Professional Documents
Culture Documents
Output 1 Electrolytes
Uploaded by
allanrnmanaloto0 ratings0% found this document useful (0 votes)
45 views31 pagesReport on Electrolytes (MAN)
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentReport on Electrolytes (MAN)
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
45 views31 pagesOutput 1 Electrolytes
Uploaded by
allanrnmanalotoReport on Electrolytes (MAN)
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 31
1 | P a g e
La Consolacion University Philippines
(formerly University of Regina Carmeli)
Graduate School Department
Name: Allan M. Manaloto, RN Professor: Dr. Amelia Sta. Maria
Subject: Advanced Pathophysiology Date: November 09, 2013
F L U I D & E L E C T R O L Y T E
A N D A C I D B A S E B A L A N C E
Learning Objectives:
I. Describe the regulation of fluid & electrolyte, & acidbase balance in the body,
including the mechanism involved to maintain homeostasis.
II. . Identify factors affecting normal body fluid, electrolyte, and acidbase balance.
III. Discuss the risk factors for and the causes and effects of fluid, electrolyte, and
acidbase imbalances.
IV. List the major electrolytes and the function of each.
V. Identify the signs and symptoms of the common fluid and electrolyte imbalances.
VI. Teach clients measures to maintain fluid and electrolyte, Acid-base balance.
I. I N T R O D U C T I O N
The cells of the body live in a fluid environment with an electrolyte and acid-
base concentration maintained within a narrow ranged. Fluid and electrolyte,
2 | P a g e
Acid-Base Balance is the foundation for understanding many different disease
processes. Changes in Electrolyte concentration affect electrical activity of nerve
and muscle cells, altered Acid-Base balance disrupted cellular functions, and fluid
fluctuation affects blood volume and cellular function.
II. CONCEPT OF FLUIDS
1. Functions:
1. Move electrolytes and water into and out of the cells.
2. Aid digestion.
3. Cleanse body of waste.
4. Regulate body temperature.
5. Lubricate joints and mucous membrane.
The distribution and amount of Total Body Water (TBW) change with age,
and although daily fluid intake may fluctuate widely, body regulates water volume
within a relatively narrow range. Total body Water (TBW) is the sum of fluids within
all body compartments.
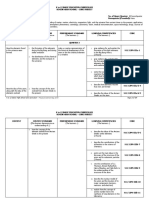
Individual TBW Condition Effect
Newborn/ Infant About 75-80% of
body weight
-Greater body surf. area
-Renal: Not yet matured
Prone to Dehydration
Children/
Adolescents
60-65% of body
weight
Men- Increase muscle
mass= greater % of TBW
Women- more fat, lesser
body fluid.
Women are more
prone to Dehydration
due to fat (fats has
tiny amount of water)
3 | P a g e
Adult Range 45-75%
(Ave. 60%)
Varies on individual
2. Regulation of Body fluids
Fluids and solutes move constantly within the body. That movement allows body
maintains HOMEOSTASIS.
Body Fluids
Intracellular Fluid (ICF):
>Fluids within Cell
>2/3 of TBW
Extracellular Fluid (ECF)
>Fluids outside cell
>1/3 of TBW
Interstitial Fluid
>space between cells &
outside the blood
vessel. Bathes the cell.
Intravascular Fluid
>blood plasma
4 | P a g e
A. Membrane Transport: Cellular I & O
Cell continually take in nutrients, fluids and chemical messenger from the
extracellular environment and expel metabolites.
Passive Transport
- Water and small electrically uncharged molecules moves easily
through pores of plasma membrane. No need for energy
expenditure cell.
- DIFFUSION: natural tendency of substance to move from area of
higher concentration to one of lower concentration.
- FILTRATION: it is the movement of the water and solutes
through membrane because of a greater pushing pressure on
one side of membrane than the other. (Area with greater
Hydrostatic pressure to area with lower Hydrostatic pressure.)
5 | P a g e
- OSMOSIS: movement of water across semi-permeable
membrane from region with higher water concentration to lower
water concentration.
Osmotic pressure -the amount of hydrostatic pressure required
to oppose the osmotic movement of water
Oncotic pressure- is the osmotic pressure exerted by proteins.
Active tranpsort
- Sodium moving out and Pottasium moving into the cell uses the
direct energy of ATP.
- SODIUM- POTTASIUM PUMP: is located in cell membrane and
actively moves Sodium from the cell to the ECF.
6 | P a g e
3. Fluid Intake and Losses (per day in a healthy adult)
INTAKE OUTPUT
Ingested: 1300ml Urine: 1500ml
Water in foods: 1000ml Stool: 200ml
Oxidation: 300ml Insensible Lung: 300ml
Skin: 600ml
TOTAL GAIN= 2,600ml TOTAL LOSS= 2,600ml
Abnormal fluid loss:
Results from physiology imbalance, Examples: Fever,Increased body
temperature, Hemorrhage, emesis, exudates, diaphoresis, thoracentesis.
Quick way to monitor fluid balance is to: Monitor I &O.
4. Homeostatic mechanism
Organs to remember in maintaining fluid and elctrolyte balance:
C.1. Kidneys
- filter 170L of plasma everyday (Adult), excreting only 1.5L of urine.
- It only takes 20mins of poor perfusion to promote Acute Tubular
Fluid Loss
Sensible:
-sweat, feces
Insensible
-Kidney, GIT,
Lungs, Skin
7 | P a g e
Necrosis if not recognzed.
C.2. Heart and Blood Vessels
- pumps & carries fluids to organs, esp. kidneys.
C.3. Lungs
- everytime you exhale, water is lost (vapor). Client who experience
rapid breathing (e.g anxiety) may need increase fluids to maintain
Homeostasis.
C.4. Pituitary
- Hypothalamus- posterior pituitary gland secretes ADH. ADH is a water
conserving hormone (causes water retention).
C.5. Adrenal Gland
-secretes Aldosterone (mineralocorticoid, a volume regulator) in which
Result in Sodium retention= Water retention and Pottasium loss.
C.6. Parathyroid Gland
-secretes PTH that causes increase calcium serum by pulling it from
Bones and placing into blood.
C.7. Other Mechanism
-Baroreceptor: responsible for monitoring circulating blood volume.
-Renin-Angiotensin-Aldosterone System (RAAS)
-Anti-Diuretic Hormoe (ADH)
-Osmoreceptors
-Atrial Natriuretic peptide (ANP)
8 | P a g e
5. Case Considerations
1. Burned Client
- adequate albumin needed to hold fluid in the vessels may not exist.
Therefore, fluid may leak out of the blood vessel into the tissues that can lead to
shock.
-these client looks: they are in fluid volume excess because of swollen tissues
due to fluid accumulation in tissues and interstitial fluid.
2. Diabetic Client
-when blood has too many glucose/ sugar particles, it causes particle-induced
diuresis. (resulting in fluid loss that can lead to hypovolemia)
3. Gerontologic Client
-Decreased cardiac, kidney, lung function, decreased muscle mass that
increases them a risks of fluid and electrolyte imbalances.
-Dehydration may present as confusion, cognitive impairment
-Monitor I and O accurately.
6. Fluid Volume Disturbances
Hypovolemia: Fluid Volume Deficit
Dehydration: loss of water alone, with increase Sodium level.
9 | P a g e
Fluid Volume Deficit (FVD)/ hypovolemia: occurs when water and electrolytes
are lost in the same proportion. Sodium and water are lost in equal amounts from
the vascular space.
Causes -Decrease intake/ poor appetite, tube feedings,
-Drugs affecting fluid and electrloytes (Ex. Diuretics)
-Diuresis (Diabetes insipidus, Addisons disease)
-Vomiting, diarrhea, GI suction, hemmorhage
Signs & Symptoms -Acute weight loss -Postural hypotension
-Decrease skin turgor -Weak, rapid pulse; Decrease BP
- Increase RR and Urine SG
Diagnosis -BUN: is elevated and out of proportion to Serum Creatinine
-Serum Electrolytes, Urine SG ang Hg & Hct (increased)
Complications -Shock! - Cogestive heart failure
-Poor Organ perfusion that may lead to ATN and Real Failure
Medical
Management
1. Acute and Severe loss- IV route is required.
2. Intavenous Solution (Isotonic): Lactated Ringer,and 0.9NaCl
because they expand plama volume.
3. Accurate and frequent assessment of LOC, I & O, Skin, CVP,
Weight, and VS.
Nursing
Management
1. Moitor and measure I & O accurately.
2. Weigh client daily.
3.Observe for weak, rapid pulse.
4. Inspect Skin turgor (thigh, forehead and sternum) and Tongue
10 | P a g e
(may become smaller bec. of fluid loss) regularly.
Hypervolemia: Fluid Vloume Excess
Fluid volume excess (FVE): is the expansion of the ECF caused by abnormal
retention of watera and sodium. Isotonic overhydration.
Causes -diminished fuction of homeostatic mech. Eg.: Heart failure, Renal
failure, liver cirrhosis.
-excessive amout of salt consumption
-Medication: Steroids; Albumin infusion; Blood product admin.
Signs & Symptoms -Jugular vein distention, bounding pulse, tachycardia
-Abnormal breath sounds (fluid collect- lung)
-Polyuria, Dyspnea, Edema- weight gain
-Increased BP and CVP
Diagnosis -Decreased hemoglobin & Hct, Decreased Sodium electrolytes
-BUN and Crea: Increased means kidney not functioning properly
and not excreting fluid.
Medical
Management
1. Management is directed at the cause. (eg. Excessive sodium
admin- discontinue infusion).
2. Pharmacologic: Diuretics
Thiazide (Hydrochlorothiazide;Metozalone)
-for mild to moderate hypervolemia
-blocks sodium reabsoption at distal tubule
11 | P a g e
Loop Diuretic (Furosemide, Bumetanide, Torsemide)
-for severe hypervolemia
-block sodium reabsorption in loop of henle
3. Nutritional Management: mild sodium restriction to 250mg/day.
Drink distilled water.
Nursing
Management
1. Measure I & O and Body weight.
2. Assess breath sounds.
3. Assess edema: feet, hands, and sacral area.
III. CONCEPT OF ELECTROLYTES
Electrolytes are elements that, when dissolved in water, acquire an electrical
charge. Cations are positively charged (Sodium, Calcium, Pottasium, Magnesium
and Hydrogen ions), Anions are negatively charged (Chloride, Phosphate,
Bicarbonate, and Sulfate).
Functions of electrolytes:
-Water distribution
-acid-base balance
-transmit nerve impulses
Abnormal Electrolyte losses:
-Vomiting
-NG Suctioning
-Drainage (wounds)
12 | P a g e
-Diarrhea, Diuretics
Causes of Excess electrolyte in blood:
-Kidney trauma/ disease
-Massive blood transfusion
-Crushing injuries/ chemotherapy
Note: Standard treatment to client with Fluid and Electrolyte imbalances- IV therapy.
1. SODIUM
Values >Normal Adult level: 135-145mEq/L.
>90% of ECF Cations (Chief electrolyte in the ECF is
Sodium).
Functions along with Anions (Chloride and Bicarbonate) they
regulate osmotic forces and therefore regulate water
balance.
assist generation and transmission of nerve impulses.
assist in Sodium-Potassium pump in cell membrane.
regulates osmolality.
Food Sources bacon, ham, cheese processed, catsup, mustard, relishes,
canned vegies
bread, cereals, snack food
Concept >Excretion of Sodium retains Potassium. Sodium is the only
electrolyte affected by water. Sodium level decreases when
there is high amount of water in the body, while sodium level
13 | P a g e
decreases when there is little amount of water in the body.
Regulation >Sodium is regulated by ADH, Thirst, and RAAS system in
the body.
SODIUM IMBALANCES
HYPERNATREMIA HYPONATREMIA
Value Sodium level >145 mEq/L Less than 135mEq/L
Causes Acute Sodium gain: Infection,
Renal failure, High Na Intake
Net loss of Water:
Hyperventilation, watery diarrhea,
DI, Polyuria
Not enough sodium in ECF or too
much water diluting the blood.
Inadequate Intake, Diuresis,
Diaphoresis, Diarrhea, SIADH
Signs/
Symptoms
Dry, sticky mucus membrane,
swollen tongue, decrease saliva
Change in LOC, Tachycardia,
decreased heart contractility
Poor skin turgor, dry mucosa,
abdominal cramping
Neuro changes: altered LOC,
cerebral edema, Coma
Anorexia, exhaustion
Diagnosis Serum Elec (Increase Na)
Increase urine SG,
decreased CVP
Decreased serum sodium, and
Urine SG
Treatment 1. Determine first the cause of
Hypernatremia.
2. Restrict all forms of Sodium
1. Key is assessment. (
Decreased Intake/ Increased Na
loss?, Excessive water in
14 | P a g e
3. Infuse hypotonic Electrolyte
solution (e.g. 0.3 NaCl)
vascular?)
3. Sodium Replacement. IVF-
LRS or Isotonic saline.
4. Water restriction
Nursing
Management
1. Carefully monitor fluid I & O.
2. Take note of pts thirst,
elevated temp, and history of
meds taken.
3. Monitor chages in behavior.
1. Early detection and treatment.
2. Monitor fluids and body wt
3. Note abnormal losses of Na or
gains of water, GI manifestation
and CNS and monitor serum Na.
4. Encourage foods high in
Sodium, if applicable. And Restrict
fluid intake.
2. POTASSIUM
Values >Normal Adult level: 3.5-5.0 mEq/L.
>98% of bodys potassium is inside cell. (ICF)
Functions skeletal and smooth muscle cotraction.
transmission of electrical impulses.
Note: Sodium and Potassium are inversely related: if one
is up, the other is down. Stomach contains large amount of
potassium.
Food Sources peaches, bananas, apricots, oranges, melons, raisins,
prunes, brocolli, potatoes, meat, milk
15 | P a g e
processed foods, whole grains, dairy products
POTASSIUM IMBALANCES
HYPERKALEMIA HYPOKALEMIA
Value Serum potassium >5.0 mEq/L Less than 3.5 mEq/L
Causes Decreased renal excretion of
kidney, Burns, tissue damage
Meds: KCL, Heparin, ACE
inhibitors, Captopril, NSAID
Acidosis
Reduce intake, GI loss- vomiting,
diarrhea, GI suction
K-losing diuretics, altered Acid-
base, Meds- Corticosteroids,
amphotericin B, Kidney disease,
Alkalosis
Signs/
Symptoms
Begins with muscle twitching,
hyperactive muscles with tingling
and burning sensation
Progress to numbness around
the mouth, weakness and flaccid
paralysis.
Diarrhea, Cardiac arrythmia
(mild losses are asymptomatic)
Sever hypoKalemia: may lead to
death due to heart/ respi failure
Cramps first then, muscular
weakness and flaccid paralysis,
hyporeflexia
Slow, DOB, weak and irregular
pulse, decreased LOC, N/V.
Diagnosis ECG: Peaked T-wave, Flat or
no P-wave, wide QRS complex
Increased serum K, ABG
ECG: flat/inverted T-wave, ST
segment depression, elevated U-
wave.
16 | P a g e
metabolic acidosis. Decreased serum K.
Treatment 1. Emergency pharma: give IV Ca
gluconate- to antagonize the
adverse heart conduction. (If BP
and HR drops, STOP the
infusion).
(IV) Regular Insulin- shift
potassium into cells.
Sodium bicarb- needed to
alkalinize the plasma and cause
temp. potassium shift to cells.
1. Admin of 40-80 mEq/L of K/day.
(IV route: KCL, K+ acetate).
2. Potassium should be admin
only after adequate urine flow.
Decreased urine vol (less 20ml/hr)
for 2 consecutive hours is an
indication to stop K+ admin.
NOTE: Admin of Potassium (max.
conc.) is 20mEq/L and rate no
faster than 10-20 mEq/L.
Potassium is NEVER admin by IV
push or IM.
Nursing
Management
1. Observe signs of muscle
weakness and dysrhythmias.
2. Always verify increase/
abnormal result of serum K.
3. Adhere to Potassium
restriction.
Foods low in K: butter, margarine,
sugar, cranberry juice, jellybeans,
honey, hard candy, root beer.
1. Monitor ECG and S/sx of K
deficit.
2.Health teachings on Potassium
rich foods.
17 | P a g e
3. CALCIUM
Values >Normal Adult level: 9.0-10.5 mg/dL
>more than 99% of bodys calcium is in skeletal system
Functions needed for vit. B12 absorption, acts like SEDATIVE on
muscle, nerve impulse transmission, blood clotting, muscle
contraction and relaxation.
promotes strong bones and teeth.
Inverse relatioship with Phosphorus.
Food Sources milk, cheese, dried beans, canned salmons , sardines
fresh oysters, green leafy vegetables
Concept >As Ionized Serum Ca decrease- PTH is secreted by
parathyroid gland and thus, Increased Ca absorption of GIT,
Increased reabsorption from renal tubule, & releases Ca
from the bone.
CALCIUM IMBALANCES
HYPERCALCEMIA HYPOCALCEMIA
Value Calcium level >10.5 mg/dL Less than 9.0mg/dl
Causes Hyperparathyroidism,
Immobilization, Increase Ca and
vit. D Intake, Thiazide diuretics
primary
hypoparathyroidism/surgical,
radical neck dissection, inflammed
pancreas Vit D consumption is
18 | P a g e
inadequate and Mg def.
Alcohol abuse, Meds (caffeine,
corticosteroids, Loop diuretics)
Signs/
Symptoms
Reduced neuromuscular
excitability, decrease tone in
smooth and striated muscle
(weakness, incoordination,
constipation, anorexia)
Decreased DTR, decreased
bowel sounds and respi arrest
(sedates respi muscle)
Late heart changes: decrease
pulse ad lead to cardiac arrest.
TETANY- tingling sensations
(tip of fingers, around mouth),
spasm of muscles of
extremities/face.
Trousseaus sign- elicited by
inflating BP cuff in upper arm-
causing carpal spasm: adducted
thumb, flexed wrist, extended
interphalangeal joints.
Chvosteks Sign- facial nerve is
tapped about 2cm anterior to
earlobe, result: twitching of
muscles of facial nerve.
Increased irritability of CNS-
19 | P a g e
seizures, Dyspnea, mental
changes (depress, hallucination)
Diagnosis Serum Ca (increased)
X-ray (osteoporosis/ kidney
stones), ECG- arrythmias
ECG: QRS complex widen,
prolonged ST interval, prolonged
QT interval.
Treatment 1. Pharmacologic
IV NaCl: dilute serum Ca
Furosemide (Lasix): diuresis w/
Ca excretion
Calcitonin- icrease bone
resorption and urinary Ca
excretion
1. Acute symptomatic is life
threatening: Admin IV Ca
gluconate, Ca Chloride
-too rapid admin causes heart
arrest
-dagerous to pt having digitalis
derive meds
-inspect IV site for extravasation.
2. Vit D Therapy
Nursing
Management
1. Monitor ct at risk.
2. If pt takes Digoxin, assess for
toxicity. Encourage ambulation.
3. Take safety/seizure precaution.
4. Force fluid with high acid-ash
concentration (cranberry juice).
1. Severe Hypocalcemia: WOF
seizure precaution and monitor
airway.
2. Osteoporosis pt- health
teachings of food.
4. MAGNESIUM
Values >Normal Adult level: 1.3-2.1 mEq/L
20 | P a g e
Functions acts directly @ myoneural junction
present in bone, heart, nerves, and muscle tissues
assist metabolism CHO & CHON, maintain electrical
activity in nerves and muscle. Acts like a sedative on
muscle.
Food Sources vegetables, nuts, fish, peas, whole grains
legumes, cocoa, peanut butter, seeds, seafoods
MAGNESIUM IMBALANCES
HYPERMAGNESIMIA HYPOMAGNESIMIA
Value Magnesium level >2.1 Eq/L Less than 1.3 mEq/L
Causes Renal Failure- kidney unable to
excrete Mg, Pt with untreated
DKA, Excessive antacid use, use
of laxatives and MOM.
chronic alcoholism (most
common), diuretics, diarrhea, GI
losses and Meds (digitalis,
cisplatin)
Signs/
Symptoms
mild hyperMg: decreased BP,
N/V, weakness, facial flushing
Increase Mg conc: lethargy,
difficulty speaking, drowsiness,
DTR lost, muscle weakness.
if more than 10mEq/L=Respi
Depress.
(Increased Mg=Sedative)
Neuromuscular changes:
hyperexcitability with muscle
weakness, tremor, tetany,
laryngeal stridor, muscular spasm
cardiac changes: prolonged
QRS, depressed ST segment
marked mood alterations
(Apathy, depression, agitation,
21 | P a g e
ataxia, insomnia)
Hyperactive DTR
Diagnosis Serum Mg (more than 2.5
mEq/L), Increased Potassium and
Ca are present concurrently
ECG: Tall T-waves, widened
QRS, Prolonged PR interval.
Serum elec (decreased Mg),
ECG, Urialysis
Treatment 1. Avoid admi of Mg to pt with RF.
2. Emergency: Respi distress-
ventilate pt, if heart conduction is
defective-give IV Ca gluconate.
2.Admin Loop diuretic (lasix) &
NaCl or LR (IV) to enhance Mg
excretion.
1. Mild Mg Def-Tx with diet alone
(oral admin of Mg salts)
2. IVF: Mg Sulfate-Assess BP,
Heart ryhthm, Respi distress,
Notify MD if Urine output is less
than 100ml for 4hrs.
Nursing
Management
1. Monitor VS, noting pt
hypotension and shallow RR.
2.Assess for decrease patellar
reflexes and chage in LOC.
1. Monitor pt receiving digitalis.
2.If severe hypomagnesia-seizure
precaution.
3. Dysphagia is present-test
swallowing first before giving
water.
4.Assess DTR and give health
teaching on Diet.
22 | P a g e
4. PHOSPHORUS
Values >Normal Adult level: 2.5 to 4.5 mg/dl (had inverse
relationship with calcium).
Functions essential for RBC and muscle function, formation of
ATP.
assist with CHO,CHON, and fat met.
Food Sources milk and mlik products, organ meats, nuts, fish, kidneys
sardines, poultry, whole grains, dried fruits
PHOSPHORUS IMBALANCES
HYPERPHOSPHATEMIA HYPOPHOSPHATEMIA
Value Phosphorus level >4.5 mg/dL Less than 3.0mg/dl
Causes RF, Increased intake, decreased
output, chemo, DKA
Admin of calories to pt with
severe protein-calorie malnutrition
Malnourished pt
Pain, heat stroke, prolonged
intense hyperventilation
Alcohol withdrawal, hepatic
encephalopathy
Signs/
Symptoms
due from decreased Ca levels:
Tetany
ATP def.-impairs cellular energy
resources (impairs Oxygen
delivery to tissue.
23 | P a g e
Neurologic: fatigue, irritability,
weakness, paresthesia, confusion,
seizure, diplopia, dysphagia
Hypoxia (Increased RR, Respi
alkalosis)
Diagnosis Serum phosphorus, X-ray
Serum Elec, X-ray (bone
becomes brittle and weak)
Treatment 1. Treat underlying cause.
2.Admin Vit D prep (Calcitrol) to
increase Ca=decrease Phosphate
3. Admin Phosphate binding gels
(may lead to high Ca levels).
4. Restricted phosphorus diet.
1. Possible dangers of IV admin of
phosphorus include tetany from
hypocalcemia and calcifications
from tissue.
2. Rate of IV should not exceed
10mEq/H
Nursing
Management
1. Avoid phosphate-containig
subs. (enema and laxative)
1. Assess for Hyper/Hypo
calcemia, and Health teaching on
diet.
IV. CONCEPT OF ACID-BASE BALANCE
Power of Hydrogen: Normal pH range: 7.35-7.45
-the more Hydrogen ions=more acidic the solution=Lower pH
-the lower Hydrogen ions=more basic the solution=Higher pH
24 | P a g e
Major Organs involved in regulating Acid-Base balance: Bones, Lungs and
Kidneys.
NOTE:
Major LUNG chemical is= Carbon Dioxide
Major KIDNEY chemicals are= Bicarbonate (HC03) and Hydrogen ion.
Respiratory Acidosis/ Alkalosis
>the problem is the Lungs.
If the Lungs are sick (retained too much
C02), the kidney compensates by
kicking HC03 into the blood and
excreting hydrogen ion out of the body.
If lungs rids of too much C02
(Hyperventilation), the kidney
compensate by retaining Hydrogen Ion
and excreting HC03.
Metabolic Acidosis/ Alkalosis
>Problem is the kidney.
If the kidney malfunction, the Lungs will
compensate (quickly)- C02 is
excreted/retained.
1. BUFFER SYSTEM
Buffer occurs in response to changes in Acid-Base balance. Act by removing or
releasing Hydrogen ions (quickly).
Hydrogen ion= Acid
Bicarbonate= Base
25 | P a g e
a. Carbonic Acid-Bicarbonate Buffering
b. Protein Buffering
c. Renal Buffering
NOTES:
the only way CO2 can build up in the blood is significant decrease in respiration.
the brain likes to the body pH to be perfect all the time. When pH gets out of
whack= Neuro and LOC can occur, therefore monitor them.
Arterial Blood Gas: Normal Values
pH Hydrogen ion concentration 7.35-7.45
PCO2 Partial pressure carbon dioxide 35-45mmHg
PO2 Partial pressure Oxygen 80-100mmGHg
HCO3 Bicarbonate 22-26mEq/L
Metabolic Acidosis Metabolic Alkalosis
Concept charac. by low pH and low
plasma HCO3 concentration.
pH: less than 7.35
HCO3 less than 22mEq/L
charac. by high pH and
high plasma HCO3 conc.
pH: more than 7.45
HCO3 more than 26mEq/L
Causes DKA, malnutrition, starvation
Shock, kidney illness
Diarrhea, ASA overdose
Drugs (Diamox, Aldactone)
vomiting; NG suctioning
Excess antacid ingestion
BT, NaHCO3 admin
Drugs (Thiazide & Loop
26 | P a g e
diuretic), Baking soda,
HypoK, steroids.
Signs and
Symptoms
hyperKalemia: if Hydrogen
ion builds up in
blood=Potassium goes out of
the cell. (Muscle twitching, oral
numbness, weakness)
Kussmauls Breathing: Deep
and rapid-CO2 is blown off in
high amount.
Early: Headache and
lethargylate is Comatose.
Chronic Renal Failure Pt
-chronic metabolic acidosis
(asymptomatic).
(related to decreased Ca)
Tingling of fingers and toes,
dizziness, tetany
Depress RR, HypoK
Hepatic Encephalopathy
(due to ammonia)
Diagnosis ABG: pH less than 7.35;
HCO3 less than 22 mEq/L
PCO2 less than 35mmhg
(compensates)
Serum elec (high potassium)
ABG: pH more than 7.45;
HCO3 more than 26 mEq/L
PCO2 normal but increases
with compensation.
Medical
Management
1. Admin Sodium Bicarb (use
only in quick, temporary basis)
2. In chronic cases= treat first
1. Admin NaCl fluids.
2. Admin Ammonium Cl (IV)
3. Admin Acetazolamide
27 | P a g e
low Ca serum. (Diamox).
Nursing
Management
1, Monitor ABG, HyperK,
Arryhthmia, HyperCa.
2. Closely monitor LOC.
3.Admin IVLR to increase base
level.
1. Monitor ABG, LOC, RR,
hypotension, DTR.
28 | P a g e
Respiratory Acidosis Respiratory Alkalosis
Concept due to inadequate CO2
excretion (Hypoventilation).
pH: less than 7.35
PCO2 more than 45mmhg
HYPERCAPNIA: build up of
CO2 in the blood to more than
45mmhg.
If PaCO2 is chronically more
than 50mmhg, the respi center
is insensitive to CO2 as respi
stimulant. Therefore Admin of
O2 may remove the stimulus of
Hypoxemia and pt develops
CO2 narcosis.
always caused by
hyperventilation.
pH: more than 7.45
PCO2 less than 35mmhg
HYPOCAPNIA: occurs when
CO2 is low; stimulates ANS
which causes: Anxiety,
tingling sensation and
sweating.
Causes Respi arrest, Airway
Obstruction, Brain trauma
Collapsed lung, weak respi
muscle, surgical incision
sleep apnea, excessive
alcohol intake, narcotics,
sedatives
Hysteria/ Anxiety
(Increased RR)
ASA overdose; Pain; Fever
Sepsis ,Anemia
Signs and Sudden: Increased RR Bp,& Vasoconstriction/
29 | P a g e
Symptoms PR, (Pt is breathing too shallow,
too slowly or nothing at all)
Excess acid=Brain vasodilate
(Head fullness feeling, mental
cloudiness, Increased ICP,
brain swelling and decreased
DTR.)
Acidic urine, Arrhythmias
Chronic Respi Acidosis
-present in pt with chronic
emphysema, bronchitis, &
obesity
decreased cerebral blood flow
(inability to concentrate and
lightheadedness)
Decreased Calcium
(numbness and tingling
sensation)
Increased RR, rapid pulse
HypoK
Diagnosis ABG: pH less than 7.35;
HCO3 normal until kidney
compensates
PCO2 more than 45mmhg
PO2 less than 80mmhg
ABG: pH more than 7.45;
HCO3 normal until kidney
compensates
PCO2 less than 35mmhg
Management (Goal: CT blow off excess CO2)
1. Treat the cause.
2. Airway Clearance.
3. Mechanical ventilation with
PEEP.
4. Admin Drugs to open airways
1. Treat the cause.
2. Monitor VS esp RR,
electrolytes, and ABG.
3. Calm the patient. Admin
anti-anxiety.
Have the client breath into a
30 | P a g e
and thin out secretions.
5. Increase fluids; O2 Therapy;
Elevate HOB. Monitor ABG.
paper bag/re-breather mask.
31 | P a g e
IV. C O N C L U S I O N
Nurses need to understand the concepts of Fluid and Electrolyte/ Acid-Base
to anticipate, Identify, and respond to possible imbalances. An awareness of fluid
and electrolyte regulation guides the nurse in anticipating potential problems and
ensuring that appropriate interventions take place. Integral part for the nurse is to
identify/assess patient who are at risk in developing imbalances in fluids,
electrolytes, and acid-base. Its a challenge for us to maintain their specific ranges
in normal values.
V. R E F E R E N C E S
Understanding Pathophysiology, 3
rd
Edition (S. Huether & K. McCance)
Brunner and Suddarths Textbook of MSN, 11
th
Edition
Hurst Reviews (Pathophysiology Review)
MSN made Incredibly easy, 3
rd
edition
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Polydioxanone Thread LiftingDocument4 pagesPolydioxanone Thread LiftingGLORIANo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- DX Report - Steven SimucaseDocument6 pagesDX Report - Steven Simucaseapi-494012486100% (3)
- Learn Earth Science essentialsDocument6 pagesLearn Earth Science essentialsJake Arman PrincipeNo ratings yet
- NCP Impaired Urinary EliminationDocument2 pagesNCP Impaired Urinary EliminationTrixy Marie EcotNo ratings yet
- Science G8 (LM Front)Document8 pagesScience G8 (LM Front)xdmhundz999No ratings yet
- Neurology Case SheetDocument9 pagesNeurology Case SheetAshwaq TpNo ratings yet
- Science Learner Module-130708064905-Php Appilcation01 :)Document350 pagesScience Learner Module-130708064905-Php Appilcation01 :)William Bryle Pertos75% (4)
- Science 8 Teachers GuideDocument230 pagesScience 8 Teachers GuideMichelle Gonzales Caliuag86% (141)
- SHS Core - Physical Science CG - 0Document17 pagesSHS Core - Physical Science CG - 0Loo DrBrad67% (3)
- APA Eating Disorders Practice Guideline Under CopyeditingDocument139 pagesAPA Eating Disorders Practice Guideline Under CopyeditingIbrahim NasserNo ratings yet
- Initial Assessment and Management Atls 10Document39 pagesInitial Assessment and Management Atls 10Fadhila K.100% (1)
- Stem - Physics 2 CGDocument15 pagesStem - Physics 2 CGVictoria Mabini100% (7)
- Immediate Loading FaizDocument85 pagesImmediate Loading FaizDrrksundar KumarNo ratings yet
- Stem - Physics 1 CGDocument13 pagesStem - Physics 1 CGVictoria MabiniNo ratings yet
- Lesson Guide in Earth and Life Science I. ObjectivesDocument5 pagesLesson Guide in Earth and Life Science I. ObjectivesallanrnmanalotoNo ratings yet
- S11ES II J 41Document4 pagesS11ES II J 41allanrnmanalotoNo ratings yet
- SEMINAR ON MULTIPLE PREGNANCY ContentDocument21 pagesSEMINAR ON MULTIPLE PREGNANCY ContentMonika shankar0% (1)
- DRR1112 IIc D 32Document5 pagesDRR1112 IIc D 32allanrnmanalotoNo ratings yet
- C105a Pre-Sea and Periodic Medical Fitness Examinations For SeafarersDocument4 pagesC105a Pre-Sea and Periodic Medical Fitness Examinations For SeafarersAbu ShabeelNo ratings yet
- AnalgesicDocument56 pagesAnalgesicMuhammad hilmiNo ratings yet
- Department of Education Region III: I. ObjectivesDocument3 pagesDepartment of Education Region III: I. ObjectivesallanrnmanalotoNo ratings yet
- DRRR 11 12 Ic 7Document3 pagesDRRR 11 12 Ic 7ben leeNo ratings yet
- DRR11 12 Ic D 34Document3 pagesDRR11 12 Ic D 34allanrnmanalotoNo ratings yet
- DRR11 12 Ia B 6Document3 pagesDRR11 12 Ia B 6allanrnmanalotoNo ratings yet
- Lesson Guide in Earth and Life Science I. ObjectivesDocument3 pagesLesson Guide in Earth and Life Science I. ObjectivesallanrnmanalotoNo ratings yet
- DRR11/12-Ic-8. Explain The Meaning of VulnerabilityDocument6 pagesDRR11/12-Ic-8. Explain The Meaning of VulnerabilityallanrnmanalotoNo ratings yet
- How Does An Event Become A Disaster? 2. When Does An Event Become A Disaster?Document3 pagesHow Does An Event Become A Disaster? 2. When Does An Event Become A Disaster?allanrnmanalotoNo ratings yet
- Learning Continuity Plan SY 2020 - 2021Document5 pagesLearning Continuity Plan SY 2020 - 2021allanrnmanalotoNo ratings yet
- DLP DRR LC 24Document3 pagesDLP DRR LC 24allanrnmanaloto100% (1)
- DRRRM LC 9Document3 pagesDRRRM LC 9allanrnmanalotoNo ratings yet
- NBNBNB, BHJHJGFJFKGDocument293 pagesNBNBNB, BHJHJGFJFKGYvi100% (2)
- 1 - Page Modified Daily Lesson Log For Senior High SchoolDocument4 pages1 - Page Modified Daily Lesson Log For Senior High Schoolallanrnmanaloto100% (1)
- STEM - Biology 1 CG - With Tagged Sci Equipment PDFDocument8 pagesSTEM - Biology 1 CG - With Tagged Sci Equipment PDFKOUJI N. MARQUEZNo ratings yet
- STEM - Gen Chem 1 and 2 CG PDFDocument18 pagesSTEM - Gen Chem 1 and 2 CG PDFChelie Trangia50% (2)
- S11ES IIa 23Document5 pagesS11ES IIa 23allanrnmanalotoNo ratings yet
- Lesson Guide in Earth and Life Science I. ObjectivesDocument2 pagesLesson Guide in Earth and Life Science I. ObjectivesallanrnmanalotoNo ratings yet
- STEM - Biology 2 CG - With Tagged Sci EquipmentDocument4 pagesSTEM - Biology 2 CG - With Tagged Sci EquipmentVictoria MabiniNo ratings yet
- S11ES IIc 28Document5 pagesS11ES IIc 28allanrnmanalotoNo ratings yet
- S11ES IIh I 39Document2 pagesS11ES IIh I 39allanrnmanaloto50% (2)
- S11ES IIi 40Document3 pagesS11ES IIi 40allanrnmanaloto50% (2)
- NSE121 - Care PlanDocument7 pagesNSE121 - Care Planramyharoon2004No ratings yet
- Infectious Bronchitis in Broiler - Veterinaria DigitalDocument3 pagesInfectious Bronchitis in Broiler - Veterinaria DigitalMahesh KajagarNo ratings yet
- Nama: Riris Putri Marito Sinaga NIM: 04022722125001 Prodi: Ilmu Kesehatan Anak No Soal 35Document13 pagesNama: Riris Putri Marito Sinaga NIM: 04022722125001 Prodi: Ilmu Kesehatan Anak No Soal 35Riris SinagaNo ratings yet
- A) Long-Term Follow-Up of Patients With Migrainous Infarction - Accepted and Final Publication From Elsevier1-s2.0-S030384671730344X-mainDocument3 pagesA) Long-Term Follow-Up of Patients With Migrainous Infarction - Accepted and Final Publication From Elsevier1-s2.0-S030384671730344X-mainRodrigo Uribe PachecoNo ratings yet
- Ulnar Nerve Entrapment - WikipediaDocument6 pagesUlnar Nerve Entrapment - WikipediaSylvia GraceNo ratings yet
- Ultraspund in Pediatric EmergencyDocument22 pagesUltraspund in Pediatric EmergencyAli Akbar RahmaniNo ratings yet
- Form Self Assessment Review 144 Diagnosa Layanan Primer: 1 Abortus Spontan Komplit O03.9 707Document78 pagesForm Self Assessment Review 144 Diagnosa Layanan Primer: 1 Abortus Spontan Komplit O03.9 707Rani AprianiNo ratings yet
- HNP3Document9 pagesHNP3dev darma karinggaNo ratings yet
- Resume Atiyeh KaboudvandDocument2 pagesResume Atiyeh Kaboudvandarian tejaratNo ratings yet
- Surgery Chapter 1 SkinDocument6 pagesSurgery Chapter 1 Skinnandoooo86No ratings yet
- Pulmonary Edema and Hemorrhagination Causes in Salt Water Drowning (39Document9 pagesPulmonary Edema and Hemorrhagination Causes in Salt Water Drowning (39Akash AkashNo ratings yet
- Daftar PustakaDocument4 pagesDaftar PustakajhnaidillaNo ratings yet
- Assessment and Concept Map Care Plan: Joseph GorospeDocument5 pagesAssessment and Concept Map Care Plan: Joseph Gorospeapi-497389977No ratings yet
- For E-PortfolioDocument14 pagesFor E-Portfolioapi-174496267No ratings yet
- Ds Pedia WardDocument2 pagesDs Pedia WardRhea Mae Valles - ReyesNo ratings yet
- Peran Ipp - Bu CostyDocument13 pagesPeran Ipp - Bu Costysahrun runtiNo ratings yet
- NLEDocument18 pagesNLEKeij AranetaNo ratings yet
- Inter Disciplinary Periodontics A Multi Disciplinary Approach To Complex Case Planning and TreatmentDocument17 pagesInter Disciplinary Periodontics A Multi Disciplinary Approach To Complex Case Planning and TreatmentInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Emergency TriageDocument8 pagesEmergency TriageJam Chelsea ChyNo ratings yet
- Chest PainDocument13 pagesChest Paing3murtulu100% (1)