Professional Documents
Culture Documents
Khih
Uploaded by
Abdur Rachman Ba'abdullah0 ratings0% found this document useful (0 votes)
18 views3 pagesOlanzapine and perphenazine were superior with respect to the rate of discontinuation of treatment. But quetiapine and ziprasidone were given in doses that were rather low. 40 percent of all patients discontinued as a result of their own decision.
Original Description:
Original Title
khih
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentOlanzapine and perphenazine were superior with respect to the rate of discontinuation of treatment. But quetiapine and ziprasidone were given in doses that were rather low. 40 percent of all patients discontinued as a result of their own decision.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
18 views3 pagesKhih
Uploaded by
Abdur Rachman Ba'abdullahOlanzapine and perphenazine were superior with respect to the rate of discontinuation of treatment. But quetiapine and ziprasidone were given in doses that were rather low. 40 percent of all patients discontinued as a result of their own decision.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
n engl j med 354;3 www.nejm.
org january 19, 2006 298
The new england j ournal of medi ci ne
correspondence
Antipsychotic Drugs and Schizophrenia
to the editor: The report by Lieberman and
colleagues (Sept. 22 issue)
1
on the Clinical Antipsy-
chotic Trials of Intervention Effectiveness (CATIE),
funded by the National Institute of Mental Health,
raises some questions that require clarification.
One can see from the results that olanzapine and
perphenazine, which were superior with respect
to the rate of discontinuation of treatment, were
given in rather high doses, as compared with the
doses used in an observational study.
2
In contrast,
the antipsychotic drugs that were discontinued
mainly because of a lack of efficacy, quetiapine
and ziprasidone, were given in doses that were
rather low (for people with schizophrenia). One
has to wonder why the doses of quetiapine or
ziprasidone were not increased when their inef-
ficacy became clear.
The study also indicates that 40 percent of all
patients discontinued as a result of their own deci-
sion. The study does not explicitly mention the
reasons for their decisions, but one can assume
that a lack of objective insight into the disorder,
subjective social attitudes toward schizophrenia,
and the social and financial backgrounds of the
patients contributed. If this was the case, further
studies that assess the power of education about
psychotic disease and social psychiatric options
are certainly indicated.
Michael Dettling, M.D.
Ion-George Anghelescu, M.D.
CharitUniversity Medicine Berlin
10961 Berlin, Germany
michael.dettling@charite.de
Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of
antipsychotic drugs in patients with chronic schizophrenia.
N Engl J Med 2005;353:1209-23.
Dossenbach M, Arango-Davila C, Silva Ibarra H, et al. Re-
sponse and relapse in patients with schizophrenia treated with
olanzapine, risperidone, quetiapine, or haloperidol: 12-month
follow-up of the International Schizophrenia Outpatient Health
Outcome (IC-SOHO) study. J Clin Psychiatry 2005;66:1021-30.
to the editor: The CATIE study of the effective-
ness of antipsychotic drugs should be subjected
to two additional analyses. First, the proportions
of patients randomly assigned to continue taking
the antipsychotic agents that they were taking at
baseline varied markedly among the treatment
groups (e.g., 23 percent of those assigned to re-
ceive olanzapine were already taking olanza-
pine, whereas only 5 percent of those assigned
to quetiapine were already taking quetiapine).
The authors should report the extent to which such
patients fared worse (or better) with respect to
particular outcomes. Patients taking olanzapine
before enrollment continued the study medica-
tion longer (whether continuing to take olanza-
pine or changing medications); because the analy-
sis combined patients staying on the medication
they were receiving at baseline with those who
changed medications, it remains unclear to what
extent the larger proportion of patients in the
olanzapine group who did not change medica-
tion at entry into the study contributed to the fa-
vorable continuation outcomes for olanzapine.
Second, a sensitivity analysis excluding data
1.
2.
this weeks letters
298 Antipsychotic Drugs and Schizophrenia
300 Vasodilators in Aortic Regurgitation
303 Childhood Growth and Coronary Events
304 Asbestos Exposure and Serum Osteopontin
305 Malignant Mesothelioma
307 Immunologic Tolerance to Intravenously
Injected Insulin
The New England Journal of Medicine
Downloaded from nejm.org on January 5, 2011. For personal use only. No other uses without permission.
Copyright 2006 Massachusetts Medical Society. All rights reserved.
correspondence
n engl j med 354;3 www.nejm.org january 19, 2006 299
on any patient with tardive dyskinesia would
help in an examination of whether, as previously
shown,
1
those with this condition did less well
than those without the condition. If so, the exclu-
sion of patients with tardive dyskinesia from the
perphenazine group might account for the drugs
relatively good performance.
Susan M. Essock, Ph.D.
Mount Sinai School of Medicine
New York, NY 10029
susan.essock@mssm.edu
Nancy H. Covell, Ph.D.
Carlos T. Jackson, Ph.D.
University of Connecticut
Storrs, CT 06269
Jackson CT, Covell NH, Essock SM. Differential effectiveness
of clozapine for patients nonresponsive to or intolerant of first
generation antipsychotic medications. Schizophr Bull 2004;30:
219-27.
To the Editor: The implications of CATIE for
cost-effectiveness, although not a direct focus of
the study, are important for countries other than
the United States, especially developing countries,
where the financial burden of taking medications
rests predominantly on the patient and the fam-
ily, rather than on the health care provider. For
example, in India, drug therapy may account for
nearly 20 percent of a patients monthly income.
1
Atypical antipsychotic agents are far more expen-
sive in such countries. Olanzapine is 8.7 and 6.8
times more expensive than perphenazine in the
United States and the United Kingdom, respec-
tively, and risperidone is 4.1 and 2.1 times more
expensive.
2,3
Would patients in developing coun-
tries prefer more expensive, effective atypical drugs
that are associated with metabolic syndromes
or inexpensive but nearly equally effective typi-
cal drugs that are associated with extrapyrami-
dal symptoms? Would health care policymakers
advocate more frequent use of clinically effective
atypical agents or cost-effective typical agents? Is
the evidence from the CATIE study solid enough
to translate the results to developing countries or
even to other developed countries? Clinicians and
policymakers still need more data.
Nitin Gupta, M.D.
South Staffordshire Healthcare NHS Trust
Burton upon Trent DE13 0RB, United Kingdom
nitingupta659@yahoo.co.in
Debasish Basu, M.D.
Mersey Care NHS Trust
Southport PR9 0LT, United Kingdom
1.
Dr. Gupta reports having received honoraria and lecture fees
from AstraZeneca and education-related fees from Eli Lilly, Janssen,
and AstraZeneca.
Grover S, Avasthi A, Chakrabarti S, Bhansali A, Kulhara P.
Cost of care of schizophrenia: a study of Indian out-patient at-
tenders. Acta Psychiatr Scand 2005;112:54-63.
Charatan F. New antipsychotics offer few benefits over tra-
ditional drugs. BMJ 2005;7519:717.
British National Formulary. London: British Medical Asso-
ciation and The Royal Pharmaceutical Society of Great Britain,
2005.
To the Editor: The report by Lieberman et al.
raises certain methodologic and statistical issues.
It appears that no consideration is given to site-
by-treatment interactions, an important issue for
multicenter trials.
1
Fully successful blinding seems
unlikely to be achieved, given the multiple dosing
regimens used in CATIE. The efficacy analyses
(Fig. 2E and 2F of the article by Lieberman et al.)
are compromised by the huge discontinuation
rates; the mixed-effects models used in the analy-
ses do not solve this problem. Successful treat-
ment time appears to combine discrete time seg-
ments and thus this variable is not suitable for
KaplanMeier and proportional-hazards regres-
sion analyses. Several outcome measures are con-
founded with the duration of treatment, notably
the rates of substantial weight gain referred to in
the editorial by Freedman
2
: Thirty percent of the
patients receiving olanzapine gained more than
7 percent of their body weight during the trials,
as compared with 7 to 16 percent of those receiv-
ing the other drugs. Patients taking olanzapine
had more time in phase 1 of the study to show
weight gain. Given the major clinical and public
health implications of CATIE, we believe that the
authors should comment on these and other meth-
odologic issues.
Naihua Duan, Ph.D.
Geffen School of Medicine at UCLA
Los Angeles, CA 90024
Helena C. Kraemer, Ph.D.
Stanford University School of Medicine
Palo Alto, CA 94305
Jim Mintz, Ph.D.
Geffen School of Medicine at UCLA
Los Angeles, CA 90024
jmintz@ucla.edu
Dr. Duan reports having received research funding from Pfizer;
Dr. Mintz, research funding from Eli Lilly and consulting fees
from Janssen and Otsuka America; and Dr. Kraemer, consulting
fees from Eli Lilly.
Kraemer HC, Robinson TN. Are certain multicenter ran-
domized clinical trial structures misleading clinical and policy
decisions? Contemp Clin Trials 2005;26:518-29.
1.
2.
3.
1.
The New England Journal of Medicine
Downloaded from nejm.org on January 5, 2011. For personal use only. No other uses without permission.
Copyright 2006 Massachusetts Medical Society. All rights reserved.
The new england j ournal of medi ci ne
n engl j med 354;3 www.nejm.org january 19, 2006 300
Freedman R. The choice of antipsychotic drugs for schizo-
phrenia. N Engl J Med 2005;353:1286-8.
the authors reply: With regard to the com-
ments of Drs. Dettling and Anghelescu, the dose
of perphenazine was relatively low (not high) in
its therapeutic range. The dose was chosen inten-
tionally to reduce the risk of extrapyramidal symp-
toms. There was evidence that doses of quetia-
pine and ziprasidone were increased relative to
those of the other drugs. Relatively high doses of
olanzapine presumably would affect its tolerabil-
ity as well as its efficacy. Suggestions that the med-
ications used would have performed differently
at other doses are conjectures.
Dr. Duan and colleagues raise issues worth
clarification. We found no site-by-treatment in-
teractions that indicated that treatment should
be discontinued for any cause. The study design
a hybrid of paradigms of double-blinded ef-
ficacy and effectiveness did make maintenance
of blinding challenging. However, an evaluation
with the use of the blinding index described by
Bang et al.
1
showed that neither clinicians nor
patients correctly guessed the treatment assign-
ments more often than would be expected by
chance. We thought that mixed-effects models
were the most appropriate option to use to exam-
ine efficacy measures. As expected, last-observa-
tion-carried-forward analyses favored the drug
with the longest treatment duration, whereas ob-
served-cases analyses diminished the differences
among patients who stayed on the assigned drugs
for long durations. The duration of successful
treatment is an outcome intended to integrate our
primary outcome, the time spent taking a drug,
with data on efficacy. We agree that the combi-
nation of disjoint time segments in this measure
can complicate the interpretation of the results,
but survival methods are suitable, in that the
amount of time is a component of the total time
to the discontinuation of treatment. Statistical
testing of safety outcomes, including weight gain,
were adjusted for time receiving treatment.
2.
Dr. Essock and colleagues raise an important
question with regard to the effects of staying on
a medicine taken previously or starting a new
one. Patients assigned to olanzapine or risperi-
done who stayed on their baseline medication
remained in phase 1 longer than other patients
in the treatment groups (hazard ratio, 0.69;
P = 0.007). However, this does not account for the
study results, since the results of a sensitivity
analysis excluding all the patients included in
the intention-to-treat analysis who were as-
signed to their baseline medication (15 percent
of the total) were similar to those of the primary
analysis; the overall test of the comparison of the
treatments, however, was not significant (P = 0.086).
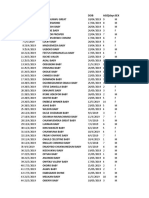
Discontinuation rates for the drugs were as fol-
lows: olanzapine, 68 percent; quetiapine, 82 per-
cent; risperidone, 76 percent; perphenazine, 75
percent; and ziprasidone, 80 percent. All compari-
sons of treatment discontinuation and efficacy
that involved perphenazine excluded patients with
tardive dyskinesia at baseline, so that the patients
taking perphenazine were compared with simi-
lar patients without tardive dyskinesia who were
assigned to the atypical comparator drugs.
We agree with Drs. Gupta and Basu that policy-
makers will need data on cost-effectiveness and
additional measures of clinical outcome to de-
termine the policy implications and relevance to
other countries.
Jeffrey A. Lieberman, M.D.
Columbia University College of Physicians and Surgeons
New York, NY 10032
jlieberman@columbia.edu
T. Scott Stroup, M.D., M.P.H.
University of North Carolina School of Medicine
Chapel Hill, NC 27599
Sonia M. Davis, Dr.P.H.
Quintiles
Research Triangle Park, NC 27709
for the CATIE Investigator Group
Bang H, Ni L, Davis CE. Assessment of blinding in clinical
trials. Control Clin Trials 2004;25:143-56.
1.
Vasodilators in Aortic Regurgitation
to the editor: In the study by Evangelista et al.
regarding long-term vasodilator therapy in pa-
tients with severe aortic regurgitation (Sept. 29 is-
sue),
1
both nifedipine and enalapril failed to in-
duce adequate vasodilation, because systolic blood
pressure and diastolic blood pressure did not
The New England Journal of Medicine
Downloaded from nejm.org on January 5, 2011. For personal use only. No other uses without permission.
Copyright 2006 Massachusetts Medical Society. All rights reserved.
You might also like
- High Altitude HypoxiaDocument4 pagesHigh Altitude HypoxiaAbdur Rachman Ba'abdullahNo ratings yet
- Adult Cutaneous Fungal Infections 1 DermatophytesDocument61 pagesAdult Cutaneous Fungal Infections 1 DermatophytesAbdur Rachman Ba'abdullahNo ratings yet
- Main Article - BM PancytopeniaDocument10 pagesMain Article - BM PancytopeniaAbdur Rachman Ba'abdullahNo ratings yet
- Ireland Vaccination Guideline For GP 2018Document56 pagesIreland Vaccination Guideline For GP 2018Abdur Rachman Ba'abdullahNo ratings yet
- Pulmonary AbscessDocument5 pagesPulmonary AbscessAbdur Rachman Ba'abdullahNo ratings yet
- Postgrad Med J 2004 Mathew 196 200Document6 pagesPostgrad Med J 2004 Mathew 196 200Abdur Rachman Ba'abdullahNo ratings yet
- Capillary Cavernous Hemangioma of Lymph Node: Pagni Fabio, MD and Dibella Camillo, MDDocument2 pagesCapillary Cavernous Hemangioma of Lymph Node: Pagni Fabio, MD and Dibella Camillo, MDAbdur Rachman Ba'abdullahNo ratings yet
- A Crazy Cause of DyspneaDocument6 pagesA Crazy Cause of DyspneaAbdur Rachman Ba'abdullahNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Article 1525968342 PDFDocument10 pagesArticle 1525968342 PDFanindhitha thandapaniNo ratings yet
- DermatomycosesDocument2 pagesDermatomycosesRay CullenNo ratings yet
- 35 DMDocument35 pages35 DMOmie TumanguilNo ratings yet
- Cesarean SectionDocument16 pagesCesarean Sectionjannnjennn67% (3)
- case study حنانDocument35 pagescase study حنانMera Abo ElhassanNo ratings yet
- Aditya MotwaneDocument3 pagesAditya Motwaneapi-257938623No ratings yet
- Sekhmet Reiki Book - ManualDocument234 pagesSekhmet Reiki Book - ManualZina Rozenblit100% (4)
- Evaluation of Applicability of Moyers' Mixed Dentition Analysis For Central India PopulationDocument6 pagesEvaluation of Applicability of Moyers' Mixed Dentition Analysis For Central India PopulationAniket PotnisNo ratings yet
- Zone Reiki Level 1Document14 pagesZone Reiki Level 1Tineke100% (9)
- Antifungal DrugsDocument28 pagesAntifungal DrugsKhairunnisa RasyidinNo ratings yet
- Aluminum and Foam Sam Splint 2004+Document3 pagesAluminum and Foam Sam Splint 2004+Ophelia PoppyNo ratings yet
- Leggett Announces County Suit Against 14 Opioid CompaniesDocument163 pagesLeggett Announces County Suit Against 14 Opioid CompaniesPublic Information OfficeNo ratings yet
- Glucose Metformin Thiazolidinedione Pioglitazone Rosiglitazone GlucoseDocument2 pagesGlucose Metformin Thiazolidinedione Pioglitazone Rosiglitazone GlucoseDarshan MoreNo ratings yet
- Health ICT Master PlanDocument6 pagesHealth ICT Master Planaboix253No ratings yet
- Fracture ReportDocument19 pagesFracture Reporteros_mimiNo ratings yet
- Merger Value CreationDocument11 pagesMerger Value CreationAziz BouignaneNo ratings yet
- Traditional Healing PracticesDocument2 pagesTraditional Healing Practicesjeon arcadiaNo ratings yet
- Guillain-Barre Syndrome Student HandoutDocument2 pagesGuillain-Barre Syndrome Student HandoutMiss LindiweNo ratings yet
- Analytical Method ValidationDocument86 pagesAnalytical Method ValidationRambabu komati - QA100% (12)
- Pereneal CareDocument2 pagesPereneal CareindumathiNo ratings yet
- Lauren L. Williamson: EducationDocument5 pagesLauren L. Williamson: Educationlauren_leshen_williamsonNo ratings yet
- Apollo Case Study StrategyDocument16 pagesApollo Case Study StrategyKundan KumarNo ratings yet
- Hosseinzadeh Et Al. 2008 - Anxiolytic and Hypnotic Effect of Crocus SativusDocument7 pagesHosseinzadeh Et Al. 2008 - Anxiolytic and Hypnotic Effect of Crocus SativusLaura DecockNo ratings yet
- Ebook Hazzards Geriatric Medicine and Gerontology 8Th Ed PDF Full Chapter PDFDocument67 pagesEbook Hazzards Geriatric Medicine and Gerontology 8Th Ed PDF Full Chapter PDFnancy.stice552100% (26)
- Bacterial Fungal Parasitic Overgrowth PDFDocument104 pagesBacterial Fungal Parasitic Overgrowth PDFportosinNo ratings yet
- Spinal Trauma, Imaging, Diagnosis and Management PDFDocument1 pageSpinal Trauma, Imaging, Diagnosis and Management PDFskeithNo ratings yet
- Geriatric AssessmentDocument27 pagesGeriatric AssessmentNeil Philip MaturanNo ratings yet
- Module 1-Introduction To Health Technology AssessmentDocument3 pagesModule 1-Introduction To Health Technology AssessmentLou Calderon100% (1)
- Umuagu Nnu DataDocument60 pagesUmuagu Nnu DataJemilehin AbiodunNo ratings yet