Professional Documents
Culture Documents
Hematological Systems - Lecture Notes
Uploaded by
Amiel Francisco ReyesOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hematological Systems - Lecture Notes
Uploaded by
Amiel Francisco ReyesCopyright:
Available Formats
Ex.
Varicosities
Deep Vein Thromboplehbities
Ex.
Aneurysm
Buergers Disease
Raynauds Disease
Plasma CHONs (Liver)
1. Albumin - largest, most abundant plasma
Fx: Maintains osmotic pressure preventing edema,
If decrease albumin- Ascites
Promotes skin integrity
2. Globulins
a. Alpha Transports steroids, hormones & bilirubin
b. - Transports iron & copper
c. Gamma Transport immunoglobulins or antibodies
3. Prothrombin (CF2) Fibrinogen (CF1)
Clotting factor to prevent bleeding
- Spleen life span = 120 days
Cellular Components:
1. RBC (Erythrocytes)
- largest
(Normal: 4 6 M/mm3)
- Anucleated (no nucleus)
- Biconcave discs
- Has molecules of Hgb (red cell pigment)
- Transports & carries O2
Hgb:
F = 12-14 gms%
M = 14-16 gms %
Hct : 3x Hgb
F = 36-42 %
M = 42-48 %
Average = 42 %
HEMATOLOGICAL SYSTEMS
Overview:
I . BLOOD-FORMING ORGANS
1.Thymus removed myasthenia gravis
2. Liver largest gland (occupies most of the right hypochondriac region)
3. Lymph nodes
4. Lymphoid organs Payers Patches (located between the small intestine- site of salmonella thypi)
5. Bone marrow
6. Spleen
II. BLOOD VESSELS
1. Veins SVC, IVC, Jugular vein, superficial blood towards the heart
2. Artery deep seated, carries blood away from the
- 2 largest artery : Aorta, carotid
3. Capillaries
III. BLOOD
Blood
Formed Elements 45 % 55% Plasma & Serum
CLOTTING FACTOR 1-13
CF 1 = Fibrinogen From
CF 2 = Prothombin Pakistan
CF 3 = Thrombin To
CF 4 = Ca # China
CF 5/6 = Proaccelerin - Labile factor People
CF 7 = Procenvertion - Stable Factor Power
CF 8 = Anti- HFA Against
CF 9 = Christmas Factor/ Anti-hemophilia Communism
CF 10 = Stuart-Prower Start
CF 11 = Plasma Thromboplastin Peace
CF 12 = Hageman Hate
CF 13 = Fibrin Stabilizing Factor Fire
COAGULATION PATHWAY/CASCADE
Intrinsic Factor Stage 1 Extrinsic Factor
EF TF TF (CF3)
CF 12
CF 9 F
CF 11
CF 9--------------------------------------------------CF 10 ------------------------------------------ CFS
Creates------Prothrombinase----------------- CF 2 Stage 2
Product of Stage 1
Thrombin
Stage 3
CF 1
Fibrin
Clot -------- --Clot dissolved
Tissue Plasminogen Activator
Plasminogen
Plasmin Stage 4
1
st
Sign of ANEMIA:
Weakness & Fatigue
Hallmark & Basis of Anemia
All symptoms cause by this
Lesions at the
corner of the mouth
D/T compensation of the
body
D/T decreased
RBC
D/T decreased Hgb that
gives color to skin
KOILONYCHIA
d/t atrophy of epidermal
cells
Life span of RBC
8-120 days
I. DISORDERS OF THE BLOOD
Pathophysiology:
BLOOD DYSCRASIA
Production of blood cells Production of both normal Spleen Disorder Defect in Coagulation
(PANCYTOPENIA) & defective cells Mechanism
1. ANEMIA
- A condition in which the hemoglobin concentration is lower than normal
- Results from :
1. Decreased Erythropoiesis (Formation-maturation process of RBC)
2. Increased Hemolysis
3. Bone Marrow Depression
4. Blood loss
Pathophysiology: Hgb Count
Reduction in the O2 carrying capacity of the blood
TISSUE HYPOXIA
Brain Restlessness Heart Respiratory GIT Skin
Headache, Irritability Anginal Pain RR Anorexia Mucus Membrane
Syncope, Vertigo PR Dyspnea Angular Cheilosis
Fatigability
Palpitation
Pallor
Brittle nails & hair
(Spoon-shaped nails)
Intolerance to Cold
Normal shape of nails = Biconcave & 180
Substances Needed For Maturation Of RBC:
1. CHON formation of all tructure/membrane
2. Iron/Fe - formation of pigment hemoglobin
3. Vit. B 12 - responsible for synthesis of nucleic acid
4. Folic Acid - matures the cell
5. Vit. C - catalyst for iron/absorption of iron
6. Vit. B6
7. Intrinsic Factor
Common:
Suicide - common in teenager
Poisoning common in children (aspirin)
Aspiration common in infant
Accidents common in adults
Choking common in toddler
SIDS common in infant in US
Bleeding:
Hematemesis vomiting of blood
Melena passage of dark stool
- Bleeding in Upper GIT
- Doudenal Cancer
Hematochezia passage of fresh blood
- Bleeding in Lower GIT
- large intestine
Nsg Dx:
Activity Intolerance
Decreased O2
Atrophy of cells
Cerebral Hypoxia
PICA
CAUSES:
I. DECREASED ERYTHROPOIESIS
Production maturation of RBC
Absence of any one of the factors
For RBC maturation will cause
Type I:
A. IRON DEFECIENCY ANEMIA
- Cells are microcytic (small) & hypochronic d/t inadequate absorption of iron leading to hypoxemic injury
HYPOCHROMIC ANEMIA HYPOPROLIFERATIVE ANEMIA
Pathophysiology: The body stores of iron decrease, leading to depletion of hemoglobin synthesis
Incidence Rate:
1. Common in developed country d/t high cereal intake & accidents
2. Common in tropical countries blood sucking insects
3. Women 15 45 y/o of reproductive yrs
4. Common among the poor d/t poor nutritional intake
Predisposing Factors:
1. Chronic blood loss- most common cause
a. Trauma
b. Menstruation
c. GIT bleeding
2. Inadequate intake of food rich in iron
3. Inadequate absorption or iron d/t :
a. Chronic diarrhea (Metabolic Acidosis)
b. Malabsorption syndrome (Celiac Disease)
c. High cereal intake with low animal CHON ingestion
d. Subtotal gastrectomy
4. Improper cooking of food/ Alcoholism
S/Sx:
1. Asymptomatic
2. General body malaise
3. All Sx of Anemia + PICA abnormal appetite or craving for non-edible food Ex. Chalk
+ PLUMMER VINSONS SYNDROME Atropic Glossitis inflammation of tongue
Stomatitis mouth sores
Dysphagia
Dx :
1. RBC
2. Hgb
3. Reticulocyte
4. Hct
5. Iron
IRON-RICH FOOD:
1
ST
: organ meat, liver
2
nd
: eggyolk
3
rd
: raisins, legumes
dried fruits
nuts
4
th
: green leafy vegetables
IRON Side-Effects:
Anorexia
N/V
Abdominal Pain
Diarrhea/ Constipation
Melena
6. Ferritin
7. Bone Marrow Aspiration = Most Definitive
Tx:
1. Blood Transfusion = Packed RBC
Nsg Mgt:
1. Monitor signs of bleeding of all hematologic test including urine, stool & GIT
2. Complete bed rest dont overtire pt
3. Encourage iron rich food
4. Instruct the pt to avoid taking tea (Tannates - impairs iron absorption)
5. Administer meds: Hematinic Agents or drugs that will increase blood heme
a.) Oral iron preparation
Ferrous SO4
Fe gluconate 300 mg OD
Fe Fumarate
Fortifier
Fergon, Feorol, Iberet
*Liquid Preparations: W/ brassy taste, disguise by chilling
Nsg Mgt Of Oral Iron Medication:
1. Administer w/ meals to lessen GIT irritation/or 0ne hours before meals
2. If diluting in iron liquid prep administer w/ straw
3. Give Orange juice for absorption
4. Monitor & inform pts S/E
5. If pt cant tolerate oral iron preparation
Administer parenteral iron preparation
1. Iron dextran (IV, IM)
2. Sorbitex (IM only)
3. Inferon, Jectofer
Nsg Mgt Parenteral Iron Preparation:
1. Administer using Z tract method to prevent discomfort, discoloration leakage to tissues.
2. Dont massage injection site. Ambulate to facilitate absorption.
3. Monitor S/E:
a.) Pain at injury site
b.) Localized abscess (nana)
c.) Lymphadenopathy
d.) Fever/ chills
e.) Urticaria itchiness
f.) If (+) to Hypotension ------------Anaphylactic shock
Give epinephrine (SNS Effect)
Largest part of GIT = Large Intestine
Widest part of GIT = Stomach
B. FOLATE DEFICIENCY ANEMIA
- Cell is macrocytic, hypochromic anemia
- A form of MEGALOBLASTIC ANEMIA
- Anemias characterized by abnormal large RBC 2
nd
to impaired DNA synthesis d/t deficiency of Folic acid
Pathophysiology:
Folic acid impaired DNA synthesis in the bone marrow impaired RBC development, impaired nuclear
maturation but cytoplasmic maturation continues large size
Causative Factors:
1. Alcoholism
2. Mal-absorption
3. Diet deficient in uncooked vegetables
Sx: All symptoms of Anemia
C. PERNICIOUS ANEMIA
- A megaloblastic chronic anemia characterized by deficiency of intrinsic factor secreted by the parietal cells
leading to Hypochlorhydria---------decrease Hcl acid secretion
- A Vit. B12 deficiency
Predisposing Factors:
1. Subtotal Gastrectomy partial removal of the stomach
2. Atrophy of gastric mucosa (elderly) ------ # 1 cause
3. Hereditary
4. Inflammatory disorder of ileum
5. Autoimmune
6. Strict vegetarian diet
7. Gastrointestinal malabsorption----Crohns Disease/ Cancer of stomach
Pathophysiology: STOMACH (composed of different cells)
Parietal or ergentaffen Oxyntic cells
Function: Produce Intrinsic Factor Function: Secrets Hcl acid
INTRINSIC FACTOR HYDROCHLORIC ACID
Binds w/ Vit. B12 to promote absorption Aids in digestion
For maturation of RBC Decreased Digestion ----- Dyspepsia & Weight Loss
Disorder in the Process
Diet: High caloric Intake to correct Wt loss
Immature RBC
Killed by Spleen
Heme----Globin
Ferroes------------Ferretin = Bilirubin ----- Jaundice
Common Route: Dorso-gluteal
Ventro-gluteal
S/Sx:
1. All Sx of Anemia +
2. GIT changes
a. RED BEEFY TONGUE = PATHOGNOMONIC SIGN
b. Dyspepsia indigestion
c. Wt loss, mild diarrhea
d. Jaundice
3. CNS Most dangerous anemia d/t neurologic involvement d/t deficiency in Vit. B 12
a. Tingling sensation
b. Paresthesia (numbness) in extremities
c. (+) Rombergs test = Ataxia
d. Psychosis
Dx:
1. Peripheral Blood Smear = shows giant RBCs, WBCs w/ giant hypersegmented nuclei
2. Very High MCV
3. Shillings Test = reveals inadequate absorption of Vit. B 12
4. Intrinsic Factor Antibody Test
Tx:
1. Vit. Supplementation : Folic Acid 1 mg daily
2. Diet Supplementation
3. Lifetime monthly injection of IM Vit. B 12 as ordered -----not oral---pt. may developed drug toleranceNo S/E
Nsg Mgt :
1. Enforce CBR
2. Diet high calorie or CHO----Increase CHON, iron & Vit C
3. Avoid irritating mouthwashes. Use of soft bristled toothbrush is encourage
4. Avoid applying electric heating pads can lead to burns
II. INCREASE HEMOLYSIS/ HEMOLYTIC ANEMIA
- Destruction of RBC greater than the rate of formation
----all + Hyperbilirubinemia-----JAUNDICE + TEA-COLORED URINE
Causes:
1. Post-viral injection
2. Exposure to ionizing radiation
3. Prolong use of toxic drugs & medications (penicillin, chloramphenicol)
Type II:
A. SICKLE CELL ANEMIA
- A severe chronic incurable hemolytic anemia that results from heritance of the sickle hemoglobin gene.
Causative Factor:
1. Genetic inheritance of the sickle gene- HbS gene
Pathophysiology:
Decreased O2, Cold, Vasoconstriction can precipitate sickling process
Factors cause defective Hgb to acquire a rigid, crystal-like C-shaped configuration
Sickled RBCs adhere to endothelium pile up & plug the vessels ischemia results pain, swelling & fever
Sx:
1. Jaundice
2. Enlarged skull & facial bones
3. Tachycardia, murmurs & cardiomegaly
Primary sites of thrombotic occlusion: spleen, lungs & CNS
4. Chest pain, dyspnea
Complications:
1. Sickle Cell Crises = Results from tissue hypoxia & necrosis
2. Acute Chest Syndrome = Manifested by a rapidly falling Hgb level, tachycardia, fever & chest infiltrates in the CXR
3 Nursing Priority:
1. A/W Avoid deoxygenating activities
- High altitude is bad
2. Fluid Deficit Promote hydration
3. Pain & Comfort
POLYCYTHEMIA
Earliest Sign : Headache
Late Sign: Pruritus
Complication: Stroke, Thrombosis
Tx:
1. Bone marrow transplant
2. Hydroxyurea = Increases the Hgb
3. Long term RBC transfusion = Packed RBC
Surgery For Hemolytic anemia = Spleenectomy
Nsg Mngt:
1. Manage the pain
Support & elevate acutely inflamed joint
Relaxation techniques
Analgesics
2. Prevent and manage infection
Monitor status of patient
Initiate prompt antibiotic therapy
3. Promote coping skills
Provide accurate information
Allow patient to verbalize her concerns about medication, prognosis & future pregnancy
4. Monitor and prevent potential complications
Provide always adequate hydration
Avoid cold, temperature that may cause vasoconstriction
5. Monitor and prevent potential complications
Leg ulcer
Aseptic technique
Priapism = Sudden painful erection
Instruct patient to empty bladder, then take a warm bath
B. POLYCYTHEMIA
- Refers to an INCREASE volume of RBCs -----reverse of sickle cell anemia
- The hematocrit is ELEVATED to more than 55%
Classified as Primary or Secondary
1. POLYCYTHEMIA VERA
- Primary Polycythemia
- A proliferative disorder in which the myeloid stem cells become uncontrolled
Causative Factor: Unknown
Pathophysiology:
The stem cells grow uncontrollably
The bone marrow becomes HYPERcellular & all the blood cells are increased in number
The spleen resumes its function of hematopoiesis and enlarges
Blood becomes thick & viscous causing sluggish circulation
Overtime, the bone marrow becomes fibrotic
Sx:
1. Skin is ruddy
2. Splenomegaly
3. Dizziness, blurred vision, HA
5. Angina, dyspnea & thrombophlebitis
Dx:
1. CBC- shows elevated RBC mass
2. Normal oxygen saturation
3 Elevated WBC & Platelets
Complications:
1. Increased risk for thrombophlebitis, CVA MI
2. Bleeding d/t dysfunctional blood cells
Tx:
1. To reduce the high blood cell mass- PHLEBOTOMY
2. Allopurinol
3. Dipyridamole
4. Chemotherapy to suppress bone marrow
Nsg Mngt:
1. Primary role of the nurse is EDUCATOR
2. Regularly assess for the development of complications
3. Assist in weekly phlebotomy
4. Advise to avoid alcohol & aspirin
5. Advise tepid sponge bath or cool water to manage pruritus
III. BONE MARROW DEPRESSION/ HYPOPLASTIC ANEMIA
- Inadequate abnormal cells-------Hypoplastic anemia/Aplastic Anemia
- All Sx + decreased WBC --------------Leukopenia ----------risk for infection
+ decreased PLATELETS--- Thrombocytopenia----- bleeding
when all 3 are present ----- PANCYTOPENIA
WBC
(Leucocytes 5,000 10,000/mm3)
GRANULOCYTES
3 Types:
1. Polymorphonuclearneutrophils (PMNs)
- Most abundant 60-70% WBC
- Lifespan of 24-48 hrs.
Function: Short-term Phagocytosis
For acute inflammation
2. Polymorphous Basophils (PMBa)
-Involved in Parasitic infection
- Release of chemical mediator for inflammation
(Serotonin, Histamine, Prostaglandin, Bradykinins)
-Absorbs large fat particles after ingestion of high fat meal
NON-GRANULOCYTES
A. Monocytes (Macrophage)
-Largest WBC
- Involved in long term phagocytosis
- For chronic inflammation
- Other name macrophage
Macrophage in CNS- Microglia
Macrophage in skin Histiocytes
Macrophage in lungs Alveolar macrophage
Macrophage in Kidneys Kupffer cells
B. Lymphocytes
3 Types:
SIGNS OF PLATELET DYFUNCTION
1. Petecchiae
2. Ecchymosis/bruises
3. Oozing of blood from venipuncture site
HIV
Window Period: 6 months
Incubation: 6 months to 5 yrs.
Sx: Kaposi Sarcoma
Dx Test: Western Blot Test
Drug of Choice:
Zidovudine ( AZT or Retrovir)
Standar Precaution:
Gloves, Gown, Goggles & Mask
3. Polymorphous Eosinophils (PMEo)
- Involved in Allergic reactions
1. B Cell L
Bone marrow or bursa dependent
- Arises from bone marrow
2. T Cell
Devt of immunity
- From thymus
- Target cell of HIV
3. NK Cell
Natural killer cell
-Have both antiviral & anti-tumor properties
C. Platelets (Thrombocytes)
(Normal: 150,000 450, 000/ mm3)
- Promotes homeostasis prevention of blood loss
by activating clotting
- Consists of immature or baby platelets known as
Megakaryocytes Target of Dengue Virus
- Normal lifespan 9 12 days
A. APLASTIC ANEMIA
A condition characterized by decreased number of RBC as well as WBC & platelets
- Common among clients undergoing chemotherapy, Cobalt therapy, Radiation therapy
- Stem cell disorder d/t bone marrow depression leading to pancytopenia all RBC are decreased
Decrease RBC Decrease WBC Decrease platelets
Anemia Leucopenia Thrombocytopenia
Susceptibility to infection No clotting
Fever Bleeding
Petechia Ecchymosis Bruising
(Purpura)
Predisposing Factors :
1. Environmental Toxins & Chemicals Pesticides, Benzene & its derivatives
2. radiation
3. Immunologic injury
4. Certain drugs causes bone marrow depression
a. Chemotherapeutic agents, = Methotrexate, Nitrogen Mustard (anti-metabolite), Vincristine
b. Broad Spectrum antibiotic =Chlorampenicol, Sulfonamides bactrim
(Pt severe isolation)
c. Phenybutazones
5. Heavy Metals
Bone Marrow Transplantation
1. Syngeneic BMT
donor from twins
2. Allogenic BMT
Related or unrelated as long
as compatible (Human leukocyte antigen)
3. Autologous BMT
Own self
- harvest marrow during remission
Pathophysiology:
Toxins cause a direct bone marrow depression acellular bone marrow decreased production of blood elements
Sx:
1. All Sx of Anemia +
2. Leucopenia increase susceptibility to infection
3. Thrombocytopenia
4. Splenomegaly
5. Retinal hemorrhages
Dx:
1. CBC- decreased blood cell numbers
2. Bone marrow aspiration at posterior iliac crest: Confirms the anemia- hypoplastic or acellular marrow replaced by fats
Fatty streaks in bone marrow
Tx:
1. Bone Marrow Transplantation
2. Immunosuppressant drugs
3. Rarely, steroids
4. Blood transfusion = Fresh Whole blood
Nsg Mgt:
1. Removal of underlying cause
2. Blood transfusion as ordered
3. CBR
4. O2 inhalation
5. Reverse isolation d/t leukopenia
6. Monitor signs of infection
7. Avoid SQ, IM or any venipuncture site
8. Use electric razor when shaving to prevent bleeding
9. Administer meds:
Immunosuppressant
Anti lymphocyte globulin (Alg) given via central venous catheter, 6 days 3 weeks to achieve max therapeutic effect of
drug.
IV. BLOOD LOSS
- Cells are normocytic (normal size), normochronic (normal content) but d/t surgery, menstruation------anemia
- All Sx + Hypovolemia
- Blood Transfusion = Fresh Whole blood
OTHER BLOOD RELATED PROBLEMS
1. DISSEMINATED INTRAVASCULAR COAGULATION (DIC)
- Acute hemorrhagic syndrome characterized by wide spread bleeding & thrombosis d/t a deficiency of clotting
factors (Prothrombin & Fibrinogen).
Predisposing Factor:
1. Rapid BT d/t hemolysis
2. Massive trauma
3. Massive burns
4. Septicemia
5. R/T Hemolytic reaction & Anaphylaxis
6. Neoplasia new growth of new tissue (tumor)
7. Pregnancy
8. Septicemia
S/Sx:
1. Petechiae widespread & systemic (lungs, lower & upper trunk)
2. Ecchymosis widespread
3. Oozing of blood from venipunctured site
4. Hemoptysis cough blood
5. Hemorrhage
6. Oliguria---------------LATE SIGN
RBC
Normal Size: 80-94 cu micron
< 80 ---- Microcytic Cell ANISOCYTOSIS
> 94 ----- Macrocytic Cell (abnormal size)
Normal Hgb content of RBC: 22-28 micromicrogram
< 22 >28
Hypochromic Hyperchromic
Dx :
1. CBC reveals decrease platelets
2. Stool for occult blood (+)
Specimen stool
3. Opthalmoscopic exam sub retinal hemorrhage
4. ABG analysis metabolic acidosis
Nsg Mgt:
1. Monitor signs of bleeding All hematologic test + urine, stool, GIT
2. Administer isotonic fluid solution
3. Administer O2 inhalation
4. Administer meds:
a. Vit K aquamephyton
b. Pitressin or vasopressin -----t o conserve H20 & has vasoconstriction effect----Most Common S/E: Chest Pain
5. NGT lavage
- Use iced saline lavage 1
st
to induce vasoconstriction inside the stomach
6. Monitor NGT output
7. Provide heplock
8. Prevent complication: Hypovolemic shock----Early Sign: Restlessness & Cool moist Skin
Late Sign of hypovolemic shock : Anuria
9. Give Heparin-----short-acting
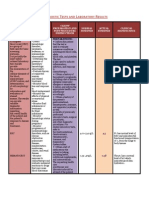
DIAGNOSTIC TEST FOR BLOOD DYSCRASIAS
1. CBC, Hgb, Hct
2. BT, CT, PT
3. ERYTHROCYTE INDEX
MCV = Mean Corpuscolar Volume -----to evaluate size of RBC
MCH = Mean corpuscular Hgb -----------to evaluate the Hgb content of RBC
MCHC = Mean corpuscular Hgb Concentrationto evaluate Hgb content of Pack RBC (in grams /100ml)
(Normal: 30-36 grams/100ml)
4. COOMBS TEST
- To evaluate the presence of immune bodies that adheres to
RBC causing hemolysis/agglutinization of RBC
(Rh Incompatibility, ABO Incompatibility)
POIKILOCYTOSIS = abnormality in shape of RBC
METARUBRICYTE = abnormal RBC w/ nucleated
Packed RBC = 250 ml
Refrigerated = 3-5 days
Platelet = 3-6 days
5. SCHILLING TEST
- To evaluate rate of absorption of Vit. B12 (Cyanocobalamine)
- Use to diagnosed Pernicious Anemia
Procedure: Administer P.O. radioactive Vit. B12 ------24 hr. urine
Check (+) (-) of Vit. B12 ------ if (-) Pernicious Anemia (do not give P.O. give parenterally)
------ if (+) in urine ---normal
Common in Pts. Who undergone gastrectomy/ cancer----they do not have intrinsic factor
6. BONE MARROW ASPIRATION/PUNCTURE/TAP
- To evaluate size, shape, character of RBC cells
- Invasive (consent)
- Local anesthesia (lidocaine 1-2%)
- Sites: Sternum ------ Position: Supine
A & P Iliac Crest ------ Position: Supine (A) & Prone/Lateral (P)
- Pediatric pts. --- use the long bones (femur, humerus)-----as we grow older the # of marrows in long bones decreases
- Apply pressure dressing over site to prevent bleeding
7. LYMPH NODE BIOPSY
- Site : Cervical LN, Axilla LN, Inguinal LN
IV. BLOOD TRANSFUSION:
Objectives:
1. To replace circulating blood volume
2. To increase O2 carrying capacity of blood
3. To combat infection if theres decrease WBC
4. To prevent bleeding if theres platelet deficiency
Nsg Mgt & Principles in Blood Transfusion
1. Proper refrigeration
2. Proper typing & cross matching
Type O universal donor
AB universal recipient
85% of people are RH (+)
3. Aseptically assemble all materials needed:
a.) Filter set
b.) Isotonic or PNSS or .9NaClfor flushing to prevent Hemolysis
Hypotonic solution Cell swells or burst
Hypertonic solution Cell will shrink or crenate
c.) Needle gauge 18 - 19 or large bore needle to prevent hemolysis.
d.) Instruct another RN to recheck the following .
Pts name, blood typing & cross typing expiration date, serial number Most important
e.) Check blood unit for bubbles, cloudiness, dark in color & sediments indicates bacterial contamination.
Return to blood bank, do not dispose
BT REACTIONS:
H - Hemolytic Reaction
A - Allergic Reaction
P - Pyrogenic Reaction
C - Circulatory Reaction
A - Air Embolism
T - Thrombocytopenia
C - Citrate Intoxication
H - Hyperkalemia d/t expired blood
f.) Never warm blood products may destroy vital factors in blood.
- Warming is done if with warming device only in EMERGENCY!
- Within 30 mins room temp only!
g.) Blood transfusion should be completed < 4hrs because blood that is exposed at room temp for > 2h causes blood
deterioration------can lead to bacterial contamination
h.) Avoid mixing or administering drug at BT line leads to hemolysis
i.) Regulate BT 10 12 gtts/min KVO or 100cc/hr to prevent circulatory overload
j.) Monitor VS before, during & after BT especially q15 mins for 1st hour
- Majority of BT reaction occurs within 1h.
BLOOD TRANSFUSION REACTIONS:
1. HEMOLYTIC REACTION
Sx:
Headache
Dizziness
Dyspnea
Palpitation
Lumbar/Sternal flank pain
Hypotension, Flushed Skin---red port wine urine
Nsg Mgt:
1. Stop BT
2. Notify Doc
3. Flush with plain NSS
4. Administer isotonic fluid sol to prevent acute tubular necrosis & counteract shock
5. Send blood unit to blood bank for reexamination
6. Obtain urine & blood samples of pt & send to lab for reexamination
7. Monitor VS & Allergic Rxn
2. ALLERGIC REACTION
S/Sx:
1. Fever/ chills
2. Urticaria/ pruritus
3. Dyspnea
4. Laryngospasm/ bronchospasm
5. Bronchial wheezing
Nsg Mgt:
1. Stop BT
2. Notify Doc
3. Flush with PNSS
4. Administer antihistamine diphenhydramine Hcl (Benadryl)
If (+) Hypotension anaphylactic shock administer epinephrine
5. Send blood unit to blood bank
6. Obtain urine & blood samples send to lab
7. Monitor VS & IO
8. Adm. Antihistamine as ordered for Allergic Rxn, if (+) to hypotension indicates anaphylactic shock
Shock -----administer epinephrine
9. Administer antipyretic & antibiotic for pyrogenic Rxn & TSB
PRIORITY CASES
Hemolytic Reaction = 1
st
d/t Hypotension---attend to destruction of Hgb
------ O2----- Brain Damage
Circulatory Reaction = 2
nd
Allergic Reaction = 3
rd
Pyrogenic Reaction = 4
th
But:
Anaphylactic = 1
st
priority
Hemolytic = 2
nd
3. PYROGENIC REACTION:
S/Sx:
a.) Fever/ chills d.) Tachycardia
b.) Headache e.) Palpitations
c.) Dyspnea f.) Diaphoresis
(Pyrogens -----fever-producing agents)
Nsg Mgt:
1. Stop BT
2. Notify Doc
3. Flush with PNSS
4. Administer antipyretics, antibiotics
5. Send blood unit to blood bank
6. Obtain urine & blood samples send to lab
7. Monitor VS & IO
8. Tepid sponge bath offer hypothermic blanket
4. CIRCULATORY OVERLOAD
Sx:
- Dyspnea
- Orthopnea
- Rales or crackles
- Exertional discomfort
Nsg Mgt:
1. Stop BT
2. Notify Doc
3. Administer diuretics
You might also like
- April CXC Exam Plus Answers 2016 (30753)Document15 pagesApril CXC Exam Plus Answers 2016 (30753)Aaron Wallace90% (10)
- MCQ of HematologyDocument22 pagesMCQ of Hematologydrafq200063% (8)
- BiologyNotesForClass11hChapter PDFDocument7 pagesBiologyNotesForClass11hChapter PDFVinod MNNo ratings yet
- Nclex TipsDocument93 pagesNclex TipsAmiel Francisco Reyes86% (7)
- Anemia Unspecified FinalDocument47 pagesAnemia Unspecified FinalMaria Paula BungayNo ratings yet
- Hematology NCLEX MCQDocument24 pagesHematology NCLEX MCQKo Ye100% (2)
- Sickle Cell CaseDocument3 pagesSickle Cell CaseAlanieNo ratings yet
- Urinary SystemDocument10 pagesUrinary Systemapi-19824701No ratings yet
- Chapter 11 Electrolytes LectureDocument76 pagesChapter 11 Electrolytes Lecturegabo dasNo ratings yet
- Connective Tissues: Rochelle M. Delos Santos Ii-A1 Bs-BiologyDocument54 pagesConnective Tissues: Rochelle M. Delos Santos Ii-A1 Bs-BiologyJordan Ramos100% (1)
- Pediatric Nursing or Child Health NusrsingDocument20 pagesPediatric Nursing or Child Health NusrsingGenynne RagasaNo ratings yet
- Genitourinary Tract InfectionsDocument80 pagesGenitourinary Tract Infectionsraene_bautistaNo ratings yet
- UntitledDocument6 pagesUntitledFritz Angelo BullonNo ratings yet
- Module 7 High Risk Newborn 2023Document25 pagesModule 7 High Risk Newborn 2023Vannesa TarifaNo ratings yet
- Fluid and Elctrolyte Balance.... Power PointDocument40 pagesFluid and Elctrolyte Balance.... Power PointMarwan M.100% (1)
- NCM 107 - Fetal Circulation Final PDFDocument4 pagesNCM 107 - Fetal Circulation Final PDFAngelica Rose VillegasNo ratings yet
- Reviewer Skeletal To EndoDocument46 pagesReviewer Skeletal To EndoSophia CaisipNo ratings yet
- Female and Male GenitaliaDocument5 pagesFemale and Male GenitaliaMary Mae BuellaNo ratings yet
- SchistosomiasisDocument33 pagesSchistosomiasishendra ari100% (1)
- Anatomy and PhysiologyDocument11 pagesAnatomy and PhysiologyFiona Aaronica Hope LibrandaNo ratings yet
- Anaphy Topic 1Document15 pagesAnaphy Topic 1RAYNE CHLOIE LASTANo ratings yet
- Breast and AxillaeDocument13 pagesBreast and AxillaeJemma NocalanNo ratings yet
- Lec - 1H - Special Senses System ReviewerDocument18 pagesLec - 1H - Special Senses System ReviewerProfessor GhoulNo ratings yet
- Human Skeleton-DlarsonDocument57 pagesHuman Skeleton-Dlarsonapi-308826929No ratings yet
- Individual Case PresentationDocument20 pagesIndividual Case Presentationim. EliasNo ratings yet
- Types of ImmunityDocument35 pagesTypes of ImmunityKailash NagarNo ratings yet
- Vital SignDocument40 pagesVital SignYoelBagusGiarto0% (1)
- Cardiovascular SystemDocument26 pagesCardiovascular SystemJenny Torreda100% (1)
- Tissues ReviewerDocument5 pagesTissues ReviewerJoannah MarieNo ratings yet
- Fluids and Electrolytes-2Document82 pagesFluids and Electrolytes-2Jem Loterte100% (1)
- Bacte Lec - Prelim ExamDocument84 pagesBacte Lec - Prelim ExamDanielle Anne LambanNo ratings yet
- Commonly Used AbbreviationsDocument3 pagesCommonly Used AbbreviationsjamesNo ratings yet
- Week 2-3 Part 1Document26 pagesWeek 2-3 Part 1EmpieNo ratings yet
- Assignment GiDocument14 pagesAssignment GiVoid LessNo ratings yet
- Maricris Q. Marquita-Uy R.N, M.DDocument42 pagesMaricris Q. Marquita-Uy R.N, M.DAdrian Mai AlanNo ratings yet
- Normal NewbornAssessmentDocument53 pagesNormal NewbornAssessmentMidori SanNo ratings yet
- Chapter 1: Human Anatomy Divisions of Human PhysiologyDocument16 pagesChapter 1: Human Anatomy Divisions of Human PhysiologyBeverly A PanganibanNo ratings yet
- Immediate Care of NewbornDocument4 pagesImmediate Care of NewbornjvjohnNo ratings yet
- Nursing Care of The NBDocument37 pagesNursing Care of The NBJan Oliver YaresNo ratings yet
- Orthopedic Devices DDocument31 pagesOrthopedic Devices Dmakenawairimu30No ratings yet
- Abdella 21 Nursing ProblemsDocument5 pagesAbdella 21 Nursing Problemsian merisNo ratings yet
- The Digestive System: Chapter 23 - Lecture NotesDocument77 pagesThe Digestive System: Chapter 23 - Lecture NotesJonalyn ChewacheoNo ratings yet
- Anatomy and Physiology With Pathophysiology TransesDocument10 pagesAnatomy and Physiology With Pathophysiology Transeshezekiah minNo ratings yet
- Urinary SystemDocument18 pagesUrinary SystemgabbybibobuNo ratings yet
- Lymphatic SystemDocument5 pagesLymphatic SystemCurex QANo ratings yet
- Anatomy Ch. 9 The Senses NotesDocument7 pagesAnatomy Ch. 9 The Senses Notesprincepalestine100% (1)
- D.Y. Patil College of Nursing Kadamwadi, Kolhapur Subject: Child Health Nursing Case Presentation On Type 1 Diabetes MellitusDocument18 pagesD.Y. Patil College of Nursing Kadamwadi, Kolhapur Subject: Child Health Nursing Case Presentation On Type 1 Diabetes MellitusJuhi Johnson JadhavNo ratings yet
- Paramyxoviridae EditedDocument30 pagesParamyxoviridae EditedstudymedicNo ratings yet
- Pregnancy Induced HypertensionDocument7 pagesPregnancy Induced HypertensionRalph Emerson RatonNo ratings yet
- Chapter 1: MicrobiologyDocument18 pagesChapter 1: MicrobiologyShanz HadjirulNo ratings yet
- Final DX ResultsDocument9 pagesFinal DX ResultszysheaiNo ratings yet
- RevalidaDocument5 pagesRevalidaHawkins FletcherNo ratings yet
- Respiratory System ReviewerDocument7 pagesRespiratory System ReviewerVictoria Ellex TiomicoNo ratings yet
- Disorders of The Reproductive SystemDocument10 pagesDisorders of The Reproductive SystemRose Kathreen Quintans AuxteroNo ratings yet
- Heart Reviewer 1Document6 pagesHeart Reviewer 1tokzzNo ratings yet
- Chemical Examination of Fecal SpecimenDocument4 pagesChemical Examination of Fecal SpecimenLois DanielleNo ratings yet
- Patho. Reviewer On Cellular InjuryDocument21 pagesPatho. Reviewer On Cellular InjurySeff CausapinNo ratings yet
- Vital SignsDocument8 pagesVital SignsKenneth DayritNo ratings yet
- S4 L5 SchistosomaDocument5 pagesS4 L5 Schistosoma2013SecBNo ratings yet
- Fluid and Electrolyte Imbalance and Nutritional ProblemDocument98 pagesFluid and Electrolyte Imbalance and Nutritional ProblemPaul EbenezerNo ratings yet
- Urinary System Disorders Practice Quiz #1 (50 Questions)Document26 pagesUrinary System Disorders Practice Quiz #1 (50 Questions)Emy TandinganNo ratings yet
- Skin - Hair.Nails Head & Neck Eyes. Ears. Nose. Sinuses Mouth. PharynxDocument92 pagesSkin - Hair.Nails Head & Neck Eyes. Ears. Nose. Sinuses Mouth. PharynxAT4-11 HUMSS 2 CEDRICK ILAO100% (1)
- Pituitary GlandDocument22 pagesPituitary GlandSara Musavi100% (2)
- Human Anatomy and PhysiologyDocument8 pagesHuman Anatomy and PhysiologyDanielle AguilaNo ratings yet
- Pharma Unit 1-2 Anti - Adrenergic DrugsDocument21 pagesPharma Unit 1-2 Anti - Adrenergic DrugsMIbrahimNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- An Overview of Nursing Informatics ..Document4 pagesAn Overview of Nursing Informatics ..Amiel Francisco ReyesNo ratings yet
- Semis - Nervous SystemDocument16 pagesSemis - Nervous SystemAmiel Francisco ReyesNo ratings yet
- Semis 2 - Drugs Acting On The Endocrine System 2Document11 pagesSemis 2 - Drugs Acting On The Endocrine System 2Amiel Francisco Reyes100% (1)
- Chapter 1Document11 pagesChapter 1Amiel Francisco ReyesNo ratings yet
- Ni For LMSDocument10 pagesNi For LMSAmiel Francisco ReyesNo ratings yet
- Ni For LMS Chapter 2Document11 pagesNi For LMS Chapter 2Amiel Francisco ReyesNo ratings yet
- NI FOR LMS CHAPTER 3 Computer SoftwareDocument6 pagesNI FOR LMS CHAPTER 3 Computer SoftwareAmiel Francisco ReyesNo ratings yet
- Learning Theories SsDocument3 pagesLearning Theories SsAmiel Francisco ReyesNo ratings yet
- Learning TheoriesstudentsDocument4 pagesLearning TheoriesstudentsAmiel Francisco ReyesNo ratings yet
- Adv of Distance LearningDocument1 pageAdv of Distance LearningAmiel Francisco ReyesNo ratings yet
- Temperature RegulationDocument48 pagesTemperature RegulationAmiel Francisco ReyesNo ratings yet
- OxygenationDocument56 pagesOxygenationHerald Clarence M. AmbayecNo ratings yet
- TutorialsDocument3 pagesTutorialsAmiel Francisco ReyesNo ratings yet
- Activity and ExerciseDocument45 pagesActivity and ExerciseAmiel Francisco ReyesNo ratings yet
- Safety and SecurityDocument44 pagesSafety and SecurityAmiel Francisco ReyesNo ratings yet
- Ni Semifinals Topics 2 COVID 19Document11 pagesNi Semifinals Topics 2 COVID 19Amiel Francisco ReyesNo ratings yet
- Ra 10173Document24 pagesRa 10173Princess Villasis BaciaNo ratings yet
- Literature Matrix Travel BehaviorDocument1 pageLiterature Matrix Travel BehaviorAmiel Francisco ReyesNo ratings yet
- Ni Semifinals Topics 1Document7 pagesNi Semifinals Topics 1Amiel Francisco ReyesNo ratings yet
- Table of The Cognitive Domain (Original)Document8 pagesTable of The Cognitive Domain (Original)Amiel Francisco ReyesNo ratings yet
- BloomrevisedDocument9 pagesBloomrevisedAmiel Francisco ReyesNo ratings yet
- Internal Examination: Course Audit FHC Mid 2Document4 pagesInternal Examination: Course Audit FHC Mid 2Amiel Francisco ReyesNo ratings yet
- BloomrevisedDocument9 pagesBloomrevisedAmiel Francisco ReyesNo ratings yet
- Strat For HealthDocument9 pagesStrat For HealthAmiel Francisco ReyesNo ratings yet
- Health StratDocument11 pagesHealth StratAmiel Francisco Reyes100% (1)
- BloomrevisedDocument9 pagesBloomrevisedAmiel Francisco ReyesNo ratings yet
- R-Difficult ClientsDocument15 pagesR-Difficult ClientsAmiel Francisco ReyesNo ratings yet
- Strat For HealthDocument9 pagesStrat For HealthAmiel Francisco ReyesNo ratings yet
- Health StratDocument11 pagesHealth StratAmiel Francisco Reyes100% (1)
- Oral PathologyDocument184 pagesOral Pathologyyalahopa100% (1)
- Blood PhysiologyDocument39 pagesBlood PhysiologySarmad Laith MortadaNo ratings yet
- Hesi ReviewDocument59 pagesHesi ReviewKrista Howe100% (3)
- Maternal Medical Disorders: SBA QuestionsDocument11 pagesMaternal Medical Disorders: SBA QuestionsBernardo Daniel Lawrencius100% (2)
- Sickle Cell DiseaseDocument8 pagesSickle Cell DiseaseShafieyah ShafiefieNo ratings yet
- Sickle Cell Anemia - SIG 1Document5 pagesSickle Cell Anemia - SIG 1maxNo ratings yet
- Day 1 Am PediaDocument8 pagesDay 1 Am PediaSucceed ReviewNo ratings yet
- Pediatric NursingDocument187 pagesPediatric NursingNorjetalexis Cabrera100% (1)
- Ped Teaching PlanDocument3 pagesPed Teaching PlandionyessNo ratings yet
- Pediatric NursingDocument187 pagesPediatric Nursingirene8000100% (2)
- Classification of The Disorders of Hemoglobin: Bernard G. Forget and H. Franklin BunnDocument13 pagesClassification of The Disorders of Hemoglobin: Bernard G. Forget and H. Franklin BunnMade Oka HeryanaNo ratings yet
- 3 1 - N U M B e R 2 - 2 0 1 1: Official Publication of The Spanish Society of NephrologyDocument117 pages3 1 - N U M B e R 2 - 2 0 1 1: Official Publication of The Spanish Society of NephrologyMahmoud DiaaNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex 1 List of Medical Case RatesDocument111 pagesPhilHealth Circular No. 0035, s.2013 Annex 1 List of Medical Case RatesChrysanthus Herrera80% (5)
- 14 2 PPT - GeneticsDocument24 pages14 2 PPT - Geneticsapi-246719131No ratings yet
- Anestesia en Transplante Renal CMGCDocument51 pagesAnestesia en Transplante Renal CMGCkarlosmgc100% (2)
- Biology - Paper 02 PDFDocument17 pagesBiology - Paper 02 PDFAlexander CorvinusNo ratings yet
- 3 1 GeneticsDocument4 pages3 1 Geneticsapi-287708416No ratings yet
- Genetic DisordersDocument17 pagesGenetic DisordersNgz Krystle ChukwudifuNo ratings yet
- MEDICALLY COMPROMISED Patients in Orthodontics / Orthodontic Courses by Indian Dental AcademyDocument107 pagesMEDICALLY COMPROMISED Patients in Orthodontics / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- GC Sect6 Job DescriptionDocument7 pagesGC Sect6 Job DescriptionMaria Lourdes MacalipayNo ratings yet
- Nclex SampleDocument11 pagesNclex SampleKadijha SingletonNo ratings yet
- Chapter 2 Board ExamDocument20 pagesChapter 2 Board ExamAljohn Galang100% (2)
- ABC: Sickle-Cell Anemia, Shock, PoisoningDocument46 pagesABC: Sickle-Cell Anemia, Shock, Poisoningroneln100% (1)
- Samson HematologyDocument14 pagesSamson HematologyshanyiarNo ratings yet