesJHH 20168Anonymous bgcWQhRNo ratings yet
- 1471 2474 13 180 PDFDocument8 pages1471 2474 13 180 PDFDini BayuariNo ratings yet
- ResearchDocument75 pagesResearchArun AhirwarNo ratings yet
- Identifying and Measuring Outcomes 6MN3hDocument16 pagesIdentifying and Measuring Outcomes 6MN3hYazeed AsrawiNo ratings yet
- Impact of Pharmacist Clinical Interventions On Treatment Outcomes in Hypertensive Patients An Outcomes StudyDocument6 pagesImpact of Pharmacist Clinical Interventions On Treatment Outcomes in Hypertensive Patients An Outcomes StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Asgedom2018 Article AntihypertensiveMedicationAdheDocument8 pagesAsgedom2018 Article AntihypertensiveMedicationAdhehendriNo ratings yet
- Schizophrenia Treatment & Management - Approach Considerations, Antipsychotic Pharmacotherapy, Other PharmacotherapyDocument13 pagesSchizophrenia Treatment & Management - Approach Considerations, Antipsychotic Pharmacotherapy, Other PharmacotherapydilaNo ratings yet
- JJJGJHGJHGHDocument6 pagesJJJGJHGJHGHTaufik NurohmanNo ratings yet
- Article - The Devil Is in DetailDocument23 pagesArticle - The Devil Is in DetailHishamudin KadiranNo ratings yet
- Rubio Valera2013Document10 pagesRubio Valera2013Marcus Fábio leite AndradeNo ratings yet
- Cardiac Self-Efficacy and Quality of Life in Patients With Coronary Heart Disease: A Cross-Sectional Study From PalestineDocument13 pagesCardiac Self-Efficacy and Quality of Life in Patients With Coronary Heart Disease: A Cross-Sectional Study From Palestineشبلي غرايبهNo ratings yet
- RRL Hypertension ComplianceDocument30 pagesRRL Hypertension ComplianceAngelaTrinidadNo ratings yet
- M Ramirez Nurs660 TherapeuticstableDocument17 pagesM Ramirez Nurs660 Therapeuticstableapi-273459660No ratings yet
- Journal of Psychosomatic Research: M.C. Shedden-Mora, B. Groß, K. Lau, A. Gumz, K. Wegscheider, B. LöweDocument8 pagesJournal of Psychosomatic Research: M.C. Shedden-Mora, B. Groß, K. Lau, A. Gumz, K. Wegscheider, B. LöweSeva RenandoNo ratings yet
- Goudarzi 2020Document7 pagesGoudarzi 2020Herick Alvenus WillimNo ratings yet
- Bahan 2-DikonversiDocument11 pagesBahan 2-DikonversiMaya ismayaNo ratings yet
- Jurnal BING Kel 6Document11 pagesJurnal BING Kel 6Nisya Andesita HNo ratings yet
- Counseling Overweight Patients: Analysis of Preventive Encounters in Primary CareDocument7 pagesCounseling Overweight Patients: Analysis of Preventive Encounters in Primary CareAgil SulistyonoNo ratings yet
- HBM 3Document10 pagesHBM 3renzelpacleb123No ratings yet
- Polypill, Indications and Use 2.1Document12 pagesPolypill, Indications and Use 2.1jordiNo ratings yet
- PJMS 34 959Document5 pagesPJMS 34 959Husni FaridNo ratings yet
- The Determinants of Hypertension Awareness, Treatment, and Control in An Insured PopulationDocument7 pagesThe Determinants of Hypertension Awareness, Treatment, and Control in An Insured PopulationHugo Suarez RomeroNo ratings yet
- Psychological Interventions For The Management of Bipolar DisorderDocument9 pagesPsychological Interventions For The Management of Bipolar DisorderFausiah Ulva MNo ratings yet
- Validation of The Short Form of The Hypertension Quality of Life Questionnaire (MINICHAL)Document35 pagesValidation of The Short Form of The Hypertension Quality of Life Questionnaire (MINICHAL)Adi SaputraNo ratings yet
- Hypertension Control Programs in Occupational Settings: Yield Benefit, Pound Including 600,000 LeadingDocument6 pagesHypertension Control Programs in Occupational Settings: Yield Benefit, Pound Including 600,000 LeadingGrace LNo ratings yet
- Articles: Backgro UndDocument8 pagesArticles: Backgro UndHaryaman JustisiaNo ratings yet
- Coping Strategies and Blood Pressure Control Among Hypertensive Patients in A Nigerian Tertiary Health InstitutionDocument6 pagesCoping Strategies and Blood Pressure Control Among Hypertensive Patients in A Nigerian Tertiary Health Institutioniqra uroojNo ratings yet
- Evaluation of Medication Adherence in Lebanese Hypertensive PatientsDocument11 pagesEvaluation of Medication Adherence in Lebanese Hypertensive PatientsDoddo IndrayanaNo ratings yet
- Diabetes ComparativosDocument9 pagesDiabetes ComparativosMarlon Salguedo MadridNo ratings yet
- Adherence To Hiv Treatment: Drug Adherence Counselling Programme DevelopmentDocument6 pagesAdherence To Hiv Treatment: Drug Adherence Counselling Programme DevelopmentmakmgmNo ratings yet
- HPCP Assignment 2Document8 pagesHPCP Assignment 2mokshmshah492001No ratings yet
- Study of Drug Use in Essential Hypertension and Their ComplianceDocument13 pagesStudy of Drug Use in Essential Hypertension and Their ComplianceRachmat MuhammadNo ratings yet
- Anty - Hypertensive Need A Change RegimenDocument4 pagesAnty - Hypertensive Need A Change RegimenSyifa MunawarahNo ratings yet
- Etminani 2020Document18 pagesEtminani 2020José Carlos Sánchez-RamirezNo ratings yet
- Research ArticleDocument12 pagesResearch ArticletiarNo ratings yet
- Antidepressants and Health-Related Quality of Life For Patients With DepressionDocument14 pagesAntidepressants and Health-Related Quality of Life For Patients With Depressionjohndoe691488No ratings yet
- The Effects of Self-Management Education Tailored To Health Literacy OnDocument7 pagesThe Effects of Self-Management Education Tailored To Health Literacy OnDINDA PUTRI SAVIRANo ratings yet
- Journal Review Final PaperDocument10 pagesJournal Review Final Paperapi-464793486No ratings yet
- Jurnal Endokrin7Document8 pagesJurnal Endokrin7Anonymous a9Wtp0ArNo ratings yet
- BMC Cardiovascular DisordersDocument11 pagesBMC Cardiovascular DisordersjlventiganNo ratings yet
- Drug Adherence in Hypertension and Cardiovascular ProtectionFrom EverandDrug Adherence in Hypertension and Cardiovascular ProtectionMichel BurnierNo ratings yet
- Diabetes Risks from Prescription and Nonprescription Drugs: Mechanisms and Approaches to Risk ReductionFrom EverandDiabetes Risks from Prescription and Nonprescription Drugs: Mechanisms and Approaches to Risk ReductionNo ratings yet
- Finding the Path in Alzheimer’s Disease: Early Diagnosis to Ongoing Collaborative CareFrom EverandFinding the Path in Alzheimer’s Disease: Early Diagnosis to Ongoing Collaborative CareNo ratings yet
- Patient With Intra-Cranial Mass.: 3.1a. Pre-Contrast Axial T1 WTD MRI 3.1b. Post-Contrast Axial T1 WTD MRIDocument11 pagesPatient With Intra-Cranial Mass.: 3.1a. Pre-Contrast Axial T1 WTD MRI 3.1b. Post-Contrast Axial T1 WTD MRIDhila- Nailatul FadhilahNo ratings yet
- Ispei (: Klinik NnuroiogiDocument12 pagesIspei (: Klinik NnuroiogiDhila- Nailatul FadhilahNo ratings yet
- Level 2 Lesson 1: Future TenseDocument3 pagesLevel 2 Lesson 1: Future Tensedomon46No ratings yet
- Presentation Title: Subheading Goes HereDocument2 pagesPresentation Title: Subheading Goes HereDhila- Nailatul FadhilahNo ratings yet
- Projects Documents Team Links What's New: Insert Workgroup Logo On Slide MasterDocument2 pagesProjects Documents Team Links What's New: Insert Workgroup Logo On Slide MasterDhila- Nailatul FadhilahNo ratings yet
- DISPENSINGmanual Act. 2Document4 pagesDISPENSINGmanual Act. 2sybyl formenteraNo ratings yet
- Cotizacion Farmacia 17.08.2022Document48 pagesCotizacion Farmacia 17.08.2022Alicia OrtizNo ratings yet
- Pharmacy Assistant-HSS/Q5401 (Healthcare) : 1. Minimum Qualification For TrainersDocument7 pagesPharmacy Assistant-HSS/Q5401 (Healthcare) : 1. Minimum Qualification For TrainersBabar AliNo ratings yet
- TS Circ02 2015 PDFDocument22 pagesTS Circ02 2015 PDFAnonymous 9NlQ4n2oNo ratings yet
- M.pharm SyllabusDocument47 pagesM.pharm SyllabustusharphaleNo ratings yet
- Generic Name of Medicine (With Dosage Form and Strength) Brand Quantity Total Cost Supplier Manufacturer Acquisition CST Per UnitDocument72 pagesGeneric Name of Medicine (With Dosage Form and Strength) Brand Quantity Total Cost Supplier Manufacturer Acquisition CST Per UnitAlex SibalNo ratings yet
- Evaluation Enzyme Inhibitors Drug Discovery PDFDocument2 pagesEvaluation Enzyme Inhibitors Drug Discovery PDFKarlaNo ratings yet
- Applications of Communication Skills in Patient Care ServicesDocument2 pagesApplications of Communication Skills in Patient Care ServicesPooja agarwalNo ratings yet
- Module Health CLB 4 Going To PharmacyDocument4 pagesModule Health CLB 4 Going To PharmacyDanniNo ratings yet
- Crit Rev Ther Drug Carrier SystDocument1 pageCrit Rev Ther Drug Carrier SystBiswarup DasNo ratings yet
- PHAR 7633 Chapter 15 Multiple Oral Dose Administration: CP EquationDocument4 pagesPHAR 7633 Chapter 15 Multiple Oral Dose Administration: CP EquationSonia BaruaNo ratings yet
- Midterm Exam Reviewer: Surgical Handwashing QuizDocument9 pagesMidterm Exam Reviewer: Surgical Handwashing QuizOfficially RandomNo ratings yet
- Paarenteral ProductionDocument32 pagesPaarenteral ProductionHanuma KanthetiNo ratings yet
- Brochure 3rd World Congress On Pharmacology and Clinical TrialsDocument9 pagesBrochure 3rd World Congress On Pharmacology and Clinical TrialsbapaknyanadlirNo ratings yet
- Tgs Tgsan PKL - Copy BEnar BeDocument129 pagesTgs Tgsan PKL - Copy BEnar BeLuqiNo ratings yet
- InnovaDocument29 pagesInnovasanjay_gawaliNo ratings yet
- Final Pico Question InformaticsDocument5 pagesFinal Pico Question Informaticsapi-310396820No ratings yet
- Recent Advances in The Development of Anti-Tuberculosis Drugs Acting On Multidrug-Resistant Strains: A ReviewDocument18 pagesRecent Advances in The Development of Anti-Tuberculosis Drugs Acting On Multidrug-Resistant Strains: A Reviewmalik003No ratings yet
- Scale Up and Postapproval Changes (Supac) Guidance For Industry: A Regulatory NoteDocument9 pagesScale Up and Postapproval Changes (Supac) Guidance For Industry: A Regulatory NoteAKKAD PHARMANo ratings yet
- Pharma Entrepreneurship - Guidlines For Developing Pharma EntrepreneurshipDocument96 pagesPharma Entrepreneurship - Guidlines For Developing Pharma EntrepreneurshipkandyjoshiNo ratings yet
- Work Immersion Portfolio: Jhon Carlo Cera CatindoyDocument22 pagesWork Immersion Portfolio: Jhon Carlo Cera CatindoyJoel DufaleNo ratings yet
- List of Substandard Drugs2008Document8 pagesList of Substandard Drugs2008Mohammad Shahbaz AlamNo ratings yet
- Registered Medicine List 2014 FMHACADocument162 pagesRegistered Medicine List 2014 FMHACASindy ElfasNo ratings yet
- FDA Foia Log - May 2019Document56 pagesFDA Foia Log - May 2019Faiz RasoolNo ratings yet
- Pharmacy Business Plan - Executive SummaryDocument4 pagesPharmacy Business Plan - Executive SummaryI.k sidneyNo ratings yet
- A2. Syringe Labelling Critical AreasDocument34 pagesA2. Syringe Labelling Critical AreasAyusafura MuzamilNo ratings yet
- BCS 1 1 PDFDocument38 pagesBCS 1 1 PDFHely PatelNo ratings yet
- Abdi Ibrahim 02Document3 pagesAbdi Ibrahim 02jj_kkNo ratings yet