Professional Documents
Culture Documents
Archive of SID: Association Between Asthma and Periodontal Disease
Uploaded by
Rizsa Aulia DanestyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Archive of SID: Association Between Asthma and Periodontal Disease
Uploaded by
Rizsa Aulia DanestyCopyright:
Available Formats
A
r
c
h
i
v
e
o
f
S
I
D
Original Article
Association between Asthma and Periodontal Disease
S. Yaghobee
1,2
, M. Paknejad
3
, A. Khorsand
3
1
Assistant Professor, Department of Periodontology, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran
2
Assistant Professor, Dental Research Center, Tehran University of Medical Sciences, Tehran, Iran
3
Associate Professor, Department of Periodontology, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran
Corresponding author:
S. Yaghobee, Department of
Periodontology, School of Den-
tistry, Tehran University of
Medical Sciences, Tehran, Iran.
s_yaghobee@yahoo.com
Received:12 J une 2007
Accepted:24 October 2007
Abstract:
Objective: An association between poor oral health and chronic lung disease has recently
been reported. The purpose of this study was to explore this potential association between
asthma and periodontal disease.
Materials and Methods: This is a descriptive case controlled study. The samples were
selected from patients referred to respiratory disease clinic in a hospital in Tehran, Iran.
The study population comprised of one hundred individuals: fifty asthmatics and fifty
asthmatic controls evaluated for Plaque index (PI), Gingival index (GI), Papillary Bleed-
ing index (PBI), Periodontal Disease index (PDI) and Calculus index (CI). The data were
analyzed by SPSS software.
Results: There were significant differences between asthmatics and non-asthmatic sam-
ples in PI, GI, BOP, and PDI (P<0.01). However, there was no such differences in CI be-
tween the two groups (P=0.084).
Conclusion: The results of the present study support recent published reports advocating a
relationship between respiratory disease and periodontal health status.
Key Words: Asthma; Periodontal Diseases; Oral Health; Periodontal Index
Journal of Dentistry, Tehran University of Medical Sciences, Tehran, Iran (2008; Vol: 5, No.2)
INTRODUCTION
Asthma is a chronic inflammatory disease of
the respiratory system characterized by being
hyper-responsive and episodic, reversible
symptoms of air flow abstraction [1]. The
prevalence of asthma has been increasing
across all age, gender, and racial groups and is
found to be higher among children than adults
[2]. Many cells and cellular elements play a
role in asthma, in particular, eosinophils, T
lymphocytes, neutrophils and epithelial cells.
In susceptible individuals, the inflammation
causes recurrent episodes of coughing, wheez-
ing, chest tightness and difficult breathing, es-
pecially at night and in the early morning;
however, asthma is a disease with many faces
[1].
Periodontal disease has been known as an in-
flammatory disease with a reaction to bacterial
plaque causing chronic inflammation, gingival
bleeding, increasing pocket depth, and ulti-
mately, alveolar bone loss. In fact, bacterial
antigens irritate the immune response of the
host leading to the effects of the disease [3].
As in asthma, the immune response is the
mechanism involved in the pathogenesis and
progression of the disease. Although the dis-
ease is mostly associated with adults, a signifi-
cant portion is seen in children and young
adults as well [3].
One of the effective defense elements of the
oral cavity is saliva including antibacterial,
antiviral, and antifungal actions [4]. In addi-
tion, immunoglobulin and growth factors are
2008; Vol. 5, No. 2
47
www.SID.ir
A
r
c
h
i
v
e
o
f
S
I
D
Journal of Dentistry, Tehran University of Medical Sciences Yaghobee et al.
also found in saliva and mucin, playing a pro-
tective role for the mucosa. Saliva also pro-
motes mineralization of the teeth [5-7]. The
main factor in diminishing the periodontal dis-
ease is the interaction between bacterial and
immunological factors. Thus, saliva affects the
severity of the periodontal disease remarkably
[8]. On the other hand, drugs affecting salivary
secretion, such as the ones used to treat or con-
trol asthma, may negatively influence perio-
dontal health.
One of the most important functions of saliva
is the secretary IgA (SIgA) actively secreted
by the salivary glands [9]. SIgA acts as a first
line of defense for the mucosa and has a major
role in restricting the periodontal disease [10].
On the other hand, in some studies, reduction
of SIgA level in saliva of asthmatics has been
reported [11]. Hyypp depicted that the aller-
gic immunoglobulin, IgE, was elevated in pa-
tients with asthma when compared with the
healthy control group [12].
Although some studies reported that asthmatic
patients had more gingivitis than healthy pa-
tients, others reported no difference in gingivi-
tis prevalence and plaque formation. There is
also a controversy about the amount of calcu-
lus in asthmatics and healthy individuals [13-
17].
In summery, association between asthma and
periodontal disease might involve either patho-
logical activation of the immune and inflam-
matory process, anti asthmatic medications, or
an interaction between them [18,19].
The purpose of the present study was to de-
termine if there is a significant difference be-
tween the periodontal health parameters in
asthmatics when compared to non-asthmatic
individuals.
MATERIALS AND METHODS
This descriptive case-controlled study was per-
formed on 50 subjects referred to asthma clinic
of Tehran Hospital, Tehran, Iran and the con-
trol group (n=50) referred to dermatology
clinic of the same hospital (48 male and 52
female, with the average age of 39.62 and
37.16 years respectively) from 2006 to 2007.
All the subjects in the control group were sys-
temically healthy. The inclusion criteria for the
test group were as follow: no immune-system
disease; not on antibiotics, either systemati-
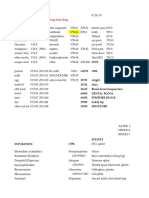
Table 1. Mean and Srandard Deviation (SD) of Plaque Index (PI).
Asthmatic patients Non-asthmatic patients Total
PI (tooth number)
N Mean (SD) N Mean (SD) N Mean (SD)
PI (16) 50 1.42 (0.84) 50 2.34 (0.98) 100 1.88 (1.02)
PI (21) 50 1.20 (0.78) 50 1.54 (1.09) 100 1.37 (0.96)
PI (24) 50 1.40 (0.81) 50 1.86 (1.09) 100 1.63 (0.97)
PI (36) 50 1.56 (0.81) 50 2.32 (0.94) 100 1.94 (0.95)
PI (41) 50 1.38 (0.83) 50 1.86 (1.14) 100 1.62 (1.02)
P1 (44) 50 1.54 (0.86) 50 2.04 (1.24) 100 1.79 (1.09)
N=number
Table 2. Mean and Srandard Deviation (SD) of Periodontal Disease Index (PDI).
Asthmatic patients Non-asthmatic patients Total
PDI (tooth number)
N Mean (SD) N Mean (SD) N Mean (SD)
PDI (16) 50 3.88 (1.02) 50 4.74 (1.32) 100 4.31 (1.25)
PDI (21) 50 3.10 (0.50) 50 3.48 (0.93) 100 3.29 (0.77)
PDI (24) 50 3.78 (0.93) 50 4.62 (1.21) 100 4.20 (1.15)
PDI (36) 50 3.52 (0.84) 50 4.36 (1.06) 100 3.94 (1.04)
PDI (41) 50 3.32 (0.65) 50 3.54 (0.97) 100 3.43 (0.83)
PDI (44) 50 3.34 (0.72) 50 4.08 (1.21) 100 3.71 (1.06)
N=number
2008; Vol. 5, No. 2
48
www.SID.ir
A
r
c
h
i
v
e
o
f
S
I
D
Yaghobee et al. Association between Asthma and Periodontitis
cally or topically, during the last 3 months; no
systemic disease affecting periodontal health;
no smoking habit; and similarity with the con-
trol group in gender, education, economical
and social aspects.
Systemic and dental examinations were per-
formed by calibrated dentists and physicians.
According to the approach described by Hal-
terman et al [20], classification of the presence
and severity of asthma was performed as fol-
lows: two hospitalizations or four asthma-
related acute visits; moderate: one hospitaliza-
tion or two acute visit or three episodes of
wheezing; and mild: no hospitalization, one
acute visit, two episodes of wheezing. All the
samples in the test group suffered from mod-
erate to sever asthma.
Three types of drugs were commonly used by
the asthmatics having xerogenic and anti-
inflammatory effects for more than 24 months:
anti-asthmatic inhaler, anti-histamines, and
corticosteroids.
Periodontal measurements, including Plaque
Index (PI), Gingival Index (GI), Papillary
Bleeding Index (PBI), Periodontal Disease In-
dex (PDI) and Calculus Index (CI), were made
for both the test and the control group. The
data were analyzed using SPSS Software.
RESULTS
The amount of plaque accumulation showed
statistically significant difference (P<0.01) be-
tween the test and the control groups (Table
1). A significant difference in PDI (P<0.01)
was found between the asthmatics and the
non-asthmatics (Table 2).
In addition, the evaluation of PBI and GI in the
two groups showed that there were significant
differences between them (P<0.01) meaning
that gingival inflammation was more seen in
the asthmatics (Table 3 and 4). However, there
was not any statistically significant difference
in CI (P=0.084) between the two groups (Ta-
ble 5).
DISCUSSION
The relationship between asthma and perio-
dontal health has been previously reported by
many authors so far. Considering the inflam-
matory nature of both asthma and periodontal
disease, also the presence of variants and co-
variant affecting the results of such studies,
Table 3. Mean and Srandard Deviation (SD) of Papillary Bleeding Index (PBI).
Asthmatic patients Non-asthmatic patients Total
PBI (tooth number)
N Mean (SD) N Mean (SD) N Mean (SD)
PBI (16) 50 1.38 (0.69) 50 1.96 (0.94) 100 1.67 (0.87)
PBI (21) 50 1.32 (0.62) 50 1.40 (0.72) 100 1.36 (0.67)
PBI (24) 50 1.38 (0.67) 50 1.76 (0.82) 100 1.57 (0.76)
PBI (36) 50 1.46 (0.78) 50 1.98 (0.97) 100 1.72 (0.92)
PBI (41) 50 1.48 (0.78) 50 1.52 (0.81) 100 1.50 (0.79)
PBI (44) 50 1.38 (0.69) 50 1.64 (0.82) 100 1.51 (0.75)
N=number
Table 4. Mean and Srandard Deviation (SD) of Gingival Index (GI).
Asthmatic patients Non-asthmatic patients Total
GI (tooth number)
N Mean (SD) N Mean (SD) N Mean (SD)
GI (16) 50 1.14 (0.86) 50 1.72 (0.78) 100 1.43 (0.89)
GI (21) 50 1.04 (0.88) 50 1.16 (0.91) 100 1.10 (0.89)
GI (24) 50 1.16 (0.82) 50 1.56 (0.97) 100 1.36 (0.92)
G1 (36) 50 1.32 (0.99) 50 1.76 (0.77) 100 1.54 (0.91)
G1 (41) 50 1.30 (0.84) 50 1.30 (0.93) 100 1.30 (0.88)
G1 (44) 50 1.20 (0.92) 50 1.48 (0.95) 100 1.34 (0.95)
N=number
2008; Vol. 5, No. 2
49
www.SID.ir
A
r
c
h
i
v
e
o
f
S
I
D
Journal of Dentistry, Tehran University of Medical Sciences Yaghobee et al.
proving such an association seems equivocal.
In the present study, uniform test and control
groups (gender, age, and socio-economic
status) along with application of standard indi-
ces eradicated the factors, which could have
affected the results.
As the results of the present study showed,
there is a significant difference in PI between
the asthmatics and the non-asthmatics being in
agree with previous studies [14,15]. Hyypp et
al [15] showed that the incidence of gingivitis
and the amount of plaque accumulation were
higher in asthmatic children than non-
asthmatic ones.
A direct relationship between bacterial pneu-
monia and dental plaque has been reported
[21]. As anaerobic bacteria have a remarkable
roll in pneumonia, and while periodontal
pockets can be a very good shelter for living
and growing of such bacteria, the relationship
between periodontal disease and inflammatory
disease of the respiratory apparatus might
seem explainable.
The measurements for PBI and GI indicated
that the incidence of gingivitis was higher
among the asthmatics, confirming the results
of the previous studies [13-15].
The distraction of the periodontium in asth-
matics was found to be higher than in non-
asthmatics according to PDI being was higher
in the test. This finding supported other studies
declaring a higher incidence of attachment loss
(AL) in patients suffering from chronic respi-
ratory disease [21].
Shulman et al [22] reported that there was not
any significant difference in PI, GI, PBI, AL
and CI between asthmatic children and healthy
ones. However, the difference in the number,
age, gender, socio-economic status, education,
and severity of the disease may rationalize the
discrepancies in the results of different studies.
According to the statistical analysis, there was
no significant difference in CI between the two
groups. While some studies in the literature
have reported that the amount of calculus for-
mation in asthmatic children was higher than
in the non-asthmatics [14,17], others have
found no relationship between asthma and the
amount of calculus formation [22].
CONCLUSION
As both periodontal and respiratory diseases
have an inflammatory nature and there are
many factors that can affect their incidence
and severity, achieving acceptable and ex-
plainable results firmly depends on a precise
study design. The results of the present study
support recent published reports advocating a
relationship between respiratory disease and
periodontal health status.
ACKNOWLEDGMENTS
The authors would like to thank and appreciate
Dental Research Center of Tehran University
of Medical Sciences.
REFERENCES
1- Practical Guide for the Diagnosis and Manage-
ment of Asthma, National Heart, Lung, and Blood
Institute, National Institutes of Health. NIH Publi-
Table 5. Mean and Srandard Deviation (SD) of Calculus Index (CI).
Asthmatic patients Non-asthmatic patients Total
CI (tooth number)
N Mean (SD) N Mean (SD) N Mean (SD)
CI (16) 50 0.96 (1.01) 50 1.24 (0.96) 100 1.10 (0.99)
CI (21) 50 0.12 (0.48) 50 0.38 (0.76) 100 0.25 (0.63)
CI (24) 50 0.60 (0.90) 50 0.72 (0.95) 100 0.66 (0.92)
CI (36) 50 0.64 (0.94) 50 1.14 (0.97) 100 0.89 (0.99)
CI (41) 50 1.20 (0.93) 50 1.46 (0.91) 100 1.33 (0.92)
CI (44) 50 0.72 (0.97) 50 0.78 (0.95) 100 0.75 (0.96)
N=number
2008; Vol. 5, No. 2
50
www.SID.ir
A
r
c
h
i
v
e
o
f
S
I
D
Yaghobee et al. Association between Asthma and Periodontitis
cation No. 97-4053, October 1997.
2- Mannino DM, Homa DM, Pertowski CA, Ashi-
zawa A, Nixon LL, J ohnson CA, et al. Surveillance
for asthma--United States, 1960-1995. MMWR
CDC Surveill Summ 1998 Apr;47(1):1-27.
3- Chapple IL. Periodontal diseases in children and
adolescents: classification, aetiology and manage-
ment. Dent Update 1996 J un;23(5):210-6.
4- Levine MJ . Development of artificial salivas.
Crit Rev Oral Biol Med 1993;4(3-4):279-86.
5- Rantonen PJ , Meurman J H. Correlations be-
tween total protein, lysozyme, immunoglobulins,
amylase, and albumin in stimulated whole saliva
during daytime. Acta Odontol Scand 2000 Aug;
58(4):160-5.
6- Seidel BM, Schulze B, Kiess W, Vogtmann C,
Borte M. Determination of secretory IgA and al-
bumin in saliva of newborn infants. Biol Neonate
2000 Oct;78(3):186-90.
7- Ishizaki H, Westermark A, van Setten G, Pyykk
I. Basic fibroblast growth factor (bFGF) in saliva--
physiological and clinical implications. Acta Oto-
laryngol Suppl 2000;543:193-5.
8- Kaufman E, Lamster IB. Analysis of saliva for
periodontal diagnosis--a review. J Clin Periodontol
2000 J ul;27(7):453-65.
9- Brandtzaeg P. Salivary immunoglobulin. In:
Tenovuo J O, editor. Human saliva: Clinical Chem-
istry and Microbiology. Vol 2. Boca Raton, Fla:
CRC Press Inc; 1989.
10- Marcotte H, Lavoie MC. Oral microbial ecol-
ogy and the role of salivary immunoglobulin A.
Microbiol Mol Biol Rev 1998 Mar;62(1):71-109.
11- Ostergaard PA. IgA levels, bacterial carrier
rate, and the development of bronchial asthma in
children. Acta Pathol Microbiol Scand [C] 1977
J un;85(3):187-95.
12- Hyypp T. Gingival IgE and histamine concen-
trations in patients with asthma and in patients with
periodontitis. J Clin Periodontol 1984 Feb;11(2):
132-7.
13- Laurikainen K, Kuusisto P. Comparison of the
oral health status and salivary flow rate of asth-
matic patients with those of nonasthmatic adults--
results of a pilot study. Allergy 1998 Mar;
53(3):316-9.
14- McDerra EJ , Pollard MA, Curzon ME. The
dental status of asthmatic British school children.
Pediatr Dent 1998 J ul-Aug;20(4):281-7.
15- Hyypp TM, Koivikko A, Paunio KU. Studies
on periodontal conditions in asthmatic children.
Acta Odontol Scand 1979;37(1):15-20.
16- Bjerkeborn K, Dahllf G, Hedlin G, Lindell M,
Moder T. Effect of disease severity and pharma-
cotherapy of asthma on oral health in asthmatic
children. Scand J Dent Res 1987 Apr;95(2):159-
64.
17- Wotman S, Mercadante J , Mandel ID, Goldman
RS, Denning C. The occurrence of calculus in
normal children, children with cystic fibrosis, and
children with asthma. J Periodontol 1973 May;
44(5):278-80.
18- Hyypp T. Studies of immunologic and in-
flammatory factors in saliva in patients with
asthma and in patients with periodontitis. J Clin
Periodontol 1981 Dec;8(6):500-7.
19- Ryberg M, Mller C, Ericson T. Saliva compo-
sition and caries development in asthmatic patients
treated with beta 2-adrenoceptor agonists: a 4-year
follow-up study. Scand J Dent Res 1991 J un;99(3):
212-8.
20- Halterman J S, Aligne CA, Auinger P, McBride
J T, Szilagyi PG. Inadequate therapy for asthma
among children in the United States. Pediatrics
2000 J an;105(1 Pt 3):272-6.
21- Scannapieco FA, Ho AW. Potential associa-
tions between chronic respiratory disease and
periodontal disease: analysis of National Health
and Nutrition Examination Survey III. J Periodon-
tol 2001 J an;72(1):50-6.
22- Shulman J D, Nunn ME, Taylor SE, Rivera-
Hidalgo F. The prevalence of periodontal-related
changes in adolescents with asthma: results of the
Third Annual National Health and Nutrition Ex-
amination Survey. Pediatr Dent 2003 May-J un;
25(3):279-84.
2008; Vol. 5, No. 2
51
www.SID.ir
You might also like
- Complementary and Alternative Medical Lab Testing Part 2: RespiratoryFrom EverandComplementary and Alternative Medical Lab Testing Part 2: RespiratoryNo ratings yet
- Diagnosis and Treatment of Chronic CoughFrom EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoNo ratings yet
- Journal 5Document5 pagesJournal 5Nadya PurwantyNo ratings yet
- Acute and Chronic Otitis MediaDocument17 pagesAcute and Chronic Otitis MediaAnnisa KhairunnisaNo ratings yet
- Allergic Rhinitis and Chronic Suppurative Otitis Media: Archives of Oto-Rhino-Laryngology January 2011Document6 pagesAllergic Rhinitis and Chronic Suppurative Otitis Media: Archives of Oto-Rhino-Laryngology January 2011tiaNo ratings yet
- Severity of Allergic Rhinitis and Asthma Development in ChildrenDocument3 pagesSeverity of Allergic Rhinitis and Asthma Development in Childrenanna dianaNo ratings yet
- Epidemiology of Childhood AsthmaDocument4 pagesEpidemiology of Childhood AsthmaAmolkumar W DiwanNo ratings yet
- 23wasan FDocument4 pages23wasan FAshok KpNo ratings yet
- Dissertation ProposalDocument15 pagesDissertation ProposalJitesh SoniNo ratings yet
- Lung Disease Associated with Rheumatoid ArthritisFrom EverandLung Disease Associated with Rheumatoid ArthritisTakahisa GonoNo ratings yet
- The Associations Between Periodontitis and Respiratory DiseaseDocument6 pagesThe Associations Between Periodontitis and Respiratory DiseaseAquila FP SinagaNo ratings yet
- KhfligzdbDocument4 pagesKhfligzdbArdiansyah P PratamaNo ratings yet
- Research: Corticosteroids For Pain Relief in Sore Throat: Systematic Review and Meta-AnalysisDocument7 pagesResearch: Corticosteroids For Pain Relief in Sore Throat: Systematic Review and Meta-AnalysiswindaintanpNo ratings yet
- Ojo Asmra Ilnk Treat y OutDocument6 pagesOjo Asmra Ilnk Treat y OutJulio Juarez MolinaNo ratings yet
- Cross-Sectional Analysis of The Association Between PDFDocument12 pagesCross-Sectional Analysis of The Association Between PDFGhimpu DanielaNo ratings yet
- Clinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareFrom EverandClinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareNo ratings yet
- Association Between Asthma and Cardiovascular DiseaseDocument9 pagesAssociation Between Asthma and Cardiovascular DiseaseAjeng RetnoNo ratings yet
- Effectiveness of 3 Generation Cephalosporin Compare To 3 Generation Cephalosporin - Macrolides For Community Acquired Pneumonia PatientsDocument10 pagesEffectiveness of 3 Generation Cephalosporin Compare To 3 Generation Cephalosporin - Macrolides For Community Acquired Pneumonia PatientslalaNo ratings yet
- Fenotipurile Astmului 2008Document9 pagesFenotipurile Astmului 2008childocNo ratings yet
- s00420-011-0631-x.pdf The association between symptoms and exposure is stronger in dropouts than in non-dropouts among employees in Norwegian smelters: a five-year follow-up study The association between symptoms and exposure is stronger in dropouts than in non-dropouts among employees in Norwegian smelters: a five-year follow-up study The association between symptoms and exposure is stronger in dropouts than in non-dropouts among employees in Norwegian smelters: a five-year follow-up studyDocument7 pagess00420-011-0631-x.pdf The association between symptoms and exposure is stronger in dropouts than in non-dropouts among employees in Norwegian smelters: a five-year follow-up study The association between symptoms and exposure is stronger in dropouts than in non-dropouts among employees in Norwegian smelters: a five-year follow-up study The association between symptoms and exposure is stronger in dropouts than in non-dropouts among employees in Norwegian smelters: a five-year follow-up studyAdi SyahNo ratings yet
- Periodontal Health and Oral Microbiota in Patients With Rheumatoid ArthritisDocument18 pagesPeriodontal Health and Oral Microbiota in Patients With Rheumatoid ArthritisKENZA EL ALAOUINo ratings yet
- Dini Journal NcbiDocument11 pagesDini Journal NcbiDewi PermataNo ratings yet
- Fast Facts: Asthma: Improve patient self-management and drug use, achieve asthma controlFrom EverandFast Facts: Asthma: Improve patient self-management and drug use, achieve asthma controlNo ratings yet
- Differences in Clinical and Laboratory Findings Between Group D and Non-Group D Non-TyphoidalDocument10 pagesDifferences in Clinical and Laboratory Findings Between Group D and Non-Group D Non-TyphoidalBana NanaNo ratings yet
- Jurnal 2Document12 pagesJurnal 2VinaNo ratings yet
- Abstracts COMAPI 2014 IJMSDocument20 pagesAbstracts COMAPI 2014 IJMSfelipetheNo ratings yet
- Jurnal+oma+dr+muslim+sp THT-KLDocument6 pagesJurnal+oma+dr+muslim+sp THT-KLHesti RiksawatiNo ratings yet
- Rheumatoid Arthritis A Single Center Egyptian Experience CorretedDocument11 pagesRheumatoid Arthritis A Single Center Egyptian Experience CorretedSara EhabNo ratings yet
- AR and ComorbiditiesDocument17 pagesAR and ComorbiditiesHeena BhojwaniNo ratings yet
- Jurnal Widi GadarDocument5 pagesJurnal Widi GadarwidiaNo ratings yet
- Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis Ear, Nose, and Throat Description at Acute Stage and After RemissionDocument6 pagesStevens-Johnson Syndrome and Toxic Epidermal Necrolysis Ear, Nose, and Throat Description at Acute Stage and After RemissionElsa Giatri SiradjNo ratings yet
- Impact of Immunoglobulin E and Airway Obstruction On BronchiectasisDocument7 pagesImpact of Immunoglobulin E and Airway Obstruction On BronchiectasisRichie Irvanto CiandraNo ratings yet
- 56 JOE Hypert Peria Cond 2010Document6 pages56 JOE Hypert Peria Cond 2010nurima diyahNo ratings yet
- Devil Lier 2018Document26 pagesDevil Lier 2018risanataliasiburianNo ratings yet
- Occupational Rhinitis Affects Occupational Asthma SeverityDocument4 pagesOccupational Rhinitis Affects Occupational Asthma SeveritySoraia Nogueira FelixNo ratings yet
- Otitis Media in Children Which Phenotypes Are Most Linked To AllergyDocument25 pagesOtitis Media in Children Which Phenotypes Are Most Linked To AllergygekwahyuNo ratings yet
- Treatment Trends in Allergic Rhinitis and Asthma: A British ENT SurveyDocument5 pagesTreatment Trends in Allergic Rhinitis and Asthma: A British ENT SurveymenthariNo ratings yet
- LUPUSDocument43 pagesLUPUSGabriel SciberrasNo ratings yet
- Acute Respiratory Distress Syndrome in Pediatric Intensive Care UnitDocument4 pagesAcute Respiratory Distress Syndrome in Pediatric Intensive Care UnitSasha Hidayat FullNo ratings yet
- DNB - Vol31 - Nosuppl 5 - 786Document6 pagesDNB - Vol31 - Nosuppl 5 - 786Nagib MuhammadNo ratings yet
- The Use of Frequency Scale For The Symptoms of GERD in Assessment of Gastro-Oesophageal Re Ex Symptoms in AsthmaDocument5 pagesThe Use of Frequency Scale For The Symptoms of GERD in Assessment of Gastro-Oesophageal Re Ex Symptoms in AsthmaShahnaz RizkaNo ratings yet
- Antihistamin in OMEDocument4 pagesAntihistamin in OMERahma NovitasariNo ratings yet
- Correlation Between Age and Tonsil Size in Patients With Chronic Tonsillitis at Aek Kanopan DistrictDocument8 pagesCorrelation Between Age and Tonsil Size in Patients With Chronic Tonsillitis at Aek Kanopan DistrictIJRASETPublicationsNo ratings yet
- Asociacin Enfermedad Periodontal EnfermedadessistTmicasDocument7 pagesAsociacin Enfermedad Periodontal EnfermedadessistTmicasNadya PurwantyNo ratings yet
- Bronchial Hyperresponsiveness To Mannitol, Airway Inflammation and Asthma Control Test in Atopic Asthmatic ChildrenDocument8 pagesBronchial Hyperresponsiveness To Mannitol, Airway Inflammation and Asthma Control Test in Atopic Asthmatic ChildrenCalistaParamithaNo ratings yet
- Disfungsi Tuba Eustachius Pada PasienDocument11 pagesDisfungsi Tuba Eustachius Pada PasienHielmy Auliya HasyimNo ratings yet
- JR DK 1Document10 pagesJR DK 1Amadea EmanuelaNo ratings yet
- Journal Homepage: - : IntroductionDocument6 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Polypharmacy in Patients Hospitalised For Acute Exacerbation of COPDDocument4 pagesPolypharmacy in Patients Hospitalised For Acute Exacerbation of COPDpina distefanoNo ratings yet
- Chang Ve Ark. 2013 Occupational Noise Exposure and Incident Hypertension in Men A ProspectiveDocument8 pagesChang Ve Ark. 2013 Occupational Noise Exposure and Incident Hypertension in Men A ProspectivefzehragumussNo ratings yet
- Respiratory ResearchDocument9 pagesRespiratory ResearchSyafitri IstiariniNo ratings yet
- Higiene Oral en Prevención NeumoniaDocument6 pagesHigiene Oral en Prevención NeumoniaNatalia NuñezNo ratings yet
- Effect of Rheumatoid Arthritis On Periodontitis: A Historical Cohort StudyDocument6 pagesEffect of Rheumatoid Arthritis On Periodontitis: A Historical Cohort StudyNadya PurwantyNo ratings yet
- Sinusistis JAMA 2015Document14 pagesSinusistis JAMA 2015IvanCarrilloNo ratings yet
- Gastroesophageal Reflux and Asthma in Children: A Systematic ReviewDocument8 pagesGastroesophageal Reflux and Asthma in Children: A Systematic Reviewcasti21No ratings yet
- Healthcare: Allergic Rhinitis and Laryngeal Pathology: Real-World EvidenceDocument9 pagesHealthcare: Allergic Rhinitis and Laryngeal Pathology: Real-World EvidencePutri Rizky AmaliaNo ratings yet
- SDRA Ventilacion Alta FrecuenciaDocument8 pagesSDRA Ventilacion Alta FrecuenciaDavid Davoas A. SolizNo ratings yet
- Lec 5Document16 pagesLec 5Bassam AlgalalyNo ratings yet
- Coding Jobaid 2016Document100 pagesCoding Jobaid 2016Vinay KumarNo ratings yet
- Posterior Capsular OpacityDocument3 pagesPosterior Capsular OpacityRandy FerdianNo ratings yet
- Principles of Endodontic SurgeryDocument29 pagesPrinciples of Endodontic SurgeryCristina Ene100% (3)
- Algorithm 1 Algorithm 2Document51 pagesAlgorithm 1 Algorithm 2Zimm RrrrNo ratings yet
- (Medical Specialty Board Review) George Williams, Navneet Grewal, Marc Popovich - Anesthesiology Critical Care Board Review (2019, Oxford University Press) PDFDocument217 pages(Medical Specialty Board Review) George Williams, Navneet Grewal, Marc Popovich - Anesthesiology Critical Care Board Review (2019, Oxford University Press) PDFLuís Irajá Nogueira De Sá NetoNo ratings yet
- Journey of The First 1000 Days 25 - 04 - 2018 For Web (Low Res) PDFDocument177 pagesJourney of The First 1000 Days 25 - 04 - 2018 For Web (Low Res) PDFchandraprakash_shuklNo ratings yet
- Anatomy of Womans Sex OrganDocument5 pagesAnatomy of Womans Sex Organsumeer khan63% (8)
- Wikipedia - Adams-Stokes Syndrome (CHECKED)Document2 pagesWikipedia - Adams-Stokes Syndrome (CHECKED)pixoguiasNo ratings yet
- External Review of London Emergency Dept.Document11 pagesExternal Review of London Emergency Dept.The London Free PressNo ratings yet
- White Spot LesionsDocument8 pagesWhite Spot LesionsMicéli Guimarães BlayaNo ratings yet
- The Christian Vansluytman ReportDocument15 pagesThe Christian Vansluytman ReportPearce RobinsonNo ratings yet
- Dental Anatomy and Occlusion NuggetsDocument53 pagesDental Anatomy and Occlusion Nuggetssethrb100% (5)
- RAMOS-BN Drug Study Delivery RoomDocument2 pagesRAMOS-BN Drug Study Delivery RoomLouwella RamosNo ratings yet
- RH Blood Group SystemDocument18 pagesRH Blood Group SystemChristian John Mabalot Carillo50% (2)
- Prolonged LabourDocument36 pagesProlonged LabourQuay Kar Ying100% (3)
- Effects of High Dose Vitamin C Supplementation On Severe Covid19 Patients in The ICU - A Retrospective AnalysisDocument1 pageEffects of High Dose Vitamin C Supplementation On Severe Covid19 Patients in The ICU - A Retrospective AnalysiszipzoinkNo ratings yet
- Preconception Counseling For Thyroid DisordersDocument7 pagesPreconception Counseling For Thyroid DisordersLiya AnjelinaNo ratings yet
- 7 Ps of Service Marketing Apollo HospitalDocument18 pages7 Ps of Service Marketing Apollo HospitalManish ManjhiNo ratings yet
- Engl-1301 - Essay 1Document5 pagesEngl-1301 - Essay 1api-533959157No ratings yet
- Breast Cancer Diagnosed During PregnancyDocument3 pagesBreast Cancer Diagnosed During PregnancyJonny CardenasNo ratings yet
- Narrative Report ShadowingDocument18 pagesNarrative Report ShadowingThriska Ravven Resurreccion100% (1)
- 1 - Overview of Maternal and Newborn Care - 08022014 - PHA RHMPP and NDPsDocument25 pages1 - Overview of Maternal and Newborn Care - 08022014 - PHA RHMPP and NDPsBoj OdejarNo ratings yet
- AppendectomyDocument9 pagesAppendectomyMohsin Chaudhari100% (1)
- Jurnal Bumil Pingsan 3Document4 pagesJurnal Bumil Pingsan 3rina astutiNo ratings yet
- VulvovaginiteDocument17 pagesVulvovaginiteAndreea DanielaNo ratings yet
- Medical Surgical Nursing Assignment - 2Document147 pagesMedical Surgical Nursing Assignment - 2Sonali Sengar0% (1)
- Amenorrhea Ovarian TumorsDocument18 pagesAmenorrhea Ovarian TumorsJeremy ShimlerNo ratings yet
- Case Study 1Document4 pagesCase Study 1api-271668042No ratings yet
- Prenatal Care Routine Full Version 2Document98 pagesPrenatal Care Routine Full Version 2Devendra SonawaneNo ratings yet
- Urodynamics (Aquick Pocket Guide)Document210 pagesUrodynamics (Aquick Pocket Guide)ZICO100% (2)