Professional Documents
Culture Documents
S 0002934307003610
Uploaded by
Natalia Rafael0 ratings0% found this document useful (0 votes)
26 views4 pagesRheumatoid arthritis is a chronic, systemic, inflammatory autoimmune disorder. It afflicts an estimated 25 men and 54 woman per 100,000 population. Early use of disease-modifying antirheumatic drugs and biologics has improved outcomes.
Original Description:
Original Title
s 0002934307003610
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentRheumatoid arthritis is a chronic, systemic, inflammatory autoimmune disorder. It afflicts an estimated 25 men and 54 woman per 100,000 population. Early use of disease-modifying antirheumatic drugs and biologics has improved outcomes.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
26 views4 pagesS 0002934307003610
Uploaded by
Natalia RafaelRheumatoid arthritis is a chronic, systemic, inflammatory autoimmune disorder. It afflicts an estimated 25 men and 54 woman per 100,000 population. Early use of disease-modifying antirheumatic drugs and biologics has improved outcomes.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
OFFICE MANAGEMENT
Rheumatoid Arthritis: Diagnosis and Management
Vikas Majithia, MD,
a,b
Stephen A. Geraci, MD
a,b
a
Department of Medicine, University of Mississippi School of Medicine, Jackson,
b
Medical Service, G.V. (Sonny) Montgomery Veterans
Affairs Medical Center, Jackson, Miss.
ABSTRACT
Accurate diagnosis of rheumatoid arthritis may be difcult early in its course and demands high clinical
suspicion, astute examination, and appropriate investigations. Early use of disease-modifying antirheu-
matic drugs and biologics has improved outcomes but requires close monitoring of disease course and
adverse events. 2007 Elsevier Inc. All rights reserved.
KEYWORDS: Diagnosis; Review; Rheumatoid arthritis; Therapy
Rheumatoid arthritis is a chronic, systemic, inammatory
autoimmune disorder causing symmetrical polyarthritis of
large and small joints, typically presenting between the ages
of 30 and 50 years.
1
The most common inammatory ar-
thritis, it aficts an estimated 25 men and 54 woman per
100,000 population and is responsible for 250,000 hospital-
izations and 9 million physician visits in the US each
year.
1-3
The etiology of rheumatoid arthritis is not fully under-
stood but involves a complex interplay of environmental
and genetic factors. Genetics also play a role in disease
severity. A triggering event, possibly autoimmune or infec-
tious, initiates joint inammation.
2
Complex interactions
among multiple immune cell types and their cytokines,
proteinases, and growth factors mediate joint destruction
and systemic complications.
2
DIAGNOSIS
The diagnosis of rheumatoid arthritis is primarily clinical.
The typical presentation is polyarticular, with pain, stiff-
ness, and swelling of multiple joints in a bilateral, symmet-
ric pattern. A minority of patients present with oligoarticular
asymmetric involvement.
1
The onset is usually insidious,
with joint symptoms emerging over weeks-months and of-
ten accompanied by anorexia, weakness, or fatigue. Patients
usually note morning stiffness lasting more than an hour.
Commonly involved joints are the wrists, proximal inter-
phalangeal, metacarpophalangeal, and metatarsophalangeal
joints, with distal interphalangeal joints and spinal joints
usually spared.
1
Typical examination ndings include
swelling, bogginess, tenderness and warmth of, with at-
rophy of muscles near, the involved joints. Weakness is
out of proportion to tenderness.
Rarely, patients may present with single joint involve-
ment or with severe systemic symptoms of fever, weight
loss, lymphadenopathy, and multiple organ involvement
such as lung or heart.
1
Infection-related reactive arthropathies, seronegative
spondyloarthropathies, and other connective tissue diseases
may have symptoms in common with rheumatoid arthritis,
as may an array of endocrine and other disorders. These
must be excluded in the initial diagnostic evaluation.
1
Table 1
lists some common diseases that should be considered in the
differential diagnosis.
There is no single test that conrms rheumatoid arthritis.
Initial laboratory tests should include a complete blood cell
count with differential, rheumatoid factor, and erythrocyte
sedimentation rate or C-reactive protein. Rarely, joint aspi-
ration also may be required, especially with monoarticular
presentations, to rule out infectious or crystal-induced ar-
thritis. Baseline renal and hepatic function tests are recom-
mended to guide medication choices.
3
Anticyclic citrulli-
nated peptide antibody carries high specicity and positive
predictive value but is present in fewer than 60% of rheu-
Requests for reprints should be addressed to Vikas Majithia, MD,
Division of Rheumatology and Molecular Immunology, Department of
Medicine, University of Mississippi School of Medicine, 2500 N. State
Street, Jackson, MS 39216.
E-mail address: vikasmajithia@medicine.umsmed.edu
0002-9343/$ -see front matter 2007 Elsevier Inc. All rights reserved.
doi:10.1016/j.amjmed.2007.04.005
The American Journal of Medicine (2007) 120, 936-939
matoid arthritis patients.
4
Tests to rule out other disorders in
the differential diagnosis (Table 1) should be performed as
clinically indicated.
The American College of Rheumatology criteria (Table 2)
are helpful in formally diagnosing and following rheu-
matoid arthritis patients in research trials.
5
In the clinical
setting, a denitive diagnosis using these criteria is not
possible in all the cases; they should be used only in com-
bination with all other available information in an individual
case.
KEY POINTS: DIAGNOSIS AND INITIAL
MANAGEMENT DECISIONS
There are 2 questions for the primary care physician when
evaluating a patient with arthritis: Is the diagnosis of rheu-
matoid arthritis likely? Does the patient need early treat-
ment or referral to a rheumatologist, or both? Findings
making rheumatoid arthritis the likely diagnosis and prompting
initiation of treatment are:
Joint swelling (and pain) of 3 or more joints
Metacarpal or metatarsal joint involvement (a positive
squeeze test, ie, signicant pain when squeezed across
these joints)
Morning stiffness lasting more than 30 minutes
Elevated erythrocyte sedimentation rate, C-reactive pro-
tein, and rheumatoid factor
Referral to a rheumatologist is indicated if the diagnosis
is unclear, more than 5 joints or large joints are involved
with accompanying signicant subjective symptoms, or lab-
oratory abnormalities are present.
TREATMENT
A comprehensive approach to managing rheumatoid arthri-
tis consists of patient education, physical/occupational ther-
apy, and drug treatment. Patients should be educated about
the disease and referred to these ancillary specialists to
maintain joint function and delay disability. Drug treatment
generally involves a 3-pronged approach: nonsteroidal anti-
inammatory drugs and low-dose oral or intra-articular glu-
cocorticoids; disease-modifying antirheumatic drugs; and
consideration of biologic response modiers/biologics.
Nonsteroidal anti-inammatory drugs reduce joint pain and
swelling, but do not alter the disease course and should not
be used alone.
3
Steroids (prednisone 10 mg daily or equiv-
alent) relieve symptoms and may slow joint damage;
3
they
should be prescribed at a low dose for short duration, pri-
marily as bridge therapy, and with daily calcium (1500
mg) and vitamin D (400-800 IU) oral supplements to limit
bone demineralization.
3
All patients with rheumatoid arthritis should be evalu-
ated for disease-modifying antirheumatic drugs treatment.
3
Early use slows disease progression and improves overall
long-term prognosis.
3
Although there is consensus among
rheumatologists that rheumatoid arthritis should be treated
early and aggressively, a number of issues (choice of initial
therapy, timing and patient criteria for initiation of combi-
nation therapy, or use of biologics) remain under evaluation.
The following is an approach consistent with the avail-
able evidence. Patients with mild disease (typically 5
joints involved and mild subjective symptoms) and normal
radiographic ndings can receive hydroxychloroquine,
sulfasalazine, minocycline, or possibly methotrexate.
Methotrexate remains the initial treatment of choice in
moderate-severe disease (typically 5 joints or large joint
involvement with signicant subjective symptoms) or ra-
diographic changes of bone loss/erosion. The target dose
(15 mg/week) should be reached within 6-8 weeks if toler-
ated. When response is inadequate, leunomide, azathio-
prine, or combination therapy (methotrexate plus another
agent) may be considered. Combinations of disease-modi-
Table 2 Classication Criteria for Rheumatoid Arthritis*
Morning stiffness (lasting 1 hour)
Arthritis of 3 or more joint areas (areas are right or left
proximal interphalangeal, metacarpophalangeal, wrist,
elbow, knee, ankle, and metatarsophalangeal joints)
Arthritis of hand joints (proximal interphalangeal or
metacarpophalangeal joints)
Symmetric arthritis, by area
Subcutaneous rheumatoid nodules
Positive rheumatoid factor
Radiographic changes (hand and wrist, showing erosion of
joints or unequivocal demineralization around joints)
*At least 4 are needed for diagnosis. Adapted from Arnett et al:
5
Arthritis Rheum. 1988;31:315-324. Copyright John Wiley & Sons, Inc.,
1988, reprinted with permission of Wiley-Liss, Inc., a subsidiary of
John Wiley & Sons, Inc.
Present for 6 weeks.
Table 1 Diseases that Can Mimic Rheumatoid Arthritis
Category Common Examples
Other connective
tissue syndromes
Systemic lupus erythematosus,
Systemic vasculitides,
Scleroderma
Systemic diseases Sarcoidosis, Stills disease, Infective
endocarditis, Rheumatic fever
Spondyloarthropathies Psoriatic arthritis, Reactive arthritis
Infectious arthritis Viral arthritides (esp. Parvo virus),
Bacterial arthritis, Gonococcal
arthritis
Crystal-induced
arthritis
Polyarticular gout
Endocrinopathies Thyroid disorders
Soft-tissue syndromes
and Degenerative
disorders
Fibromyalgia, Polyarticular
osteoarthritis
Deposition disorders Hemochromatosis
Malignancy
(paraneoplastic
syndromes)
Lung cancer, Multiple myeloma
937 Majithia and Geraci RA: Systemic, Inammatory Disease
fying antirheumatic drugs may be more effective than sin-
gle-drug regimens.
3
Women of childbearing age should use
adequate contraception when taking certain (teratogenic)
disease-modifying antirheumatic drugs (Table 3).
Biologics, the latest generation of antirheumatic drugs,
have novel molecular mechanisms that target cytokines,
signaling molecules and cells involved in inammation and
joint destruction. These include the tumor necrosis factor
antagonists: adalimumab, etanercept, and iniximab (rst
line agents); the Interleukin-1 antagonist, anakinra; the
anti-B cell antibody, rituximab; and the down-regulator of
T-cell co-stimulation, abatacept. All biologics are associ-
ated with an increased risk of infection (bacterial, viral, and
fungal) and tuberculosis reactivation. Table 3 lists disease-
modifying antirheumatic drugs and biologic dosing regi-
mens, times to onset of benet, adverse effects, and safety
monitoring.
3
It is important to note that there is disagreement among
rheumatologists about the choice of initial therapy. There is
evidence that combination of methotrexate and a biologic
agent is the most effective current therapy but the short- and
long-term risks, as well as the cost-effectiveness of biologic
agents, are not well dened.
3
Due to these unanswered
questions, common rheumatology practice is to begin meth-
otrexate alone as initial therapy.
Chronic treatment of rheumatoid arthritis is a continuous
process, and periodic patient re-assessment is paramount.
Patients should be evaluated every 2-3 months for control of
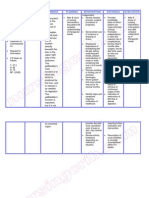
Table 3 Rheumatoid Arthritis Treatment: Disease-Modifying Antirheumatic Drugs and Biologic Agents
Drug Dosage
Onset of
Effect Adverse Events Monitoring
Abatacept 500-1000 mg (weight
based) at 0, 2 and
4 weeks then every
4 weeks
2-12 weeks ISR, infections, hypersensitivity,
COPD exacerbation
Monitor for TB, other infections;
CBC, chemistry and LFTs at
baseline and with each
infusion
Adalimumab 40 mg sc biweekly 2-12 weeks ISR, infections, TBr;
demyelinating disorders (rare)
TB, fungal, other infections; CBC
and LFTs at baseline and then
every 2-3 months
Anakinra 100 mg sc daily 4-12 weeks ISR, leucopenia, infections,
hypersensitivity
CBC at baseline and every 3
months
Azathioprine 50-150 mg po daily 2-3 months GI intolerance, cytopenia,
hepatitis, infections
CBC, LFTs every 2-4 weeks
initially, then every 2-3
months
Cyclosporine 2.5-5 mg po daily 2-3 months GI intolerance, cytopenia,
infections, hypertension, renal
disease
Cr every 2 weeks at initiation,
then monthly; consider CBC,
LFTs, and K
Etanercept 25 mg sc twice/ week
or 50 mg sc weekly
2-12 weeks ISR, infections, TBr;
demyelinating disorders (rare)
TB, fungal, other infections; CBC
and LFTs at baseline and then
every 2-3 months
Hydroxychloroquine 200-400 mg po daily 2-6 months GI intolerance, Retinal toxicity Fundoscopy every 12 months
Iniximab 3 mg/kg at weeks 0,
2 and 4, then
every 8 weeks
2-12 weeks ISR, infection, TBr;
demyelinating disorders (rare)
TB, fungal, other infections; CBC
and LFTs at baseline and then
every 2-3 months
Leunomide 20 mg daily 4-12 weeks GI intolerance, skin rash,
hepatitis, cytopenia; highly
teratogenic
Hepatitis B and C serology in
high-risk patients; CBC, Cr and
LFTs monthly x6, then every
1-2 months; reduce dose or
stop if LFTs elevate
Methotrexate 15-25 mg orally, sc
or IM weekly
1-2 months GI intolerance, oral ulcers,
alopecia, hepatitis,
pneumonitis, cytopenia, rash;
teratogenic
CBC, Cr and LFTs monthly x6,
then every 1-2 months; adjust
dose or stop if LFTs elevate
Minocycline 100 mg twice daily 1-3 months Dizziness, skin pigmentation none
Rituximab 1000 mg at 0 and 15
days
2-12 weeks ISR, infection risk, new and
reactivation viral infections,
respiratory difculty,
cytopenia
Monitor for TB, other infections;
CBC, chemistry and LFTs at
baseline and 2 weeks, every
2-3 months thereafter
Sulfasalazine 2-3 gm daily 1-3 months GI intolerance, oral ulcers,
cytopenia, rash
CBC every 2-3 months
Sc subcutaneous; po orally; imintramuscularly; ISR injection site reaction; CBC complete blood count; LFTs liver function tests;
UA urinalysis with microscopic examination; Cr serum creatinine; TBr tuberculosis reactivation.
938 The American Journal of Medicine, Vol 120, No 11, November 2007
disease activity, extra-articular manifestations, medication
side effects, and functional capacity. Annual hand and feet
radiographs (for joint surface erosions and demineraliza-
tion) also are recommended.
3
KEY POINTS: MANAGEMENT
In managing chronic rheumatoid arthritis, the primary care
physician should assess course (improvement or progres-
sion), net disability, and medication side effects (including
osteoporosis with chronic steroid use). Ongoing surveil-
lance for infection, tuberculosis, and malignancy (age-ap-
propriate screening), osteoporosis and immunizations (in-
uenza vaccine and pneumovax) are essential components
of care. Cardiovascular risk factor reduction is warranted
due to a higher risk for development of coronary artery
disease related to the underlying disease or medications.
SUMMARY
Prompt and accurate diagnosis, early aggressive treatment,
including disease-modifying antirheumatic drugs or biolog-
ics, symptom control, and close monitoring of disease state
and medication toxicity are the keys to effective manage-
ment of the patient with rheumatoid arthritis. Subspecialty
referral should be considered in all patients with moderate-
severe disease or demonstrating incomplete response.
References
1. Harris ED. Clinical features of rheumatoid arthritis. In: Kelleys Text-
book of Rheumatology, 7th ed. Philadelphia, PA: W.B. Saunders; 2005:
1043-1078.
2. Firestein GS. Etiology and pathogenesis of rheumatoid arthritis. In:
Kelleys Textbook of Rheumatology, 7th ed. Philadelphia, PA: W.B.
Saunders; 2005:996-1042.
3. American College of Rheumatology Subcommittee on Rheumatoid
Arthritis Guidelines. Guidelines for the management of rheumatoid
arthritis: 2002 update. Arthritis Rheum. 2002;46:328-346.
4. Van-Gaalen FA, Linn-Rasker SP, van Venrooij WJ, et al. Autoantibod-
ies to cyclic citrullinated peptides predict progression to rheumatoid
arthritis in patients with undifferentiated arthritis: a prospective cohort
study. Arthritis Rheum. 2004;50(3):709-715.
5. Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism
Association 1987 revised criteria for the classication of rheumatoid
arthritis. Arthritis Rheum. 1988;31:315-324.
939 Majithia and Geraci RA: Systemic, Inammatory Disease
You might also like
- Chronic Virus Report of Three Cases Indolent Orofacial Herpes Simplex Infection in Chronic Leukemia: ADocument4 pagesChronic Virus Report of Three Cases Indolent Orofacial Herpes Simplex Infection in Chronic Leukemia: ANatalia RafaelNo ratings yet
- P1D 15 Playground Colors PDFDocument1 pageP1D 15 Playground Colors PDFNatalia RafaelNo ratings yet
- Pagina 324Document8 pagesPagina 324Natalia RafaelNo ratings yet
- 21 CFR 56 Comite de Revision Institucional 1998Document12 pages21 CFR 56 Comite de Revision Institucional 1998Natalia RafaelNo ratings yet
- Enf de Chron GuidelinesDocument11 pagesEnf de Chron GuidelinesNatalia RafaelNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- History TakingDocument4 pagesHistory TakingaliNo ratings yet
- Evaluation & Management CodingDocument14 pagesEvaluation & Management Codingsherrij1025No ratings yet
- Eng PDFDocument45 pagesEng PDFEll TabokomNo ratings yet
- Mod 6 CommunicationDocument43 pagesMod 6 CommunicationAhmad FarooqNo ratings yet
- Community Health NursingDocument2 pagesCommunity Health NursingCharissa Magistrado De LeonNo ratings yet
- English For The Professional NurseDocument12 pagesEnglish For The Professional NurseOryza SativaNo ratings yet
- Hyperemesis Gravidarum: Kelompok 5 Andi Cipta Andi Salma Vadhila Nur Alia Resmi Julita Putri RismayantiDocument7 pagesHyperemesis Gravidarum: Kelompok 5 Andi Cipta Andi Salma Vadhila Nur Alia Resmi Julita Putri RismayantiChayeol ParkNo ratings yet
- Nutrition - Dietetics CpdprogramDocument1 pageNutrition - Dietetics CpdprogramPRC BoardNo ratings yet
- Jason Christopher DecDocument71 pagesJason Christopher DecDave MinskyNo ratings yet
- Health Care Delivery SystemDocument40 pagesHealth Care Delivery SystemBhumika100% (1)
- CITY STAR November 2016 EditionDocument20 pagesCITY STAR November 2016 Editioncity star newspaperNo ratings yet
- JD RBSK DeicDocument2 pagesJD RBSK DeicAjay UpadhyayNo ratings yet
- General Competency Radiology In-Training Test Questions For Diagnostic Radiology ResidentsDocument9 pagesGeneral Competency Radiology In-Training Test Questions For Diagnostic Radiology ResidentsSabinaNo ratings yet
- Health Disparity and Literacy PaperDocument5 pagesHealth Disparity and Literacy PaperlameckwesiNo ratings yet
- Aspects of Early Movement Therapy in Line With The Medical DiagnosisDocument2 pagesAspects of Early Movement Therapy in Line With The Medical DiagnosisHajduGrétaNo ratings yet
- Susarla - Pediatric TraumaDocument1 pageSusarla - Pediatric TraumaRicardo GrilloNo ratings yet
- Pediatric Transplant Rating InstrumentDocument10 pagesPediatric Transplant Rating InstrumentcoxalfonsoNo ratings yet
- HE Teaching PlanDocument6 pagesHE Teaching PlanAiza ToledanaNo ratings yet
- Letter To B.C. Health MinisterDocument3 pagesLetter To B.C. Health MinisterThe Globe and MailNo ratings yet
- Canadanian Jurnal Diabetes PDFDocument342 pagesCanadanian Jurnal Diabetes PDFdyahNo ratings yet
- Ashley M Hannah - Resume 2017Document2 pagesAshley M Hannah - Resume 2017api-358481330No ratings yet
- C CCCCCCCCCCCC C C C CDocument20 pagesC CCCCCCCCCCCC C C C CZandra Kiamco MillezaNo ratings yet
- Arp2017 5627062Document6 pagesArp2017 5627062Syamsi KubangunNo ratings yet
- Nursing Care Plan Cholecystectomy Gall Bladder RemovalDocument2 pagesNursing Care Plan Cholecystectomy Gall Bladder Removalderic100% (16)
- Ambuja Cement Foundation Visit ReportDocument5 pagesAmbuja Cement Foundation Visit ReportRavisinh ValaNo ratings yet
- HHMT Declaration Form Jan 14Document8 pagesHHMT Declaration Form Jan 14api-248499989No ratings yet
- Unit 3 Module Networking TemplateDocument17 pagesUnit 3 Module Networking Templateapi-562162979No ratings yet
- PEJC Prelim X Midterm ReviewerDocument20 pagesPEJC Prelim X Midterm Reviewerjessamae.bucad.cvtNo ratings yet
- Teaching PlanDocument2 pagesTeaching PlanalyNo ratings yet
- Course Code Description Units Pre-Requisite: Obe CurriculumDocument2 pagesCourse Code Description Units Pre-Requisite: Obe CurriculumShyla ManguiatNo ratings yet