Professional Documents
Culture Documents
Novel Perspectives On Mucormycosis
Uploaded by
abogadomedicoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Novel Perspectives On Mucormycosis
Uploaded by
abogadomedicoCopyright:
Available Formats
CLINICAL MICROBIOLOGY REVIEWS, July 2005, p. 556569 Vol. 18, No.
3
0893-8512/05/$08.000 doi:10.1128/CMR.18.3.556569.2005
Copyright 2005, American Society for Microbiology. All Rights Reserved.
Novel Perspectives on Mucormycosis: Pathophysiology, Presentation,
and Management
Brad Spellberg,
1,2
* John Edwards, Jr.,
1,2
and Ashraf Ibrahim
1,2
Department of Medicine, Los Angeles Biomedical Institute at Harbor-UCLA Medical Center, Torrance, California,
1
and David Geffen School of Medicine at UCLA, Los Angeles, California
2
INTRODUCTION.......................................................................................................................................................556
PATHOGENESIS........................................................................................................................................................556
Host Defenses..........................................................................................................................................................556
Role of Iron in Pathogenesis.................................................................................................................................557
Fungal-Endothelial Interactions...........................................................................................................................558
CLINICAL PRESENTATION...................................................................................................................................558
General Principles ..................................................................................................................................................558
Epidemiology and Disease Manifestations..........................................................................................................558
Rhinocerebral mucormycosis ............................................................................................................................559
Pulmonary mucormycosis ..................................................................................................................................560
Cutaneous mucormycosis...................................................................................................................................560
Gastrointestinal mucormycosis.........................................................................................................................560
Disseminated mucormycosis..............................................................................................................................561
Miscellaneous forms...........................................................................................................................................561
TREATMENT..............................................................................................................................................................561
General Principles ..................................................................................................................................................561
Role of Surgery........................................................................................................................................................562
Antifungal Therapy.................................................................................................................................................562
Polyenes................................................................................................................................................................563
Azoles....................................................................................................................................................................564
Echinocandins .....................................................................................................................................................564
Novel Iron Chelators ..............................................................................................................................................565
Other Adjunctive Therapies ..................................................................................................................................565
PROGNOSIS...............................................................................................................................................................565
CONCLUSIONS .........................................................................................................................................................565
REFERENCES ............................................................................................................................................................566
INTRODUCTION
The zygomycoses are infections caused by fungi of the class
Zygomycetes, comprised of the orders Mucorales and Ento-
mophthorales. The Entomophthorales are rare causes of sub-
cutaneous and mucocutaneous infections known as entomoph-
thoromycosis, which largely afict immunocompetent hosts in
developing countries. In contrast, fungi of the order Mucorales
are causes of mucormycosis, a life-threatening fungal infection
almost uniformly affecting immunocompromised hosts in ei-
ther developing or industrialized countries.
Fungi belonging to the order Mucorales are distributed into
six families, all of which can cause cutaneous and deep infec-
tions (129). Species belonging to the family Mucoraceae are
isolated more frequently from patients with mucormycosis
than any other family. Among the Mucoraceae, Rhizopus oryzae
(Rhizopus arrhizus) is by far the most common cause of infec-
tion (129). Other less frequently isolated species of the Muc-
oraceae family that cause a similar spectrum of infections in-
clude Rhizopus microsporus var. rhizopodiformis, Absidia
corymbifera, Apophysomyces elegans, Mucor species, and Rhi-
zomucor pusillus (61, 81, 129). Increasing cases of mucormy-
cosis have been also reported due to infection with Cunning-
hamella spp. (in the Cunninghamellaceae family) (24, 78, 82,
161). To date, rare case reports have demonstrated the ability
of species belonging to the remaining four families to cause
mucormycosis (12, 68, 72, 89, 129).
PATHOGENESIS
Host Defenses
Both mononuclear and polymorphonuclear phagocytes of
normal hosts kill Mucorales by the generation of oxidative
metabolites and the cationic peptides defensins (33, 166, 169)
(Fig. 1). Clinical evidence demonstrates that these phagocytes
are the major host defense mechanism against mucormycosis.
For example, neutropenic patients are at increased risk of
developing mucormycosis. Furthermore, patients with dysfunc-
tional phagocytes are also at higher risk for developing mucor-
mycosis. Hyperglycemia and acidosis are known to impair the
ability of phagocytes to move toward and kill the organisms by
both oxidative and nonoxidative mechanisms (23). Addition-
ally, corticosteroid treatment affects the ability of mouse bron-
* Corresponding author. Mailing address: Division of Infect. Dis.,
Harbor-UCLA Medical Center, 1124 West Carson St. RB2, Torrance,
CA 90502. Phone: (310) 222-5381. Fax: (310) 782-2016. E-mail: bspell-
berg@labiomed.org.
556
choalveolar macrophages to prevent germination of the spores
in vitro or after in vivo infection induced by intranasal inocu-
lation (169). The exact mechanisms by which ketoacidosis,
diabetes, or steroids impair the function of these phagocytes
remain unknown.
Role of Iron in Pathogenesis
A recently identied important clinical feature is the in-
creased susceptibility to mucormycosis of patients with ele-
vated available serum iron. It has been known for two decades
that patients treated with the iron chelator deferoxamine have
a markedly increased incidence of invasive mucormycosis (16).
However, it is now clear that iron chelation is not the mecha-
nism by which deferoxamine enables mucormycosis infections.
While deferoxamine is an iron chelator from the perspective of
the human host, Rhizopus spp. actually utilize deferoxamine as
a siderophore to supply previously unavailable iron to the
fungus (15, 30). Rhizopus spp. can accumulate 8- and 40-fold-
greater amounts of iron supplied by deferoxamine than can
Aspergillus fumigatus and Candida albicans, respectively, and
this increased iron uptake by Rhizopus spp. is linearly corre-
lated with its growth in serum (15). Additionally, data from
animal models emphasize the exceptional requirement of iron
for Rhizopus pathogenicity since administration of deferox-
amine or free iron worsens survival of animals infected with
Rhizopus spp. but not Candida albicans (1, 16, 30, 158). Finally,
animal models have demonstrated that other iron chelators,
which are not used as siderophores by the fungus, do not
similarly exacerbate mucormycosis infection (16).
Patients with diabetic ketoacidosis are at high risk of develop-
ing rhinocerebral mucormycosis (61, 81, 129). Multiple lines of
evidence support the conclusion that patients in systemic acidosis
have elevated levels of available serum iron, likely due to release
of iron from binding proteins in the presence of acidosis (9). For
example, sera collected from patients with diabetic ketoacidosis
supported growth of Rhizopus oryzae in the presence of acidic pH
(7.3 to 6.88) but not in the presence of alkaline pH (7.78 to 8.38).
Acidic sera that supported the growth of R. oryzae were found to
contain increased available serum iron (69 g/dl versus 13 g/dl
for sera which did not support the growth of R. oryzae). Finally,
simulated acidotic conditions decreased the iron-binding capacity
of sera collected from normal volunteers, suggesting that acidosis
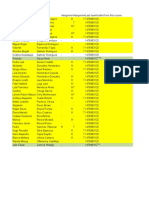
FIG. 1. Pathogenetic mechanisms of and host defense mechanisms against mucormycosis. To cause disease, the agents of mucormycosis must
scavenge from the host sufcient iron for growth, must evade host phagocytic defense mechanisms, and must access vasculature to disseminate.
A) In a normal host, primary defense mechanisms against mucormycosis include sequestration of iron in serum by specialized iron-binding proteins
(1), phagocytes including circulating neutrophils (2a) and tissue macrophages (2b), and endothelial cells (3), which regulate vascular tone and
permeability. Acting in concert, these mechanisms prevent establishment of infection in tissue and subsequent endovascular invasion. B) In
susceptible hosts, normal defense mechanisms break down. For example, in diabetic ketoacidosis (DKA), the acidic pH of the serum causes
dissociation of free iron from sequestering proteins (1). This release of free iron allows rapid fungal growth. Defects in phagocytic defense
mechanisms (2), for example, deciency in cell number (neutropenia) or functional defects caused by corticosteroids or the hyperglycemia and
acidosis of diabetic ketoacidosis, allow proliferation of the fungus. Finally, adherence to and damage of endothelial cells by the fungus (3) allows
fungal angioinvasion and vessel thrombosis and subsequent tissue necrosis and dissemination of the fungal infection.
VOL. 18, 2005 NOVEL PERSPECTIVES ON MUCORMYCOSIS 557
temporarily disrupts the capacity of transferrin to bind iron (9).
Therefore, the increased susceptibility to mucormycosis of pa-
tients with diabetic ketoacidosis is likely due at least in part to an
elevation in available serum iron during diabetic ketoacidosis.
Fungal-Endothelial Interactions
A hallmark of mucormycosis infections is the virtually uni-
form presence of extensive angioinvasion with resultant vessel
thrombosis and tissue necrosis. This angioinvasion is associ-
ated with the ability of the organism to hematogenously dis-
seminate from the original site of infection to other target
organs. Hence, damage of and penetration through endothelial
cells lining blood vessels is likely a critical step in the organ-
isms pathogenetic strategy. R. oryzae spores but not germlings
(i.e., pregerminated spores) have the ability to adhere to sub-
endothelial matrix proteins including laminin and type IV col-
lagen in vitro (17). Similarly, we have recently found that R.
oryzae spores adhere to subendothelial matrix proteins signif-
icantly better than do R. oryzae hyphae, however spores and
hyphae adhere equivalently to human umbilical vein endothe-
lial cells (64). The disparity of spore and germ tube adherence
to subendothelial matrix proteins but equivalent adherence to
endothelial cells indicates that R. oryzae adhesins to endothe-
lial cells are likely distinct from the adhesins used to bind to
subendothelial matrix proteins.
We also found that germlings of R. oryzae damage endothe-
lial cells in vitro. This damage is independent of serum factors
and requires phagocytosis of R. oryzae by endothelial cells (64).
Surprisingly, R. oryzae viability was not required for endothelial
cell damage, but phagocytosis was required for dead R. oryzae
to cause damage (64). In a subsequent pilot study, intravenous
administration of four doses of heat-killed R. oryzae blasto-
spores resulted in a 40% mortality in diabetic mice (unpub-
lished observations). The precise mechanisms by which dead R.
oryzae mediates tissue injury remain unclear. Nevertheless, the
clinical implication is that simply killing R. oryzae once it has
already established a presence in tissue may not prevent sub-
sequent tissue injury, perhaps in part explaining the lack of
efcacy of cidal antifungal agents during clinical disease.
CLINICAL PRESENTATION
General Principles
As mentioned earlier, the clinical hallmark of mucormycosis
is vascular invasion resulting in thrombosis and tissue infarc-
tion/necrosis. Mucormycosis virtually always occurs in patients
with defects in host defense and/or with increased available
serum iron, although rare cases have been reported in appar-
ently normal hosts (83, 85, 119). In most cases, the infection is
relentlessly progressive and results in death unless treatment
with a combination of surgical debridement and antifungal
therapy is initiated promptly.
Epidemiology and Disease Manifestations
Mucormuycosis is less common than other opportunistic
fungal infections, such as those caused by Candida and As-
pergillus spp. One population-based study estimated the inci-
dence of mucormycosis to be 1.7 cases per million people per
year, which translates to approximately 500 cases per year in
the United States (126). In autopsy series, the prevalence of
mucormycosis has ranged from 1 to 5 cases per 10,000 autop-
sies, making the infection 10- to 50-fold less common than
invasive Candida or Aspergillus infections (56, 154, 178). Fi-
nally, in patients at higher risk, such as those undergoing allo-
geneic bone marrow transplantation, the prevalence of mucor-
mycosis has been described to be as high as 2 to 3% (90, 96).
Based on clinical presentation and the involvement of a
particular anatomic site, mucormycosis can be divided into at
least six clinical categories: (i) rhinocerebral, (ii) pulmonary,
(iii) cutaneous, (iv) gastrointestinal, (v) disseminated, and (iv)
miscellaneous. Of note, these categories of invasive mucormy-
cosis tend to occur in patients with specic defects in host
defense (Table 1). For example, diabetics in ketoacidosis typ-
ically develop the rhinocerebral form of the disease, and much
more rarely develop pulmonary or disseminated disease (75,
99, 107, 118).
The mechanism for ketoacidosis preferentially causing sus-
ceptibility to the rhinocerebral form of the disease remains
unclear. As mentioned earlier, patients in ketoacidosis, or in-
deed any systemic acidosis, have increased available iron in
serum due to dissociation of iron from sequestering proteins in
acidic conditions (9). However, the predominant presentation
of mucormycosis in the setting of deferoxamine therapy is
disseminated disease (37, 46, 123, 151, 160), indicating that
increased available iron cannot, by itself, explain the preferen-
tial occurrence of rhinocerebral disease in ketoacidosis. Fur-
thermore, while it is known that hyperglycemia and acidosis
negatively impact neutrophil chemotaxis and phagocytic activ-
ity (23), these observations cannot explain the preferential
occurrence of rhinocerebral disease in diabetic ketoacidosis
because neutropenic patients more commonly develop pulmo-
nary mucormycosis than rhinocerebral disease (98, 150).
Much more readily understood are the risk factors for inva-
sive skin and soft tissue infections caused by the agents of
mucormycosis. These infections occur in patients with dis-
rupted cutaneous barriers, as a result of either traumatic im-
plantation of soil, maceration of skin by a moist surface (5,
119), or even via direct access through intravenous catheters or
subcutaneous injections (4, 73, 125). These cases illustrate an
alarming trend in the epidemiology of mucormycosis. Mucor-
mycosis, formerly virtually always community acquired and
often in the setting of diabetic ketoacidosis, is rapidly becom-
ing a nosocomial infection in patients with malignancy or un-
dergoing organ or hematopoietic cell transplantation (108).
Given the increasing incidence of diabetes and cancer in the
TABLE 1. Relationship between predisposing condition and
site of infection
Predisposing condition Predominant site of infection
Diabetic ketoacidosis Rhinocerebral
Neutropenia Pulmonary and disseminated
Corticosteroids Pulmonary, disseminated, or
rhinocerebral
Deferoxamine Disseminated
Malnutrition Gastrointestinal
Trauma, catheter/injection site,
skin maceration
Cutaneous/subcutaneous
558 SPELLBERG ET AL. CLIN. MICROBIOL. REV.
increasingly obese and elderly United States population, it is
not surprising that a recent review found a marked increase in
reported cases of mucormycosis over the last two decades (45).
As mentioned, there has also been a shift from community
onset to nosocomial onset of disease. Nosocomial mucormy-
cosis has been associated with iatrogenic immunosuppression
(79, 108, 130) and a variety of procedures or devices used in
hospitals, including antifungal prophylaxis (69, 130), bandages
or medication patches (43, 119), intravenous catheters (4, 11,
74, 87), and even tongue depressors (50, 54, 92) (see below).
At transplant centers there has also been an alarming rise in
the incidence of mucormycosis (69, 140). For example, at the
Fred Hutchinson Cancer Center, Marr et al. have described a
doubling in the number of cases from 1985 to 1989 to 1995 to
1999 (94). Similarly, Kontoyianis et al. have described a greater
than doubling in the incidence of mucormycosis in transplant
patients over a similar time span (79). In patients undergoing
hematological stem cell transplantation, mucormycosis devel-
ops at least as commonly in nonneutropenic periods as in
neutropenic periods. For example, two major transplant cen-
ters have recently reported that more than half the cases of
mucormycosis occurred more than 90 days after transplanta-
tion (90, 94).
Major risk factors for mucormycosis in the transplant setting
include underlying myelodysplastic syndrome (possibly due to
iron overload from repeated blood transfusions) and graft-
versus-host disease treated with steroids (90, 94, 116, 140).
Administration of antithymocyte globulin may also pose a risk
for mucormycosis (140). Although less than half of these pa-
tients are neutropenic at the time of disease onset, prolonged
neutropenia is a risk factor for mucormycosis in this setting
(130), as are diabetes mellitus and steroid use (130). The role
of antifungal prophylaxis in predisposing patients to develop-
ing mucormycosis is increasingly being described, as discussed
further below. Prophylaxis with either itraconazole (130) or
voriconazole (65, 66, 69, 96, 163) has been implicated in pre-
disposing to mucormycosis.
Rhinocerebral mucormycosis. Rhinocerebral mucormycosis
continues to be the most common form of the disease, account-
ing for between one-third and one-half of all cases of mucor-
mycosis (122). About 70% of rhinocerebral cases (occasionally
referred to as craniofacial) are found in diabetic patients in
ketoacidosis (99). More rarely, rhinocerebral mucormycosis
has also occurred in patients who received a solid organ trans-
plant or those with prolonged neutropenia (2, 45, 118, 119, 122,
179). Recently, rhinocerebral disease has been an increasing
problem in patients undergoing hematopoietic stem cell trans-
plantation (94, 102). These cases have largely been associated
with steroid use for graft-versus-host disease.
The initial symptoms of rhinocerebral mucormycosis are
consistent with either sinusitis or periorbital cellulitis (32, 149)
and include eye or facial pain and facial numbness, followed by
the onset of conjunctival suffusion, blurry vision, and soft tissue
swelling (75, 118, 153). Fever is variable and may be absent in
up to half of cases (149); white blood cell counts are typically
elevated, as long as the patient has functioning bone marrow
(153). If untreated, infection usually spreads from the ethmoid
sinus to the orbit, resulting in loss of extraocular muscle func-
tion and proptosis. Marked chemosis may also be seen. The
infection may rapidly extend into the neighboring tissues. On-
set of signs and symptoms in the contralateral eye, with result-
ing bilateral proptosis, chemosis, vision loss, and ophthalmo-
plegia, is an ominous sign that suggests the development of
cavernous sinus thrombosis.
Upon visual inspection, infected tissue may appear normal
during the earliest stages of spread of the fungus. Infected tissue
then progresses through an erythematous phase, with or without
edema, before onset of a violaceous appearance, and nally the
development of a black, necrotic eschar as the blood vessels be-
come thrombosed and tissue infarction occurs (57, 119). Infection
can sometimes extend from the sinuses into the mouth and pro-
duce painful, necrotic ulcerations of the hard palate (119).
Cranial nerve ndings represent extensive infection and sig-
nal a grave prognosis. Progressive vision loss and ultimately
blindness may result either from involvement of the optic
nerve or from arteriolar invasion resulting in infarction (58,
109, 143, 153) or from cavernous sinus thrombosis. Cranial
nerves ve and seven may also be affected, resulting in ipsilat-
eral loss of facial sensation and ptosis and pupillary dilation
(32, 118, 153). Infection can also spread posteriorly from either
the orbit or sinuses to the central nervous system. A bloody
nasal discharge may be the rst sign that infection has invaded
through the terbinates and into the brain. When there is ex-
tensive central nervous system involvement, the angioinvasive
nature of the fungus may result in cavernous sinus thrombosis
and internal carotid artery encasement and thrombosis with
extensive resulting cerebral infarctions (7, 88, 104, 153). Occa-
sionally cerebral vascular invasion may lead to hematogenous
dissemination of the infection (84, 122), with or without devel-
opment of mycotic aneurysms (135).
A high index of suspicion is required to make the diagnosis
of rhinocerebral mucormycosis, as evidenced by the fact that
autopsy series have found up to half of cases are diagnosed
postmortem (78, 101, 154). Imaging techniques may be sug-
gestive of mucormycosis but are rarely diagnostic. Indeed, the
initial imaging study is frequently negative or has only subtle
ndings. The most common nding on computerized tomog-
raphy (CT) scanning of the head or sinuses is subtle sinus
mucosal thickening or thickening of the extraocular muscles. It
is also common to detect no abnormalities in the bones of the
sinuses despite clinical evidence of progressive disease (149).
However, when present, the nding of bony erosion of the
sinuses is strongly suggestive of the diagnosis in the appropri-
ate clinical context (e.g., patient in diabetic ketoacidosis with
proptosis). It should be emphasized that it is very uncommon
to visualize an organized retroorbital mass.
Although evidence of infection of the soft tissues of the orbit
may sometimes be seen by CT scan, magnetic resonance im-
aging is more sensitive (40). Still, as with CT scans, patients
with early rhinocerebral mucormycosis may have a normal
magnetic resonance imaging, and surgical exploration with bi-
opsy of the areas of suspected infection should always be per-
formed in high-risk patients. It is critically important to em-
phasize that if mucormycosis is suspected, initial empirical
therapy with a polyene antifungal should begin while the diag-
nosis is being conrmed, rather than waiting while a protracted
series of diagnostic tests are completed.
Given the limitations of imaging studies, diagnosing mucor-
mycosis almost always requires histopathologic evidence of
fungal invasion of the tissues. Culturing organisms from a
VOL. 18, 2005 NOVEL PERSPECTIVES ON MUCORMYCOSIS 559
potentially infected site is rarely sufcient to establish the di-
agnosis of mucormycosis because the causative agent is ubiq-
uitous, may colonize normal persons, and is a relatively fre-
quent laboratory contaminant. Additionally, the organism may
be killed during tissue grinding (168), which is routinely used
to process tissue specimens for culture. Thus, a sterile culture
does not rule out the infection (149). Furthermore, waiting for
the results of the fungal culture may delay the institution of
appropriate therapy.
There are no reliable serologic, PCR-based, or skin tests for
mucormycosis. Therefore, the diagnosis should be made by
biopsy of infected tissues. The biopsy should demonstrate the
characteristic wide, ribbon-like, aseptate hyphal elements that
branch at right angles. The organisms are often surrounded by
extensive necrotic debris. Other fungi, including Aspergillus,
Fusarium, or Scedosporium spp, may look similar to the Muc-
orales on biopsy. However, these molds have septae, are usu-
ally thinner, and branch at acute angles. The genus and species
of the infecting organism may be determined by culture of the
infected tissue. However, the organism is rarely isolated from
cultures of blood, cerebrospinal uid, sputum, urine, feces or
swabs of infected areas.
Pulmonary mucormycosis. Mucormycosis of the lung occurs
most commonly in leukemic patients who are receiving che-
motherapy or in patients undergoing hematopoietic stem cell
transplants. Indeed, the pulmonary form of the disease is the
most common form found in neutropenic and stem cell-trans-
plant patients (94, 102). These patients typically have severe
neutropenia and are frequently receiving broad-spectrum an-
tibiotics for unremitting fever (150), while in patients under-
going allogeneic stem cell transplantation, the disease often
occurs postengraftment and is strongly associated with graft-
versus-host disease. Patients with diabetic ketoacidosis can also
develop pulmonary mucormycosis, although infections in these
patients are less common and less fulminant and follow a more
subacute course than is typically seen in patients with neutro-
penia (132, 150).
Pulmonary mucormycosis may develop as a result of inha-
lation or by hematogenous or lymphatic spread. Symptoms of
pulmonary mucormycosis include dyspnea, cough, and chest
pain (150). In a recent series of 32 cases of pulmonary mucor-
mycosis, fever was present in the majority of patients (150).
Angioinvasion results in necrosis of tissue parenchyma, which
may ultimately lead to cavitation and/or hemoptysis, which
may be fatal if a major blood vessel is involved (49, 171).
Radiographically, a variety of ndings may be present, in-
cluding, in descending order of frequency: lobar consolidation,
isolated masses, nodular disease, and cavitation (70, 98, 150).
Wedge-shaped infarcts of the lung may also be seen, particu-
larly following thrombosis of the pulmonary vessels due to
fungal angioinvasion (93). High-resolution chest CT scan is the
best method of determining the extent of pulmonary mucor-
mycosis and may demonstrate evidence of infection before it is
seen on the chest x-ray. One suggestive nding is expansion of
a mass or consolidation across tissue planes, in particular to-
wards the great vessels in the mediastinum (127). Unfortu-
nately, sputum culture is highly unreliable. In two case series,
sputum and bronchiolar alveolar lavage cultures were negative
in 18 of 19 cases of biopsy-proven pulmonary mucormycosis
(127, 150). Therefore, biopsy with histopathological assess-
ment remains the best modality to diagnose pulmonary
mucormycosis.
If pulmonary infection is not treated, hematogenous dissem-
ination to the contralateral lung and other organs frequently
occurs. Patients with untreated pulmonary mucormycosis usu-
ally die from disseminated disease before respiratory failure
occurs. The notable exception is the rare patient with massive
hemoptysis (103, 113). The overall mortality of pulmonary
mucormycosis is approximately 50 to 70% but is 95% if the
pulmonary mucormycosis is part of a disseminated process (45,
150).
Cutaneous mucormycosis. As mentioned, patients who are
at high risk of developing cutaneous mucormycosis are those
with disruption of the normal protective cutaneous barrier.
The agents of mucormycosis are typically incapable of pene-
trating intact skin. However, burns, traumatic disruption of
skin, and persistent maceration of skin enable the organisms to
penetrate into deeper tissues. A typical case results from trau-
matic implantation of soil, for example, as a result of a motor
vehicle accident or penetrating injury with plant material (e.g.,
a thorn) (4, 119). In diabetic and immunocompromised pa-
tients, cutaneous lesions may also arise at insulin injection or
catheter insertion sites (73, 125). Contaminated surgical dress-
ings have also been implicated as a source of cutaneous mu-
cormycosis (43, 100). Cutaneous mucormycosis has also oc-
curred in the context of contaminated tape used to secure an
endotracheal tube in a ventilated patient (5).
Cutaneous disease can be very invasive locally and penetrate
from the cutaneous and subcutaneous tissues into the adjacent
fat, muscle, fascia, and even bone. Secondary vascular invasion
may also lead to hematogenously disseminated infection of the
deep organs. Cutaneous and subcutaneous disease may lead to
necrotizing fasciitis, which has a mortality approaching 80%
(18, 80, 115, 124). However, isolated cutaneous mucormycosis
(i.e., not disseminated disease) has a favorable prognosis and a
low mortality if aggressive surgical debridement is done
promptly (4).
Gastrointestinal mucormycosis. Mucormycosis of the gas-
trointestinal tract is rare. It mainly occurs in patients who are
extremely malnourished (especially infants or children) and is
thought to arise from ingestion of the fungi. In particular,
gastrointestinal mucormycosis has been seen in premature ne-
onates, often in association with widespread disseminated dis-
ease (6, 27, 71, 76, 128, 137). Necrotizing enterocolitis has been
described largely in premature neonates (35, 71, 106, 128, 139,
157, 174, 177) and more rarely in neutropenic adults (146,
152). Rare cases of gastrointestinal mucormycosis have been
described in association with other immune-compromising
conditions, including AIDS (19), systemic lupus erythematosus
(55), and organ transplantation (77, 95, 97, 138).
The stomach, colon, and ileum are the most commonly in-
volved sites. Cases of hepatic mucormycosis have also been
associated with ingestion of herbal medications (111). Because
this infection is acute and rapidly fatal, it is often diagnosed
postmortem. The symptoms are varied and depend on the site
affected. Nonspecic abdominal pain and distention associated
with nausea and vomiting are the most common symptoms.
Fever and hematochezia may also occur. The patient is often
560 SPELLBERG ET AL. CLIN. MICROBIOL. REV.
thought to have an intra-abdominal abscess. The diagnosis may
be made by biopsy of the suspected area during surgery or
endoscopy. Recently, a iatrogenic outbreak of gastric mucor-
mycosis occurred due to contamination of the wooden appli-
cators used to mix drugs that were poured down the patients
nasogastric feeding tubes (92). These patients presented with
massive gastric bleeds. The diagnosis was made by culture of
gastric aspirates and culture of the box of wooden tongue
depressors. This experience further underscores the alarming
trend of increasing iatrogenic/nosocomial onset for mucormy-
cosis.
Disseminated mucormycosis. Hematogenously dissemi-
nated mucormycosis may originate from any primary site of
infection. Pulmonary mucormycosis in severely neutropenic
patients has the highest incidence of dissemination. Less com-
monly, dissemination can arise from the gastrointestinal tract,
the sinuses, or cutaneous lesions, the last occurring particularly
in burn patients. The most common site of dissemination is the
brain, but metastatic lesions may also be found in the spleen,
heart, skin, and other organs. Cerebral infection following dis-
semination is distinct from rhinocerebral mucormycosis and
results in abscess formation and infarction. Patients present
with sudden onset of focal neurological decits or coma. The
mortality associated with dissemination to the brain ap-
proaches 100% (144). Even without central nervous system
involvement, disseminated mucormycosis has a mortality of
90% (45). In patients undergoing hematopoietic stem cell
transplantation, the 1-year mortality is 95% due to a combi-
nation of underlying disease, graft-versus-host disease, and the
infection (57, 94).
Recent case series have described frequent dissemination in
the context of voriconazole prophylaxis of transplant patients.
In ve recent case series, a total of 18 cases of disseminated
mucormycosis have occurred in patients post-allogeneic hema-
topoietic stem cell transplantation who were receiving voricon-
azole either prophylactically or therapeutically for other infec-
tions (65, 66, 96, 140, 163). An additional patient who had
leukemia and was treated with combination voriconazole plus
caspofungin for proven Aspergillus pneumonia, who subse-
quently developed disseminated mucormycosis, has been de-
scribed (13). Finally, three patients who developed mucormy-
cosis while receiving voriconazole for empirical neutropenic
fever (not in the transplant setting) or for prophylaxis post-
renal transplantation have been described (112, 163).
It has been pointed out that the increase in frequency of
mucormycosis in transplant patients preceded the availability
of voriconazole and that therefore the precise role of voricon-
azole in predisposing patients to mucormycosis is unclear (69).
For example, increasingly intensive immunosuppressive regi-
mens and broader availability of allogeneic transplantation
(e.g., to patients of increasing age) may be playing a role.
Furthermore, the increasing use of peripheral stem cell trans-
plants (in lieu of bone marrow-derived cells), nonmyeloablative
conditioning regimens, and unrelated donor and/or HLA-mis-
matched transplants have increased the incidence of graft-
versus-host disease. As mentioned, graft-versus-host disease
and its treatment with corticosteroids are strongly linked with
the risk of mucormycosis in the transplant setting (90, 94, 116,
140). Indeed, most of the reported cases of mucormycosis
occurring during voriconazole therapy have occurred in pa-
tients receiving corticosteroids for graft-versus-host disease
(66, 96, 140).
Nevertheless, the uniformity of the reports of mucormycosis
in patients receiving voriconazole infections implicates a link
between the drug and the disease. Voriconazole has broad
activity against Aspergillus, Candida, and Scedosporium spp.
and the dematiaceous fungi, but has no clinically relevant ac-
tivity against the agents of mucormycosis (34, 117, 120, 147).
Therefore, it is possible that the predisposition to mucormy-
cosis is due to selective inhibition of other fungi, which allows
the agents of mucormycosis to colonize the patient. As well, it
is also possible that voriconazole is preventing early-onset
deadly infections caused by other species of fungi (i.e., Candida
and Aspergillus), thereby allowing highly immunocompromised
patients, who in the past would have died earlier posttrans-
plant, to live long enough to become infected with the agents
of mucormycosis. It should be reiterated that a similar phe-
nomenon has been described with itraconazole prophylaxis,
the use of which is also an independent risk factor for devel-
opment of mucormycosis in this setting (130). Finally, there
have been two case reports of breakthrough mucormycosis in
patients receiving either caspofungin (133) or caspofungin plus
voriconazole (13) for other infections.
The diagnosis of disseminated disease is difcult because
patients are usually severely ill from multiple diseases and
virtually always have negative blood cultures. If there is evi-
dence of infarction in multiple organs, the diagnosis of mucor-
mycosis should be considered. However, aspergillosis is com-
monly associated with an identical clinical picture. When
disseminated mucormycosis is suspected, a careful search
should be made for cutaneous lesions that can be biopsied for
diagnostic purposes.
Miscellaneous forms. Agents of the Mucorales may cause
infection in virtually any body site. Brain involvement in the
absence of sinus infection, endocarditis, and pyelonephritis
occur occasionally, mainly in intravenous drug abusers (156,
162, 164, 176). Other reports have described mucormycosis in
bones (91, 121), mediastinum (25, 86), trachea (8, 175), kid-
neys (172), and peritoneum associated with dialysis (4, 136).
Other unusual forms of infection include superior vena cava
syndrome (51) and external otitis (110). Although mucormy-
cosis is not commonly seen in AIDS patients, there have been
a number of case reports of this infection in this patient pop-
ulation (41, 105, 134).
TREATMENT
General Principles
Four factors are critical for eradicating mucormycosis: ra-
pidity of diagnosis, reversal of the underlying predisposing
factors (if possible), appropriate surgical debridement of in-
fected tissue, and appropriate antifungal therapy. Early diag-
nosis is important because small, focal lesions can often be
surgically excised before they progress to involve critical struc-
tures or disseminate (107). Unfortunately, there are no sero-
logic or PCR-based tests to allow rapid diagnosis. As men-
tioned, autopsy series have reported that up to half the cases of
mucormycosis are diagnosed postmortem (78, 101, 154), un-
VOL. 18, 2005 NOVEL PERSPECTIVES ON MUCORMYCOSIS 561
derscoring the critical need to maintain a high index of clinical
suspicion and to aggressively pursue diagnostic biopsy. Cor-
recting or controlling predisposing problems is also essential
for improving the treatment outcome. In diabetic ketoacidotic
patients, hyperglycemia and acidemia should be corrected.
Discontinuation of deferoxamine or immunosuppressive ther-
apy, particularly steroids, should be strongly considered when
the diagnosis of mucormycosis is made.
Given the rapidly progressive nature of rhinocerebral mu-
cormycosis and the marked increase in mortality when the
fungus penetrates the cranium, any diabetic patient with a
headache and visual changes is a candidate for prompt evalu-
ation with imaging studies and nasal endoscopy to rule out
mucormycosis. Furthermore, to reiterate a concept that is fre-
quently poorly grasped by clinicians inexperienced with mu-
cormycosis, the initial imaging study is frequently negative or
has subtle ndings. Radiographic ndings lag behind clinical
progression in this disease, and a negative imaging study does
not provide a rationale to delay more aggressive diagnostic
maneuvers (e.g., endoscopy with biopsy) if clinical suspicion is
high. The appearance of tissue at endoscopy may also lag
behind invasion, as the mucosa can appear pink and viable
during the initial phase of fungal invasion. Therefore, if the
suspicion for disease is high, blind biopsies of sinus mucosa
and/or thickened extraocular muscles are warranted to make
the diagnosis.
Finally, time is of the essence in the management of mucor-
mycosis. Because patients with rhinocerebral disease may ini-
tially present with normal mental status and appear clinically
stable, the urgency for establishing the diagnosis is frequently
underappreciated. The key concept is that initial spread of the
fungus to the brain may be relatively asymptomatic. Once the
fungus has penetrated the cranium or entered the major intra-
cranial vasculature, mortality increases substantially. Addition-
ally, starting the patient on an antifungal is not denitive ther-
apy, since surgery may be a key addition to the treatment
strategy. The sensitivity of the organisms varies considerably,
so that a patient on amphotericin B alone may be receiving
completely ineffective therapy during the diagnostic period.
Minutes and hours count, and if the clinical suspicion is high,
the workup should proceed on an emergent basis even if the
patient currently appears clinically stable. Indeed, delayed di-
agnosis has been associated with a dramatically worse outcome
(75). One strategy to expedite the workup is to rely upon
frozen sections to guide further diagnostic and therapeutic
decisions rather than waiting for xed and stained histopathol-
ogy from a biopsy. Use of frozen sections in this setting has
been shown to shorten the time to diagnosis and has been
associated with improved outcomes in two recent case series
(48, 53).
Role of Surgery
Mucormycosis is frequently rapidly progressive, and antifun-
gal therapy alone is often inadequate to control the infection.
The numerous agents of mucormycosis have a broad range of
susceptibilities to antifungal agents; some strains may be highly
resistant to amphotericin B. Furthermore, the hallmark angio-
invasion, thrombosis, and tissue necrosis of this disease result
in poor penetration of anti-infective agents to the site of in-
fection. Therefore, even if the causative organism is suscepti-
ble to the treating antifungal agent in vitro, the antifungal may
be ineffective in vivo. Finally, surgery is necessary due to the
massive amount of tissue necrosis occurring during mucormy-
cosis, which may not be prevented by killing the organism (63).
Surgical debridement of infected and necrotic tissue should be
performed on an urgent basis.
In rhinocerebral mucormycosis, early surgical excision of the
infected sinuses and appropriate debridement of the retro-
orbital space can often prevent the infection from extending
into the eye, thereby obviating the need for enucleation and
resulting in extremely high cure rates (85%) (107). Repeated
surgical exploration of the sinuses and orbit may be necessary
to ensure that all necrotic tissue has been debrided and the
infection has not progressed. Published case series continue to
support the need for surgical debridement to optimize out-
comes. For example, in a case series totaling 49 patients with
rhinocerebral mucormycosis, the mortality was 70% in cases
treated with antifungal agents alone versus 14% in cases
treated with antifungal agents plus surgery (75, 118). Similarly,
in a combined series of rhinocerebral, cutaneous, and pulmo-
nary mucormycosis, 11 of 17 (65%) patients treated with sur-
gery plus antifungal agents survived the infection, compared to
zero of seven (0%) patients treated with antifungal agents
alone (119). Clearly there is the potential for selection bias in
these case series, as patients who do not undergo surgery may
have fundamental differences in severity of illness or comor-
bidities. Nevertheless, the observational clinical data support
the concept that surgical debridement is necessary to optimize
cure rates.
In patients with pulmonary mucormycosis, surgical treat-
ment plus antifungal therapy also greatly improves outcome
compared to the use of antifungal therapy alone (10, 79, 116,
127, 150). In one series, the mortality of patients treated with
antifungal agents alone was 68%, versus 11% in patients
treated with antifungal agents plus surgery (150).
Finally, localized (nondisseminated) cutaneous mucormyco-
sis treated with aggressive surgical debridement and adjunctive
antifungal therapy has a mortality of 10% (4, 73). A similar
experience has been described with isolated renal mucormy-
cosis (172). However, because surgical debridement of necrotic
tissue is frequently highly disguring, if the patient survives the
acute phase of the disease, major reconstructive surgery may
be necessary.
Antifungal Therapy
A major obstacle for clinicians to choose among the current
available antifungal agents in treating mucormycosis is the lack
of available clinical trials (Table 2). Prospective interventional
study of mucormycosis has been impractical for several rea-
sons. First, although the disease is unusually deadly, it occurs at
a lower frequency relative to other opportunistic infections. By
extrapolation from studies of Aspergillus infection (52), which
is more common, dozens to possibly even hundreds of trial
sites and multiple years would be required to accrue sufcient
patients to adequately power a standard phase III superiority
study. Such a study would undoubtedly cost tens of millions of
dollars, and mucormycosis cases represent an insufcient po-
562 SPELLBERG ET AL. CLIN. MICROBIOL. REV.
tential market to spur any pharmaceutical company to sponsor
such a study.
An additional barrier to clinical trials of mucormycosis is the
abysmal rate of success of monotherapy. Because of this low
success rate, it might be considered unethical to randomize
patients in a clinical trial to any less intensive regimen (i.e.,
standard-dose versus high-dose monotherapy, monotherapy
versus combination therapy, etc.). For these reasons, prospec-
tive interventional trials have not been performed. Lacking any
signicant clinical trial data, physicians have been forced to
rely upon anecdotal case reports, limited retrospective reviews,
and unpublished observations in determining the rst-line
therapy for mucormycosis. Such reports are intrinsically sub-
ject to publication and observer bias and allow no comparison
of the relative efcacies of various treatment strategies. For
these reasons, animal models of mucormycosis are essential to
provide well-controlled comparative analyses of antifungal
therapies.
Several murine models have been developed to study mucor-
mycosis in vivo, including intravenous (59), intranasal (169), and
intrasinus (167) diabetic mice models. Additionally, neutropenic
(148), corticosteroid- (169), and deferoxamine-treated mouse
models (1) and a deferoxamine-treated guinea pig model (15, 16)
have been reported. More rarely, immunocompetent mice have
been studied (28). A variety of species have been utilized in these
models, including R. oryzae, R. microsporus, and Mucor and Ab-
sidia spp. There is no clear advantage to any one of these models
in evaluating the efcacy of different antifungal regimens, and
none of the models completely accurately recapitulates the nor-
mal route of infection (inhalation) of the majority of mucormy-
cosis infections. Nevertheless, given the lack of controlled clinical
trials for mucormycosis, these models are essential to evaluating
the relative merits of different antifungal strategies.
Polyenes. There have been no prospective randomized trials
to dene the optimal antifungal therapy for mucormycosis.
Until recently, only members of the polyene class, including
TABLE 2. Antifungal strategies for mucormycosis
Therapy Antifungal Pros Cons
Established therapies
Amphotericin B deoxycholate (AmB) 50 years experience Toxicity
Cidal Resistance seen in individual isolates
Liposomal amphotericin B (LAmB) Less toxic than AmB Most expensive polyene
Improved CNS penetration (47)
High-dose LAmB (15 mg/kg/day)
superior to AmB (1 mg/kg/day)
in murine model (59)
Superior to AmB in retrospective
clinical study (45)
Amphotericin B lipid complex
(ABLC)
Less toxic than AmB Inferior CNS penetration vs. LAmB
in one rabbit study (47)
Not superior to placebo or AmB in
murine model even at high doses
(up to 30 mg/kg/day) (62, 141)
No comparative clinical data
published
Investigational/adjunctive
therapies
Itraconazole Superior toxicity prole
Successful case reports (36, 125)
Poor activity in animal models
despite in vitro susceptibility (28,
29, 159)
Breakthrough mucormycosis
described during prophylactic
itraconazole (130)
Posaconazole More effective than itraconazole
in animal models (28, 148)
Not yet FDA approved
Successful case reports (65, 155) Static in vitro
Possible combination with
polyene therapy, but no data
available
Activity inferior to AmB in murine
models (28, 148)
Caspofungin Very low toxicity Virtually no clinical data for
mucormycosis
Synergistic with ABLC in murine
model (141)
Minimal activity as monotherapy in
murine model (60)
FDA approved (not for
mucormycosis)
Iron chelation Theoretical benet in No data available
combination with antifungals No effective agents are FDA
approved
Hyperbaric oxygen Nontoxic Not widely available
Successful case reports (22, 42) No controlled studies
Cytokine therapy In vitro activity (44) Limited data
Successful case reports (3) Expensive
Toxicity prole unclear
VOL. 18, 2005 NOVEL PERSPECTIVES ON MUCORMYCOSIS 563
amphotericin B deoxycholate and its lipid derivatives, had
been demonstrated to have activity against the agents of mu-
cormycosis. Furthermore, the various species that cause mu-
cormycosis have a broad range of susceptibilities to amphoter-
icin. Therefore, the recommended dose of amphotericin B
deoxycholate has been 1 to 1.5 mg/kg/day (61, 81, 145), which
results in a very high toxicity rate. Unfortunately, given the
underdeveloped state of the molecular biology of the Mucor-
ales, virtually nothing is known about the mechanisms of drug
resistance in these organisms. The molecular basis of drug
resistance in these organisms is an area that is highly merito-
rious of future research.
Fortunately, a series of new therapies that have the potential
to impact the outcomes of mucormycosis have or may soon
become available. The lipid formulations of amphotericin are
signicantly less nephrotoxic than amphotericin B deoxy-
cholate and can be safely administered at higher doses for a
longer period of time. However, the use of increased dosing for
lipid-based amphotericin also increases costs enormously. For
example, in contrast to US$5 per day for a 1-mg/kg daily dose
of amphotericin B deoxycholate, 5 to 15 mg/kg of lipid-based
amphotericins can cost between US$500 and US$3,000 per day
(142). Nevertheless, several case reports and case series of
patients with mucormycosis have documented successful out-
comes with either liposomal amphotericin B or amphotericin B
lipid complex (21, 38, 170, 173).
In our murine model of disseminated R. oryzae infection in
mice in diabetic ketoacidosis, high-dose liposomal amphoteri-
cin B (15 mg/kg/day) was considerably more effective than
amphotericin B deoxycholate (1 mg/kg/day), nearly doubling
the survival rate (59). Further in support of the rst-line role of
liposomal amphotericin are the results of a recent retrospec-
tive review of 120 cases of mucormycosis in patients with he-
matological malignancies (45). Treatment with liposomal am-
photericin was associated with a 67% survival rate, compared
to 39% survival when patients were treated with amphotericin
B deoxycholate (P 0.02,
2
). Given the retrospective nature
of this study, there is clear potential for several types of bias to
affect the outcome. Nevertheless, based on the combination of
these retrospective clinical data, the historically poor success
rates with amphotericin B deoxycholate, and the available an-
imal data showing superiority of liposomal amphotericin B
over amphotericin B deoxycholate, there is a developing con-
sensus that high doses of lipid formulation amphotericin are
the preferred initial antifungal therapy for patients with
mucormycosis.
Recent data are useful for guiding the choice of liposomal
amphotericin B versus amphotericin B lipid complex. A study
in rabbits (47) demonstrated that liposomal amphotericin B
penetrated brain parenchyma at levels more than vefold
above those of amphotericin B lipid complex. In fact, the brain
levels of amphotericin B lipid complex were lower than the
levels of amphotericin B deoxycholate, despite the fact that
amphotericin B lipid complex was administered at a vefold-
higher dose. Furthermore, in contrast to liposomal amphoter-
icin B, amphotericin B lipid complex (5, 20, or 30 mg/kg/day)
did not improve survival compared to placebo or amphotericin
B deoxycholate in our murine model of disseminated R. oryzae
infection (62, 141). Finally, in contrast to the recent review of
the effect of liposomal amphotericin B in clinical mucormyco-
sis, no comparable data set has been published reviewing the
effect of amphotericin B lipid complex in this setting.
Until direct comparisons of the efcacy of liposomal ampho-
tericin B versus amphotericin B lipid complex are published,
denitive conclusions regarding their relative efcacies for mu-
cormycosis cannot be made. For now, the pharmacokinetic
data, animal model data, and retrospective clinical data all
support the rst-line use of high-dose liposomal amphotericin
B for mucormycosis, particularly for cases of central nervous
system disease, with amphotericin B lipid complex serving as a
reasonable second-line agent. Therefore, a rational approach
to the treatment of life-threatening mucormycosis infections is
emergent surgical consultation followed by immediate initia-
tion of liposomal amphotericin B at 10 to 15 mg/kg/day.
Azoles. Itraconazole is the only marketed azole drug that has
in vitro activity against Mucorales (147). There are case reports
of successful therapy with itraconazole alone (36, 125). How-
ever, as mentioned above, itraconazole prophylaxis has been
described as a risk factor for breakthrough mucormycosis
(130). Furthermore, animal studies revealed that itraconazole
was completely ineffective against Rhizopus and Mucor spp.
even though the isolates were susceptible in vitro (28, 29, 159).
In contrast, itraconazole did have activity in vivo against a
hypersusceptible strain of Absidia (MIC, 0.03 g/ml). There-
fore, itraconazole should not be considered a rst-line agent
against mucormycosis, but its use may be considered as ad-
junctive therapy in selected situations where highly susceptible
fungi have been cultured.
Voriconazole, a recently approved second-generation
broad-spectrum triazole, is not active against the Mucorales in
vitro (147). Conversely, posaconazole and ravuconazole, inves-
tigational triazoles, have promising in vitro activity against the
agents of mucormycosis (120, 147). In experimental animal
models of disseminated mucormycosis, posaconazole is more
efcacious than itraconazole but less efcacious than ampho-
tericin B deoxycholate (28, 148). There are increasing reports
of salvage posaconazole therapy for refractory mucormycosis.
Successful outcomes have been seen in patients with rhinoce-
rebral mucormycosis in conjunction with amphotericin (65),
and in a heart/kidney transplant patient who failed on ampho-
tericin therapy (155). Further data are needed to determine
whether posaconazole, alone or in combination with ampho-
tericin, may be useful for the treatment of mucormycosis.
Echinocandins. Caspofungin, the rst member of the novel
echinocandin class of antifungal drugs to be marketed in the
United States, has minimal activity against the agents of mu-
cormycosis when tested in vitro by standard techniques (31,
39). However, the accuracy of current in vitro testing of caspo-
fungin activity against molds remains unclear. It is now known
that R. oryzae expresses the target enzyme for caspofungin
(60), and in the murine model of disseminated mucormycosis,
caspofungin did have limited activity against R. oryzae (60).
Furthermore, we found that the combination of caspofungin (1
mg/kg/day) plus amphotericin B lipid complex (5 mg/kg/day)
was synergistic (141). While either therapy alone mediated no
survival benet, the combination signicantly improved sur-
vival (50% survival for the combination versus 0% for placebo,
caspofungin alone, or amphotericin B lipid complex alone).
Clinical experience with caspofungin in the setting of mu-
564 SPELLBERG ET AL. CLIN. MICROBIOL. REV.
cormycosis is extremely limited. In a report of a patient with
necrotizing pancreatitis and abdominal mucormycosis, the ad-
dition of caspofungin to liposomal amphotericin did not im-
prove the outcome, but the patient had already clinically pro-
gressed on liposomal amphotericin prior to initiation of
caspofungin (165). As mentioned, there have also been reports
of breakthrough mucormycosis in patients receiving either
caspofungin alone (133) or caspofungin plus voriconazole (13).
Conversely, the related experimental echinocandin micafungin
has been added on a salvage basis to a patient failing antifungal
therapy for craniofacial mucormycosis (67). The patient began
responding to therapy shortly after the addition of micafungin
and was ultimately cured. These data suggest that echinocan-
dins may have a role as a second agent, especially in combina-
tion with a polyene, in serious cases of mucormycosis. More
study of the utility of echinocandins in this setting is needed.
Novel Iron Chelators
The central role of iron metabolism in the pathogenesis of
mucormycosis suggests the possibility of utilizing effective iron
chelators as adjunctive antifungal therapy. In fact, two exper-
imental iron chelators have been studied in vitro against R.
oryzae (16). In contrast to deferoxamine, the other iron chela-
tors did not allow the organism to take up iron and did not
support its growth in vitro in the presence of iron. Further-
more, while deferoxamine signicantly worsened disseminated
R. oryzae infection in guinea pigs, one of the other chelators
had no impact on the in vivo infection and one of them more
than doubled the mean survival time (16). The latter agent is
approved for use in India and Europe and is available on a
compassionate-use basis for iron overload in the United States
and Canada. The potential for this iron chelator to serve as
adjunctive therapy in combination with other antifungal agents
is under active investigation.
Other Adjunctive Therapies
Case reports have suggested that hyperbaric oxygen may be
a benecial adjunct to the standard surgical and medical anti-
fungal therapy of mucormycosis, particularly for patients with
rhinocerebral disease (22, 42). It is hypothesized that hyper-
baric oxygen might be useful for treating mucormycosis in
conjunction with standard therapy because higher oxygen pres-
sure improves the ability of neutrophils to kill the organism
(26). Additionally, high oxygen pressure inhibits the germina-
tion of fungal spores and growth of mycelia in vitro (131).
Whether hyperbaric oxygen actually improves the outcome of
patients with mucormycosis remains to be established through
appropriately controlled prospective clinical trials.
The role of adjunctive cytokine therapy for mucormycosis
has been understudied. Cytokines that activated phagocytic
activity, such as gamma interferon and granulocyte-macro-
phage colony-stimulating factor, increase the ability of phago-
cytes to kill agents of mucormycosis in vitro (44). A recent case
report suggested a favorable outcome in a leukemic child with
rhinocerebral mucormycosis following the addition of gamma
interferon and granulocyte-macrophage colony-stimulating
factor to the regimen (3). Further studies of cytokines that
activate host phagocyte function are warranted for this disease.
PROGNOSIS
Previously, cases of rhinocerebral mucormycosis were al-
most consistently fatal (84). Although the mortality rate of
rhinocerebral disease remains high, the infection can be cured
when diagnosed early and treated with aggressive surgery and
antifungal agents (discussed further below) (20, 114, 119). Re-
cent series have described a mortality of approximately 40% in
diabetics with rhinocerebral mucormycosis (107, 118) and a
similar survival rate for rhinocerebral disease in patients with
hematological malignancies (45). Of note, the prognosis is
much better if the disease has not penetrated beyond the sinus
prior to surgical debridement; in local sinonasal disease, the
mortality has been reported to be 10% (107). The nature of
the underlying disease and the reversibility of the immune
dysfunction are also important determinants of survival. One
study showed that 75% of patients with rhinocerebral disease
who had no underlying immune compromise survived, while
60% of those with diabetes and only 20% of patients with other
immunocompromised states were cured (14).
The overall survival rate of patients with mucormycosis is
approximately 50%, although survival rates of up to 85% have
been reported more recently. Much of the variability in out-
come is due to the various forms of the disease. Rhinocerebral
mucormycosis has a higher survival rate than does pulmonary
or disseminated mucormycosis because the rhinocerebral dis-
ease can frequently be diagnosed earlier and the most common
underlying cause, diabetic ketoacidosis, can be treated readily
(114). In contrast, pulmonary mucormycosis has a high mor-
tality (65% at 1 year) (94) because it is difcult to diagnose
and it frequently occurs in neutropenic patients. For example,
in one large study, only 44% with pulmonary mucormycosis
were diagnosed premortem, and the overall survival rate was
only 20% (150). In a separate study in which 93% of the
infections were diagnosed premortem, the survival rate was
73% (114). Mortality in patients with disseminated disease
approaches 100%, in large part because surgical removal of
infected tissues is not feasible and in part because these pa-
tients tend to be the most highly immunocompromised (e.g.,
allogeneic stem cell transplantation).
CONCLUSIONS
Mucormycosis is an increasingly common infection in immu-
nocompromised patients. The central role of iron in the or-
ganisms pathogenesis has only recently been appreciated. The
interaction between the Mucorales and endothelial cells is also
beginning to be understood. Both of these pathogenetic fea-
tures of disease may be amenable to novel therapeutic inter-
vention in the future. Currently, novel regimens for the treat-
ment of mucormycosis include combination lipid-based
amphotericin plus either an echinocandin or itraconazole or
both. As well, compassionate-use posaconazole is currently
available, and its potential for combination therapy with a
polyene, caspofungin, or both is meritorious for study. In the
future, novel iron chelator therapy may be useful as an adjunct
to standard antifungal therapy. Finally, prompt diagnosis, re-
versal of predisposing conditions, and aggressive surgical de-
bridement remain cornerstones of therapy for this deadly dis-
ease.
VOL. 18, 2005 NOVEL PERSPECTIVES ON MUCORMYCOSIS 565
REFERENCES
1. Abe, F., H. Inaba, T. Katoh, and M. Hotchi. 1990. Effects of iron and
desferrioxamine on Rhizopus infection. Mycopathologia 110:8791.
2. Abedi, E., A. Sismanis, K. Choi, and P. Pastore. 1984. Twenty-ve years
experience treating cerebro-rhino-orbital mucormycosis. Laryngoscope 94:
10601062.
3. Abzug, M. J., and T. J. Walsh. 2004. Interferon-gamma and colony-stimu-
lating factors as adjuvant therapy for refractory fungal infections in chil-
dren. Pediatr. Infect. Dis. J. 23:769773.
4. Adam, R. D., G. Hunter, J. DiTomasso, and G. Comerci, Jr. 1994. Mucor-
mycosis: emerging prominence of cutaneous infections. Clin. Infect. Dis.
19:6776.
5. Alsuwaida, K. 2002. Primary cutaneous mucormycosis complicating the use
of adhesive tape to secure the endotracheal tube. Can. J. Anaesth. 49:880
882.
6. Amin, S. B., R. M. Ryan, L. A. Metlay, and W. J. Watson. 1998. Absidia
corymbifera infections in neonates. Clin. Infect. Dis. 26:990992.
7. Anaissie, E. J., and A. H. Shikhani. 1985. Rhinocerebral mucormycosis with
internal carotid occlusion: report of two cases and review of the literature.
Laryngoscope 95:11071113.
8. Andrews, D. R., A. Allan, and R. I. Larbalestier. 1997. Tracheal mucormy-
cosis. Ann. Thorac. Surg. 63:230232.
9. Artis, W. M., J. A. Fountain, H. K. Delcher, and H. E. Jones. 1982. A
mechanism of susceptibility to mucormycosis in diabetic ketoacidosis: trans-
ferrin and iron availability. Diabetes 31:11091114.
10. Asai, K., K. Suzuki, T. Takahashi, Y. Ito, T. Kazui, and Y. Kita. 2003.
Pulmonary resection with chest wall removal and reconstruction for inva-
sive pulmonary mucormycosis during antileukemia chemotherapy. Jpn.
J. Thorac. Cardiovasc. Surg. 51:163166.
11. Baraia, J., P. Munoz, J. C. Bernaldo deq Uiros, and E. Bouza. 1995.
Cutaneous mucormycosis in a heart transplant patient associated with a
peripheral catheter. Eur. J. Clin. Microbiol. and Infect. Dis. 14:813815.
12. Bearer, E. A., P. R. Nelson, M. Y. Chowers, and C. E. Davis. 1994. Cuta-
neous zygomycosis caused by Saksenaea vasiformis in a diabetic patient.
J. Clin. Microbiol. 32:18231824.
13. Blin, N., N. Morineau, F. Gaillard, O. Morin, N. Milpied, J. L. Harousseau,
and P. Moreau. 2004. Disseminated mucormycosis associated with invasive
pulmonary aspergillosis in a patient treated for post-transplant high-grade
non-Hodgkins lymphoma. Leukemia Lymphoma 45:21612163.
14. Blitzer, A., and W. Lawson. 1993. Fungal infections of the nose and para-
nasal sinuses. Part I. Otolaryngol. Clin. North Am. 26:10071035.
15. Boelaert, J. R., M. de Locht, J. Van Cutsem, V. Kerrels, B. Cantinieaux, A.
Verdonck, H. W. Van Landuyt, and Y. J. Schneider. 1993. Mucormycosis
during deferoxamine therapy is a siderophore-mediated infection. In vitro
and in vivo animal studies. J. Clin. Investig. 91:19791986.
16. Boelaert, J. R., J. Van Cutsem, M. de Locht, Y. J. Schneider, and R. R.
Crichton. 1994. Deferoxamine augments growth and pathogenicity of Rhi-
zopus, while hydroxypyridinone chelators have no effect. Kidney Int. 45:
667671.
17. Bouchara, J. P., N. A. Oumeziane, J. C. Lissitzky, G. Larcher, G. Tronchin,
and D. Chabasse. 1996. Attachment of spores of the human pathogenic
fungus Rhizopus oryzae to extracellular matrix components. Eur. J. Cell
Biol. 70:7683.
18. Boyd, A. S., B. Wiser, H. H. Sams, and L. E. King. 2003. Gangrenous
cutaneous mucormycosis in a child with a solid organ transplant: a case
report and review of the literature. Pediatr. Dermatol. 20:411415.
19. Brullet, E., X. Andreu, J. Elias, J. Roig, and M. Cervantes. 1993. Gastric
mucormycosis in a patient with acquired immunodeciency syndrome [let-
ter]. Gastrointestinal Endosc. 39:106107.
20. Bullock, J. D., L. M. Jampol, and A. J. Fezza. 1974. Two cases of orbital
phycomycosis with recovery. Am. J. Ophthalmol. 78:811815.
21. Cagatay, A. A., S. S. Oncu, S. S. Calangu, T. T. Yildirmak, H. H. Ozsut, and
H. H. Eraksoy. 2001. Rhinocerebral mucormycosis treated with 32 gram
liposomal amphotericin B and incomplete surgery: a case report. BMC
Infect. Dis. 1:22.
22. Chassaing, N., L. Valton, M. Kany, E. Bonnet, E. Uro-Coste, M. B. Delisle,
P. Bousquet, and G. Geraud. 2003. [Rhino-cerebral fungal infection suc-
cessfully treated with supplementary hyperbaric oxygen therapy]. Rev. Neu-
rol. (Paris) 159:11781180.
23. Chinn, R. Y., and R. D. Diamond. 1982. Generation of chemotactic factors
by Rhizopus oryzae in the presence and absence of serum: relationship to
hyphal damage mediated by human neutrophils and effects of hyperglyce-
mia and ketoacidosis. Infect. Immun. 38:11231129.
24. Cohen-Abbo, A., P. M. Bozeman, and C. C. Patrick. 1993. Cunninghamella
infections: review and report of two cases of Cunninghamella pneumonia in
immunocompromised children. Clin. Infect. Dis. 17:173177.
25. Connor, B. A., R. J. Anderson, and J. W. Smith. 1979. Mucor mediastinitis.
Chest 75:524526.
26. Couch, L., F. Theilen, and J. T. Mader. 1988. Rhinocerebral mucormycosis
with cerebral extension successfully treated with adjunctive hyperbaric ox-
ygen therapy. Arch. Otolaryngol. Head Neck Surg. 114:791794.
27. Craig, N. M., F. L. Lueder, J. M. Pensler, B. S. Bean, M. L. Petrick, R. B.
Thompson, and L. R. Eramo. 1994. Disseminated Rhizopus infection in a
premature infant. Pediatr. Dermatol. 11:346350.
28. Dannaoui, E., J. F. Meis, D. Loebenberg, and P. E. Verweij. 2003. Activity
of posaconazole in treatment of experimental disseminated zygomycosis.
Antimicrob. Agents Chemother. 47:36473650.
29. Dannaoui, E., J. Meletiadis, J. W. Mouton, J. F. Meis, and P. E. Verweij.
2003. In vitro susceptibilities of zygomycetes to conventional and new an-
tifungals. J. Antimicrob. Chemother. 51:4552.
30. de Locht, M., J. R. Boelaert, and Y. J. Schneider. 1994. Iron uptake from
ferrioxamine and from ferrirhizoferrin by germinating spores of Rhizopus
microsporus. Biochem. Pharmacol. 47:18431850.
31. Del Poeta, M., W. A. Schell, and J. R. Perfect. 1997. In vitro antifungal
activity of pneumocandin L-743,872 against a variety of clinically important
molds. Antimicrob. Agents Chemother. 41:18351836.
32. Dhiwakar, M., A. Thakar, and S. Bahadur. 2003. Improving outcomes in
rhinocerebral mucormycosisearly diagnostic pointers and prognostic fac-
tors. J. Laryngol Otol. 117:861865.
33. Diamond, R. D., C. C. Haudenschild, and N. F. Erickson 3rd. 1982. Mono-
cyte-mediated damage to Rhizopus oryzae hyphae in vitro. Infect. Immun.
38:292297.
34. Diekema, D. J., S. A. Messer, R. J. Hollis, R. N. Jones, and M. A. Pfaller.
2003. Activities of caspofungin, itraconazole, posaconazole, ravuconazole,
voriconazole, and amphotericin B against 448 recent clinical isolates of
lamentous fungi. J. Clin. Microbiol. 41:36233626.
35. Diven, S. C., C. A. Angel, H. K. Hawkins, J. L. Rowen, and K. E. Shattuck.
2004. Intestinal zygomycosis due to Absidia corymbifera mimicking necro-
tizing enterocolitis in a preterm neonate. J. Perinatol. 24:794796.
36. Eisen, D. P., and J. Robson. 2004. Complete resolution of pulmonary
Rhizopus oryzae infection with itraconazole treatment: more evidence of
the utility of azoles for zygomycosis. Mycoses 47:159162.
37. Eiser, A. R., R. F. Slifkin, and M. S. Neff. 1987. Intestinal mucormycosis in
hemodialysis patients following deferoxamine. Am. J. Kidney Dis. 10:7173.
38. Ericsson, M., M. Anniko, H. Gustafsson, C. A. Hjalt, R. Stenling, and A.
Tarnvik. 1993. A case of chronic progressive rhinocerebral mucormycosis
treated with liposomal amphotericin B and surgery [letter]. Clin. Infect.
Dis. 16:585586.
39. Espinel-Ingroff, A. 1998. Comparison of In vitro activities of the new tria-
zole SCH56592 and the echinocandins MK-0991 (L-743,872) and
LY303366 against opportunistic lamentous and dimorphic fungi and
yeasts. J. Clin. Microbiol. 36:29502956.
40. Fatterpekar, G., S. Mukherji, A. Arbealez, S. Maheshwari, and M. Castillo.
1999. Fungal diseases of the paranasal sinuses. Semin. Ultrasound CT MR
20:391401.
41. Fujii, T., N. Takata, S. Katsutani, and A. Kimura. 2003. Disseminated
mucormycosis in an acquired immunodeciency syndrome (AIDS) patient.
Intern. Med. 42:129130.
42. Garcia-Covarrubias, L., D. M. Barratt, R. Bartlett, and K. Van Meter.
2004. [Treatment of mucormycosis with adjunctive hyperbaric oxygen: ve
cases treated at the same institution and review of the literature]. Rev.
Investig. Clin. 56:5155.
43. Gartenberg, G., E. J. Bottone, G. T. Keusch, and I. Weitzman. 1978. Hos-
pital-acquired mucormycosis (Rhizopus rhizopodiformis) of skin and sub-
cutaneous tissue: epidemiology, mycology and treatment. N. Engl. J. Med.
299:11151118.
44. Gil-Lamaignere, C., M. Simitsopoulou, E. Roilides, A. Maloukou, R. M.
Winn, and T. J. Walsh. 2005. Interferon-gamma and granulocyte-macro-
phage colony-stimulating factor augment the activity of polymorphonuclear
leukocytes against medically important zygomycetes. J Infect. Dis. 191:
11801187.
45. Gleissner, B., A. Schilling, I. Anagnostopolous, I. Siehl, and E. Thiel. 2004.
Improved outcome of zygomycosis in patients with hematological diseases?
Leukemia Lymphoma 45:13511360.
46. Goodill, J. J., and J. G. Abuelo. 1987. Mucormycosisa new risk of defer-
oxamine therapy in dialysis patients with aluminum or iron overload? [let-
ter]. N. Engl. J. Med. 317:54.
47. Groll, A. H., N. Giri, V. Petraitis, R. Petraitiene, M. Candelario, J. S.
Bacher, S. C. Piscitelli, and T. J. Walsh. 2000. Comparative efcacy and
distribution of lipid formulations of amphotericin B in experimental Can-
dida albicans infection of the central nervous system. J. Infect. Dis. 182:
274282.
48. Guevara, N., D. Roy, C. Dutruc-Rosset, J. Santini, P. Hofman, and L.
Castillo. 2004. Mucormycosisearly diagnosis and treatment. Rev. Laryn-
gol. Otol. Rhinol. (Bord) 125:127131.
49. Harada, M., T. Manabe, K. Yamashita, and N. Okamoto. 1992. Pulmonary
mucormycosis with fatal massive hemoptysis. Acta Pathol. Jpn. 42:4955.
50. Harper, J. J., C. Coulter, G. R. Lye, and G. R. Nimmo. 1996. Rhizopus and
tongue depressors [letter; comment]. Lancet 348:1250.
51. Helenglass, G., J. A. Elliott, and N. P. Lucie. 1981. An unusual presentation
of opportunistic mucormycosis. Br. Med. J. (Clin. Res. ed.) 282:108109.
52. Herbrecht, R., D. W. Denning, T. F. Patterson, J. E. Bennett, R. E. Greene,
J. W. Oestmann, W. V. Kern, K. A. Marr, P. Ribaud, O. Lortholary, R.
566 SPELLBERG ET AL. CLIN. MICROBIOL. REV.
Sylvester, R. H. Rubin, J. R. Wingard, P. Stark, C. Durand, D. Caillot, E.
Thiel, P. H. Chandrasekar, M. R. Hodges, H. T. Schlamm, P. F. Troke, and
B. de Pauw. 2002. Voriconazole versus amphotericin B for primary therapy
of invasive aspergillosis. N. Engl. J. Med. 347:408415.
53. Hofman, V., L. Castillo, F. Betis, N. Guevara, M. Gari-Toussaint, and P.
Hofman. 2003. Usefulness of frozen section in rhinocerebral mucormycosis
diagnosis and management. Pathology 35:212216.
54. Holzel, H., S. Macqueen, A. MacDonald, S. Alexander, C. K. Campbell,
E. M. Johnson, and D. W. Warnock. 1998. Rhizopus microsporus in wooden
tongue depressors: a major threat or minor inconvenience? J. Hosp. Infect.
38:113118.
55. Hosseini, M., and J. Lee. 1998. Gastrointestinal mucormycosis mimicking
ischemic colitis in a patient with systemic lupus erythematosus. Am. J.
Gastroenterol. 93:13601362.
56. Hotchi, M., M. Okada, and T. Nasu. 1980. Present state of fungal infections
in autopsy cases in Japan. Am. J. Clin. Pathol. 74:410416.
57. Husain, S., B. D. Alexander, P. Munoz, R. K. Avery, S. Houston, T. Pruett,
R. Jacobs, E. A. Dominguez, J. G. Tollemar, K. Baumgarten, C. M. Yu,
M. M. Wagener, P. Linden, S. Kusne, and N. Singh. 2003. Opportunistic
mycelial fungal infections in organ transplant recipients: emerging impor-
tance of non-Aspergillus mycelial fungi. Clin. Infect. Dis. 37:221229.
58. Hussain, S., N. Salahuddin, I. Ahmad, I. Salahuddin, and R. Jooma. 1995.
Rhinocerebral invasive mycosis: occurrence in immunocompetent individ-
uals. Eur. J. Radiol. 20:151155.
59. Ibrahim, A. S., V. Avanessian, B. Spellberg, and J. E. Edwards, Jr. 2003.
Liposomal amphotericin B, and not amphotericin B deoxycholate, improves
survival of diabetic mice infected with Rhizopus oryzae. Antimicrob. Agents
Chemother. 47:33433344.
60. Ibrahim, A. S., J. C. Bowman, V. Avanessian, K. Brown, B. Spellberg, J. J.
Edwards, and C. M. Douglas. 2005. Caspofungin inhibits Rhizopus oryzae
1,3D-glucan synthase, lowers quantitative PCR-measured brain burden,
and improves survival at a low but not a high dose during murine dissem-
inated zygomycosis. Antimicrob. Agents Chemother. 49:721727.
61. Ibrahim, A. S., J. E. J. Edwards, and S. G. Filler. 2003. Zygomycosis, p.
241251. In W. E. Dismukes, P. G. Pappas, and J. D. Sobel (ed.), Clinical
mycology. Oxford University Press, New York, N.Y.
62. Ibrahim, A. S., S. Klein, H. Lee, Y. Fu, H. Waskin, and J. Edwards, Jr. 2000.
Presented at the 40th Interscience Conference on Antimicrobial Agents
and Chemotherapy, Toronto, Canada.
63. Ibrahim, A. S., B. Spellberg, V. Avanessian, Y. Fu, and J. E. Edwards. 2005.
Rhizopus oryzae adheres to, is phagocytosed by, and damages endothelial
cells in vitro. Infect. Immun. 73:778783.
64. Ibrahim, A. S., B. Spellberg, V. Avanessian, Y. Fu, and J. E. Edwards, Jr.
2005. Rhizopus oryzae adheres to, is phagocytosed by, and damages endo-
thelial cells in vitro. Infect Immun 73:778783.
65. Ide, L., I. Buysschaert, H. Demuynck, R. De Man, A. Verlinde, E. De Laere,
and I. Surmont. 2004. Zygomycosis in neutropenic patients with past As-
pergillus infection: a role for posaconazole? Clin. Microbiol. Infect. 10:862
863.
66. Imhof, A., S. A. Balajee, D. N. Fredricks, J. A. Englund, and K. A. Marr.
2004. Breakthrough fungal infections in stem cell transplant recipients
receiving voriconazole. Clin. Infect. Dis. 39:743746.
67. Jacobs, P., L. Wood, A. Du Toit, and K. Esterhuizen. 2003. Eradication of
invasive mucormycosiseffectiveness of the Echinocandin FK463. Hematol-
ogy 8:119123.
68. Kamalam, A., and A. S. Thambiah. 1980. Cutaneous infection by Syncepha-
lastrum. Sabouraudia 18:1920.
69. Kauffman, C. A. 2004. Zygomycosis: reemergence of an old pathogen. Clin.
Infect. Dis. 39:588590.
70. Kawakami, K., Y. Watanabe, and S. Kadowaki. 2004. [Early onset invasive
pulmonary zygomycosis following allogeneic peripheral blood stem cell
transplantation in a patient with therapy-related myelodysplastic syn-
drome]. Rinsho Ketsueki 45:319321.
71. Kecskes, S., G. Reynolds, and G. Bennett. 1997. Survival after gastrointes-
tinal mucormycosis in a neonate. J. Paediatr. Child Health 33:356359.
72. Kemna, M. E., R. C. Neri, R. Ali, and I. F. Salkin. 1994. Cokeromyces
recurvatus, a mucoraceous zygomycete rarely isolated in clinical laborato-
ries. J. Clin. Microbiol. 32:843845.
73. Kerr, O. A., C. Bong, C. Wallis, and M. J. Tidman. 2004. Primary cutaneous
mucormycosis masquerading as pyoderma gangrenosum. Br. J. Dermatol.
150:12121213.
74. Khardori, N., S. Hayat, K. Rolston, and G. P. Bodey. 1989. Cutaneous
Rhizopus and Aspergillus infections in ve patients with cancer. Arch.
Dermatol. 125:952956.
75. Khor, B. S., M. H. Lee, H. S. Leu, and J. W. Liu. 2003. Rhinocerebral
mucormycosis in Taiwan. J. Microbiol. Immunol. Infect. 36:266269.
76. Kline, M. W. 1985. Mucormycosis in children: review of the literature and
report of cases. Pediatr. Infect. Dis. 4:672676.
77. Knoop, C., M. Antoine, J. L. Vachie ry, G. Depre , C. Alonso-Vega, M.
Struelens, J. L. Van Laethem, P. Lingier, N. Nagy, F. Jacobs, M. R.
Kramer, and M. Estenne. 1998. Gastric perforation due to mucormycosis
after heart-lung and heart transplantation. Transplant. 66:932935.
78. Kontoyianis, D. P., S. Vartivarian, E. J. Anaissie, G. Samonis, G. P. Bodey,
and M. Rinaldi. 1994. Infections due to Cunninghamella bertholletiae in
patients with cancer: report of three cases and review. Clin. Infect. Dis.
18:925928.
79. Kontoyiannis, D. P., V. C. Wessel, G. P. Bodey, and K. V. Rolston. 2000.
Zygomycosis in the 1990s in a tertiary-care cancer center. Clin. Infect. Dis.
30:851856.
80. Kordy, F. N., I. Z. Al-Mohsen, F. Hashem, E. Almodovar, S. Al Hajjar, and
T. J. Walsh. 2004. Successful treatment of a child with posttraumatic ne-
crotizing fasciitis caused by Apophysomyces elegans: case report and review
of literature. Pediatr. Infect. Dis. J. 23:877879.
81. Kwon-Chung, K. J., and J. E. Bennett. 1992. Medical mycology, p. 524559.
Lea & Febiger, Philadelphia, Pa.
82. Kwon-Chung, K. J., R. C. Young, and M. Orlando. 1975. Pulmonary mu-
cormycosis caused by Cunninghamella elegans in a patient with chronic
myelogenous leukemia. Am. J. Clin. Pathol. 64:544548.
83. Larsen, K., C. von Buchwald, B. Ellefsen, and D. Francis. 2003. Unex-
pected expansive paranasal sinus mucormycosis. ORL J. Otorhinolaryngol.
Relat. Spec. 65:5760.
84. LeCompte, P. M., and W. A. Miessner. 1947. Mucormycosis of the central
nervous system associated with hemochromatosis. Am. J. Pathol. 23:673
676.
85. Lee, F. Y., S. B. Mossad, and K. A. Adal. 1999. Pulmonary mucormycosis:
the last 30 years. Arch. Intern. Med. 159:13011309.
86. Leong, A. S. Y. 1978. Granulomatous mediastinitis due to Rhizopus species.
Am. J. Clin. Pathol. 70:103107.
87. Leong, K. W., B. Crowley, B. White, G. M. Crotty, D. S. OBriain, C. Keane,
and S. R. McCann. 1997. Cutaneous mucormycosis due to Absidia corym-
bifera occurring after bone marrow transplantation. Bone Marrow Trans-
plant. 19:513515.
88. Lowe, J. T., Jr., and W. R. Hudson. 1975. Rhincerebral phycomycosis and
internal carotid artery thrombosis. Arch. Otolaryngol. 101:100103.
89. Lye, G. R., G. Wood, and G. Nimmo. 1996. Subcutaneous zygomycosis due
to Saksenaea vasiformis: rapid isolate identication using a modied sporu-
lation technique. Pathology 28:364365.
90. Maertens, J., H. Demuynck, E. K. Verbeken, P. Zache e, G. E. Verhoef, P.
Vandenberghe, and M. A. Boogaerts. 1999. Mucormycosis in allogeneic
bone marrow transplant recipients: report of ve cases and review of the
role of iron overload in the pathogenesis. Bone Marrow Transplant. 24:
307312.
91. Maliwan, N., C. V. Reyes, and J. W. Rippon. 1984. Osteomyelitis secondary
to cutaneous mucormycosis. Report of a case and a review of the literature.
Am. J. Dermatopathol. 6:479481.
92. Maravi-Poma, E., J. L. Rodriguez-Tudela, J. G. de Jalon, A. Manrique-
Larralde, L. Torroba, J. Urtasun, B. Salvador, M. Montes, E. Mellado, F.
Rodriguez-Albarran, and A. Pueyo-Royo. 2004. Outbreak of gastric mucor-
mycosis associated with the use of wooden tongue depressors in critically ill
patients. Intensive Care Med. 30:724728.
93. Marchevsky, A. M., E. J. Bottone, S. A. Geller, and D. K. Giger. 1980. The
changing spectrum of disease, etiology, and diagnosis of mucormycosis.
Hum. Pathol. 11:457464.
94. Marr, K. A., R. A. Carter, F. Crippa, A. Wald, and L. Corey. 2002. Epide-
miology and outcome of mould infections in hematopoietic stem cell trans-
plant recipients. Clin. Infect. Dis. 34:909917.
95. Martinez, E. J., M. R. Cancio, J. T. t. Sinnott, A. L. Vincent, and S. G.
Brantley. 1997. Nonfatal gastric mucormycosis in a renal transplant recip-
ient. South. Medical J. 90:341344.
96. Marty, F. M., L. A. Cosimi, and L. R. Baden. 2004. Breakthrough zygomy-
cosis after voriconazole treatment in recipients of hematopoietic stem-cell
transplants. N. Engl. J. Med. 350:950952.
97. Mazza, D., J. Gugenheim, E. Baldini, and J. Mouiel. 1999. Gastrointestinal
mucormycosis and liver transplantation; a case report and review of the
literature [letter]. Transplant. Int. 12:297298.
98. McAdams, H. P., M. Rosado de Christenson, D. C. Strollo, and E. F. Patz,
Jr. 1997. Pulmonary mucormycosis: radiologic ndings in 32 cases. AJR
Am. J. Roentgenol. 168:15411548.
99. McNulty, J. S. 1982. Rhinocerebral mucormycosis: predisposing factors.
Laryngoscope 92:11401143.
100. Mead, J. H., G. P. Lupton, C. L. Dillavou, and R. B. Odom. 1979. Cutane-
ous Rhizopus infection. Occurrence as a postoperative complication asso-
ciated with an elasticized adhesive dressing. JAMA 242:272274.
101. Mori, T., M. Egashira, N. Kawamata, K. Oshimi, K. Nakamura, T. Oguri,
H. Aida, A. Hiruma, and M. Ichinohe. 2003. Zygomycosis: two case reports
and review of reported cases in the literature in Japan. Nippon Ishinkin
Gakkai Zasshi 44:163179.
102. Morrison, V. A., and P. B. McGlave. 1993. Mucormycosis in the BMT
population. Bone Marrow Transplant. 11:383388.
103. Murray, H. W. 1975. Pulmonary mucormycosis with massive fatal hemop-
tysis. Chest 68:6568.
104. Mutsukura, K., Y. Tsuboi, A. Imamura, F. Fujiki, and T. Yamada. 2004.
[Garcin syndrome in a patient with rhinocerebral mucormycosis]. No To
Shinkei 56:231235.
VOL. 18, 2005 NOVEL PERSPECTIVES ON MUCORMYCOSIS 567
105. Nagy-Agren, S. E., P. Chu, G. J. Smith, H. A. Waskin, and F. L. Altice. 1995.
Zygomycosis (mucormycosis) and HIV infection: report of three cases and
review. J. Acquir. Immune Dec. Syndr. Hum. Retrovirol. 10:441449.
106. Nissen, M. D., A. K. Jana, M. J. Cole, J. M. Grierson, and G. L. Gilbert.
1999. Neonatal gastrointestinal mucormycosis mimicking necrotizing en-
terocolitis. Acta Paediatr. 88:12901293.
107. Nithyanandam, S., M. S. Jacob, R. R. Battu, R. K. Thomas, M. A. Correa,
and O. DSouza. 2003. Rhino-orbito-cerebral mucormycosis. A retrospec-
tive analysis of clinical features and treatment outcomes. Indian J. Oph-
thalmol. 51:231236.
108. Nussbaum, E. S., and W. A. Hall. 1994. Rhinocerebral mucormycosis:
changing patterns of disease. Surg. Neurol. 41:152156.
109. OBrien, T. J., and P. McKelvie. 1994. Rhinocerebral mucormycosis pre-
senting as periorbital cellulitis with blindness: report of 2 cases. Clin. Exp.
Neurol. 31:6878.
110. Ogunlana, E. O. 1975. Fungal air spora at Ibadan, Nigeria. Appl. Microbiol.
29:458463.
111. Oliver, M. R., W. C. Van Voorhis, M. Boeckh, D. Mattson, and R. A.
Bowden. 1996. Hepatic mucormycosis in a bone marrow transplant recipi-
ent who ingested naturopathic medicine. Clin. Infect. Dis. 22:521524.
112. Oren, I. 2005. Breakthrough zygomycosis during empirical voriconazole
therapy in febrile patients with neutropenia. Clin. Infect. Dis. 40:770771.
113. Pagano, L., P. Ricci, A. Nosari, A. Tonso, M. Buelli, M. Montillo, L.
Cudillo, A. Cenacchi, C. Savignana, and L. Melillo. 1995. Fatal haemoptysis
in pulmonary lamentous mycosis: an underevaluated cause of death in
patients with acute leukaemia in haematological complete remission. A
retrospective study and review of the literature. Gimema Infection Program
(Gruppo Italiano Malattie Ematologiche dellAdulto). Br. J. Haematol.
89:500505.
114. Parfrey, N. A. 1986. Improved diagnosis and prognosis of mucormycosis. A
clinicopathologic study of 33 cases. Medicine 65:113123.
115. Patino, J. F., and D. Castro. 1991. Necrotizing lesions of soft tissues: a
review. World J. Surg. 15:235239.
116. Pavie, J., M. Lafaurie, C. Lacroix, A. Marie Zagdanski, D. Debrosse, G.
Socie, F. Derouin, E. Gluckman, and J. Michel Molina. 2004. Successful
treatment of pulmonary mucormycosis in an allogenic bone-marrow trans-
plant recipient with combined medical and surgical therapy. Scand. J. In-
fect. Dis. 36:767769.
117. Perfect, J. R., K. A. Marr, T. J. Walsh, R. N. Greenberg, B. DuPont, J. de
la Torre-Cisneros, G. Just-Nubling, H. T. Schlamm, I. Lutsar, A. Espinel-
Ingroff, and E. Johnson. 2003. Voriconazole treatment for less-common,
emerging, or refractory fungal infections. Clin. Infect. Dis. 36:11221131.
118. Peterson, K. L., M. Wang, R. F. Canalis, and E. Abemayor. 1997. Rhino-
cerebral mucormycosis: evolution of the disease and treatment options.
Laryngoscope 107:855862.
119. Petrikkos, G., A. Skiada, H. Sambatakou, A. Toskas, G. Vaiopoulos, M.
Giannopoulou, and N. Katsilambros. 2003. Mucormycosis: ten-year expe-
rience at a tertiary-care center in Greece. Eur. J. Clin. Microbiol. Infect.
Dis. 22:753756.
120. Pfaller, M. A., S. A. Messer, R. J. Hollis, and R. N. Jones. 2002. Antifungal
activities of posaconazole, ravuconazole, and voriconazole compared to
those of itraconazole and amphotericin B against 239 clinical isolates of
Aspergillus spp. and other lamentous fungi: report from SENTRY Anti-
microbial Surveillance Program, 2000. Antimicrob. Agents Chemother. 46:
10321037.
121. Pierce, P. F., M. B. Wood, G. D. Roberts, R. H. Fitzgerald, Jr., C. Robert-
son, and R. S. Edson. 1987. Saksenaea vasiformis osteomyelitis. J. Clin.
Microbiol. 25:933935.
122. Pillsbury, H. C., and N. D. Fischer. 1977. Rhinocerebral mucormycosis.
Arch. Otolaryngol. 103:600604.
123. Ponz, E., J. M. Campistol, T. Ribalta, J. Montoliu, J. Ram rez, J. Almirall,
and L. Revert. 1991. [Disseminated mucormycosis in a hemodialyzed fe-
male patient treated with deferoxamine]. Rev. Clin. Espanol. 188:8587.
124. Prasad, R. M., S. M. Bose, K. Vaiphei, and G. R. Verma. 2003. Post
operative abdominal wall mucormycosis mimicking as bacterial necrotising
fasciitis. J. Postgrad. Med. 49:187188.
125. Quinio, D., A. Karam, J. P. Leroy, M. C. Moal, B. Bourbigot, O. Masure, B.
Sassolas, and A. M. Le Flohic. 2004. Zygomycosis caused by Cunningha-
mella bertholletiae in a kidney transplant recipient. Med. Mycol. 42:177
180.
126. Rees, J. R., R. W. Pinner, R. A. Hajjeh, M. E. Brandt, and A. L. Reingold.
1998. The epidemiological features of invasive mycotic infections in the San
Francisco Bay area, 19921993: results of population-based laboratory ac-
tive surveillance. Clin. Infect. Dis. 27:11381147.
127. Reid, V. J., D. L. Solnik, T. Daskalakis, and K. P. Sheka. 2004. Manage-
ment of bronchovascular mucormycosis in a diabetic: a surgical success.
Ann. Thorac. Surg. 78:14491451.
128. Reimund, E., and A. Ramos. 1994. Disseminated neonatal gastrointestinal
mucormycosis: a case report and review of the literature. Pediatr. Pathol.
14:385389.
129. Ribes, J. A., C. L. Vanover-Sams, and D. J. Baker. 2000. Zygomycetes in
human disease. Clin. Microbiol. Rev. 13:236301.
130. Rickerts, V., A. Bohme, and G. Just-Nubling. 2002. Risk factor for invasive
zygomycosis in patients with hematologic malignancies. Mycoses 45(Suppl.
1):2730.
131. Robb, S. M. 1966. Reactions of fungi to exposure to 10 atmospheres pres-
sure of oxygen. J. Gen. Microbiol. 45:1729.
132. Rothstein, R. D., and G. L. Simon. 1986. Subacute pulmonary mucormy-
cosis. J. Med. Vet. Mycol. 24:391394.
133. Safdar, A., S. OBrien, and I. F. Kouri. 2004. Efcacy and feasibility of
aerosolized amphotericin B lipid complex therapy in caspofungin break-
through pulmonary zygomycosis. Bone Marrow Transplant. 34:467468.
134. Santos, J., P. Espigado, C. Romero, J. Andreu, A. Rivero, and J. A. Pineda.
1994. Isolated renal mucormycosis in two AIDS patients. Eur. J. Clin.
Microbiol. Infect. Dis. 13:430432.
135. Sehgal, A., M. Raghavendran, D. Kumar, A. Srivastava, D. Dubey, and A.
Kumar. 2004. Rhinocerebral mucormycosis causing basilar artery aneurysm
with concomitant fungal colonic perforation in renal allograft recipient: a
case report. Transplantation 78:949950.
136. Serna, J. H., A. Wanger, and A. K. Dosekun. 2003. Successful treatment of
mucormycosis peritonitis with liposomal amphotericin B in a patient on
long-term peritoneal dialysis. Am. J. Kidney Dis. 42:E1417.
137. Sharma, M. C., S. S. Gill, S. Kashyap, R. Kataria, D. K. Gupta, P. Sahni,
and S. K. Acharya. 1998. Gastrointestinal mucormycosisan uncommon
isolated mucormycosis. Indian J. Gastroenterol. 17:131133.
138. Singh, N., T. Gayowski, J. Singh, and V. L. Yu. 1995. Invasive gastrointes-
tinal zygomycosis in a liver transplant recipient: case report and review of
zygomycosis in solid-organ transplant recipients. Clin. Infect. Dis. 20:617
620.
139. Siu, K. L., and W. H. Lee. 2004. A rare cause of intestinal perforation in an
extreme low birth weight infantgastrointestinal mucormycosis: a case re-
port. J. Perinatol. 24:319321.
140. Siwek, G. T., K. J. Dodgson, M. de Magalhaes-Silverman, L. A. Bartelt,
S. B. Kilborn, P. L. Hoth, D. J. Diekema, and M. A. Pfaller. 2004. Invasive
zygomycosis in hematopoietic stem cell transplant recipients receiving vori-
conazole prophylaxis. Clin. Infect. Dis. 39:584587.
141. Spellberg, B., Y. Fu, J. Edwards Jr., and A. S. Ibrahim. 2005. Combination
therapy with amphotericin B lipid complex and caspofungin acetate of
disseminated zygomycosis in diabetic ketoacidotic mice. Antimicrob.
Agents Chemother. 49:830832.
142. Spellberg, B., M. D. Witt, and C. K. Beck. 2004. Amphotericin B: is a
lipid-formulation gold standard feasible? Clin. Infect. Dis. 38:304307.
143. Sponsler, T. A., J. W. Sassani, L. N. Johnson, and J. Towghi. 1992. Ocular
invasion in mucormycosis. Survey Ophthalmol. 36:345350.
144. Straatsma, B. R., L. E. Zimmerman, and J. D. M. Gass. 1962. Phycomy-
cosis: a clinicopathologic study of fty-one cases. Lab. Investig. 11:963985.
145. Sugar, A. M. 2005. Agents of mucormycosis and related species, p. 2979. In
G. L. Mandell, J. E. Bennett, and R. Dolin (ed.), Principles and practice of
infectious disease, 6th ed. Elsevier, Philadelphia, Pa.
146. Suh, I. W., C. S. Park, M. S. Lee, J. H. Lee, M. S. Chang, J. H. Woo, I. C.
Lee, and J. S. Ryu. 2000. Hepatic and small bowel mucormycosis after
chemotherapy in a patient with acute lymphocytic leukemia. J. Korean
Med. Sci. 15:351354.
147. Sun, Q. N., A. W. Fothergill, D. I. McCarthy, M. G. Rinaldi, and J. R.
Graybill. 2002. In vitro activities of posaconazole, itraconazole, voricon-
azole, amphotericin B, and uconazole against 37 clinical isolates of zygo-
mycetes. Antimicrob. Agents Chemother. 46:15811582.
148. Sun, Q. N., L. K. Najvar, R. Bocanegra, D. Loebenberg, and J. R. Graybill.
2002. In vivo activity of posaconazole against Mucor spp. in an immuno-
suppressed-mouse model. Antimicrob. Agents Chemother. 46:23102312.
149. Talmi, Y. P., A. Goldschmied-Reouven, M. Bakon, I. Barshack, M. Wolf, Z.
Horowitz, M. Berkowicz, N. Keller, and J. Kronenberg. 2002. Rhino-orbital
and rhino-orbito-cerebral mucormycosis. Otolaryngol. Head Neck Surg.
127:2231.
150. Tedder, M., J. A. Spratt, M. P. Anstadt, S. S. Hegde, S. D. Tedder, and J. E.
Lowe. 1994. Pulmonary mucormycosis: results of medical and surgical ther-
apy. Ann. Thorac. Surg. 57:10441050.
151. Teggi, A., A. Fedele, R. Bagnato, F. Traditi, C. M. Lanzalone, and F. De
Rosa. 1989. [A case of disseminated mucormycosis]. Recenti Prog. Med.
80:308313.
152. ter Borg, F., E. J. Kuijper, and H. van der Lelie. 1990. Fatal mucormycosis
presenting as an appendiceal mass with metastatic spread to the liver during
chemotherapy-induced granulocytopenia. Scand. J. Infect. Dis. 22:499501.
153. Thajeb, P., T. Thajeb, and D. Dai. 2004. Fatal strokes in patients with
rhino-orbito-cerebral mucormycosis and associated vasculopathy. Scand.
J. Infect. Dis. 36:643648.
154. Tietz, H. J., D. Brehmer, W. Janisch, and H. Martin. 1998. Incidence of
endomycoses in the autopsy material of the Berlin Charite Hospital. My-
coses 41(Suppl. 2):8185.
155. Tobon, A. M., M. Arango, D. Fernandez, and A. Restrepo. 2003. Mucor-
mycosis (zygomycosis) in a heart-kidney transplant recipient: recovery after
posaconazole therapy. Clin. Infect. Dis. 36:14881491.
156. Tuder, R. M. 1985. Myocardial infarct in disseminated mucormycosis: case
568 SPELLBERG ET AL. CLIN. MICROBIOL. REV.
report with special emphasis on the pathogenic mechanisms. Mycopatho-
logia 89:8188.
157. Vadeboncoeur, C., J. M. Walton, J. Raisen, P. Soucy, H. Lau, and S. Rubin.
1994. Gastrointestinal mucormycosis causing an acute abdomen in the
immunocompromised pediatric patientthree cases. J. Pediatr. Surg. 29:
12481249.
158. Van Cutsem, J., and J. R. Boelaert. 1989. Effects of deferoxamine, ferox-
amine and iron on experimental mucormycosis (zygomycosis). Kidney Int.
36:10611068.
159. Van Cutsem, J., F. Van Gerven, J. Fransen, and P. A. Janssen. 1989.
Treatment of experimental zygomycosis in guinea pigs with azoles and with
amphotericin B. Chemotherapy 35:267272.
160. Veis, J. H., R. Contiguglia, M. Klein, J. Mishell, A. C. Alfrey, and J. I.
Shapiro. 1987. Mucormycosis in deferoxamine-treated patients on dialysis
[letter]. Ann. Intern. Med. 107:258.
161. Ventura, G. J., H. M. Kantarjian, E. Anaissie, R. L. Hopfer, and V.
Fainstein. 1986. Pneumonia with Cunninghamella species in patients with
hematologic malignancies. A case report and review of the literature. Can-
cer 58:15341536.
162. Vesa, J., O. Bielsa, O. Arango, C. Llado, and A. Gelabert. 1992. Massive
renal infarction due to mucormycosis in an AIDS patient. Infection 20:234
236.
163. Vigouroux, S., O. Morin, P. Moreau, F. Mechinaud, N. Morineau, B. Mahe,
P. Chevallier, T. Guillaume, V. Dubruille, J. L. Harousseau, and N.
Milpied. 2005. Zygomycosis after prolonged use of voriconazole in immu-
nocompromised patients with hematologic disease: attention required.
Clin. Infect. Dis. 40:e3537.
164. Virmani, R., D. H. Connor, and H. A. McAllister. 1982. Cardiac mucormy-
cosis. A report of ve patients and review of 14 previously reported cases.
Am. J. Clin. Pathol. 78:4247.
165. Voitl, P., C. Scheibenpug, T. Weber, O. Janata, and A. M. Rokitansky.
2002. Combined antifungal treatment of visceral mucormycosis with caspo-
fungin and liposomal amphotericin B. Eur. J. Clin. Microbiol. Infect. Dis.
21:632634.
166. Waldorf, A. R. 1989. Pulmonary defense mechanisms against opportunistic
fungal pathogens. Immunol. Ser. 47:243271.
167. Waldorf, A. R., and R. D. Diamond. 1984. Cerebral mucormycosis in dia-
betic mice after intrasinus challenge. Infect. Immun. 44:194195.
168. Waldorf, A. R., C. Halde, and N. A. Vedros. 1982. Murine model of pul-
monary mucormycosis in cortisone-treated mice. Sabouraudia 20:217224.
169. Waldorf, A. R., N. Ruderman, and R. D. Diamond. 1984. Specic suscep-
tibility to mucormycosis in murine diabetes and bronchoalveolar macro-
phage defense against Rhizopus. J. Clin. Investig. 74:150160.
170. Walsh, T. J., J. W. Hiemenz, N. L. Seibel, J. R. Perfect, G. Horwith, L. Lee,
J. L. Silber, M. J. DiNubile, A. Reboli, E. Bow, J. Lister, and E. J. Anaissie.
1998. Amphotericin B lipid complex for invasive fungal infections: analysis
of safety and efcacy in 556 cases. Clin. Infect. Dis. 26:13831396.
171. Watts, W. J. 1983. Bronchopleural stula followed by massive fatal hemop-
tysis in a patient with pulmonary mucormycosis. A case report. Arch.
Intern. Med. 143:10291030.
172. Welk, B., A. A. House, E. Ralph, E. Tweedy, and P. P. Luke. 2004. Successful
treatment of primary bilateral renal mucormycosis with bilateral nephrec-
tomy. Urology 64:590.
173. Weng, D. E., W. H. Wilson, R. Little, and T. J. Walsh. 1998. Successful
medical management of isolated renal zygomycosis: case report and review.
Clin. Infect. Dis. 26:601605.
174. White, C. B., P. J. Barcia, and J. W. Bass. 1986. Neonatal zygomycotic
necrotizing cellulitis. Pediatrics 78:100102.
175. Wolf, O., Z. Gil, L. Leider-Trejo, A. Khaf, P. Biderman, and D. M. Fliss.
2004. Tracheal mucormycosis presented as an intraluminal soft tissue mass.
Head Neck 26:541543.
176. Woods, K. F., and B. J. Hanna. 1986. Brain stem mucormycosis in a narcotic
addict with eventual recovery. Am. J. Med. 80:126128.
177. Woodward, A., C. McTigue, G. Hogg, A. Watkins, and H. Tan. 1992. Mu-
cormycosis of the neonatal gut: a new disease or a variant of necrotizing
enterocolitis? J. Pediatr. Surg. 27:737740.
178. Yamazaki, T., H. Kume, S. Murase, E. Yamashita, and M. Arisawa. 1999.
Epidemiology of visceral mycoses: analysis of data in annual of the patho-
logical autopsy cases in Japan. J. Clin. Microbiol. 37:17321738.
179. Yanagisawa, E., S. Friedman, R. S. Kundargi, and H. W. Smith. 1977.
Rhinocerebral phycomycosis. Laryngoscope 87:13191335.
VOL. 18, 2005 NOVEL PERSPECTIVES ON MUCORMYCOSIS 569
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Difficult Airway AlgorithmDocument48 pagesDifficult Airway AlgorithmshikhaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- One Answer To Cancer by William Donald Kelley, D.D.S., M.S.Document53 pagesOne Answer To Cancer by William Donald Kelley, D.D.S., M.S.Teti Haxhidauti94% (16)
- Assessing The Ear and HearingDocument32 pagesAssessing The Ear and HearingArlyn Mendenilla0% (1)
- Respiratory PhysiologyDocument16 pagesRespiratory PhysiologyYsabel Salvador DychincoNo ratings yet
- IELTS WordsDocument97 pagesIELTS WordsLeeNo ratings yet
- Etica Semipresencial IztaDocument1 pageEtica Semipresencial IztaabogadomedicoNo ratings yet
- Certificado de Control Interno DRJGMTDocument1 pageCertificado de Control Interno DRJGMTabogadomedicoNo ratings yet
- Fundamentos Grupo PresencialDocument11 pagesFundamentos Grupo PresencialabogadomedicoNo ratings yet
- Unidad 2 ExentosDocument1 pageUnidad 2 ExentosabogadomedicoNo ratings yet
- Est Inf II 44DDocument22 pagesEst Inf II 44DabogadomedicoNo ratings yet
- Etica Semipresencial IztaDocument1 pageEtica Semipresencial IztaabogadomedicoNo ratings yet
- Est Inf II 43DDocument29 pagesEst Inf II 43DabogadomedicoNo ratings yet
- Calificacion Unidad 5 Est Inf 2 4.3Document1 pageCalificacion Unidad 5 Est Inf 2 4.3abogadomedicoNo ratings yet
- Lista Enero Junio 2016 Estadistica InferencialDocument14 pagesLista Enero Junio 2016 Estadistica InferencialabogadomedicoNo ratings yet
- Est Inf II 43DDocument29 pagesEst Inf II 43DabogadomedicoNo ratings yet
- Calificacion Unidad 5 Est Inf 2 4.3Document1 pageCalificacion Unidad 5 Est Inf 2 4.3abogadomedicoNo ratings yet
- Pathogenesis of MucormycosisDocument7 pagesPathogenesis of MucormycosisabogadomedicoNo ratings yet
- Lista Fundamentos D5Document4 pagesLista Fundamentos D5abogadomedicoNo ratings yet
- Lista Ing de Sis D3Document3 pagesLista Ing de Sis D3abogadomedicoNo ratings yet
- Development of Chagas Cardiac Manifestations Among Texas Blood DonorsDocument5 pagesDevelopment of Chagas Cardiac Manifestations Among Texas Blood DonorsabogadomedicoNo ratings yet
- Lista Fundamentos D5Document4 pagesLista Fundamentos D5abogadomedicoNo ratings yet
- Lista Fundamentos D5Document4 pagesLista Fundamentos D5abogadomedicoNo ratings yet
- Examen Semana 4Document2 pagesExamen Semana 4abogadomedicoNo ratings yet
- Fundamentos D6Document2 pagesFundamentos D6abogadomedicoNo ratings yet
- Lista Fundamentos D5Document4 pagesLista Fundamentos D5abogadomedicoNo ratings yet
- Texas and Mexico Sharing A Legacy of PovertyDocument6 pagesTexas and Mexico Sharing A Legacy of PovertyabogadomedicoNo ratings yet
- Author Guide LinesDocument24 pagesAuthor Guide LinesMohamed TahaNo ratings yet
- Efficacy of Doctorvox On Mutational FalsettoDocument8 pagesEfficacy of Doctorvox On Mutational FalsettoANA CRISTINA MENDEZ DIAZNo ratings yet
- Perioperative Fasting and Feeding in Adults, Obstetric, Paediatric and Bariatric Population-Practice Guidelines From The Indian Society of AnaesthesiologistsDocument29 pagesPerioperative Fasting and Feeding in Adults, Obstetric, Paediatric and Bariatric Population-Practice Guidelines From The Indian Society of Anaesthesiologistsambitiousamit1No ratings yet
- Chapter - 2 Microorganisms (Continuation)Document2 pagesChapter - 2 Microorganisms (Continuation)ARSHAD JAMILNo ratings yet
- Gingival Inflammation in Mouth Breathing PatientsDocument5 pagesGingival Inflammation in Mouth Breathing PatientsCamiLunaNo ratings yet
- Fidelis Drug List 2018Document80 pagesFidelis Drug List 2018Annie AnnaNo ratings yet
- Myths PDFDocument8 pagesMyths PDFLuisa Elena HernandezNo ratings yet
- Level of Knowledge, Attitudes and Preventive Strategies Against Airborne Transmitted Diseases: Basis For A Management ModelDocument20 pagesLevel of Knowledge, Attitudes and Preventive Strategies Against Airborne Transmitted Diseases: Basis For A Management ModelBhell MendiolaNo ratings yet
- Proceedings GRANADA 1Document70 pagesProceedings GRANADA 1wingsskyNo ratings yet
- Fisiologi StarvasiDocument47 pagesFisiologi Starvasicynthia maharaniNo ratings yet
- Detect Pharmaceutical Health Hazards and ActDocument81 pagesDetect Pharmaceutical Health Hazards and Acttemesgen dinsaNo ratings yet
- Sitogenetika Dan Peranannya Dalam Keganasan Hematologi: ResearchDocument23 pagesSitogenetika Dan Peranannya Dalam Keganasan Hematologi: ResearchFebryanti Priskila SilaenNo ratings yet
- Factory Farming in The Developing WorldDocument10 pagesFactory Farming in The Developing WorldDaisyNo ratings yet
- Abreviaciones ChatDocument4 pagesAbreviaciones ChatrojarodNo ratings yet
- Science: Quarter 1 - Module 1: Week 1-2Document31 pagesScience: Quarter 1 - Module 1: Week 1-2Kirt Dimamay HilarioNo ratings yet
- Syphilis: Jessica Lyons Period D STD Project 4/22/13Document3 pagesSyphilis: Jessica Lyons Period D STD Project 4/22/13jesssielynnn33No ratings yet
- Practice Test 05 - Hints & Solutions - Lakshya NEET 2024Document15 pagesPractice Test 05 - Hints & Solutions - Lakshya NEET 2024Pandey 14No ratings yet
- Grade 8-Q1-TG PDFDocument34 pagesGrade 8-Q1-TG PDFMerlinda LibaoNo ratings yet
- Keep Fit For Life: Meeting The Nutritional Needs of Older PersonsDocument83 pagesKeep Fit For Life: Meeting The Nutritional Needs of Older Personsapi-342482642No ratings yet
- Alcohol Research Paper OutlineDocument6 pagesAlcohol Research Paper Outlineafmctmvem100% (1)
- Atrial Fibrillation PathophysiologyDocument2 pagesAtrial Fibrillation PathophysiologyanabbabarNo ratings yet
- A Proposed Pediatric Medical Center Research ThesisDocument3 pagesA Proposed Pediatric Medical Center Research ThesisMarielle AbanteNo ratings yet
- Bird Nets PDFDocument4 pagesBird Nets PDFPaul LawlessNo ratings yet
- Foot and Ankle Injuries Kylee Phillips - 0Document74 pagesFoot and Ankle Injuries Kylee Phillips - 0rizwan.mughal1997No ratings yet
- Ent AssessmentDocument23 pagesEnt AssessmentPdianghunNo ratings yet
- Adams4e Tif Ch47Document19 pagesAdams4e Tif Ch47fbernis1480_11022046100% (1)