Professional Documents
Culture Documents
Michigan Department of Community Health: LabLink Spring 2014
Uploaded by
Michigan News0 ratings0% found this document useful (0 votes)
39 views6 pagesDr. James T. Rudrik has accepted the permanent position as Director of the Division of Infectious Diseases effective March 24, 2014. He has more than 30 years of service in the laboratory testing field, both in private as well as public institutions. Please feel free to contact Dr. Rudrik regarding any issues related to infectious disease laboratory testing.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDr. James T. Rudrik has accepted the permanent position as Director of the Division of Infectious Diseases effective March 24, 2014. He has more than 30 years of service in the laboratory testing field, both in private as well as public institutions. Please feel free to contact Dr. Rudrik regarding any issues related to infectious disease laboratory testing.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
39 views6 pagesMichigan Department of Community Health: LabLink Spring 2014
Uploaded by
Michigan NewsDr. James T. Rudrik has accepted the permanent position as Director of the Division of Infectious Diseases effective March 24, 2014. He has more than 30 years of service in the laboratory testing field, both in private as well as public institutions. Please feel free to contact Dr. Rudrik regarding any issues related to infectious disease laboratory testing.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
LabLink
Director of Infectious Diseases Division James T. Rudrik, Ph.D.
Dr. James T. Rudrik, former Manager of the Microbiology Section, has
accepted the permanent position as Director of the Division of Infectious
Diseases effective March 24, 2014.
Dr. Rudrik brings a wealth of knowledge and a vast amount of valuable
experience in the practice of laboratory medicine to this position. He has
more than 30 years of service in the laboratory testing field, both in
private as well as public institutions and he has been with the Michigan
Department of Community Health Bureau of Laboratories for the past 15
years.
Dr. Rudrik will continue to work collaboratively with clinical partners and
other state and federal agencies to ensure that we are providing the
highest quality of laboratory testing for our public health partners and
Michigan residents.
Please feel free to contact Dr. Rudrik regarding any issues related to
infectious disease laboratory testing. He can be reached at (517)335-
8067.
this issue
New Division Director P.1
Electronic Test Ordering and
ResultsP.2
New Section Manager P.2
New Antimicrobial Resistance
Microbiologist P.3
MALDI-TOF at MDCH P.3
Non-conforming Event P.4
Director,
Bureau of Laboratories
Sandip Shah, Ph.D.,
HCLD(ABB)
SPRI NG 2014
Vol. 19 No. 2
www.michigan.gov/mdchlab
and click Whats New?
The Michigan Department of Community Health Bureau of
Laboratories is pleased to announce the appointment of Janice
Matthews-Greer, Ph.D., D(ABMM), as the Virology
Section Manager in the Bureau of Laboratories.
Dr. Matthews-Greer comes to MDCH BOL from the
Louisiana State University Health Science Center at Shreveport
where she served as the Director of Diagnostic Virology for 10
years and held appointments as Professor of Research in
Pediatrics and Professor of Clinical Pathology. She is certified as a Diplomat of the American
Board of Medical Microbiology with a specialty in Medical Virology and Public Health and is
active in the American Society for Microbiology (ASM) serving as Council Representative At
Large, on the ASM Professional Affairs Committee, and as an ASM Branch Lectureship
Speaker. Dr. Matthews-Greer is also an accomplished researcher with over 36 articles in peer-
reviewed journals and 77 abstracts presented at local, national and international meetings.
Dr. Matthews-Greer started in her new position on April 28, 2014. She may be contacted on
issues related to virology at 517-335-8099.
New Virology Section Manager at the Bureau of Laboratories
More About ETOR
Additional tests are being added as they complete their pilot phases. As
new tests become available, the list of tests will be updated in the ETOR
manual. If you are interested in using ETOR for a test not listed
above, please contact us at LIMS_Help@michigan.gov (underscore
between LIMS and Help) and we can prioritize a pilot for that test.
Please note, at this time, ETOR is available only for specimens submit-
ted to the Lansing laboratory. However, C. trachomatis & N. gonor-
rhoeae Non-Culture tests may be ordered through ETOR for samples
submitted to the Lansing OR Saginaw laboratories.
Questions may be sent to LIMS_Help@michigan.gov (underscore be-
tween LIMS and Help).
MDCH Bureau of Laboratories
Web Portal for Electronic Test Ordering and Results Delivery
The Michigan Department of Community Health Bureau of Laboratories (MDCH BOL) instituted a web portal
for Electronic Test Ordering and Results (ETOR) Delivery at the start of 2014. ETOR is an alternate, voluntary
method for clients to order laboratory tests and receive test results. Participating clients are able to log into the
web portal and electronically fill out their test request forms; print a packing list to be submitted with the
sample to the MDCH BOL for testing; track their samples through the MDCH laboratory; and look up, down-
load or print pdf copies of final reports. Clients using the web portal no longer have to hand write or submit
test request forms. This information is collected in the web portal and imported into the BOL Laboratory
Information Management System (LIMS) upon arrival of the specimen. Clients have the option to continue
receiving final reports via fax or hard copy, as they do now. Web portal result delivery is also available to the
client. Upon request, any client may discontinue their fax or hard copy reporting system in favor of receiving
only web portal results. Access to the ETOR web portal is through a State of Michigan Single Sign On (SSO)
Account. Clients who currently have a SSO account will only need to request the ETOR application link.
Clients without SSO accounts will need to register for one. Complete instructions can be found in the ETOR
Manual (a link to this manual can be found at http://www.michigan.gov/mdchlab).
Current tests available to be ordered through ETOR are:
C. trachomatis & N. gonorrhoeae Non-Culture Measles IgG
C. trachomatis Non-Culture Measles IgM
Hepatitis A Antibody (IgM) Mumps IgG
Hepatitis B Antibody (Anti-HBsAg) Mumps IgM
Hepatitis B Surface Antigen (HBsAg) Rabies AB Serology
Hepatitis B Surface Antigen (HBsAg) Exposure Rubella IgG
Hepatitis C Antibody Rubella IgM
HIV AB - Oral Mucosal Transudate Student/Employee Immune Status Panel
HIV Ag/Ab - Serum Syphilis (USR)
Lead Filter Paper Trichomonas vaginalis Non-Culture (Fee-for-service only)
Lead Whole Blood Varicella Zoster IgG
AFB Identification - Isolate ID AFB Nucleic Acid Amplification
Fungal Identification - Isolate ID
The MDCH Bureau of Laboratories (BOL) is happy to announce
the appointment of Carrie Anglewicz as the Antimicrobial
Resistance Microbiologist in the Laboratory Systems Section.
Carrie has worked as a Senior Microbiologist in the Enterics/
STD/Chromatography Unit in the Microbiology Section at the
BOL where she primarily worked with food borne disease
organisms. Carrie has also served as adjunct faculty for Michigan
State Universitys Biomedical Laboratory Diagnostics Program training students in laboratory
methods during their clinical rotation at the BOL. In her new position, Carrie will serve as a
laboratory advisor on antimicrobial resistance issues. Carrie may be contacted via email at
AnglewiczC@michigan.gov or by phone at 517-335-9654.
Antimicrobial Resistance Microbiologist at the Bureau of Laboratories
MALDI-TOF mass spectrometry forms the basis of MALDI Biotyper analyses. A laser in the MALDI-TOF
mass spectrometer irradiates the matrix/sample mixture, evaporating the matrix and releasing positively
charged proteins in a so-called soft ionization process. The ability of the matrix to absorb UV light and
transfer protons onto the extracted proteins is crucial to this process. The protein ions are electrostatically
accelerated over a short distance and arrive in the flight tube at a speed that is proportional to their mass.
Protein ions with different masses arrive at the detector after different time periods. By simply measuring the
time between pulsed acceleration and the corresponding detector signal (in the nanosecond range), the speed
of the ions can be measured very precisely and converted into an accurate molecular mass. MALDI Biotyper
analysis generates a characteristic mass and intensity distribution of the mainly ribosomal proteins. Because
this mass spectrum is species-specific for a large number of microorganisms, it represents a 'molecular
fingerprint'. Unknown microorganisms can be identified by comparing their 'fingerprint' with the thousands
of patterns in the reference database.
Figure 1. The MALDI-TOF target plate has ninety-six spots that can be
inoculated using an applicator such as a toothpick. The spot is overlaid with the
matrix solution and after drying, it is loaded into the analyzer. The whole
process takes just minutes. A longer time may be necessary if an extra
extraction process is needed adding approximately an hour.
Often, the turnaround time for identification is within a day of receiving the isolate. Previously, using bio-
chemical testing and 16s sequencing it could take days or even a week or two for final identification.
Figure 2. Example of the spectral pattern
produced for Escherichia coli.
A spectral pattern is compared to the data-
base in the softwares library generating
identification. When an identification
cannot be obtained using our laboratory
algorithm the organism will be sequenced
and submitted for biochemical analysis.
The identification using MALDI-TOF has reduced the cost per test to less than a dollar compared to more
than forty dollars with previous methods. We will continue to expand the use of MALDI-TOF in other areas
of the laboratory in the near future.
MALDI-TOF at MDCH
The MALDI-TOF MS has recently been validated for use in the Bacteriology Unit at MDCH.
MALDI-TOF MS (matrix-assisted laser desorption/ionization time of flight mass spectrometry)
replaces the routine use of 16s sequencing and biochemical identification of microorganisms.
Currently, biochemical tests form the basis of most techniques used to identify microorganisms.
Organisms are added to media containing specific carbohydrates or substrates which lead, for
example, to a characteristic color change of the added reagent. This color change can be compared
with reference values. Correlating the results of a number of such tests on a sample culture provides
an indication of the organism's identity. The Bruker MALDI Biotyper uses a different methodology:
it identifies microorganisms by analyzing the expression of their intrinsic proteins using mass
spectrometry. This mass spectral pattern of protein expression is compared with reference patterns in a
database.
The starting material for a classification using the MALDI Biotyper is an individual colony from a
culture on an agar plate. The sample is transferred to a position on a MALDI target and air-dried. Af-
ter drying, a small quantity of matrix solution is added. The organic solvent in the matrix solution ex-
tracts proteins from the microorganisms; the extracted proteins are mainly ribosomal proteins, which
are present in high concentrations. Once the matrix has crystallized, sample preparation is complete
and the samples can be analyzed. If this straightforward sample preparation method is unsuccessful, a
supplementary protocol containing short chemical extraction steps can be used to increase the range of
organisms that can be identified by MALDI analysis.
The discovery of a non-conforming event following the completion of complement fixation (CF)
fungal antibody testing and subsequent root-cause analysis, resulted in a product recall and the im-
plementation of process improvements at the MDCH Bureau of Laboratories (BOL) Virology Sec-
tion and the manufacturer. Inconsistent Histoplasma yeast CF antibody test results detected during
paired analysis alerted the Virology staff of a potential reagent defect. All commercially obtained CF
controls were within acceptable limits and there was no indication of testing failure to explain these
unusual findings. Troubleshooting and root cause analysis were performed to determine the exact cause
of these discordant results and to implement any value added process improvements. Results of the
investigation convinced the manufacturer to recall the specific CF Histoplasma antigen lot number
from the market. The manufacturer implemented additional quality control measures to ensure con-
sistent lot to lot results and created custom packaging to reduce the amount of quality control testing
performed at the BOL.
A serum specimen from a 36 year old male patient, Patient A, drawn on 1/4/13, was received at BOL
for CF testing on 1/9/13. The BOL routinely checks for the existence of a previous specimen (acute)
on each patient. If an acute specimen had been tested at BOL within 8 weeks of the convalescent draw
date, the acute specimen is run in parallel with the current (convalescent) specimen to detect a four-
fold change in antibody titer. In this case, Patient A had an acute specimen drawn on 12/18/12 with a
reported Histoplasma yeast titer of 1:128. Therefore both acute and convalescent specimens were test-
ed in parallel on the same day for comparison. Unexpectedly, both the acute and convalescent speci-
mens tested negative for the presence of Histoplasma yeast antibody. The Histoplasma yeast antisera
(positive control) provided by the manufacturer was within acceptable limits indicating all reagents
were working properly. Since discrepant results were noted, repeat testing was initiated, patient speci-
mens were not reported, the supervisor was notified, and a full investigation ensued.
To determine causation both specimens were retested the next day using an unopened 5 ml vial of His-
toplasma CF antigen of the same lot and shipment date as the suspect lot. Surprisingly, both specimens
now tested positive and were within one dilution of the expected titer of 1:128, pointing to a
Non-conforming Event Leads to Product Recall and Process Improvements
Peggy Casey, BS, MT (ASCP)
Kristine Smith, BS, MT (ASCP)
problem with the particular vial of Histoplasma yeast antigen used the day before. All remaining 8 uno-
pened Histoplasma antigen vials of this suspect lot number were tested against both the vendor supplied
kit controls and two known positive (confirmed cases) patient sera (titers 1:64 and 1:256). The kit control,
which is an antibody produced in goats, gave the expected titer with all 8 vials. However, only a few of
the vials gave expected titers using the two previously tested patient sera. BOL then contacted the
manufacturer to alert them of the inconsistent antigen results and to seek resolution and reimbursement.
Cooperative discussions with the manufacturers technical staff followed by multiple specimen exchanges
along with new antigen lot number testing revealed improper mixing or dispensing of antigen into the 5
ml vials during the manufacturing process which led to these inconsistent results. Due to this discovery,
the defective lot number was pulled from the market to prevent future false negative Histoplasma yeast CF
antibody results. The manufacturer also instituted random testing of each new antigen lot number at the
final 5 ml dispense step and utilized known positive human sera for quality control testing to ensure
accurate, consistent antigen. Root cause analysis also revealed that an alteration in antigen packaging
volumes would represent a value added improvement to our testing process at BOL. Upon request, the
manufacturer agreed to package all future antigen shipments in custom 40 ml vials, as opposed to the
current 5 ml vials. This decreased the number of quality control analyses performed on new antigen lot
numbers from 20-30 to less than 3 per year. The acceptable CF positive control result is still unexplained.
The vendor theorized that the positive CF control contained non-specific goat antibodies against soluble
yeast antigens that are shed from yeast cells and are inadvertently used in the immunization process.
In summary, the detection of a non-conforming event, discordant Histoplasma yeast antibody results in an
acute serum specimen in comparison to results obtained during paired analysis, led to a valuable root
cause analysis. Since the defective antigen was discovered early on, there were no incorrect patient results
reported by the BOL. This unusual event led to multiple process improvements at the manufacturer and
the BOL. Due to custom antigen packaging, the amount of quality control testing required for each new
lot number of CF antigen has been greatly reduced. The manufacturer reimbursed the BOL for all
defective product and reagents used during the investigation.
As we have all heard by now, there have been two confirmed imported cases of Middle East
Respiratory Syndrome Coronavirus (MERS-CoV) in the United States.
The first Middle East Respiratory Syndrome Coronavirus (MERSCoV) case in the United States
was confirmed on Friday, May 2, 2014 in a traveler from Saudi Arabia to the U.S. The traveler has
since recovered and has been released from the hospital. Public health officials have contacted
healthcare workers, family members and travelers who had close contact with this patient. So far,
none of these contacts have exhibited any symptoms of infection with MERSCoV.
On May 11, 2014, the second imported case of MERSCoV was confirmed in a traveler who
came to the U.S. from Saudi Arabia. This patient is hospitalized and doing well. People who had
close contact with this second patient are currently being contacted. These two U.S. cases are not
linked.
So far, including this latest U.S. importation, there have been 698 confirmed cases of MERSCoV
infection with 285 deaths, 54 active cases and 359 recovered individuals in 14 countries. To date, all
reported cases have originated in six countries in the Arabian Peninsula. Most of these people
developed severe acute respiratory illness, with fever, cough and shortness of breath. There is no
available vaccine or specific treatment recommended for the virus.
MDCH Bureau of Laboratories is an approved state public health laboratory for MERS-CoV testing
using the CDC rRT-PCR assay. Contact your local health department or MDCH at 517-335-8165 to
seek approval to coordinate testing.
Authorization for testing can be obtained by contacting MDCH Communicable Disease Division
at: 5173358165 during normal business hours or 5173359030 after normal business hours.
To date, little is known about pathogenic potential and transmission dynamics of MERSCoV. To
increase the likelihood of detecting an infection, CDC recommends collecting multiple specimens
from different sites at different times after onset of symptoms, if possible. Lower respiratory tract
specimens should be a priority for collection and testing by PCR.
Middle East Respiratory Syndrome Coronavirus (MERS-CoV)
Bruce A. Robeson MT(ASCP)
Points to consider when determining which specimen types to collect from a patient
under investigation for MERS include:
1. The number of days between specimen collection and onset of symptoms
2. Symptoms at the time of specimen collection
Additional points to consider:
1. Maintain proper infection control measures when collecting specimens
2. Use approved collection methods and equipment when collecting specimens
3. Handle, store and ship specimens by following appropriate protocols
Lower respiratory specimens are preferred, but collecting nasopharyngeal and oropharyngeal (NP/OP)
specimens, as well as stool and serum, are strongly recommended depending upon the length of time
between onset of symptoms and specimen collection. For example, if symptom onset for a PUI (Patient
Under Investigation) with ongoing lower respiratory tract infection was 14 or more days ago, a single
serum specimen for serologic testing in addition to a lower respiratory specimen and an NP/OP
specimen are recommended.
Respiratory specimens should be collected as soon as possible after symptoms begin ideally within 7
days and before antiviral medications are administered. However, if more than a week has passed since
onset of symptoms and the patient is still symptomatic, respiratory samples should still be collected,
especially lower respiratory specimens since respiratory viruses can still be detected by rRT-PCR.
For short periods ( 72 hours), most specimens should be held at 2-8oC rather than frozen. For delays
potentially exceeding 72 hours, freeze specimens at -70oC as soon as possible after collection (with
exceptions as noted below). Label each specimen container with the patients ID number, specimen type
and the date the sample was collected.
Respiratory Specimens
A. Lower respiratory tract
Broncheoalveolar lavage, tracheal aspirate, pleural fluid
Collect 2-3 mL into a sterile, leak-proof, screw-cap sputum collection cup or sterile dry container.
Refrigerate specimen at 2-8oC up to 72 hours; if exceeding 72 hours, freeze at -70oC and ship on dry
ice.
Sputum
Have the patient rinse the mouth with water and then expectorate deep cough sputum directly into a sterile,
leak-proof, screw-cap sputum collection cup or sterile dry container. Refrigerate specimen at 2-8oC up to
72 hours; if exceeding 72 hours, freeze at -70oC and ship on dry ice. (Continued on next page)
Continued from previous page
B. Upper respiratory tract
Nasopharyngeal AND oropharyngeal swabs (NP/OP swabs)
Use only synthetic fiber swabs with plastic shafts. Do not use calcium alginate swabs or swabs
with wooden shafts, as they may contain substances that inactivate some viruses and inhibit PCR
testing.
Place swabs immediately into sterile tubes containing 2-3 ml of viral transport media. NP/OP
specimens can be combined, placing both swabs in the same vial. Refrigerate specimen at 2-8oC up
to 72 hours; if exceeding 72 hours, freeze at -70oC and ship on dry ice.
Nasopharyngeal wash/aspirate or nasal aspirates
Collect 2-3 mL into a sterile, leak-proof, screw-cap sputum collection cup or sterile dry container.
Refrigerate specimen at 2-8oC up to 72 hours; if exceeding 72 hours, freeze at -70oC and ship on dry
ice.
Serum (for rRT-PCR testing)
For rRT-PCR testing (i.e., detection of the virus and not antibodies), a single serum specimen
collected optimally during the first week after symptom onset, preferably within 3-4 days, after
symptom onset, may be also be beneficial.
Children and adults Collect 1 tube (5-10 mL) of whole blood in a serum separator tube. Allow the
blood to clot, centrifuge briefly, and separate sera into sterile tube container. The minimum amount of
serum required for testing is 200 L. Refrigerate the specimen at 2-8oC and ship on ice- pack;
freezing and shipment on dry ice is permissible.
Infants A minimum of 1 mL of whole blood is needed for testing of pediatric patients. If possible,
collect 1 mL in an EDTA tube and in a serum separator tube. If only 1 mL can be obtained, use a
serum separator tube.
EDTA blood (plasma)
Collect 1 tube (10 mL) of heparinized (green-top) or EDTA (purple-top) blood. Refrigerate specimen
at 2-8oC and ship on ice-pack; do not freeze.
Stool
Collect 2-5 grams of stool specimen (formed or liquid) in sterile, leak-proof, screw-cap sputum
collection cup or sterile dry container. Refrigerate specimen at 2-8oC up to 72 hours; if exceeding 72
hours, freeze at -70oC and ship on dry ice.
All specimens must be pre-packed to prevent breakage and spillage. Specimen containers should be
sealed with Parafilm and placed in ziplock bags.
LabLink is published quarterly by the Michigan Department of Community Health,
Bureau of Laboratories, to provide laboratory information to
Michigan health professionals and public health community.
MDCH is an Equal Opportunity Employer, Services and Programs
Provider DCH-0096
Save the Date
August 2, 2014
Explore Lab Science Fishing Event
More info will be available in July
www.michigan.gov/explorelabscience
Place enough absorbent material to absorb the entire contents of the Secondary Container (containing
Primary Container) and separate the Primary Containers (containing specimen) to prevent breakage. Send
specimens with cold packs or other refrigerant blocks that are self-contained, not actual wet ice. This prevents
leaking and the appearance of a spill. When large numbers of specimens are being shipped, they should be
organized in a sequential manner in boxes with separate compartments for each specimen.
Specimens should be stored and shipped at the temperatures indicated above. If samples are unable to be shipped
within 72 hours of collection, they should be stored at -70C and shipped on dry ice.
You might also like
- To Our Customers: DuMouchellesDocument1 pageTo Our Customers: DuMouchellesMichigan NewsNo ratings yet
- MPSC Fines DTE Energy $840,000 For Improper Billing, ShutoffsDocument2 pagesMPSC Fines DTE Energy $840,000 For Improper Billing, ShutoffsMichigan NewsNo ratings yet
- Shots FiredDocument2 pagesShots FiredMichigan NewsNo ratings yet
- ShootingsDocument4 pagesShootingsMichigan NewsNo ratings yet
- Detroit Pharmacy and Pharmacist Summarily Suspended For Over Dispensing Controlled SubstancesDocument1 pageDetroit Pharmacy and Pharmacist Summarily Suspended For Over Dispensing Controlled SubstancesMichigan NewsNo ratings yet
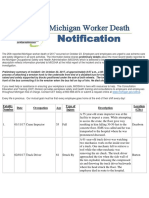
- The 25th Reported Michigan Worker Death of 2017 Occurred On October 23Document6 pagesThe 25th Reported Michigan Worker Death of 2017 Occurred On October 23Michigan NewsNo ratings yet
- Six Public Building Projects Honored For $2.1 Million in Annual Energy Savings Through Use of Performance ContractsDocument3 pagesSix Public Building Projects Honored For $2.1 Million in Annual Energy Savings Through Use of Performance ContractsMichigan NewsNo ratings yet
- Liposuction Doctor Suspended For Health Code ViolationsDocument1 pageLiposuction Doctor Suspended For Health Code ViolationsMichigan NewsNo ratings yet
- Schuette West Bloomfield Doctor Plead No Contest To Larceny ChargesDocument2 pagesSchuette West Bloomfield Doctor Plead No Contest To Larceny ChargesMichigan NewsNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Baby Checklist: Room Furniture Baby Wear Baby BeddingDocument2 pagesBaby Checklist: Room Furniture Baby Wear Baby BeddingLawrence ConananNo ratings yet
- Speaking With Confidence: Chapter Objectives: Chapter OutlineDocument12 pagesSpeaking With Confidence: Chapter Objectives: Chapter OutlinehassanNo ratings yet
- Scientific Method - AssessmentDocument13 pagesScientific Method - AssessmentA.BensonNo ratings yet
- A. Questions: Conversation Activities - TravelDocument11 pagesA. Questions: Conversation Activities - TravelkicsirekaNo ratings yet
- ENDOCRINE-BOARD REVIEW Dr. SchearDocument57 pagesENDOCRINE-BOARD REVIEW Dr. SchearNayara PataroNo ratings yet
- SWOT Analysis Textile IndustryDocument23 pagesSWOT Analysis Textile Industrydumitrescu viorelNo ratings yet
- Class VII Half Yearly Maths, M.junaidDocument4 pagesClass VII Half Yearly Maths, M.junaidmohd junaidNo ratings yet
- Questions-1D and 2D Flow: Depth To WaterDocument4 pagesQuestions-1D and 2D Flow: Depth To WaterJoseph ChangNo ratings yet
- Features and Highlights - : CapableDocument2 pagesFeatures and Highlights - : CapableaarianNo ratings yet
- Table of Content and PrefaceDocument5 pagesTable of Content and PrefaceHaiderEbrahimNo ratings yet
- Making Fertilizer Using Ipil Ipil LeavesDocument10 pagesMaking Fertilizer Using Ipil Ipil LeavesRaine TalionNo ratings yet
- Derivation of Gravity Loads PDFDocument4 pagesDerivation of Gravity Loads PDFHenry TuganoNo ratings yet
- Jamir, Dewan R. EMGT Field Project Part 1Document116 pagesJamir, Dewan R. EMGT Field Project Part 1fucker66No ratings yet
- Principles of ForecastingDocument41 pagesPrinciples of Forecastingrajeevseth100% (1)
- Buongiorno - Etal - 2009 The Big Experimental CheckDocument15 pagesBuongiorno - Etal - 2009 The Big Experimental CheckMikhail TarabrinNo ratings yet
- Selulitis Orbita Pada Laki-Laki Usia 64 Tahun: Laporan KasusDocument8 pagesSelulitis Orbita Pada Laki-Laki Usia 64 Tahun: Laporan KasusLuh Dita YuliandinaNo ratings yet
- Astm D6321-98-2004Document3 pagesAstm D6321-98-2004Thyagu LingamurthyNo ratings yet
- Class 12 Psychology PDFDocument209 pagesClass 12 Psychology PDFSoumyashis Bhattacharya0% (1)
- SG5.0 20RT UEN Ver13 202101Document105 pagesSG5.0 20RT UEN Ver13 202101Asep SaepudinNo ratings yet
- Ebp Cedera Kepala - The Effect of Giving Oxygenation With Simple Oxygen Mask andDocument6 pagesEbp Cedera Kepala - The Effect of Giving Oxygenation With Simple Oxygen Mask andNindy kusuma wardaniNo ratings yet
- "Automatic Tyre Pressure Inflation System": Bachelor of TechnologyDocument41 pages"Automatic Tyre Pressure Inflation System": Bachelor of Technologymd washiqeNo ratings yet
- Module I: Introduction To Environmental PollutionDocument14 pagesModule I: Introduction To Environmental PollutionAman John TuduNo ratings yet
- Kantha Embroidery by Nanduri Asha, Shreya Gulati, Saloni PriyaDocument17 pagesKantha Embroidery by Nanduri Asha, Shreya Gulati, Saloni PriyaShreyaa Gulati100% (3)
- HP Compaq 6531s Inventec Zzi MV Rev A03 (6820s)Document54 pagesHP Compaq 6531s Inventec Zzi MV Rev A03 (6820s)y2k_yah7758No ratings yet
- A554-15 Standard Specification For Welded Stainless Steel Mechanical TubingDocument8 pagesA554-15 Standard Specification For Welded Stainless Steel Mechanical TubingChuthaNo ratings yet
- Homework 3rd SteelDocument4 pagesHomework 3rd SteelPiseth HengNo ratings yet
- Designing New Vanillin Schiff Bases and Their Antibacterial StudiesDocument4 pagesDesigning New Vanillin Schiff Bases and Their Antibacterial StudiesAvinash PurohitNo ratings yet
- List BRG TGL 12Document49 pagesList BRG TGL 12Rizal MuhammarNo ratings yet
- 00capítulo - The Routledge Handbook of Henri Lefebvre, The City and Urban SocietyDocument12 pages00capítulo - The Routledge Handbook of Henri Lefebvre, The City and Urban SocietyJeronimoNo ratings yet
- Introducing RS: A New 3D Program For Geotechnical AnalysisDocument4 pagesIntroducing RS: A New 3D Program For Geotechnical AnalysisAriel BustamanteNo ratings yet