Professional Documents
Culture Documents
Nursing Annotated Bibliography
Uploaded by
Assignment Help Australia100%(1)100% found this document useful (1 vote)
524 views7 pagesAnnotated Bibliography Assignment help sample for Nursing. Get help with annotated bibliography homework from our highly experienced experts.
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAnnotated Bibliography Assignment help sample for Nursing. Get help with annotated bibliography homework from our highly experienced experts.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
100%(1)100% found this document useful (1 vote)
524 views7 pagesNursing Annotated Bibliography
Uploaded by
Assignment Help AustraliaAnnotated Bibliography Assignment help sample for Nursing. Get help with annotated bibliography homework from our highly experienced experts.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 7
Annotated Bibliography
[Type the document subtitle]
[Pick the date]
Akanji, AO., Ohaeri, JU. (2011). Metabolic syndrome in severe mental disorders.
Metabolic Syndrome in severe mental disorders, 9(2), 91-96
Main aim of this article is to determine if there is a relationship between metabolic syndrome
and severe mental disorders. The scope of this study extends beyond the previously
conducted studies which focused solely on schizophrenia. Other illnesses such as bipolar
disorder, generalised anxiety disorder and severe depression have been included in the study.
Authors in the article mainly argue that psychotropic drugs which are utilised to treat a
variety of mental disorders are known to adversely affect metabolism in individuals also
causing weight gain.
The article is directly related to the chosen research topic as metabolic syndrome is
commonly diagnosed in individuals suffering from mental disorders. The manner in which
mental illness in an individual correlates with and causes metabolic syndrome has been
explained in the article. Intended audience of this article consists of the general population
who might not be aware of the fact that people suffering from mental illness are also at a
much higher risk of facing metabolism related conditions.
Authors of this article reviewed historical literature available on the subject from Medline
and stated their findings. Since the study lacks a practical experiment base, no tables or
figures were available in the study.
A major strength of this article is that it seeks to bring together a vast variety of research
regarding the co-existence of mental illness and various metabolic conditions. A major
weakness on the other hand consists of the fact that most literature sources consulted are
single experiments whose results have not been duplicated till date.
The article concluded by suggesting that individuals faced with a severe mental disorder are
at least at two to three times higher risk of developing a metabolic syndrome as compared
with normal individuals. This article aids our understanding of the research topic as it drives
attention to the fact that additional attention needs to be paid towards people suffering from
mental health disorders as their mental condition might lead to several co-morbidities that can
also be a serious threat to their quality of life.
Barua, A., Basilio, M., Ghosh, M., Kar, N. (2012). Chronic Co-morbidities associated
with depression in elderly. Annals of Tropical Medicine and Public Health, 5(2), 145-149
Main objective of the article is to study the chronic co-morbid conditions which tend to exit
along with depression in elderly individuals. Scope of the article is limited to examining co-
morbidities in elderly individuals and depression. This might be attributed to the fact that
depression is among the most common mental health disorders in the world. Authors in this
article mainly argue that elderly individuals throughout the world tend to develop depressive
symptoms owing to a variety of factors. Depression in turn serves to interfere with normal
physical functioning of an individual thereby causing physical co-morbidities.
The article is directly related to the topic as it serves to enlighten the researcher about a
diverse range of physical co-morbidities which might be faced by elderly individuals with a
mental condition. This article is intended at the general population and might help in taking
better care of elderly individuals faced with depression.
A retrospective study based on systematic review of prevalence of depression in the elderly
population was carried out. Mental health surveys in a community health setting were carried
out in different continents such as Australia, Europe, Asia, North and South America and
studies published between 1955 and 2005 were considered. No tables or special aids were
provided in the article.
Biggest strength of this article is that it draws from a large body of evidence which spans
globally. A weakness on the other hand might be noticed in the fact that some articles were
drawn from unreliable sources such as Google and Yahoo searches and not from academic
databases.
The article concluded by suggesting that elderly individuals who are faced with depression
are at a much higher risk for developing chronic co-morbid conditions such as arthritis, visual
impairment, cognitive impairment, and ADL.
Holahan, CJ., Pahl, SA., Cronkite, RC., Holahan, CK, North, RJ, Moos, RH. (2010).
Depression and Vulnerability to incident physical illness across 10 years. J ournal of
Affective Disorders, 123(1-3), 222-229
Main aim of this article is to examine the role of depression in onset of physical illness in
individuals. The scope of this study like its predecessors in the area was not limited to any
specific physical illness but included the topic of physical illness in general. Authors of this
article have based this study on the argument that establishing a firm relationship between
depression and a wide spectrum of physical illness is necessary and central to improving
quality of life of depressed individuals and reducing burden of illness on the society.
Text of this study relates completely and directly to the chosen topic of determining major
co-morbidities that people diagnosed with a mental illness are at a higher risk of. The text
expands on a wide spectrum of physical illness and specifies a range of physical co-
morbidities that might generally be acquired by depressed patients. A few specific physical
co-morbidities which are widely discussed to exist along with depression have also been
referred to in the literature. The article seeks to address medical practitioners and primary
care givers who would be able to utilise this study in order to improve quality of life of
depressed individuals.
The study was conducted by following 388 clinically depressed patients over a period of 10
years. Data consisting of health behaviour, medical conditions as diagnosed by physicians
and socio-demographic factors were recorded in a self reported questionnaire at baseline, 1, 4
and 10 years during the period of follow up. Tables were immensely helpful as they clearly
demonstrated the relationship between depression and probability of acquiring physical co-
morbidities.
A major strength of the article is that it draws from a wide variety of research on the topic
and has a broad scope. A major limitation on the other hand consists of the fact that patients
might report several physical conditions as a result of their depression as opposed to their
actual presence.
The article concluded by suggesting that there is a strong co-relation between depression and
existence of chronic physical illness. This article aids our understanding of the topic as it
broadens awareness of the fact that depression is not merely a mental illness but affects
physical wellness as well.
Scott, D., Burke, K., Williams, S., Happell, B., Canoy, D., Ronan, K. (2012). Increased
prevalence of chronic physical health disorders in Australians with diagnosed mental
illness. Australian and New Zealand J ournal of Public Health, 36(5), 483-486
Main aim of this article is to compare the prevalence of chronic physical health disorders in
Australians faced with mental illness and general population. Scope of this study seeks to
include a wide variety of physical health disorders such as abnormal weight gain, pain in
joints and metabolic syndrome. Authors in this article mainly argue that various mental health
conditions and treatments that patients are required to undertake tend to adversely affect
physical health causing metabolic dysfunctions and weight gain.
Like others, this article directly addresses the research topic. An experimental approach has
been adopted to explain common co-morbidities that exist with mental health disorders. The
article intends to address health professionals and tends to alert them towards the coexistence
of chronic physical co-morbidities in individuals faced with mental health conditions.
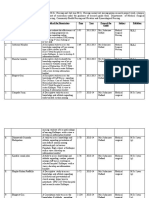
An online participant survey was conducted with a total of 1716 Australian individuals. 58%
of these participants were females. Self reported body mass index and chronic physical
conditions were utilised as outcome measures of the study. Tables presented in the article
aided understanding as they served to provide clarity. They listed participant demographics
along with the nature of their physical and mental conditions.
A major strength of the article is that it provides experimental evidence to the existence of
chronic physical co-morbidities along with mental health conditions. A major weakness
however might be seen from the fact that self reported physical conditions might be a result
of participant perception.
The article concluded by suggesting that Australian adults faced with mental conditions are at
a much higher risk of developing chronic physical conditions as compared to their
counterparts without any mental illness. The article aids our understanding of the topic as it
serves to provide further clarity and evidence to the fact that co-morbidities exist with mental
illness.
Sowden, GL., Huffman, JC. (2009). The impact of mental illness on cardiac outcomes: A
review for the cardiologist. I nternational J ournal of Cardiology, 132(1), 30-37
Main aim of this article is to determine the impact of mental health on cardiac outputs of
individuals. Scope of this study included examination of mental health conditions such as
depression, bipolar disorder, anxiety and schizophrenia along with their pathophysiological
progression, treatment and impact on cardiac outputs. Authors in the article mainly argue that
mental health conditions as identified above are significant cardiac risk factors and patients
identified with these conditions face a significantly higher risk of cardiac morbidity and
mortality as compared to their counterparts in the general population.
The article bears a direct correlation with the research topic as cardiac conditions have often
been determined to co-morbidly exist with mental health conditions. The manner in which
mental health conditions impact and increase the risk of cardiac malfunctioning has also been
highlighted in the article. The article has been designed to address cardiologists who would
be able to follow pathophysiological progression of these conditions along with treatments
offered and their relationship with cardiac outputs. This would enable them to offer better
care to their patients.
This study was conducted with the help of extensive research in Medline and PsycInfo and
locating relevant articles. Owing to lack of practical experimental base of the article, there are
no tables, figures or any other special aids which might aid understanding.
A major strength of this article is that serves to spread awareness about the link between
cardiac outputs and mental health of an individual. A major limitation of the article might be
seen in that it does not serve to outline any intervention which might be helpful in improving
cardiac outputs in mental health patients.
The article concluded by suggesting that mental health conditions such as depression,
anxiety, bipolar disorder and schizophrenia are high risk factors for cardiac mortality and
morbidity. This article aids our understanding of the topic as it introduces us to another
domain of co-morbidities that exists with mental illness.
APPENDIX
You might also like
- Behavioral Checklist PDFDocument7 pagesBehavioral Checklist PDFMartin Castañeda Salas100% (1)
- Rating Scales in SchizophreniaDocument87 pagesRating Scales in Schizophreniadrkadiyala2No ratings yet
- Abnormal Psychology Testbanks 2.1Document14 pagesAbnormal Psychology Testbanks 2.1Mark Jayson Jueves100% (1)
- The Stigma of Mental IllnessDocument15 pagesThe Stigma of Mental IllnessJulie HechanovaNo ratings yet
- MSC Nursing QuestionsDocument21 pagesMSC Nursing QuestionsRohini Kumar100% (1)
- Abilash Gopal, Alexander Ropper, III, Louis Tramontozzi Deja Review Psychiatry 2007Document242 pagesAbilash Gopal, Alexander Ropper, III, Louis Tramontozzi Deja Review Psychiatry 2007fuglicia100% (2)
- Generic Summary of The Professional Change Process Clinical ThinkingDocument17 pagesGeneric Summary of The Professional Change Process Clinical ThinkingNurul Fatin HusnaNo ratings yet
- Brochure RevisedDocument2 pagesBrochure Revisedapi-434089240No ratings yet
- Nursing Care PlanDocument9 pagesNursing Care PlanBishwajitMazumderNo ratings yet
- Research Critique: Subject: Research Speciality - Medical Surgical NursingDocument14 pagesResearch Critique: Subject: Research Speciality - Medical Surgical NursingGayatri MudliyarNo ratings yet
- Annotated Bibiliography 6Document12 pagesAnnotated Bibiliography 6falguni mondal100% (1)
- Folie A Deux - Michael A. Sacks 1988Document8 pagesFolie A Deux - Michael A. Sacks 1988Grandfather NurgleNo ratings yet
- MutismDocument10 pagesMutismlaviNo ratings yet
- Nursing Leadership AssignmentDocument10 pagesNursing Leadership AssignmentAssignment Help Australia100% (5)
- Psychiatric Mental Health Comprehensive Case Study 1Document11 pagesPsychiatric Mental Health Comprehensive Case Study 1api-402950137No ratings yet
- Case StudyDocument10 pagesCase StudyHomework PingNo ratings yet
- Assignment ON: Writing The Reference and BibliographyDocument8 pagesAssignment ON: Writing The Reference and BibliographyAru VermaNo ratings yet
- Collaboration Issues and Models Within and Outside Nursing: Sangeetha Antoe M.SC (N)Document66 pagesCollaboration Issues and Models Within and Outside Nursing: Sangeetha Antoe M.SC (N)rinku100% (1)
- Case Study of A Client Diagnosed With Major Depressive Disorder PDFDocument103 pagesCase Study of A Client Diagnosed With Major Depressive Disorder PDFAnonymous vfp4bjGL100% (1)
- Advanced Nursing PracticeDocument12 pagesAdvanced Nursing PracticeKish KimzNo ratings yet
- Framework, Scope & Trends of Nursing PracticeDocument11 pagesFramework, Scope & Trends of Nursing PracticeRajesh Sharma50% (2)
- Revised Proforma Guidelines Internal Assessment II PBBSC 011007Document58 pagesRevised Proforma Guidelines Internal Assessment II PBBSC 011007mljg30100% (2)
- Maniba Bhula Nursing College: Subject: Nursing Education Topic: Essay Type TestDocument6 pagesManiba Bhula Nursing College: Subject: Nursing Education Topic: Essay Type TestRinal BaradNo ratings yet
- Issues of Mental Health NursingDocument16 pagesIssues of Mental Health NursingElita FadhliNo ratings yet
- Evidence Based Practice in NursingDocument86 pagesEvidence Based Practice in NursingKrea kristalleteNo ratings yet
- Autism Europe, PERSONS WITH AUTISM SPECTRUM DISORDERS Identification, Understanding, InterventionDocument28 pagesAutism Europe, PERSONS WITH AUTISM SPECTRUM DISORDERS Identification, Understanding, Interventioninfo-TEANo ratings yet
- MSC Nursing EducationDocument28 pagesMSC Nursing EducationSoniyaNo ratings yet
- Theory of Goal AttainmentDocument1 pageTheory of Goal AttainmentJonathan Cruz TalonNo ratings yet
- Orem'S Theory and Nursing ProcessDocument20 pagesOrem'S Theory and Nursing ProcessSusma KaliNo ratings yet
- Introduction:-: Background of Theorist (Dorothea Orem 1914-2007)Document27 pagesIntroduction:-: Background of Theorist (Dorothea Orem 1914-2007)Pragnya BhattacharjeeNo ratings yet
- Collaboration Issues and Models Within and Outside Nursing: Presented To: Presented By: Dr. Prabhjot Saini SanjanaDocument80 pagesCollaboration Issues and Models Within and Outside Nursing: Presented To: Presented By: Dr. Prabhjot Saini SanjanaManinder SekhonNo ratings yet
- Professional Organisations in NursingDocument11 pagesProfessional Organisations in NursingSri Devy100% (1)
- Lesson PlanDocument8 pagesLesson PlanUpendra Nayka50% (2)
- Stressors Nursing StudentsDocument9 pagesStressors Nursing StudentsJamesRGNNo ratings yet
- FF Staff Relationship and TechniquesDocument15 pagesFF Staff Relationship and TechniquesAnkita Patel100% (1)
- Annotated Bibliography AssignmentDocument5 pagesAnnotated Bibliography Assignmentapi-242256465100% (2)
- Business PlanDocument26 pagesBusiness PlanAssignment Help Australia78% (9)
- Personal Philosophy of NursingDocument3 pagesPersonal Philosophy of Nursingapi-448020611No ratings yet
- Paplau, AbdellahDocument41 pagesPaplau, AbdellahJ Ta RaNo ratings yet
- Patricia Benner R.N., PH.D., F.A.A.N., F.R.C.N.: PurposeDocument6 pagesPatricia Benner R.N., PH.D., F.A.A.N., F.R.C.N.: PurposeKhieryl MaranionNo ratings yet
- Health Promotion Stress Management AssignmentDocument10 pagesHealth Promotion Stress Management Assignmentapi-211472021No ratings yet
- Evaluation of Students Performance in Clinical Practice: Objective IDocument11 pagesEvaluation of Students Performance in Clinical Practice: Objective IAMY LALRINGHLUANI M.Sc. Child Health (Paediatric ) NursingNo ratings yet
- Health Care Delivery Concerns, National Health andDocument26 pagesHealth Care Delivery Concerns, National Health andKavi rajputNo ratings yet
- Annotated BibliographyDocument4 pagesAnnotated Bibliographymadelinegrey100% (1)
- Awareness of Mothers Regarding Child Abuse and Its Prevention in IndiaDocument4 pagesAwareness of Mothers Regarding Child Abuse and Its Prevention in IndiaEditor IJTSRDNo ratings yet
- Interdisciplinary Collaboration: Experience of Working in An Interdisciplinary Team in Healthcare at The MOI Teaching and Referral Hospital, Intensive Care UnitDocument3 pagesInterdisciplinary Collaboration: Experience of Working in An Interdisciplinary Team in Healthcare at The MOI Teaching and Referral Hospital, Intensive Care UnitInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- General Objective: at The End of Class, The Students Should Be Able To Explore About The Perspectives of Global and National NursingDocument18 pagesGeneral Objective: at The End of Class, The Students Should Be Able To Explore About The Perspectives of Global and National Nursingamita chaudhariNo ratings yet
- Vancouver Citation StyleDocument13 pagesVancouver Citation StylenioditaNo ratings yet
- Human RightsDocument112 pagesHuman RightsAKHILA PKNo ratings yet
- Complementary Therapies in NursingDocument12 pagesComplementary Therapies in NursingHamza Ishtiaq100% (1)
- Theory of Interpersonal RelationsDocument6 pagesTheory of Interpersonal RelationsEJ Gabao100% (6)
- Futuristic NursingDocument3 pagesFuturistic NursingDeerpraj CmNo ratings yet
- Dissertation Topics Medical Surgical NursingDocument8 pagesDissertation Topics Medical Surgical NursingBuyThesisPaperUK100% (2)
- IPHS Fo SC PHC CHCDocument18 pagesIPHS Fo SC PHC CHCDrArun SinghNo ratings yet
- Nursing DelegationDocument2 pagesNursing DelegationAndre FortunaNo ratings yet
- Abdellah's TheoryDocument6 pagesAbdellah's TheoryBaldeep GrewalNo ratings yet
- E-ISSN: 2347-8640 P-ISSN: 2454-2660, Issue JETIR, (JULY September 2016)Document9 pagesE-ISSN: 2347-8640 P-ISSN: 2454-2660, Issue JETIR, (JULY September 2016)VaishaliNo ratings yet
- Nursing DiagnosisDocument3 pagesNursing DiagnosisjesuslovmeNo ratings yet
- Annotated Bibliography: INTRODUCTION-An Annotated Bibliography Is Typically Short (Usually ADocument6 pagesAnnotated Bibliography: INTRODUCTION-An Annotated Bibliography Is Typically Short (Usually AVinita TiwariNo ratings yet
- Annectotal RecordDocument6 pagesAnnectotal RecordValarmathiNo ratings yet
- Legal Issues in Community Health NursingDocument22 pagesLegal Issues in Community Health NursingJune SavillaNo ratings yet
- Effectiveness of Video Assisted Teaching Module On Knowledge and Attitude Regarding Health Effects of Internet Addiction Disorders Among AdolescentsDocument4 pagesEffectiveness of Video Assisted Teaching Module On Knowledge and Attitude Regarding Health Effects of Internet Addiction Disorders Among AdolescentsAnonymous lAfk9gNPNo ratings yet
- An Experimental Study To Assess-5996Document5 pagesAn Experimental Study To Assess-5996Priyanjali SainiNo ratings yet
- Course Plan of Community Health NursingDocument13 pagesCourse Plan of Community Health NursingParbati samantaNo ratings yet
- Sainath School of Nursing, GNM SyllabusDocument101 pagesSainath School of Nursing, GNM SyllabusFabin JoseNo ratings yet
- Community Health Nursing ProcessDocument8 pagesCommunity Health Nursing ProcessAncy Varkey0% (1)
- MSC Disseration ProjectsDocument12 pagesMSC Disseration ProjectsKowsalyaram RamNo ratings yet
- Health and Illness ConceptsDocument3 pagesHealth and Illness ConceptsSdvNo ratings yet
- Definition of NursingDocument58 pagesDefinition of NursingN. SivaNo ratings yet
- Rajiv Gandhi University of Health Sciences, Bangalore, KarnatakaDocument13 pagesRajiv Gandhi University of Health Sciences, Bangalore, KarnatakaAmit TamboliNo ratings yet
- Establishment of Edn InstitutionDocument88 pagesEstablishment of Edn InstitutionNise Mon KuriakoseNo ratings yet
- Process Recording, Suicide Assesment and Psyche-Med ConditionDocument44 pagesProcess Recording, Suicide Assesment and Psyche-Med ConditionShy Dela PuertaNo ratings yet
- Notes on Nursing: What it is, and what it is notFrom EverandNotes on Nursing: What it is, and what it is notRating: 4 out of 5 stars4/5 (24)
- Education Program On Childhood ObesityDocument8 pagesEducation Program On Childhood ObesityAssignment Help AustraliaNo ratings yet
- CSR Case Study HelpDocument8 pagesCSR Case Study HelpAssignment Help Australia100% (1)
- Nursing Case Study HelpDocument8 pagesNursing Case Study HelpAssignment Help Australia100% (1)
- Lululemon Case StudyDocument8 pagesLululemon Case StudyAssignment Help Australia67% (3)
- Law Assignment Help SampleDocument16 pagesLaw Assignment Help SampleAssignment Help AustraliaNo ratings yet
- Psychopathology: Shafa Ahmad bms15091813 Amal Abdulkhadir bms15091333Document13 pagesPsychopathology: Shafa Ahmad bms15091813 Amal Abdulkhadir bms15091333SHAFA AHMED MUTAHAR HURAIRAHNo ratings yet
- Anger Disorder Among Us TeensDocument3 pagesAnger Disorder Among Us TeensChristine See de BelenNo ratings yet
- COMMON BEHAVIOURAL DISORDER OF CHILDREN AND MANAGEMENT .Edu TechDocument83 pagesCOMMON BEHAVIOURAL DISORDER OF CHILDREN AND MANAGEMENT .Edu Techjmbrand jmNo ratings yet
- Schizoaffective With Bipolar DisordersDocument14 pagesSchizoaffective With Bipolar DisordersNaomi MasudaNo ratings yet
- Schizophrenia EssayDocument6 pagesSchizophrenia EssayLaura Jinparn100% (1)
- Addiction EssayDocument5 pagesAddiction Essayapi-341235528No ratings yet
- MHRC Submission Croton DUAL - DIAGNOSIS 2Document77 pagesMHRC Submission Croton DUAL - DIAGNOSIS 2HarjotBrarNo ratings yet
- Jurnal PDFDocument14 pagesJurnal PDFIcha IchaNo ratings yet
- Common Problem of Critical Care of PatientDocument5 pagesCommon Problem of Critical Care of PatientSaif Ahmed jubarNo ratings yet
- The Epidemiology of Post-Traumatic Stress Disorder: Steven S. Coughlin, PH.DDocument20 pagesThe Epidemiology of Post-Traumatic Stress Disorder: Steven S. Coughlin, PH.DanggiaNo ratings yet
- Theory and Practice of Counseling and Psychotherapy: Coginitive BehaviorDocument15 pagesTheory and Practice of Counseling and Psychotherapy: Coginitive BehaviorNor LelaNo ratings yet
- Human Behavior and Crisis Managementfffff PDFDocument78 pagesHuman Behavior and Crisis Managementfffff PDFDan Lawrence Dela CruzNo ratings yet
- Social Anxiety 1Document6 pagesSocial Anxiety 1api-549818636No ratings yet
- OpenStax - Psychology - CH15 PSYCHOLOGICAL DISORDERSDocument42 pagesOpenStax - Psychology - CH15 PSYCHOLOGICAL DISORDERSAngelaNo ratings yet
- The Autism Diagnostic Interview-Revised and CarsDocument2 pagesThe Autism Diagnostic Interview-Revised and CarsDiegoAlexAcostaNo ratings yet
- HESI Blueprint For Psychiatric Health NursingDocument2 pagesHESI Blueprint For Psychiatric Health NursingJenny Vorst40% (5)
- Personality Disorders: Mudr. Martin Perna Dept. of Psychiatry, Masaryk University, BrnoDocument31 pagesPersonality Disorders: Mudr. Martin Perna Dept. of Psychiatry, Masaryk University, BrnoabrihamNo ratings yet
- Informative EssayDocument1 pageInformative EssayAnonymous QfGtm07gjNo ratings yet
- Title Defense FormatDocument10 pagesTitle Defense Formatlance dunglay lesinNo ratings yet