Professional Documents
Culture Documents
Anaerobic Bacteria: Raroromiki Raroromiki
Uploaded by
Aldwin BagtasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anaerobic Bacteria: Raroromiki Raroromiki
Uploaded by
Aldwin BagtasCopyright:
Available Formats
RaRoRoMiKi RaRoRoMiKi
1
ANAEROBIC BACTERIA
CHARACTERICTICS:
Anaerobes generate energy by
fermentation (breakdown of sugar to
pyruvate)
Lack of the capacity to utilize O2 as a
terminal hydrogen acceptor
Some are sensitive to O2 concentration
as low as 0.5% O2
Most can survive in 3-5% O2
A few can grow poorly in the presence
of air
aerotolerant anaerobes (multiply in
the absence of oxygen like Clostridium
Histolyticum)
Many are members of the normal flora
created by presence of facultative
anaerobes
Obligate anaerobe- strictly no O2
OTHER CHARACTERISTICS
1. Part of normal flora
2. Can survive at O2 free
microenvironment of the body
3. Causes mix infection
4. Can grow on enrich media (reducing
agent) maintains redox potential
FACTORS THAT INHIBIT GROWTH OF
ANAEROBES BY OXYGEN
1. Toxic compounds are produce
- e.g. H2O2, superoxides
2. Absence of catalase and superoxide
dismutase
3. Oxidation of essential sulfhydryl groups
in enzymes without sufficient reducing
power to regenerate them
FACTORS RESPONSIBLE FOR THEIR VIRULENCE
Lipopolysaccharide
Promotes abscess formation,
enhanced coagulation
Polysaccharide capsule
Correlated with abscess
production
Enzymes
a. Collagenase
b. Heparinase
develop thrombophlebitis and
septic emboli
Short chain fatty acids
a. Butyrate seen on dental
plaque
b. Succinic acid- reduces
phagocytic killing
MULTIPLICATION OF THE OPPORTUNISTIC
PATHOGENS IS FACILITATED BY:
1. Inhibition of phagocytosis and intracellular
killing by PMN in the presence of
bacteroides by
a. Competition of opsonins
b. Inhibition of capsular materials
2. Protection of antibiotics, susceptibility
strains in mixtures thru destruction by the
beta lactamases
3. Utilization of O2 by facultative species that
aids in producing a suitable environment for
growth of anaerobe
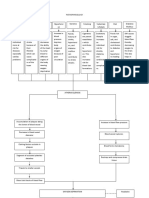
Morphology
Gram
stain
Genus
Sporeforming
bacilli
+ Clostridium
Non-
sporeforming
bacilli
+
Actinomyces,
Bifidobacteria, Eubacteria,
Propionibacterium,
Mobilincus, Lactobacilli
-
Bacteroides,
Fusobacterium, Prevotella,
Porphyromas
Non-
sporeforming
cocci
+
Peptococci,
Peptostreptococci,
Streptococci
- Veilonella
CLINICAL MANIFESTATIONS
A. Clinical hints
1. Odor- foul smelling odor, fishy odor
2. Tissue- gas
3. Location- proximity with mucus membrane
4. Necrotic tissue- black, gangrenous
5. Endocarditis with (-) blood culture
6. Infection associated with malignancy
7. Black discoloration
8. Blood containing exudates
9. Associated with sulfur granules- small black
granules
10. Bacteremic feature with jaundice
11. Human Bites
B. Infection produced
1. Bacteremia
2. Brain abscess
3. Otogenic meningitis
4. Dental infection
5. Pulmonary Infection
6. Puerperal sepsis peptostreptococcus &
peptococcus
7. Chronic meningitis
RaRoRoMiKi RaRoRoMiKi
2
LABORATORY DIAGNOSIS
A. Collection
- Anaerobes are endogenous in nature
I. Appropriate specimens for anaerobic culture
1. Pus
2. Pleural fluid thoracentesis
3. Urine Suprapubic aspiration
4. Pulmonary secretions
5. Uterine secretions or sinus tract material
II. Collection by needle aspiration is preferable
than swab culture because of:
a. Better survival of pathogen
b. Greater quantity of specimen
c. Less contamination with extraneous
organism are often achieved
B. Handling
- If swab must be used, a 2 tube system must be
used
a. 1st tube contains swab in O2 free CO2
b. 2nd tube contains PRAS (pre-reduced
anaerobically sterilized culture media)
Specimen should be placed in anaerobic
transport device with gas mixture
C. Isolation
Gram stain should be done in the
laboratory
a. Choice of appropriate media and
methods of culture
b. Quality control for the types of
bbacteria that laboratory culture reveal
A solid or liquid medium maybe used and
must provide an aerobic environment
anaerobic culture system (mechanically
reduces 02, CO2-terminal acceptor)
I. Anaerobic Jar
1. Candle jar
Reduces O2 environment
Only increases CO2 tension
2. Gas Pak Jar
a. Palladium aluminum coated pellets
Catalyst
Chemically reduces O2
Reacts with residual O2 in the
presence of h2 to form H2O
b. Gas Pak envelope
Generates CO2 and H2 gases
addition of 10 ml H2O = H2O2+CO2
c. Methylene blue strip
Indicator presence of O2
Blue (+) O2
White (-) O2
II. Anaerobic Glove Chamber
Close system
Used for premature babies e.g.incubator
III. Roll Tube
Has a pedal gas (CO2 & H2) would come out
place test tube directly to the outlets
METHODS FOR EXCLUDING OXYGEN
1. Fluid media containing fresh animal tissue
or 0.1% agar containing a reducing agent,
thioglycolate.
2. Anaerobic jar
3. Anaerobic glove chamber
D. Identification
- Plates are checked at:
18-24 hrs for faster growing species like
Clostridium perfringens & B. fragilis and
daily thereafter up to
5-7 days for slowly growing species lke
actinomyces, eubacterium and
propionbacterium
Genus is determined by:
Gram stain, cellular morphology, gas liquid
chromatography
Species determination is based on fermentation
of sugars and other biochemical determination
TREATMENT
Susceptibility testing should be done
Surgical drainage and resection of necrotic
tissue
debridement
Most are resistant to aminoglycosides
For bacteroides group, if resistant to
penicillin and cephalosporin, they may use:
a. Clindamycin
b. Metronidazole
c. Chloramphenicol
Special Thanks to:
ZombDAVID and RemingKENT!!
You might also like
- Unit 1 - 2.1 Anaerobic BacteriologyDocument35 pagesUnit 1 - 2.1 Anaerobic BacteriologyProvince Public Health Laboratory JanakpurNo ratings yet
- Anaerobic Culture .: Ahmed GomaaDocument42 pagesAnaerobic Culture .: Ahmed Gomaaah7510No ratings yet
- Physio - MicroorgDocument30 pagesPhysio - MicroorgLeeShauran100% (2)
- Lab #4Document5 pagesLab #4dianna dossantosNo ratings yet
- Topic 5 Controlling Microbial Growth in Vitro TranscriptDocument13 pagesTopic 5 Controlling Microbial Growth in Vitro TranscriptShayne Mata TeranteNo ratings yet
- Cultivation of AnaerobesDocument27 pagesCultivation of AnaerobesAnkush Biswas ABNo ratings yet
- Cultivation of Anaerobic BacteriaDocument21 pagesCultivation of Anaerobic BacteriaMallika Basera100% (1)
- Anaerobic Bacteria: Dept. of Microbiology Medical Faculty, Padjadjaran UniversityDocument52 pagesAnaerobic Bacteria: Dept. of Microbiology Medical Faculty, Padjadjaran UniversitySabrina Indri WardaniNo ratings yet
- Growth Media: CultureDocument11 pagesGrowth Media: CultureMERVENo ratings yet
- Bacteriology Lesson Week 2Document83 pagesBacteriology Lesson Week 2kerynne dyNo ratings yet
- ANAEROBES OF CLINICAL IMPORTANCEDocument16 pagesANAEROBES OF CLINICAL IMPORTANCESnowie BalansagNo ratings yet
- CHAPTER 11 MC3Document5 pagesCHAPTER 11 MC3Kiana Valerie MirandaNo ratings yet
- Curs 3 Lecture Nutrition and Bacteria CultivationDocument74 pagesCurs 3 Lecture Nutrition and Bacteria CultivationHåíthãm KhãtïßNo ratings yet
- Chapter 6 - Microbial Growth - ModifiedDocument14 pagesChapter 6 - Microbial Growth - ModifiedZiad BinFarsNo ratings yet
- Micropara Lab-6 2023Document10 pagesMicropara Lab-6 2023Dela Cruz, Juan Paulo L. BNSR IHSNNo ratings yet
- The Requirements For Growth Physical Requirements oDocument37 pagesThe Requirements For Growth Physical Requirements ojasmin_zamanNo ratings yet
- VOLUME 1: Gram Negative Bacteria of General, Medical, and Industrial ImportanceDocument5 pagesVOLUME 1: Gram Negative Bacteria of General, Medical, and Industrial ImportancenopenopenopeNo ratings yet
- Culture MethodsDocument26 pagesCulture Methodsdrunken monkeyNo ratings yet
- Anaerobic Bacteria GuideDocument52 pagesAnaerobic Bacteria GuidezaheerbinzubairNo ratings yet
- Bacteriology Handouts Objectives and StructuresDocument30 pagesBacteriology Handouts Objectives and StructuresTin BabistaNo ratings yet
- Preparing and testing culture mediaDocument3 pagesPreparing and testing culture mediaLeslie Ann PotencianoNo ratings yet
- Microbial Growth and PhysiologyDocument44 pagesMicrobial Growth and PhysiologyFu'e AbdumalikNo ratings yet
- An Introduction: Marx P. Catalan, RMTDocument48 pagesAn Introduction: Marx P. Catalan, RMTstoopiidgurl91% (11)
- Thermal Death Points and Microbial Control MethodsDocument18 pagesThermal Death Points and Microbial Control MethodsClaudia Keith McBroom43% (7)
- 3general Microbiology Microbial Growth and Metabolism For Students-ShadiDocument41 pages3general Microbiology Microbial Growth and Metabolism For Students-Shadisulaimanhijazi24No ratings yet
- Introduction To MicrobiologyDocument55 pagesIntroduction To MicrobiologyAngelica Valdez BalmesNo ratings yet
- A Review On Anaerobic ChambersDocument14 pagesA Review On Anaerobic ChambersSouvik TewariNo ratings yet
- Lab Report Pathogen Microbe 1Document11 pagesLab Report Pathogen Microbe 1Syazmin KhairuddinNo ratings yet
- Ecology Concepts (PART 4) : Role of Bacteria in The EnvironmentDocument13 pagesEcology Concepts (PART 4) : Role of Bacteria in The EnvironmentMhel CenidozaNo ratings yet
- Basic Anaerobic Culture MethodDocument19 pagesBasic Anaerobic Culture MethodChristine AghabiNo ratings yet
- Bacteriology HandoutDocument30 pagesBacteriology HandoutMoonyeen Jann Casera BalicNo ratings yet
- Chap 6 Reading WorksheetDocument5 pagesChap 6 Reading WorksheetSarahNo ratings yet
- Abrera, Lucky Lynn R.-Activity5 - MicroparaDocument5 pagesAbrera, Lucky Lynn R.-Activity5 - MicroparaLucky Lynn AbreraNo ratings yet
- Kepler Bio101Document4 pagesKepler Bio101wonderopokuasante9No ratings yet
- Microbiology and Parasitology1Document249 pagesMicrobiology and Parasitology1Keshi Wo100% (3)
- Anaerobic Bacteria IntroDocument34 pagesAnaerobic Bacteria IntroManny GabrielNo ratings yet
- Microbial Lecture 6Document6 pagesMicrobial Lecture 6Tri WiyonoNo ratings yet
- Ch. 6 ReviewDocument4 pagesCh. 6 ReviewaplesgjskNo ratings yet
- MicrobiologyDocument40 pagesMicrobiologyRasty Baku100% (1)
- Bacteriology HandoutsDocument30 pagesBacteriology HandoutsMarco Tolentino100% (8)
- Microbial Control Part 2Document26 pagesMicrobial Control Part 2Christiel John MagtibayNo ratings yet
- Bacterial Growth and Cultivation TechniquesDocument65 pagesBacterial Growth and Cultivation TechniquesKimberly Joy GregorioNo ratings yet
- Methods of Pure CultureDocument14 pagesMethods of Pure CulturejamilaNo ratings yet
- Chapter 2 Wastewater MicrobiologyDocument41 pagesChapter 2 Wastewater Microbiologykheng weiNo ratings yet
- Bacterial Morphology Stains Growth and NutritionDocument51 pagesBacterial Morphology Stains Growth and NutritionCelestine MarivelezNo ratings yet
- Food Spoilage and Preservation HODocument4 pagesFood Spoilage and Preservation HOSwathy Rao ShaikNo ratings yet
- Growth, Survival and Death of MicroorganismsDocument15 pagesGrowth, Survival and Death of MicroorganismsLidi SofyNo ratings yet
- Basic Microbiology& Immunology (PMI 311)Document50 pagesBasic Microbiology& Immunology (PMI 311)Meray George Wagih EbrahimNo ratings yet
- Micro para 2Document2 pagesMicro para 2Reselle EspirituNo ratings yet
- 5.lecture For Microbial Nutrition and GrowthDocument89 pages5.lecture For Microbial Nutrition and GrowthTrixie De GuzmanNo ratings yet
- Lab Manual SBUDocument19 pagesLab Manual SBUSiti Anis IzzatieNo ratings yet
- INSTRUMENTS FOR MICROBIOLOGY LABDocument12 pagesINSTRUMENTS FOR MICROBIOLOGY LABSTG COVERSNo ratings yet
- Microbial Respiration and Superoxide DismutaseDocument29 pagesMicrobial Respiration and Superoxide DismutaseAzman YaacubNo ratings yet
- Streptococcus Pneumoniae MbbsDocument53 pagesStreptococcus Pneumoniae MbbsShyam MishraNo ratings yet
- Bacte Notes #1 - Introduction To BacteriologyDocument14 pagesBacte Notes #1 - Introduction To BacteriologyMartin ClydeNo ratings yet
- Animal Cell Technology: Developments, Processes and ProductsFrom EverandAnimal Cell Technology: Developments, Processes and ProductsR. E. SpierNo ratings yet
- Complications in Anesthesiology 4th EditionDocument1,041 pagesComplications in Anesthesiology 4th EditionAldwin BagtasNo ratings yet
- Community Report For October 2014Document3 pagesCommunity Report For October 2014Aldwin BagtasNo ratings yet
- Letter of IntentDocument1 pageLetter of IntentAldwin BagtasNo ratings yet
- Physiologic OB: Maternal Physiology IDocument10 pagesPhysiologic OB: Maternal Physiology IAldwin BagtasNo ratings yet
- CENSUS - AUG 16-17 Day1Document2 pagesCENSUS - AUG 16-17 Day1Aldwin BagtasNo ratings yet
- Aida Amojilar HXDocument4 pagesAida Amojilar HXAldwin BagtasNo ratings yet
- RabiesDocument9 pagesRabiesAldwin BagtasNo ratings yet
- OB BulsaoDocument1 pageOB BulsaoAldwin BagtasNo ratings yet
- Form No. Iifb-26 Jose R. Reyes Memorial Medical CenterDocument1 pageForm No. Iifb-26 Jose R. Reyes Memorial Medical CenterAldwin BagtasNo ratings yet
- Bartola TaDocument2 pagesBartola TaAldwin BagtasNo ratings yet
- Census - Aug 22-23 Day1Document2 pagesCensus - Aug 22-23 Day1Aldwin BagtasNo ratings yet
- Census - Aug 25-26 Day1Document2 pagesCensus - Aug 25-26 Day1Aldwin BagtasNo ratings yet
- By Medical Students For Medical StudentsDocument90 pagesBy Medical Students For Medical StudentsAldwin BagtasNo ratings yet
- Census - Aug 17-18 Day2Document2 pagesCensus - Aug 17-18 Day2Aldwin BagtasNo ratings yet
- Census - Aug 18-19 Day3Document2 pagesCensus - Aug 18-19 Day3Aldwin BagtasNo ratings yet
- OB - TransesDocument112 pagesOB - TransesAldwin BagtasNo ratings yet
- CENSUS - AUG 16-17 Day1Document2 pagesCENSUS - AUG 16-17 Day1Aldwin BagtasNo ratings yet
- CENSUS - AUG 16-17 Day1Document2 pagesCENSUS - AUG 16-17 Day1Aldwin BagtasNo ratings yet
- Microbiology Lecture 6 - Bacterial GeneticsDocument4 pagesMicrobiology Lecture 6 - Bacterial GeneticsAldwin BagtasNo ratings yet
- Endorsement Aug24 25Document2 pagesEndorsement Aug24 25Aldwin BagtasNo ratings yet
- Chapter6 TB MeningitisDocument50 pagesChapter6 TB MeningitisAldwin BagtasNo ratings yet
- Census Aug 15-16Document2 pagesCensus Aug 15-16Aldwin BagtasNo ratings yet
- Sampling: Design and ProceduresDocument4 pagesSampling: Design and ProceduresAldwin BagtasNo ratings yet
- Microbiology Lecture 1 - Structure, Classification and MorphologyDocument4 pagesMicrobiology Lecture 1 - Structure, Classification and MorphologyAldwin BagtasNo ratings yet
- Non-Spore Forming BacteriaDocument2 pagesNon-Spore Forming BacteriaAldwin BagtasNo ratings yet
- JNC 7 (Klasifikasi Hipertensi) PDFDocument2 pagesJNC 7 (Klasifikasi Hipertensi) PDFAbdur RahmanNo ratings yet
- Medical exam form summaryDocument4 pagesMedical exam form summaryAldwin Bagtas0% (1)
- JNC 7 (Klasifikasi Hipertensi) PDFDocument2 pagesJNC 7 (Klasifikasi Hipertensi) PDFAbdur RahmanNo ratings yet
- Who FCH Cah 06.1Document123 pagesWho FCH Cah 06.1Ðr SalmaNo ratings yet
- Case Study: Exercise 2: Triage 1Document26 pagesCase Study: Exercise 2: Triage 1Chandra DewiNo ratings yet
- Health and its failure: Causes, Types, and Prevention of DiseasesDocument9 pagesHealth and its failure: Causes, Types, and Prevention of DiseasesAbhimanyu BahreeNo ratings yet
- Understanding Mental Illness Across CulturesDocument6 pagesUnderstanding Mental Illness Across Culturesjessaminequeency4128No ratings yet
- The SCARE Statement Consensus-Based Surgical Case ReportDocument7 pagesThe SCARE Statement Consensus-Based Surgical Case ReportIhsan KNo ratings yet
- Risk of Ovarian Cancer Algorithm (ROCA) Using Serial CA 125Document9 pagesRisk of Ovarian Cancer Algorithm (ROCA) Using Serial CA 125primadian atnaryanNo ratings yet
- ACCIDENT REPORTING AND INVESTIGATION PROCEDUREDocument23 pagesACCIDENT REPORTING AND INVESTIGATION PROCEDUREkirandevi1981No ratings yet
- UrinalysisDocument16 pagesUrinalysisJestha Parayno De Vera100% (6)
- Maharashtra Government PGM Admissions 2015-2016 Round 2 Selection ListDocument30 pagesMaharashtra Government PGM Admissions 2015-2016 Round 2 Selection ListAbhinav BhardwajNo ratings yet
- OB Meds WorksheetDocument18 pagesOB Meds WorksheetrickyandsheenaNo ratings yet
- MSA Testing Reveals Body's Energetic HealthDocument4 pagesMSA Testing Reveals Body's Energetic HealthDenise MathreNo ratings yet
- SAR Training Suggested ReadingDocument1 pageSAR Training Suggested Readingsesse_mNo ratings yet
- Top 10 Herbal Medicines in the PhilippinesDocument11 pagesTop 10 Herbal Medicines in the PhilippinesFritzie MacarayanNo ratings yet
- Pathophysiology Tia VS CvaDocument6 pagesPathophysiology Tia VS CvaRobby Nur Zam ZamNo ratings yet
- EBM On TherapyDocument34 pagesEBM On TherapyRahmah LatifahNo ratings yet
- Research Background: (Budget 2016: Chapter 5 - An Inclusive and Fair Canada, 2021)Document4 pagesResearch Background: (Budget 2016: Chapter 5 - An Inclusive and Fair Canada, 2021)Talha NaseemNo ratings yet
- John Paul PeraltaDocument5 pagesJohn Paul PeraltaAndrea Joyce AngelesNo ratings yet
- Colon Neuroendocrine Tumour Synoptic CAPDocument9 pagesColon Neuroendocrine Tumour Synoptic CAPMichael Herman ChuiNo ratings yet
- PHMB-Silver Sulfadiazine - HCDT-20-019Document7 pagesPHMB-Silver Sulfadiazine - HCDT-20-019gloriaNo ratings yet
- Infant CPRDocument1 pageInfant CPRDaniica MacaranasNo ratings yet
- Medicine BOF 2017 OctoberDocument7 pagesMedicine BOF 2017 Octoberweerawarna fernandoNo ratings yet
- The Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaDocument8 pagesThe Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaCristian Manuel Goicochea ChuqueNo ratings yet
- Recurrent Gingival Cyst of Adult: A Rare Case Report With Review of LiteratureDocument5 pagesRecurrent Gingival Cyst of Adult: A Rare Case Report With Review of Literaturesayantan karmakarNo ratings yet
- Therapeutic Communication TechniquesDocument4 pagesTherapeutic Communication TechniquesJustine Plaza100% (1)
- Comparison of Roth Appliance and Standard Edgewise Appliance Treatment ResultsDocument9 pagesComparison of Roth Appliance and Standard Edgewise Appliance Treatment ResultsseboistttNo ratings yet
- Errata: Shadow of The Demon LordDocument3 pagesErrata: Shadow of The Demon LordKaio CorsatoNo ratings yet
- Oral and Maxillofacial PathologyDocument79 pagesOral and Maxillofacial PathologyMai AnhNo ratings yet
- TESCTflyer 2012Document11 pagesTESCTflyer 2012Marco TraubNo ratings yet
- Eosinophin in Infectious DiseaseDocument29 pagesEosinophin in Infectious DiseasentnquynhproNo ratings yet
- Thyroidectomy Nursing CareDocument73 pagesThyroidectomy Nursing CareZNEROL100% (1)
- Acute Lymphoblastic LeukaemiaDocument3 pagesAcute Lymphoblastic LeukaemiamelpaniNo ratings yet