Professional Documents
Culture Documents
J.V. Divatia - Hypercalcemia PDF
Uploaded by
Aji SuyonoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
J.V. Divatia - Hypercalcemia PDF
Uploaded by
Aji SuyonoCopyright:
Available Formats
Malignant Hypercalcemia
JV Divatia
Professor and Head
Department of Anaesthesia, Critical Care and Pain
Tata Memorial Hospital
Mumbai, India
Physiologic Role of Ca
Contraction of skeletal, cardiac, and smooth
muscles
Blood clotting;
Transmission of nerve impulses
Excitable cells, such as neurons, are very
sensitive to changes in calcium ion concentrations
Hypercalcemia : progressive depression of the
nervous system
Hypocalcemia : CNS excitation
Distribution of Ca
0.1 per cent of the
total body Ca is in
the ECF
1 per cent is in the
cells
Rest is stored in
bones
bones can serve as
large reservoirs
Ionic Ca is the form that is important for
most functions of calcium in the body
Case
62 y/o male with h/o squamous cell
carcinoma of tonsillar pillar
treated 18 months prior with combined
chemo/XRT
presents with 2 weeks of worsening
fatigue, anorexia, polyuria with occasional
incontinence, constipation, and muscle
weakness
Examination
Fluctuating level of consciousness
Vitals normal, no fever
Dehydrated
Coarse upper airway sounds
No other pertinent findings
Investigations
CBC normal
Mildly elevated BUN and Cr
Normal LFTs
Standard electrolytes normal
Concern of pneumonia
Chest x-ray ordered
Multiple pulmonary metastases
Calcium checked
4.5 mmol / L
Hypercalcemia
Epidemiology
Occurs in about 10 to 20% of patients with
cancer
Both solid tumors and leukemias
Most common
Breast
Lung
Multiple myeloma
Pathogenesis
Three mechanisms
Osteolytic metastases with local cytokine
release
Tumor secretion of parathyroid hormone-
related protein (PTHrP)
Tumor production of calcitriol
Osteolytic Metastases
Osteolytic Metastases
Breast cancer
Non-small cell lung cancer
Cytokines released
Tumor necrosis factor
Interleukin-1
Stimulate osteoclast precursor differentiation
into mature osteoclasts
Leading to more bone breakdown and release of
calcium
Parathyroid HormoneRelated Protein
Responsible for most instances of hypercalcemia
of malignancy
Little influence on calcium homeostasis
except in disease states, when large tumors, especially
of the squamous cell type, lead to massive
overproduction of the hormone
Developmental influences on fetal bone
development and in adult physiology
PTH-Related Protein
Most common in patients with non-
metastatic tumors
Called humoral hypercalcemia of
malignancy
Secretion of PTH itself is a rare event
PTHrP binds to same receptor as PTH
and stimulates adeynylate cyclase activity
Increased bone resorption
Increases kidney calcium reabsorption and
phosphate excretion
Calcitriol
Hodgkins disease (mechanism in
majority)
Non-Hodgkins (mechanism in 1/3)
Usually responds to glucocorticoid therapy
Diagnosis
Hypercalcemia : Manifestations
Gastrointestinal
Constipation is most
common
Anorexia, Vague
abdominal pain
Rarely can lead to
pancreatitis
Renal
Nephrolithiasis
More common in
hyperparathyroidism
Nephrogenic diabetes
insipidus
Polyuria, polydipsia
Chronic renal failure
Longstanding high Ca
Usually nonspecific
Hypercalcemia : Manifestations
Cardiovascular
Short QT interval
Supraventricular
arrhythmias
Ventricular
arrhythmias
Neuropsychiatric
Anxiety
Depression
Cognitive dysfunction
Delirium
Psychosis
Hallucinations
Somnolence
Coma
ECG changes in Hypercalcemia
C C C C
Suspect Hypercalcemia.
In any cancer patient presenting with
acute pancreatitis, unexplained
somnolence or polyuria
Due to underlying malignancy in any
patient presenting with acute pancreatitis,
unexplained somnolence or polyuria
Malignancy must be ruled out in patients
that present with a very high calcium and
no other obvious cause
C C C C
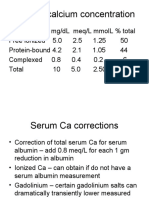
Investigations
Total Ca 10.8
mg/dL
Albumin = 1.2g/dL
Na 138 mmol/L
Cl 90 mmol/L
K 5.6 mmol/L
Corrected Ca ?
Ionized Ca
Total Ca
Calculate Corrected Ca
Total Ca + [0.8(4.0 albumin)].
Serum creatinine, electrolytes,
& alkaline phosphatase.
A low serum Cl (<100 mEq/L)
suggests hypercalcemia of
malignancy.
C C C C
13 mg/dL
Treatment
Aims
Lower serum calcium concentration
Treat complications if present
Treat underlying disease
Hydration is of utmost importance in these
patients, and intravenous saline should be given
rapidly once hypercalcemia is confirmed.
Hypercalcemia causes hypovolemia and
hypovolemia aggravates hypercalcemia
C C C C
Hydration!
Volume
Large volume of normal Saline
administration
Expands intravascular volume
Increases calcium excretion
Inhibition of proximal tubule and loop
reabosrption
Reduces passive reabsorption of calicum
Follow fluid status b/c of danger of fluid
overload
Fluid therapy
Give 1 L NS over first hour, then at lower rate till
hypovolemia is corrected
Establish urine output
Exercise caution: Close CVS monitoring
Renal impairment
Cardiovascular dysfunction
C C C C
Start diuretics
Only after VOLUME REPLETION
hypovolemia causes renal hypoperfusion
hampering calcium excretion.
Consider loop diuretics
Very useful if hypervolemia exists
C C C C
Start specific therapy
Bisphosphonates
Pamidronate: 6090 mg IV 24 hours OR
Zoledronic acid: 4 mg IV over 15 minutes
Calcitonin
Useful as rapid onset
48 IU/Kg SC or IV every 12 hours
Glucocorticoids (especially in lymphoma)
Prednisolone: 60 mg/day PO or
Hydrocortisone: 100 mg IV every 6 hours
C C C C
Calcitonin
Salmon calcitonin
Increases renal excretion of calcium
Decreases bone reabsorption by
interfering with osteoclast maturation
Weak agent
Works the fastest
Bisphosphonates
Adsorb to the surface of bone
hyroxyapatite
Interfere with osteoclast activity
Cytotoxic to osteoclasts
Inhibit calcium release from bone
Three commonly used
Pamidronate
Zoledronic acid
Etidronate (1
st
generation, weaker)
Bisphosphonates
More potent than calcitonin
Maxium effect occurs in 2 to 4 days
Trend to use of IV zoledronic acid in the
acute situation
Both are can be renal toxic
More potent than pamidronate
Administered over a shorter period of time (15
minutes vs. 2 hours)
Side effect
Osteonecrosis of the jaw
Recent case reports of jaw bone necrosis
in patients on pamidronate
EDUCATION needed
Gallium Nitrate
Effective
More potential for nephrotoxicity
Rarely used
Dialysis
Last resort
Dialysis fluid with little or no calcium is
effective
Useful when patients cant tolerate large
volume resuscitation
If calcium needs to be correct emergently
Management
Decrease dietary intake of calcium
Treat the Cause
Chemotherapy or Radiation if feasible
Evaluate prognosis
Hypercalcemia occurs in many advanced
malignancies
C C C C
C C C C
High index of suspicion
Measure serum calcium
Mild hypercalcemia
11 to 12 mg/dL
Asymptomatic
Hydration with saline
Eliminate dietary sources
of calcium & thiazide
diuretics
Moderate hypercalcemia
12 to 18 mg/dL
Symptomatic
Hydration
Loop diuretics
Bisphosphonate
Eliminate dietary calcium
thiazide diuretics
Severe hypercalcemia
> 18 mg/dL
Hydration
Loop diuretics
Calcitonin
Bisphosphonates
Steriods
Hemodialysis
Eliminate dietary Calcium
thiazide diuretics
Measure serum calcium and other
electrolytes particularly serum K
at least BD till Ca decreasing
Treatment of Hypercalcemia
16
th
APACCM
February 14-18, Jaipur, India
Physical Findings
Usually not specific
Dehydration secondary to diuresis caused
by the hypercalcemia
Corneal deposition of calcium
band keratopathy on slit lamp exam
Diagnosis
Malignancy must be ruled out in patients
that present with a very high calcium and
no other obvious cause
You might also like
- Fluids and ElectrolytesDocument31 pagesFluids and ElectrolytesUmarNo ratings yet
- 1 - Fluid and Electrolytes (Schwartz Based)Document52 pages1 - Fluid and Electrolytes (Schwartz Based)Alexandra RebosuraNo ratings yet
- 27 - Hypo and Hypernatremia - and Hypo and Hyperkalieama PDFDocument48 pages27 - Hypo and Hypernatremia - and Hypo and Hyperkalieama PDFEITHAR OmarNo ratings yet
- LEC 3 Parathyroid Gland DisordersDocument39 pagesLEC 3 Parathyroid Gland Disordersalhusien.abd2000No ratings yet
- Parathyroid & Calcium 1Document52 pagesParathyroid & Calcium 1Mujeeb AfzalNo ratings yet
- Calcium HomeostasisDocument37 pagesCalcium Homeostasispolog.jm610No ratings yet
- Hyperkalemia: An SEO-Optimized Guide to Diagnosis and TreatmentDocument22 pagesHyperkalemia: An SEO-Optimized Guide to Diagnosis and TreatmentsuviacesoNo ratings yet
- Management of Potassium Disorders 17706 ArticleDocument4 pagesManagement of Potassium Disorders 17706 ArticlealeNo ratings yet
- SLIDE03 FluidElectrolyteImbalanceDocument57 pagesSLIDE03 FluidElectrolyteImbalanceGrace Amato-Moore100% (1)
- Hypercalcemia & MSCCDocument29 pagesHypercalcemia & MSCCSA NodeNo ratings yet
- Hippo EM Board Review - Electrolyte Emergencies Written SummaryDocument5 pagesHippo EM Board Review - Electrolyte Emergencies Written SummaryMichael IvanNo ratings yet
- Hypercalcemia Diagnosis and TreatmentDocument5 pagesHypercalcemia Diagnosis and Treatmentandrei_groza_2No ratings yet
- HypocalcemiaDocument34 pagesHypocalcemiaClaudia IrimieNo ratings yet
- Disorders of Potassium Balance: Zhao Chenghai PathophysiologyDocument24 pagesDisorders of Potassium Balance: Zhao Chenghai PathophysiologyBayu SetiaNo ratings yet
- TWIS, Fluid and Electrolytes-4Document45 pagesTWIS, Fluid and Electrolytes-4Madison FNo ratings yet
- Hyperparathyroid Case Report: A Self TestingDocument16 pagesHyperparathyroid Case Report: A Self Testinghusna fauziahNo ratings yet
- Pathology of Parathyrid Gland FinalDocument63 pagesPathology of Parathyrid Gland FinalGurpreet Kaur SagooNo ratings yet
- Common Electrolyte Disturbances and Management Edited 2023Document46 pagesCommon Electrolyte Disturbances and Management Edited 2023abdurabengNo ratings yet
- Calcium HomeostasisDocument38 pagesCalcium Homeostasiskelvinmaina9993No ratings yet
- Lect 9 Parathyroid Gland-1Document30 pagesLect 9 Parathyroid Gland-1warda farooqNo ratings yet
- Parathyroid Gland AnatomyDocument27 pagesParathyroid Gland AnatomyABUBEKER BESHIRNo ratings yet
- Disorders of K BalanceDocument23 pagesDisorders of K BalanceElvis obajeNo ratings yet
- Fluid and ElectrolyteDocument71 pagesFluid and ElectrolytePratishtha SinghNo ratings yet
- אלון קלציום חלק 3Document25 pagesאלון קלציום חלק 3Alon GoldfainerNo ratings yet
- Tau Chempath Lecture - Fluid & Electrolyte BalanceDocument48 pagesTau Chempath Lecture - Fluid & Electrolyte BalanceJoshua KalundaNo ratings yet
- Fluids and Electrolyte DisordersDocument74 pagesFluids and Electrolyte DisordersPrincewill SeiyefaNo ratings yet
- Electrolyte Imbalances and Their Management.: by Nabawanda Saluwa Facilitator: DR - Ssebuliba MosesDocument44 pagesElectrolyte Imbalances and Their Management.: by Nabawanda Saluwa Facilitator: DR - Ssebuliba MosesNinaNo ratings yet
- Calcium and Magnesium Imbalances: Arlyn Olivas ReportDocument16 pagesCalcium and Magnesium Imbalances: Arlyn Olivas ReportAngelica Mercado SirotNo ratings yet
- Drugs Affecting Calcium Balance: Harsh Vinayak Roll No. 39 Mbbs 2 Yr Student BATCH 2019 Rdasmc, AyodhyaDocument24 pagesDrugs Affecting Calcium Balance: Harsh Vinayak Roll No. 39 Mbbs 2 Yr Student BATCH 2019 Rdasmc, AyodhyaA2Z GyanNo ratings yet
- Chapter 2 - C - III Portal HypertensionDocument37 pagesChapter 2 - C - III Portal HypertensionEmmaNo ratings yet
- Baldwin Tub Ulo InterstitialDocument36 pagesBaldwin Tub Ulo InterstitialdrryanalwynNo ratings yet
- Drugs Affecting Calcium BalanceDocument63 pagesDrugs Affecting Calcium BalanceRd Chandane100% (1)
- Plasma Enzyme DiagnosisDocument30 pagesPlasma Enzyme DiagnosisKayode IbitoyeNo ratings yet
- Renal Diseases " Review "Document22 pagesRenal Diseases " Review "api-3827876No ratings yet
- By DR Madhusudan C Associate Professor Department of MedicineDocument39 pagesBy DR Madhusudan C Associate Professor Department of MedicineTeena ChandranNo ratings yet
- Acetaminophen Toxicity: Michira I Getange Umb/15-A/054Document31 pagesAcetaminophen Toxicity: Michira I Getange Umb/15-A/054Ahmed Ben BellaNo ratings yet
- HypoparathyroidismDocument28 pagesHypoparathyroidismRon Opulencia100% (2)
- Tumor Lysis SyndromeDocument12 pagesTumor Lysis Syndromeapi-647779956No ratings yet
- Calcium, Phosphate, MagnesiumDocument55 pagesCalcium, Phosphate, MagnesiumUdochukwu EnebeNo ratings yet
- Body FluidDocument37 pagesBody FluidBir Mohammad SonetNo ratings yet
- Surgical Diseases of The Parathyroid GlandsDocument34 pagesSurgical Diseases of The Parathyroid Glandsanand787No ratings yet
- Electrolytres ImbalancesDocument39 pagesElectrolytres ImbalancesALLAINE MARIE TANNo ratings yet
- Alternatives To Transfusion 2 AK-VDocument29 pagesAlternatives To Transfusion 2 AK-VJanet ChanNo ratings yet
- FLUID AND ELECTROLYTE THERAPYDocument47 pagesFLUID AND ELECTROLYTE THERAPYSeblewongel AsemeNo ratings yet
- Hypercalcemia: Colorado ACP Meeting February 2017 David Tanaka MD FACPDocument33 pagesHypercalcemia: Colorado ACP Meeting February 2017 David Tanaka MD FACPRo KohnNo ratings yet
- ELECTROLYTE AND ACID-BASE (Final)Document55 pagesELECTROLYTE AND ACID-BASE (Final)Minale MenberuNo ratings yet
- PALS Fluids and ElectrolytesDocument32 pagesPALS Fluids and ElectrolytesZi SongNo ratings yet
- Hypernatremia and Fluid Resuscitation: Staci Smith, DODocument34 pagesHypernatremia and Fluid Resuscitation: Staci Smith, DOSyed BuRhan Ud-DinNo ratings yet
- Principle of Fluid & Electrolyte Management in ADocument47 pagesPrinciple of Fluid & Electrolyte Management in AAbdulazeez Abdulmalik100% (1)
- Acute Renal Failure: The Kidney Is Your Friend (Under 40 CharactersDocument31 pagesAcute Renal Failure: The Kidney Is Your Friend (Under 40 CharactersAlina BoiangiuNo ratings yet
- Case Presentation Hypokalemic ManDocument61 pagesCase Presentation Hypokalemic ManHussain AzharNo ratings yet
- HyponatremiaDocument42 pagesHyponatremiaAbdu Raheem100% (1)
- Disorders of Calcium, Inorganic Phosphate and Magnesium Metabolism 1Document62 pagesDisorders of Calcium, Inorganic Phosphate and Magnesium Metabolism 1IiiNo ratings yet
- GOUT AND PSEUDOGOUT: CRYSTAL-ASSOCIATED ARTHRITISDocument56 pagesGOUT AND PSEUDOGOUT: CRYSTAL-ASSOCIATED ARTHRITISSindhu BabuNo ratings yet
- Fluid and Electrolyte NewDocument54 pagesFluid and Electrolyte NewSelam Tesfaye ShebaNo ratings yet
- Fluid & Electrolyte 2Document47 pagesFluid & Electrolyte 2Worku KifleNo ratings yet
- Fluid & Electrolyte ImbalanceDocument47 pagesFluid & Electrolyte ImbalanceBijeta ThapaNo ratings yet
- CALCIUM METABOLISM RaminDocument42 pagesCALCIUM METABOLISM RaminRamin MaharjanNo ratings yet
- Internal PluginDocument1 pageInternal PluginAji SuyonoNo ratings yet
- Derfibrilalltorrr'' ' ' ''LJLJLHJKHJKHKHKDocument109 pagesDerfibrilalltorrr'' ' ' ''LJLJLHJKHJKHKHKazli yudhaNo ratings yet
- 1 Cardiac Arrest Pea and Asystole - 2015 PDFDocument1 page1 Cardiac Arrest Pea and Asystole - 2015 PDFAivi PhungNo ratings yet
- Algo StrokeDocument2 pagesAlgo StrokeLocomotorica FK Uki100% (1)
- Algo PostarrestDocument1 pageAlgo PostarrestMuhammad Rizki ImannudinNo ratings yet
- Algo Acs PDFDocument1 pageAlgo Acs PDFNety Pandung SalembanNo ratings yet
- Algo Acs PDFDocument1 pageAlgo Acs PDFNety Pandung SalembanNo ratings yet
- Shout For Help/Activate Emergency Response: CPR StartDocument2 pagesShout For Help/Activate Emergency Response: CPR StartdavpierNo ratings yet
- Williamson A, A Review of Three Commonly Used Visual Analogue ScoreDocument1 pageWilliamson A, A Review of Three Commonly Used Visual Analogue ScoreAji SuyonoNo ratings yet
- Strategies in The Selection of Antibiotic Therapy in The ICUDocument56 pagesStrategies in The Selection of Antibiotic Therapy in The ICUAji SuyonoNo ratings yet
- KateterisasiDocument12 pagesKateterisasiAji SuyonoNo ratings yet
- Soal B. InggrisDocument9 pagesSoal B. InggrisAji SuyonoNo ratings yet
- Prosedur Pengiriman Rekrutmen PkhiDocument1 pageProsedur Pengiriman Rekrutmen PkhiAji SuyonoNo ratings yet
- Pembahasan Soal UN Bahasa Inggris SMP 2012 (Paket Soal E45) PDFDocument16 pagesPembahasan Soal UN Bahasa Inggris SMP 2012 (Paket Soal E45) PDFWayan Sudiarta75% (4)
- Human Anatomy - Module 1 & 2 - Final TermDocument46 pagesHuman Anatomy - Module 1 & 2 - Final TermwelpNo ratings yet
- Bone DiseasesDocument21 pagesBone DiseasesshawetshaebanNo ratings yet
- Principles of Anatomy and Physiology 14th Edition PDFDocument21 pagesPrinciples of Anatomy and Physiology 14th Edition PDFTATHAGATA MACHERLA27% (82)
- Endocrine PathologyDocument13 pagesEndocrine Pathologysarguss14100% (1)
- Diagnosis, Evaluation, Prevention, and Treatment of CKD-MBDDocument71 pagesDiagnosis, Evaluation, Prevention, and Treatment of CKD-MBDJinnasit Tee0% (1)
- Pharmacology Test 3 ReviewDocument6 pagesPharmacology Test 3 ReviewNatalia BortellNo ratings yet
- Physiology & Pathophysiology - 2000Document4,648 pagesPhysiology & Pathophysiology - 2000tcabanilNo ratings yet
- Chronic Kidney Disease Feb 2021Document56 pagesChronic Kidney Disease Feb 2021ToyoNo ratings yet
- Endocrine Histology NotesDocument5 pagesEndocrine Histology NotesJulie TranNo ratings yet
- Test Bank Gould Pathophysiology 5th EditionDocument18 pagesTest Bank Gould Pathophysiology 5th EditionKeith Estrada100% (20)
- Human Physiology LecturesDocument171 pagesHuman Physiology LecturesPhysiology by Dr Raghuveer57% (7)
- Musculoskeletal Manifestations of Systemic DiseasesDocument16 pagesMusculoskeletal Manifestations of Systemic Diseasesreem100% (1)
- TumsDocument2 pagesTumsAdrianne BazoNo ratings yet
- Osmosis Endocrine, Pathology - Thyroid and Parathyroid Disorders - Hyperparathyroidism and Hypoparathyroidism PDFDocument5 pagesOsmosis Endocrine, Pathology - Thyroid and Parathyroid Disorders - Hyperparathyroidism and Hypoparathyroidism PDFYusril MarhaenNo ratings yet
- The Effect of Inflammation On BoneDocument14 pagesThe Effect of Inflammation On BoneKelas CNo ratings yet
- Ray Peat Various TopicsDocument4 pagesRay Peat Various TopicsTamaraBlickhan100% (3)
- PHR 121 Anatomy & Physiology: Diploma in PharmacyDocument51 pagesPHR 121 Anatomy & Physiology: Diploma in PharmacyAzmi ArifinNo ratings yet
- Endocrinology 9912Document64 pagesEndocrinology 9912Ravi Kant IyerNo ratings yet
- PATOFISIOLOGI ENDOKRIN & METABOLIKDocument192 pagesPATOFISIOLOGI ENDOKRIN & METABOLIKEsa Karimatuz ZaharaNo ratings yet
- Endocrine Case StudyDocument3 pagesEndocrine Case StudyJenny ViNo ratings yet
- Anemia in Renal DiseaseDocument59 pagesAnemia in Renal DiseaseShephali SharmaNo ratings yet
- Calcium Homeostasis: Endocrine Regulation of (Ca)Document4 pagesCalcium Homeostasis: Endocrine Regulation of (Ca)PRANAB KUMAR MUKHERJEENo ratings yet
- Pediatric Reference Ranges Endocrinology 0981 PDFDocument14 pagesPediatric Reference Ranges Endocrinology 0981 PDFMMCSTORENo ratings yet
- Calcium Case Report: The Perfect Lesson in Electrolyte BalanceDocument28 pagesCalcium Case Report: The Perfect Lesson in Electrolyte BalanceLucius33No ratings yet
- HypercalcemiaDocument26 pagesHypercalcemiaLiezel Mae DyNo ratings yet
- Calsium and StuntingDocument6 pagesCalsium and Stuntingmira watiNo ratings yet
- MCEM Original Practice MCQs No2Document11 pagesMCEM Original Practice MCQs No2Ugeshwaran Aristotle Reddy100% (2)
- Feline Chronic Kidney Disease - Integrated ApproachDocument12 pagesFeline Chronic Kidney Disease - Integrated ApproachClara SanchezNo ratings yet
- Complete Guide To Keto SupplementsDocument6 pagesComplete Guide To Keto Supplementssvasta24No ratings yet
- Chemical Coordination 1Document22 pagesChemical Coordination 1SureshNo ratings yet