Professional Documents
Culture Documents
Clinical Skills Cheatsheet
Uploaded by
Cin BinCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Skills Cheatsheet
Uploaded by
Cin BinCopyright:
Available Formats
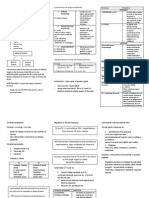
CLINICAL SKILLS CHEATSHEET- Taking Histories
Introduction
- Greeting, exchange names
- Explain what you are doing, obtain consent, and let patient know they can
stop at any time
Presenting complaint (ask with open questions)
- History of complaint (sequence of events)
- SOCRATES
- Confirm key problems and screen from associated symptoms
- What have you tried so far? What makes it better or worse
- SUMMARISE
Patient beliefs
- What do you think this is?
- Beliefs, concerns, expectations, effect of life, feelings, motivation for
lifestyle modification, self management strategies
- SUMMARISE
History
- Medical history
o Medical conditions- including mental, ongoing treatment and self-
management
o Past surgeries and hospitalisations, inc obstetrics
o Medications- dose, frequency, OTC/herbal
o Adherence to medications (hows it working/side effects)-
patients thoughts on medications
o Allergies/adverse effects
o SUMMARISE
- Family History
- Personal, occupational and social history
o Smoking/alcohol
o Drug use, history
o Sexual history
o Lifestyle
o SUMMARISE
Review of symptoms
- EXPLAIN WHY (check if we missed)- head to toe, be careful of what
patient has already said, ~10 things (specific to gender)
CONCLUSION
- Summarise key points for patient
- Check any other issues and concerns
- Tell them what the plan is after interview, leave in courteous manner
Take note of:
- What is going on
- What subsequent examination to do (or order tests)
- Management issues
- Any social or cultural issues
PHYSICAL EXAMINATION CHEATSHEET
Make sure to tell patient what youre doing for each step
Wash hands!
- start off with hand examination, go to vital signs (pulse, respiratory rate, blood
pressure and ear temperature)
Vital signs
- Make sure to elevate arm to heart heart
Hand Exam
- Look, feel, move
- Get patient to shake/move, check tremors
- Skin (scars, dry)
- Nails (clubbing, whiteness- liver)
- Circulation- color, temperature, pulses, capillary return
- Assess carpal, metocarpals, interphalangeal joints, MCPJs, CMCJs bones-
pain
- Motor function-
o Radial- extend wrist
o Medial- abduct pollis brevis (thumb)
o Ulna- abduct little finger
- Sensory function
o Radial- thumb
o Medial- middle palm
o Ulnar- little finger
- Specific things to check for
ENT exam
- Gross examination of paranasal sinuses, nose, throat, glands, mouth, neck
and ears (back)
- Oral cavity with spatula and torch (teeth, lips, tongue back, gingival
recesses, buccal mucosa, hard and soft palate, throat, pharynx)
- Nose and nasal passages with torch/spatula (check chonchae, swelling)
- Examaine paranasal sinuses
- Examine and palpate salivary glands (parotid, sublingual, submandibular,
mental)
- Palpate lymph nodes (submental, submandiubular, tonsillar,
preauricular) and check tonsils
- Ear exam
You might also like
- History Taking Physical ExamininationDocument41 pagesHistory Taking Physical ExamininationAya AmerNo ratings yet
- Approach To Differential Diagnosis PDFDocument62 pagesApproach To Differential Diagnosis PDFanasNo ratings yet
- The Problem Oriented Medical RecordDocument3 pagesThe Problem Oriented Medical RecordPia Angelica DizonNo ratings yet
- Aquifer Case 27Document4 pagesAquifer Case 27Dina KristevaNo ratings yet
- Aquifer Study CaseDocument8 pagesAquifer Study CaseRosanaNo ratings yet
- Transplantation: Presented by Santhiya K II M.SC Biotechnology 18PBT014Document54 pagesTransplantation: Presented by Santhiya K II M.SC Biotechnology 18PBT014AbiNo ratings yet
- Cardio-Physiology Exam QuestionsDocument17 pagesCardio-Physiology Exam Questionsjimmy100% (1)
- Biliary Disorders and Pancreatic Conditions ExplainedDocument59 pagesBiliary Disorders and Pancreatic Conditions ExplainedErick Sioco InsertoNo ratings yet
- Bates Thorax Lungs With TermsDocument4 pagesBates Thorax Lungs With Termscrystalshe100% (1)
- A Seminar About History TakingDocument13 pagesA Seminar About History Takingdr_jamal1983No ratings yet
- The Nervous System: Anatomy and Physiology of the Brain and Spinal CordDocument5 pagesThe Nervous System: Anatomy and Physiology of the Brain and Spinal CordChristine Marylou PalomoNo ratings yet
- Complete USMLE CS Guide Notes& - 40 1& - 41 & - 40 1& - 41Document99 pagesComplete USMLE CS Guide Notes& - 40 1& - 41 & - 40 1& - 41Elie Massaad100% (1)
- Genetics: OLFU - College of MedicineDocument7 pagesGenetics: OLFU - College of MedicineMiguel CuevasNo ratings yet
- DR Pradeep Usmle Step 2 Cs GuideDocument8 pagesDR Pradeep Usmle Step 2 Cs GuidepradeepNo ratings yet
- Evaluation Checklist Case 7 Bronchial AsthmaDocument7 pagesEvaluation Checklist Case 7 Bronchial AsthmaChristian MendiolaNo ratings yet
- Gyne Case COCDocument37 pagesGyne Case COCLian BaylosisNo ratings yet
- Pain Case - SOAP Note (2011)Document2 pagesPain Case - SOAP Note (2011)Alfie Lee100% (3)
- Health HistoryDocument19 pagesHealth HistoryAngelene Caliva100% (1)
- Thyroid DisordersDocument21 pagesThyroid DisordersSuliman GarallehNo ratings yet
- Brachial Plexus1 High Yield TableDocument3 pagesBrachial Plexus1 High Yield Tablenreena aslamNo ratings yet
- Er FinalsDocument63 pagesEr FinalsNaren RaviNo ratings yet
- Surgery Tips and ResourcesDocument2 pagesSurgery Tips and ResourcesAbeebs SalahouNo ratings yet
- My Usmle Step 2 CK Experience2Document3 pagesMy Usmle Step 2 CK Experience2jjNo ratings yet
- Aquifer Case - Summary - FamilyMedicine32 - 33-YDocument9 pagesAquifer Case - Summary - FamilyMedicine32 - 33-YHyunsoo EllisNo ratings yet
- Diseases of The Central Nervous SystemDocument5 pagesDiseases of The Central Nervous SystemWTF192No ratings yet
- Risk Factors - Step 2 PDFDocument5 pagesRisk Factors - Step 2 PDFAmberNo ratings yet
- Clinical Medication WorksheetDocument1 pageClinical Medication WorksheetSrkocher100% (1)
- Medical Terms in Lay Language2Document7 pagesMedical Terms in Lay Language2Mavra zNo ratings yet
- Abdominal Examination Check ListDocument9 pagesAbdominal Examination Check ListIbrahim Ahmed IbrahimNo ratings yet
- Hyperthyroidism History TakingDocument11 pagesHyperthyroidism History TakingmokkailinNo ratings yet
- The Detailed Neurologic Examination in Adults - UpToDate PDFDocument29 pagesThe Detailed Neurologic Examination in Adults - UpToDate PDFMiguel GarciaNo ratings yet
- PE Form - NeonateDocument3 pagesPE Form - NeonateStef ReyesNo ratings yet
- Medical HistoryDocument167 pagesMedical HistoryPragya Saran100% (1)
- Abdominal Examination: Male - Palpate Prostate Gland Female - Feel For CervixDocument5 pagesAbdominal Examination: Male - Palpate Prostate Gland Female - Feel For CervixRemelou Garchitorena AlfelorNo ratings yet
- Clinical CasesDocument12 pagesClinical CasesAndreea HanuNo ratings yet
- AQ FamilyMedicine 06Document12 pagesAQ FamilyMedicine 06Eduardo OrtizNo ratings yet
- The OSCE OrientationDocument25 pagesThe OSCE OrientationginadaisluNo ratings yet
- Endocrine Pathophysiology Nursing NotesDocument4 pagesEndocrine Pathophysiology Nursing Notesgrad_nurse_2015100% (2)
- Pestana VignettesDocument41 pagesPestana VignettesDane BrodkeNo ratings yet
- Cardiovascular AssessmentDocument21 pagesCardiovascular AssessmentRhitzle AnnNo ratings yet
- Nutshell NeuroDocument15 pagesNutshell NeuroAdeel abbas rajaNo ratings yet
- Endocrine ReviewDocument9 pagesEndocrine ReviewSpencer ThomasNo ratings yet
- Abdominal Examination: Before Examining The PatientDocument4 pagesAbdominal Examination: Before Examining The PatientrebeccaNo ratings yet
- Sign and SymptomsDocument8 pagesSign and SymptomsCaral Grace Gatdula-PenalbaNo ratings yet
- CS Physical Exam ChecklistDocument7 pagesCS Physical Exam Checklistxuni cNo ratings yet
- Admission NotesDocument16 pagesAdmission NotesCaisar Dewi MaulinaNo ratings yet
- Anaemia in Pregnancy: By-Dr. Soumya.p (2nd Yr PG) Mod - Dr. Rita. D (Professor and Hod)Document98 pagesAnaemia in Pregnancy: By-Dr. Soumya.p (2nd Yr PG) Mod - Dr. Rita. D (Professor and Hod)SoumyaNo ratings yet
- Heart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesDocument3 pagesHeart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesPrarthana Thiagarajan100% (3)
- Review ManualDocument2,812 pagesReview ManualdillyboyNo ratings yet
- Neuro Final Exam ReviewDocument23 pagesNeuro Final Exam ReviewAaron James GrayNo ratings yet
- Endocrine DisordersDocument3 pagesEndocrine DisordersIrish OrleansNo ratings yet
- First Aid PsychiatryDocument156 pagesFirst Aid PsychiatryMae Matira AbeladorNo ratings yet
- Cardiac Exam Guide: Inspection, Palpation, AuscultationDocument23 pagesCardiac Exam Guide: Inspection, Palpation, AuscultationAreza Eka PermanaNo ratings yet
- History Taking2Document25 pagesHistory Taking2Capture UnseenNo ratings yet
- Aquifer Case - Summary - FamilyMedicine21 - 12-YDocument10 pagesAquifer Case - Summary - FamilyMedicine21 - 12-YHyunsoo EllisNo ratings yet
- SHOCK Slide WorkbookDocument10 pagesSHOCK Slide WorkbookPATHMAPRIYA GANESANNo ratings yet
- Thorax and Lungs SGDocument2 pagesThorax and Lungs SGDestinee Caple100% (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Microcirculation as Related to ShockFrom EverandMicrocirculation as Related to ShockDavid SheproNo ratings yet
- Terry Berry Recognition Calendar 2020Document13 pagesTerry Berry Recognition Calendar 2020Anonymous lb5JB23No ratings yet
- Fat Burner: Fitzoye Nutrition IntroducingDocument6 pagesFat Burner: Fitzoye Nutrition IntroducingrajeshNo ratings yet
- Aortic AneurysmDocument26 pagesAortic Aneurysmchetanm2563100% (1)
- 13.24 Abdominal-InjuryDocument42 pages13.24 Abdominal-InjuryMuhammad FajarNo ratings yet
- Abas 3 TemplateDocument2 pagesAbas 3 Templatenathalie.gardnerNo ratings yet
- Understanding the pros and cons of early marriage for teenagersDocument15 pagesUnderstanding the pros and cons of early marriage for teenagersShoba ManoharanNo ratings yet
- Industrial Safety: University of Kirkuk College of Engineering Mechanical DepartmentDocument4 pagesIndustrial Safety: University of Kirkuk College of Engineering Mechanical DepartmentAbdullah HusseinNo ratings yet
- Marginal Ulcer, A Case StudyDocument4 pagesMarginal Ulcer, A Case StudySailaja NandennagariNo ratings yet
- Benefits of An Experimental Program of Equestrian Therapy For Children With ADHD PDFDocument10 pagesBenefits of An Experimental Program of Equestrian Therapy For Children With ADHD PDFJuli DeviaNo ratings yet
- Pai NMJI 2004 Systematic Reviews Illustrated Guide3Document10 pagesPai NMJI 2004 Systematic Reviews Illustrated Guide3mphil.rameshNo ratings yet
- Chapter 9 KeyDocument17 pagesChapter 9 KeySrinu WestNo ratings yet
- Drug Study - Cimetidine (Tagamet)Document3 pagesDrug Study - Cimetidine (Tagamet)mikErlh100% (3)
- 02 GeriatricsDocument38 pages02 Geriatricsandirio7486No ratings yet
- Eng QP FormatDocument15 pagesEng QP Formatpriyansh asnaniNo ratings yet
- Gina Cushenberry Nutrition Resume 2016Document6 pagesGina Cushenberry Nutrition Resume 2016api-308173770No ratings yet
- Dengue NS1Document1 pageDengue NS1rajNo ratings yet
- Bronchitis, Pneumonia and Bronchial Asthma in ChildrenDocument82 pagesBronchitis, Pneumonia and Bronchial Asthma in Childrenstrawberry pieNo ratings yet
- PATHFit I Chapter 4Document6 pagesPATHFit I Chapter 4bamboogabrieltaclaNo ratings yet
- Significance of Rural Development: Dr. Radhika KapurDocument16 pagesSignificance of Rural Development: Dr. Radhika KapurRay chijiokeNo ratings yet
- Eucalyptus OilDocument17 pagesEucalyptus OilSorinGeorgeNo ratings yet
- Challenges and Problems of Teenage Mothers During the PandemicDocument69 pagesChallenges and Problems of Teenage Mothers During the PandemicDesiree Joy GutierrezNo ratings yet
- Congenital Adrenal HyperplasiaDocument29 pagesCongenital Adrenal HyperplasiaMohan RaoNo ratings yet
- 2809 Genome 03Document2 pages2809 Genome 03api-278365530No ratings yet
- Engine Oil MsdsDocument4 pagesEngine Oil MsdsTawanda MushayiNo ratings yet
- Medicinal Plants Used To Combat A Major Gynecological ChallengeDocument13 pagesMedicinal Plants Used To Combat A Major Gynecological ChallengeESSENCE - International Journal for Environmental Rehabilitation and ConservaionNo ratings yet
- Pa Tho Physiology of Hodgkin'sDocument10 pagesPa Tho Physiology of Hodgkin'sIvica Rae100% (1)
- ANM application detailsDocument3 pagesANM application detailsSOFIKUL HUUSAINNo ratings yet
- ACE Personal Trainer Manual, 4 Edition: Cardiorespiratory Training: Programming and ProgressionsDocument42 pagesACE Personal Trainer Manual, 4 Edition: Cardiorespiratory Training: Programming and ProgressionsLouis TrầnNo ratings yet
- PNLE June 2007 With Key AnswersDocument82 pagesPNLE June 2007 With Key AnswersJustin CubillasNo ratings yet
- Lesson 2 - Counseling (DIASS)Document53 pagesLesson 2 - Counseling (DIASS)Majo Padolina100% (2)