Professional Documents
Culture Documents
Cardiomyopathy Nursing Concept Map
Uploaded by
friendofnurseOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiomyopathy Nursing Concept Map
Uploaded by
friendofnurseCopyright:
Available Formats
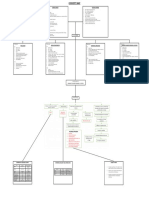
NURSING CONCEPT
MAP
Ashley Deyerle
2/9/2013
B.G.
51 y.o. male w/
Cardiomyopat
hy ejection
fraction of
Excess fluid volume related to increased venous pressure and
decreased renal perfusion secondary to cardiac failure as
evidenced by rapid weight gain, edema, adventitious breath
sounds, oliguria, and patients statement, My ankles are so
swollen.
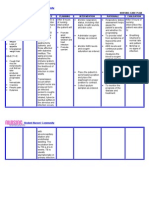
Implementations
Administer prescribed diuretics
Monitor for therapeutic effect of diuretic (e.g., increased urine output
and decreased adventitious breath sounds
Monitor potassium levels after diuresis to detect excessive electrolyte
loss.
Monitor intake and output to assess fluid status.
Monitor respiratory pattern for symptoms of respiratory difficulty to
detect pulmonary edema.
!"IE#" G$!%! "#periences reduction or absence of edema and stable
!ctivity intolerance related to fatigue secondary to cardiac insufficiency and
pulmonary congestion as evidenced by dyspnea, shortness of breath, weakness,
increase in heart rate on e#ertion, and patients statement, $ feel too weak to do
anything
Implementations
!"IE#" G$!% %ill achieve a realistic program of activity that balances physical
activity with energy&conserving activities
Impaired
&as exchan&e related to increased preload and
alveolar&capillary membrane changes as
evidenced by abnormal arterial blood gases,
hypo#emia, dyspnea, tachypnea, tachycardia,
restlessness, and patients statement, $ am so
short of breath
Implementations
!"IE#" G$!% Maintains ade'uate
o#ygen(carbon dio#ide e#change at the alveolar&
capillary membrane to meet o#ygen needs of the
body
'ecreased cardiac output related to altered
contractility, altered preload, and(or altered stroke
volume as evidenced by decreased e)ection fraction,
increased *+,, decreased peripheral pulses, )ugular
vein distention, orthopnea, -. and -/ sounds, and
oliguria
Implementations
'eficient (nowled&e related to lack of
information about disease process as
evidenced by 'uestions about the disease and
patients statement, $ dont know why $ keep
getting sick
Implementation
!"IE#" G$!% 0escribes disease
process and rationales for dietary, medication,
and e#ercise regimen
1. ,erform a comprehensive appraisal of peripheral circulation (e.g., check peripheral pulses, edema, capillary
refill, color, and temperature of e#tremity to determine circulatory status.
2. 1ote signs and symptoms of decreased cardiac output to detect changes in status.
3. Monitor fluid balance (e.g., $(2 and daily weight to evaluate renal perfusion.
4. Monitor for cardiac dysrhythmias to detect cardiac decomposition.
5. Monitor for dyspnea, fatigue, tachypnea, and orthopnea to identify involvement of respiratory system.
!"IE#" G$!% Maintains ade'uate blood pumped by the heart to meet metabolic demands of the body
Monitor rate, rhythm, depth, and effort of respirations.
Auscultate breath sounds, noting areas of decreased(absent ventilation and presence of adventitious sounds
Monitor for increased restlessness, an#iety, and air hunger
Administer supplemental 23 as ordered to maintain O2 levels.
,osition to alleviate dyspnea (e.g., semi&4owlers position)
1. Appraise the patients current level of knowledge related to specific disease process to identify needed areas of
teaching.
2. 0escribe common signs and symptoms of the disease so patient will know signs and symptoms to report to
health care provider.
3. $nstruct the patient and caregiver on measures to prevent(minimi5e side effects of treatment for the disease so
patient may be able to decrease number of acute episodes of 64.
4. Appraise the patients and caregivers current level of knowledge about prescribed diet to assess areas needing
additional instruction.
5. 7eview patients knowledge of medications to determine where further teaching is needed.
1. "ncourage alternate rest and activity periods to reduce cardiac workload and conserve energy.
2. ,rovide calming diversionary activities to promote rela#ation to reduce 23 consumption and to relieve dyspnea
and fatigue.
3. Monitor patients 23 response (e.g., pulse rate, cardiac rhythm, and respiratory rate to self&care or nursing
activities to determine level of activity that can be performed.
4. 8each patient and caregiver techni'ues of self&care that will minimi5e 23 consumption
5. *ollaborate with occupational, physical, and(or recreational therapists to plan and monitor activity(e#ercise
program.
.9&3
You might also like
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Basic Concept - ATI Template Childhood InjuriesDocument1 pageBasic Concept - ATI Template Childhood InjuriesRafia HassanNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- Completed Concept MapDocument4 pagesCompleted Concept Mapapi-607361848No ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Care PlanDocument11 pagesCare PlanAlyssa CardinalNo ratings yet
- Nursing AssessmentDocument16 pagesNursing AssessmentJihan Novita100% (1)
- Case Study 101: Abdominal Aortic Aneurysm With Acute Kidney InjuryDocument8 pagesCase Study 101: Abdominal Aortic Aneurysm With Acute Kidney InjuryPatricia Ann Nicole ReyesNo ratings yet
- 2017 Fluid and Electrolytes LECTURE NOTESDocument34 pages2017 Fluid and Electrolytes LECTURE NOTESHarley Justiniani Dela CruzNo ratings yet
- n360 Concept Map Care Plan Week 3 Sheryl SatoDocument15 pagesn360 Concept Map Care Plan Week 3 Sheryl Satoapi-283363983No ratings yet
- Focused ReviewDocument6 pagesFocused ReviewGina GiammalvoNo ratings yet
- Medsurg 2007Document15 pagesMedsurg 2007WisdomIsMisery100% (1)
- Oxytocin (Pitocin) : Slide 1Document16 pagesOxytocin (Pitocin) : Slide 1Kalesha JonesNo ratings yet
- Lewis COPD Case StudyDocument2 pagesLewis COPD Case Studyatarisgurl08No ratings yet
- Pediatric Concept MapDocument12 pagesPediatric Concept Mapapi-352157080No ratings yet
- ATI Prototype DrugsDocument11 pagesATI Prototype Drugsjinnyduong100% (1)
- Study Guide Med Surg #1Document22 pagesStudy Guide Med Surg #1cfunk929No ratings yet
- Ati Medication Template VasopressinDocument1 pageAti Medication Template VasopressinSharee HaywoodNo ratings yet
- Understanding CHF and Monitoring Fluid StatusDocument4 pagesUnderstanding CHF and Monitoring Fluid StatusWeng RamojalNo ratings yet
- Copd Case StudyDocument6 pagesCopd Case StudyDivine ParagasNo ratings yet
- Discussion QuestionsDocument2 pagesDiscussion QuestionsMary RiasNo ratings yet
- Concept MapDocument1 pageConcept Mapapi-246466200No ratings yet
- Ati Medication Template KetorolacDocument1 pageAti Medication Template KetorolacSharee HaywoodNo ratings yet
- Major Hormone Glands and Their FunctionsDocument5 pagesMajor Hormone Glands and Their FunctionsSTEFFI GABRIELLE GOLEZNo ratings yet
- Pharm Exam ReviewDocument13 pagesPharm Exam ReviewAshleyNo ratings yet
- Assessment and Concept Map Care Plan: Joseph GorospeDocument5 pagesAssessment and Concept Map Care Plan: Joseph Gorospeapi-497389977No ratings yet
- System Disorder GHDDocument1 pageSystem Disorder GHDSariahNo ratings yet
- Influenza VirusDocument17 pagesInfluenza Virusapi-458845511No ratings yet
- Stroke Signs, Risks, and Nursing CareDocument1 pageStroke Signs, Risks, and Nursing CareMariel Febreo MerlanNo ratings yet
- CH 29 - Management of Patients With Structural, Infectious, and Inflmmatory Cardiac DisordersDocument15 pagesCH 29 - Management of Patients With Structural, Infectious, and Inflmmatory Cardiac DisordersPye Antwan Delva100% (1)
- Nursing Interventions Concept MapDocument3 pagesNursing Interventions Concept Mapphelenaphie menodiado panlilioNo ratings yet
- AlbuterolDocument1 pageAlbuterolCassieNo ratings yet
- FundaDocument101 pagesFundaMelanieTriezlVillaseñorJosonNo ratings yet
- Case Simu 101Document5 pagesCase Simu 101Princess Levie CenizaNo ratings yet
- Managing Diabetes Sick DaysDocument14 pagesManaging Diabetes Sick DaysJake Yvan DizonNo ratings yet
- Acute Renal Failure-Student-Rapid ReasoningDocument4 pagesAcute Renal Failure-Student-Rapid Reasoningapi-268403950No ratings yet
- A. Cardiac Failure: Biologic CrisisDocument11 pagesA. Cardiac Failure: Biologic CrisisJillian CaumbanNo ratings yet
- Sena, Zyrus Reoder ADocument4 pagesSena, Zyrus Reoder AAkoSiIngridNo ratings yet
- HESI Women's Health:Newborn DrugsDocument8 pagesHESI Women's Health:Newborn Drugsisapatrick8126No ratings yet
- Teamworks! Game: Summary ReportDocument2 pagesTeamworks! Game: Summary ReportAngela May Pustasa AllamNo ratings yet
- Clinical Case Study - Online Discussion Form Fall 2020-1Document14 pagesClinical Case Study - Online Discussion Form Fall 2020-1Sabrina Odies100% (1)
- GYNECOLOGICALNURSINGDocument4 pagesGYNECOLOGICALNURSINGSheana TmplNo ratings yet
- Renal Concept MapDocument1 pageRenal Concept MapShaira Ann CalambaNo ratings yet
- Generic and Trade Names, Mechanisms, InterventionsDocument4 pagesGeneric and Trade Names, Mechanisms, InterventionsSonia FernandesNo ratings yet
- Ba GastrectomyDocument10 pagesBa GastrectomyHope3750% (2)
- Congestive Heart Failure OutlineDocument4 pagesCongestive Heart Failure OutlineDominique PorterNo ratings yet
- Chapter 30Document26 pagesChapter 30Nurse UtopiaNo ratings yet
- Medical Surgical: SNS (Anti-Cholinergic/adrenergic)Document12 pagesMedical Surgical: SNS (Anti-Cholinergic/adrenergic)Pedro SorianoNo ratings yet
- Waiters Osteoarthritis PDFDocument1 pageWaiters Osteoarthritis PDFmp1757No ratings yet
- Concept Map Due 04Document9 pagesConcept Map Due 04api-545711468No ratings yet
- COPD Concept MapDocument1 pageCOPD Concept MapSherree HayesNo ratings yet
- Care PlanDocument2 pagesCare PlanLorina Lynne ApelacioNo ratings yet
- Main drug therapy for ulcerative colitis is sulfa for one yearDocument4 pagesMain drug therapy for ulcerative colitis is sulfa for one yearcathyNo ratings yet
- Health Assessment 51-100 QuestionnaireDocument27 pagesHealth Assessment 51-100 QuestionnairetflorenzNo ratings yet
- Heart Failure AssignmentDocument6 pagesHeart Failure AssignmentclarheenaNo ratings yet
- Nursing Concept Map 1Document3 pagesNursing Concept Map 1Norah Okafor Ezike67% (3)
- ENDOCRINE NURSING-FINAL HDDocument15 pagesENDOCRINE NURSING-FINAL HDJayvee Novenario Casaljay100% (1)
- VSim Pharm (Mary Richards)Document3 pagesVSim Pharm (Mary Richards)Jay Blastic's arts and FunNo ratings yet
- Waiters Rhabdomyolysis PDFDocument1 pageWaiters Rhabdomyolysis PDFmp1757No ratings yet
- Lewis: Medical-Surgical Nursing, 7th Edition: Comprehensive GlossaryDocument49 pagesLewis: Medical-Surgical Nursing, 7th Edition: Comprehensive Glossarylani50% (2)
- Maternity Evolve ExamDocument36 pagesMaternity Evolve Examfriendofnurse100% (26)
- Lecture Outline - Fluids and ElectrolytesDocument19 pagesLecture Outline - Fluids and Electrolytesfriendofnurse100% (1)
- Child Evolve ExamDocument37 pagesChild Evolve Examfriendofnurse100% (14)
- Acid Base Self Study With Practice QuestionsDocument13 pagesAcid Base Self Study With Practice QuestionsfriendofnurseNo ratings yet
- Nursing Management of CAD and ACSDocument9 pagesNursing Management of CAD and ACSfriendofnurse100% (4)
- Renal Medications WorksheetDocument11 pagesRenal Medications Worksheetfriendofnurse100% (1)
- CD4 count determines AIDS diagnosis and disease progressionDocument2 pagesCD4 count determines AIDS diagnosis and disease progressionfriendofnurseNo ratings yet
- Ball & Bindler Pediatric Nursing - Caring For ChildrenDocument105 pagesBall & Bindler Pediatric Nursing - Caring For Childrenfriendofnurse50% (4)
- Fundamentals of Nursing Chapter 12Document7 pagesFundamentals of Nursing Chapter 12friendofnurseNo ratings yet
- Idc NCPDocument14 pagesIdc NCPEnrique BabierraNo ratings yet
- Faraz Pearls For MRCPDocument223 pagesFaraz Pearls For MRCPSyed Ali Akbar86% (14)
- 10 1056@NEJMcpc1913468 PDFDocument10 pages10 1056@NEJMcpc1913468 PDFAbdelkader HociniNo ratings yet
- 10.blood Vessels & HeartDocument4 pages10.blood Vessels & Heartharips motupalliNo ratings yet
- Latest Fcps McqsDocument205 pagesLatest Fcps McqsMuntaha JavedNo ratings yet
- IM-CAP Concept MapDocument1 pageIM-CAP Concept MapTrisNo ratings yet
- NCP SDocument8 pagesNCP SMarvie CadenaNo ratings yet
- Nursing Care Plan (Pedia)Document5 pagesNursing Care Plan (Pedia)JA BerzabalNo ratings yet
- Test - Mark Klimek Blue Book - QuizletDocument139 pagesTest - Mark Klimek Blue Book - QuizletCora Acucena96% (25)
- Chronic Obstructive Pulmonary DiseaseDocument8 pagesChronic Obstructive Pulmonary DiseaseGeozel VivienneNo ratings yet
- Powerful Natural Remedies for COVID-19 and Variant StrainsDocument24 pagesPowerful Natural Remedies for COVID-19 and Variant StrainsTracyNo ratings yet
- ATS Categories and DescriptorsDocument5 pagesATS Categories and DescriptorsdewiNo ratings yet
- Amniotic Fluid EmbolismDocument8 pagesAmniotic Fluid EmbolismArri KurniawanNo ratings yet
- Mnemonics for Medical ConditionsDocument4 pagesMnemonics for Medical ConditionsLheidaniel MMM.100% (1)
- Lecture Notes On The Basic Principles of SurgeryDocument33 pagesLecture Notes On The Basic Principles of SurgerynabazNo ratings yet
- Nursing Care Plan For Myocardial Infarction NCPDocument8 pagesNursing Care Plan For Myocardial Infarction NCPRhomyrose CampanaNo ratings yet
- Respiratory Quiz QuestionsDocument5 pagesRespiratory Quiz Questionssv12b100% (2)
- ABC Lecture NotesDocument7 pagesABC Lecture NotesLady Shayne YapNo ratings yet
- 3rd Lesson Assessing Child Bearing WomenDocument6 pages3rd Lesson Assessing Child Bearing WomendaningdubouzetNo ratings yet
- LSMU 6th Year Therapy1stDocument35 pagesLSMU 6th Year Therapy1stSuruchi Jagdish SharmaNo ratings yet
- Nursing Care Plan for a Patient with Tuberculosis (TBDocument2 pagesNursing Care Plan for a Patient with Tuberculosis (TBVen Belista86% (14)
- History Taking in SurgeryDocument25 pagesHistory Taking in SurgeryAsem Al-domainiNo ratings yet
- PAROS (Case 3)Document2 pagesPAROS (Case 3)Carl Michael RazoNo ratings yet
- General Surgery Topic ListDocument2 pagesGeneral Surgery Topic Listalijax522No ratings yet
- Nursing Management For Acute Respiratory FailureDocument7 pagesNursing Management For Acute Respiratory FailureEvolynNo ratings yet
- General Pathology 2nd BM Neoplasia Blood Vessel Cardiovascular Pathology Pulmonary PathologyDocument64 pagesGeneral Pathology 2nd BM Neoplasia Blood Vessel Cardiovascular Pathology Pulmonary PathologyCherry RahimaNo ratings yet
- Erico - Ceramic ComponentsDocument4 pagesErico - Ceramic Componentsjaredf@jfelectric.comNo ratings yet
- Clinical Respiratory J - 2022 - Buran Cirak - Effectiveness of 12 Week Inspiratory Muscle Training With Manual Therapy inDocument12 pagesClinical Respiratory J - 2022 - Buran Cirak - Effectiveness of 12 Week Inspiratory Muscle Training With Manual Therapy inZulfah MidahNo ratings yet
- Critical Care NephrologyDocument209 pagesCritical Care NephrologyJohn Karol Ramirez100% (5)
- Eco en UrgenciasDocument25 pagesEco en UrgenciasCristina Regueiro AraujoNo ratings yet