Professional Documents
Culture Documents
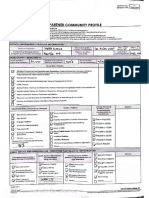
Ampicillin-Rcog Guideline On Pprom
Uploaded by
Rida MfOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ampicillin-Rcog Guideline On Pprom
Uploaded by
Rida MfCopyright:
Available Formats
PRETERM PRELABOUR RUPTURE OF MEMBRANES
This is the first edition of the guideline.
1. Purpose and scope
The aim of this guideline is to make recommendations relating to the diagnosis, investigation and
management of women with preterm prelabour rupture of the membranes (PPROM). The guideline evaluates
various antenatal tests in helping to predict the fetus at risk from intrauterine infection. The role of
prophylactic antibiotics, steroids and tocolytic agents and the optimum gestation to deliver women with
pregnancies complicated by PPROM is examined and recommendations are provided based on published
evidence.
2. Background
PPROM complicates only 2% of pregnancies but is associated with 40% of preterm deliveries and can result
in significant neonatal morbidity and mortality.
13
The three causes of neonatal death associated with PPROM
are prematurity, sepsis and pulmonary hypoplasia. Women with intrauterine infection deliver earlier than non-
infected women and infants born with sepsis have a mortality rate four times higher than those without
sepsis.
4
In addition, there are maternal risks associated with chorioamnionitis.
There is evidence demonstrating an association between ascending infection from the lower genital tract and
PPROM. In women with PPROM about one-third of pregnancies have positive amniotic fluid cultures
5,6
and
studies have shown that bacteria have the ability to cross intact membranes.
7,8
3. Identification and assessment of evidence.
This RCOG guideline was developed in accordance with standard methodology for producing RCOG Green-
top Guidelines. The Cochrane Library (including the Cochrane Database of Systematic Reviews, DARE and
EMBASE), TRIP, Medline and PubMed (electronic databases) were searched for relevant randomised controlled
trials, systematic reviews and meta-analyses. The search was restricted to articles published between 1966 and
2005. The databases were searched using the relevant MeSH terms, including all subheadings, and this was
combined with a keyword search. Search words included preterm prelabour rupture of membranes,
amnioinfusion, sealing amniotic membranes, intra-amniotic infection, Nitrazine, fetal fibronectin,
amniocentesis, antenatal corticosteroids, and tocolytics and the search limited to humans and English
language. The National Library for Health and the National Guidelines Clearing House were also searched for
relevant guidelines and reviews.
1 of 11
RCOG Guideline No. 44
Guideline No. 44
November 2006
4. How is the diagnosis of PPROM best achieved?
The diagnosis of spontaneous rupture of the membranes is best achieved by maternal history followed
by a sterile speculum examination.
Ultrasound examination is useful in some cases to help confirm the diagnosis.
Digital examination should be avoided where PPROM is suspected.
The diagnosis is made by a history suggestive of spontaneous rupture of membranes (SROM)
followed by a sterile speculum examination demonstrating pooling of fluid in the posterior vaginal
fornix; a Nitrazine test is not necessary. Ultrasound examination demonstrating oligohydramnios is
also used to help confirm the diagnosis of spontaneous rupture of the membranes.
912
Digital vaginal examination is best avoided unless there is a strong suspicion that the woman may
be in labour. This is because micro-organisms may be transported from the vagina into the cervix,
leading to intrauterine infection, prostaglandin release and preterm labour. A retrospective study
reported that the latency interval between SROM and delivery in those who had a digital vaginal
examination was significantly shorter than if a sterile speculum examination only was performed.
13
A series of tests have been used to confirm membrane rupture; the most widely used has been the Nitrazine
test, which detects pH change,
14,15
which has a sensitivity of 90% and a false positive rate of 17%.
16
More
recently, other tests have been evaluated in the diagnosis of ruptured membranes and fetal fibronectin and
raised insulin-like growth factor binding protein-1 in cervical/vaginal secretions have reported sensitivities of
94% and 75% and specificities of 97%, respectively.
17,18
5. What antenatal tests should be performed?
Women should be observed for signs of clinical chorioamnionitis at least 12-hourly.
A weekly high vaginal swab and at least a weekly maternal full blood count should be considered.
Fetal monitoring using cardiotocography should be considered where regular fetal surveillance is required.
Biophysical profile scoring or Doppler velocimetry should not be considered as first-line surveillance or
diagnostic tests for fetal infection.
The criteria for the diagnosis of clinical chorioamnionitis include maternal pyrexia, tachycardia, leucocytosis,
uterine tenderness, offensive vaginal discharge and fetal tachycardia. During inpatient observation, the woman
should be regularly examined for such signs of intrauterine infection and an abnormal parameter or a
combination of them may indicate intrauterine infection. The frequency of maternal temperature, pulse and
fetal heart rate auscultation should be between 4 hours and 8 hours.
9,10,19
Maternal pyrexia (above 37.8C), offensive vaginal discharge and fetal tachycardia (rate above 160
beats/minute) indicate clinical chorioamnionitis. There is a variation in the literature regarding the
accuracy of the laboratory tests of leucocytosis and raised C-reactive protein in the prediction of
chorioamnionitis. The sensitivities and false positive rates for leucocytosis in the detection of
clinical chorioamnionitis range from 2947% and 518%, respectively.
9,19
The specificity of C-
reactive protein is 3855%.
9,20,21
Although weekly culture of swabs from the vagina are often taken
as part of the clinical management of women with PPROM, the data evaluating this practice do not
show conclusively that it is beneficial. It has been shown that positive genital tract cultures predict
53% of positive amniotic fluid cultures with a false-positive rate of 25%.
22
However, the presence of
leucocytosis may be useful clinically in cases where there is doubt about the diagnosis of
RCOG Guideline No. 44 2 of 11
B
C
C
Evidence
level IIb
C
B
Evidence
level IIa
chorioamnionitis. Furthermore, high vaginal swabs may indicate group B streptococcus, which
provides the opportunity for intrapartum antibiotic therapy.
Abnormal biophysical profile scores and increased systolic/diastolic ratios in the umbilical artery
have been shown to be markers of intrauterine infection.
23
The true and false positive rates for an
abnormal biophysical profile score in the prediction of clinical chorioamnionitis range from
2580% and 29%, respectively.
2429
Another dataset using positive amniotic fluid and positive fetal
blood cultures as endpoints for infection found that the biophysical profile score or Doppler
studies of the placental or fetal circulation did not provide accurate distinction between infected
and noninfected cases.
11,30
Fetal tachycardia predicts 2040% of cases of intrauterine infection with
a false-positive rate of about 3%.
9,11,31
Cardiotocography is useful because a fetal tachycardia, if
present, may represent a late sign of infection and is frequently used in the clinical definition of
chorioamnionitis in studies.
There are no randomised controlled trials to support the premise that pregnancy outcome is improved by the
use of frequent biophysical or Doppler assessment. The disparity in the literature evaluating these noninvasive
tests of fetal wellbeing suggests that, although some studies have shown benefit, overall the tests are of limited
value in differentiating between fetuses with and without infection.
5.1 What is the role of amniocentesis?
Routine amniocentesis is not recommended for women with PPROM.
Intrauterine infection, as defined by positive amniotic fluid cultures, is found in 36% of women with
PPROM. Most infections are subclinical without obvious signs of chorioamnionitis.
5
Positive
amniotic fluid cultures increase the risks of preterm delivery, neonatal sepsis, respiratory distress
syndrome, chronic lung disease, periventricular leukomalacia, intraventricular haemorrhage and
cerebral palsy.
3234
Current evidence suggests that infection is a cause rather than a consequence of amniorrhexis.
35
Amniocentesis has the potential to detect subclinical infection before the onset of maternal signs
of chorioamnionitis and before the onset of fetal sepsis, allowing appropriate intervention such as
administration of antibiotics in infected cases and/or delivery, depending on the gestation, and
expectant management for women with negative amniotic fluid cultures. Rapid tests on amniotic
fluid such as Gram stain and assay of cytokines such as interleukins 6 and 18, which indicate
intrauterine infection, may be performed.
34,36,37
Although prophylactic antibiotic therapy in cases of PPROM has been shown to have benefits, proponents for
clinical management using amniocentesis argue that treatment should be targeted to appropriate women
because a potential adverse effect of prolonged antibiotic therapy in PPROM includes superinfection with
virulent organisms.
38
It remains to be determined in future studies whether amniocentesis improves
outcomes. Amniocentesis should be performed in specialised units.
Although there are data documenting an association between subclinical intrauterine infection and adverse
neonatal outcome, the role of amniocentesis in improving outcome remains to be determined.
6. Management
6.1 Are prophylactic antibiotics recommended?
Erythromycin (250 mg orally 6 hourly) should be given for 10 days following the diagnosis of PPROM.
3 of 11
RCOG Guideline No. 44
Evidence
level IIa
Evidence
level IIa
B
A
Co-amoxiclav is not recommended for women with PPROM because of concerns about necrotising
enterocolitis.
Twenty-two trials involving over 6000 women with PPROM before 37 weeks were included in a
meta-analysis.
39
The use of antibiotics following PPROM was associated with a statistically
significant reduction in chorioamnionitis (RR 0.57; 95% CI 0.370.86). There was a significant
reduction in the numbers of babies born within 48 hours (RR 0.71; 95% CI 0.580.87) and seven
days (RR 0.80; 95% CI 0.710.90). Neonatal infection was significantly reduced in the babies whose
mothers received antibiotics (RR 0.68; 95% CI 0.530.87). There was also a significant reduction in
the number of babies with an abnormal cerebral ultrasound scan prior to discharge from hospital
(RR 0.82; 95% CI 0.680.98). There was no significant reduction in perinatal mortality although
there was a trend for reduction in the treatment group.
There was a variation in the choice of antibiotics used and the duration of therapy in the studies
examined in the meta-analysis.
39
Ten trials tested broad-spectrum penicillin, either alone or in
combination, five tested macrolide antibiotics (erythromycin) either alone or in combination and
one trial tested clindamycin and gentamycin. The duration of treatment varied between two doses
and 10 days. Any penicillin (except co-amoxiclav) or erythromycin versus placebo was associated
with a significant reduction in the numbers of babies born within 48 hours and who had positive
blood cultures. Co-amoxiclav versus placebo was associated with an increase in the numbers of
babies born with necrotising enterocolitis.
If group B streptococcus is isolated in cases of PPROM, antibiotics should be given in line with the
recommendation for routine intrapartum prophylaxis in the RCOG Green-top Guideline No. 36: Prevention
of Early Onset Neonatal Group B Streptococcal Disease.
4
6.2 What is the role of antenatal corticosteroids?
Antenatal corticosteroids should be administered in women with PPROM.
A meta-analysis of 15 randomised controlled trials involving more than 1400 women with preterm
rupture of the membranes demonstrated that antenatal corticosteroids reduced the risks of
respiratory distress syndrome (RR 0.56; 95% CI 0.460.70), intraventricular haemorrhage (RR, 0.47;
95% CI 0.310.70) and necrotising enterocolitis (RR 0.21; 95% CI 0.050.82). They do not appear
to increase the risk of infection in either mother (RR 0.86; 95% CI 0.611.20) or baby (RR 1.05; 95%
CI 0.661.68).
41
As stated in the RCOG Green-top Guideline No. 7,
42
indications for antenatal corticosteroid therapy include
women with PPROM between 24 and 34 weeks of gestation.
6.3 Tocolysis. Should tocolytic agents be used?
Prophylactic tocolysis in women with PPROM without uterine activity is not recommended.
Women with PPROM and uterine activity who require intrauterine transfer or antenatal corticosteroids
should be considered for tocolysis.
6.3.1 Prophylactic tocolysis
Three randomised studies of a total of 235 women with PPROM reported that the proportion of
women remaining undelivered 10 days after membrane rupture was not significantly higher in
those receiving tocolysis compared with those receiving none.
4345
RCOG Guideline No. 44 4 of 11
A
Evidence
level Ia
A
Evidence
level Ia
A
Evidence
level Ib
A recent retrospective casecontrol study showed that tocolysis after PPROM did not increase the
interval between membrane rupture and delivery or reduce neonatal morbidity.
46
6.3.2 Therapeutic tocolysis
A randomised trial involving 30 women demonstrated that delivery can be inhibited for 24 hours by
intravenous ritodrine.
47
After 24 hours there was no difference in the duration of pregnancy in either group.
A randomised study involving 109 women showed that, for preterm labour associated with preterm rupture
of the membranes after 28 weeks of gestation, there were no significant differences between treatment
groups in intrauterine time after the onset of regular contractions.
48
The results of another randomised study
of 79 women with contractions following PPROM did not suggest that there is benefit to tocolysis in terms
of prolonging the interval to delivery or in reducing perinatal morbidity or mortality.
49
A recent casecontrol
study involving 193 women found that aggressive tocolysis after PPROM did not increase latency or decrease
neonatal morbidity compared with either limited tocolysis or no tocolysis at all.
12
Tocolytic treatment for women in preterm labour was the subject of the RCOG Clinical Guideline No. 1 (B):
Tocolytic Drugs for Women in Preterm Labour.
50
In the absence of clear evidence that tocolysis improves neonatal outcome following PPROM, it is reasonable
not to use it. It is possible that tocolysis could have adverse effects, such as delaying delivery from an infected
environment, since there is an association between intrauterine infection, prostaglandin and cytokine release
and delivery. However, the benefits of antenatal steroids apply equally to women with PPROM and, in some
clinical circumstances, the riskbenefit ratio may lead to consideration of tocolysis for this purpose. Similarly
it would seem wise to consider tocolysis for transfer of women, depending on individual circumstances.
7. Amnioinfusion
Should amnioinfusion in labour be carried out?
Transvaginal amnioinfusion in labour is not recommended for women with preterm rupture of
membranes.
Transabdominal amnioinfusion is not recommended as a method of preventing pulmonary hypoplasia
in very preterm PPROM.
Transvaginal amnioinfusion during labour has been the subject of a Cochrane review
51
where one
randomised controlled trial involving 66 women with SROM between 26 and 35 weeks of gestation
and who received amnioinfusion during labour was examined.
52
The results showed no significant
differences between amnioinfusion and no amnioinfusion for caesarean section, low Apgar scores
and neonatal death. The implication for practice is that there is insufficient evidence to guide
clinical practice concerning the use of amnioinfusion.
A recently published trial of 65 women with PPROM between 24 and 33 weeks of gestation who
were randomised to transabdominal amnioinfusion or expectant management showed that the risk
of postnatal death from pulmonary hypoplasia was similar in both groups.
53
Another casecontrol study involving 24 women reported no difference in the incidence of
pulmonary hypoplasia between controls and treated women.
54
One other recent study involving 71 women with PPROM before 26 weeks of gestation
demonstrated that the percentage of intrauterine fetal survival was higher in treated than in
controlled groups (64.8% versus 32.3%, P < 0.01).
55
5 of 11
RCOG Guideline No. 44
Evidence
level IIa
A
B
Evidence
level Ib
Evidence
level IIb
Evidence
level IIa
At present, there is insufficient evidence to recommend this treatment outside randomised trials. There is
presently a randomised controlled trial comparing expectant management with serial amnioinfusions in
women with early second trimester PPROM.
56
8. Use of fibrin glue
What is the role of fibrin glue in the sealing of chorioamniotic membranes to prevent pulmonary
hypoplasia?
Fibrin sealants are not recommended as routine treatment for second-trimester oligohydramnios
caused by PPROM.
There are publications involving small patient numbers with midtrimester PPROM describing
transvaginal or transabdominal injection of fibrin into the amniotic fluid with the aim of sealing the
membranes.
5759
The amniopatch resulted in an increase in amniotic fluid volume in some cases.
Larger studies are needed when examining neonatal outcome before this treatment can be
recommended as routine practice.
9. Outpatient monitoring
Can patients be monitored at home?
Women should be considered for outpatient monitoring of PPROM only after rigorous individual
selection by a consultant obstetrician.
Outpatient monitoring should be considered only after a period of 4872 hours of inpatient observation
Women should be advised of the signs and symptoms of chorioamnionitis and under what
circumstances they should seek specialist advice.
Women being monitored at home for PPROM should take their temperature twice daily or should be
advised of the symptoms associated with infection.
There should be clearly described local arrangements for the frequency of outpatient visits and what
should be carried out at these visits.
In a randomised study of home versus hospital management outcomes, the two groups were comparable with
a similar latency period and gestational age at delivery.
10
There were no significant differences in the
frequencies of chorioamnionitis, respiratory distress syndrome or neonatal sepsis. However, only 18% of the
women were eligible and agreed to randomisation. The women were randomised after 72 hours in hospital
and 5774%, respectively, in the home and the hospital groups had an amniocentesis for Gram stain and
culture. This study does not support routine home management in women with PPROM but supports rigorous
individual selection of women for this treatment.
There are insufficient data to make recommendations of home, daycare and outpatient monitoring
rather than continued hospital admission in women with PPROM. It would be considered
reasonable to maintain the woman in hospital for at least 48 hours before a decision is made to
allow her to go home. This method of management should be individualised and restricted to
certain groups of women. Women should be instructed to take regular temperature recordings at
home every 12 hours or to be aware of the symptoms associated with infection.
RCOG Guideline No. 44 6 of 11
B
Evidence
level III
B
Evidence
level III
10. Delivery of the fetus
When is the appropriate time to deliver?
Delivery should be considered at 34 weeks of gestation.
Where expectant management is considered beyond 34 weeks of gestation, women should be
counselled about the increased risk of chorioamnionitis and its consequences versus the decreased risk
of serious respiratory problems in the neonate, admission for neonatal intensive care and caesarean
section.
Many studies have demonstrated benefits in conservative management for gestations of less than 34 weeks,
whereas the management of pregnancies complicated by PPROM between 34 and 37 weeks of gestation
continues to be a contentious issue.
60
A recent retrospective study examining 430 women with PPROM demonstrated that composite
neonatal minor morbidity such as hyperbilirubinaemia and transient tachypnoea of the newborn
was significantly higher among pregnancies delivered at 34 weeks of gestation or less as compared
with those delivered at 36 weeks.
61
Composite major neonatal morbidity, including respiratory
distress syndrome and intraventricular haemorrhage, was significantly higher among pregnancies
delivered at 33 weeks of gestation or less as compared with those delivered at 36 weeks. There was
no difference in the major morbidity rates for those pregnancies delivered beyond 34 weeks. The
authors conclusion was that expectant management at 34 weeks and beyond is of limited benefit.
A randomised trial assigning 93 women with PPROM between 32 weeks and 36 weeks and 6 days
of gestation either to immediate or delayed delivery showed that the incidence of respiratory
distress syndrome, intraventricular haemorrhage and confirmed neonatal sepsis was not
significantly different in the two groups.
62
Although, in the expectantly managed group, the 27.7%
incidence of chorioamnionitis was higher than the 10.9% in the induced group, this difference did
not reach statistical significance.
In another report, 129 women with PPROM between 30weeks and 34 weeks of gestation were
randomly assigned to either immediate delivery or expectant management.
63
The mean gestational
age at delivery was 31.7 weeks in the immediate delivery group and 32 weeks in that managed
expectantly. Although the incidence of chorioamnionitis was significantly less in the immediate
delivery group (2%) as compared with the expectant management group (15%; P < 0.05), there
were no significant differences between the groups with regard to neonatal morbidity.
In a prospective randomised study of 120 women with PPROM between 34 weeks and 37 weeks
of gestation, the expectantly managed group had a higher incidence of chorioamnionitis (16%)
compared with the immediate delivery group (2%, P < 0.05). The incidence of sepsis was 5% in the
expectantly managed group and 0% in the immediate delivery group but this was not statistically
significant. There was no difference in the risk of respiratory distress syndrome.
60
A retrospective series examining neonatal outcome following cases with PPROM between 32 weeks and 36
weeks showed that the specific gestation for reduced morbidity was 34 weeks.
64
The incidence of respiratory
distress syndrome and the length of hospital stay were reduced in infants delivered after 34 weeks of
gestation. The incidence of respiratory distress syndrome was 22.5% and 5.8% at 33 and 34 weeks,
respectively. Although the incidence beyond 34 weeks was relatively low, the condition affected infants into
the 36th week, with incidences of 10.41.5% at 35 and 36 weeks, respectively.
Data from existing studies call for further research to elucidate the optimal delivery gestational age for women
7 of 11
RCOG Guideline No. 44
B
B
Evidence
level III
Evidence
level Ib
References
1. Maxwell GL. Preterm premature rupture of membranes. Obstet
Gynecol Surv 1993;48:57683.
2. Merenstein GB, Weisman LE. Premature rupture of the
membranes: neonatal consequences. Semin Perinatol
1996;20:37580.
3. Douvas SG, Brewer JMJ, McKay ML, Rhodes PGJ, Kahlstorf JH,
Morrison JC. Treatment of preterm rupture of the membranes.
J Reprod Med 1984;29:7414.
4. Cotton DB, Hill LM, Strassner HT, Platt LD, Ledger WJ. Use of
amniocentesis in preterm gestation with ruptured membranes.
Obstet Gynecol 1984;63:3848.
5. Carroll SG, Sebire NJ, Nicolaides KH. Pre-term pre-labour
amniorrhexis. Curr Opin Obstet Gynecol 1996;8:4418
6. Broekhuizen FF, Gilman M, Hamilton PR. Amniocentesis for
Gram Stain and culture in preterm premature rupture of the
membranes. Obstet Gynecol 1985;66:31621.
7. Galask RP, Varner MW, Petzold CR, Wilbur SL. Bacterial
Aattachment to the chorioamnioticnic membranes. Am J Obstet
Gynecol 1984; 148: 91528.
8. Gyr TN, Malek A, MathezLoic, Altermatt HJ, Bodmer R,
Nicolaides, et al. Permeation of human chorioamniotic
membranes by Escherichia coli in vitro. Am J Obset Gynecol
1994;170:2237.
9. Ismail A, Zinaman MJ, Lowensohn RI, Moawad AH. The
significance of Creactive protein levels in women with
premature rupture of membranes. Am J Obstet Gynecol
1985;151:5414.
10. Carlan SJ, OBrien WF, Parsons MT, Lense JJ. Preterm premature
rupture of membranes: a randomised study of home versus
hospital management. Obstet Gynecol 1993;81:614.
11. Carroll SG, Papiaoannou S, Nicolaides KH. Assessment of fetal
activity and amniotic fluid volume in the prediction of
intrauterine infection in preterm prelabour amniorrhexis. Am J
Obstet Gynecol 1995;172:142735.
12. Combs CA, McCune M, Clark R, Fishman A. Aggressive tocolysis
does not prolong pregnancy or reduce neonatal morbidity after
preterm premature rupture of the membranes. Am J Obstet
Gynecol 2004;190:172831.
13. Lewis DF, Major CA, Towers CV, Asrat T, Harding JA, Garite TJ.
Effects of digital vaginal examination on latency period in
preterm premature rupture of membranes. Am J Obstet
Gynecol 1992;80:6304.
14. Baptisti A. Chemical test for the determination of ruptured
membranes. Am J Obstet Gynecol 1938;35:68890.
15. Abe T. The detection of rupture of the fetal membranes with the
nitrazine indicator. Am J Obstet Gynecol 1940;39:4004.
16. Friedman ML, McElin TW. Diagnosis of ruptured fetal
membranes. Clinical study and review of the literature. Am J
Obstet Gynecol 1969;104:54450.
17. Gaucherand P, Guibaud S, Awada A, Rudigoz RC. Comparative
study of three amniotic fluid markers in premature of
membranes: fetal fibronectin, alpha-fetoprotein, diamino-
oxydase. Acta Obstet Gynecol Scand 1995, 74:11821.
18. Rutanen EM, Pekonen F, Karkkainen T. Measurement of insulin-
like growth factor binding protein-1 in cervical/vaginal
secretions: comparison with the ROM-check Membrane
Immunoassay in the diagnosis of ruptured fetal membranes.
Clin Chim Acta 1993;214:7381.
19. Romem Y, Artal R. C-reactive protein as a predictor for
chorioamnionitis in cases of premature rupture of the
membranes. Am J Obstet Gynecol 1984;150:54650.
20. Watts DH, Krohn MA, Hillier SL, Wener MH, Kiviat NB,
Eschenbach DA. Characteristics of women in preterm labour
associated with elevated C-reactive protein levels. Obstet
Gynecol 1993;82:50914.
21. Kurki T, Teramo K, Ylikorkala O, Paavonen J. C-reactive protein in
preterm premature rupture of the membranes. Arch Gynecol
Obstet 1990;247:317.
22. Carroll SG, Papaioannou S, Ntumazah IL, Philpott-Howard J,
Nicolaides KH. Lower genital tract swabs in the prediction of
intrauterine infection in preterm prelabour rupture of the
membranes. BJOG 1996;103:5459.
23. Yucel N, Yucel O, Yekeler H. The relationship between umbilical
artery Doppler findings, fetal biophysical score and placental
inflammation in cases of premature rupture of membranes.
Acta Obstet Gynecol Scand 1997;76:5325.
24. Vintzileos AM, Campbell WA, Nochimson DJ, Weinbaum PJ,
Mirochnick MH, Escoto DT. Fetal biophysical profile versus
amniocentesis in predicting infection in preterm premature
rupture of the membranes. Obstet Gynecol 1986;68:48894.
25. Goldstein I, Romero R, Merrill S, OConnor WM, Mazor M,
Hobbins JC. Fetal body and breathing movements as predictors
of intraamniotic infection in preterm premature rupture of
membranes. Am J Obstet Gynecol 1988;159:3638.
26. Roussis P, Rosemond RL, Glass C, Boehm F. Preterm premature
rupture of membranes: detection of infection. Am J Obstet
Gynecol 1991;165:1099104.
27. Del Valle GO, Joffe GM, Izquierdo LA, Smith JF, Gilson GJ, Curet
LB. The biophysical profile and the nonstress test: poor
predictors of chorioamnionitis and fetal infection in prolonged
preterm premature rupture of membranes. Obstet Gynecol
1992;80:10610.
28. Gauthier DW, Meyer WJ, Bieniarz A. Biophysical profile as a
predictor of amniotic fluid culture results. Obstet Gynecol
1992;80:1025.
29. Lewis DF,Adair CD,Weeks JW,Barrilleaaux PS,Edwards MS,Garite
TJ. A randomised clinical trial of daily nonstress testing versus
biophysical profile in the management of preterm premature
rupture of membranes. Am J Obstet Gynecol 1999;181:14959.
30. Carroll SG, Papiaoannou S, Nicolaides KH. Doppler studies
of the placental and fetal circulation in pregnancies with
preterm prelabour amniorrhexis. Ultrasound Obstet Gynecol
1995;5:1848.
31. Ferguson MG, Rhodes PG, Morrison JC, Puckett CM. Clinical
amniotic fluid infection and its effect on the neonate. Am J
Obstet Gynecol 19895;151:105861.
with PPROM between 34 weeks and 37 weeks of gestation. There are currently two ongoing randomised
controlled trials comparing intentional delivery versus conservative management in women with PPROM
between 32 weeks and 35 weeks: Lacaze-Masmonteil T, Chari R, University of Alberta; Clinical Trials.gov
identifier NCT00259519
65
and Morris J, Royal North Shore Hospital, Australia, ISRCTN 44485060.
66
Details of
the trials can be found at: www.clinicaltrials.gov/ct/show/.
Until then, published data question the benefit of continued expectant management beyond 34 weeks of
gestation. There is little evidence that intentional delivery after 34 weeks adversely affects neonatal outcome.
There is a suggestion from these studies that expectant management beyond 34 weeks is associated with an
increased risk of chorioamnionitis.
RCOG Guideline No. 44 8 of 11
9 of 11
RCOG Guideline No. 44
32. Yoon BH, Jun JK, Romero R et al. Amniotic fluid inflammatory
cytokines (interleukin-6, interleukin-1beta, and tumor necrosis
factor-alpha), neonatal brain white matter lesions, and cerebral
palsy. Am J Obstet Gynecol 1997;177:1926.
33. Yoon BH, Romero R, Jun JK et al. Amniotic fluid cytokines
(interleukin-6, tumor necrosis factor-alpha, interleukin-1 beta,
and interleukin-8) and the risk for the development of broncho-
pulmonary dysplasia. Am J Obstet Gynecol 1997;177:82530.
34. Yoon BH, Park CW, Chaiworapongsa T. Intrauterine infection
and the development of cerebral palsy. BJOG 2003;110:Suppl
20:1247
35. Carroll SG, Ville Y, Greenough A, Gamsu H, Patel B,
PhilpottHoward J, Nicolaides KH. Preterm prelabour
amniorrhexis: Intrauterine infection and interval between
membrane rupture and delivery. Arch Dis Child Fetal Neonatal
Ed 1995;72:F4346.
36. Jacobsson B, Holst RM, Mattsby-Baltzer I, Nikolaitchouk N,
Wennerholm UB, Hagberg H. Interleukin-18 in cervical mucus
and amniotic fluid: relationship to microbial invasion of the
amniotic fluid, intra-amniotic inflammation and preterm
delivery. BJOG 2003;110:598603.
37. Coultrip LL, Grossman JH. Evaluation of rapid diagnostic tests in
the detection of microbial invasion of the amniotic cavity. Am
J Obstet Gynecol 1992;167:123142.
38. Blackwell SC, Berry SM. Role of amniocentesis for the diagnosis
of subclinical intraamniotic infection in preterm premature
rupture of the membranes. Curr Opin Obstet Gynecol
1999;11:54147.
39. Kenyon S, Boulvain M, Neilson J.Antibiotics for preterm rupture
of membranes.Cochrane Database Syst Rev 2003;(2):CD001058.
40. Royal College of Obstetricians and Gynaecologists. Prevention
of Early Onset Neonatal Group B Streptococcal Disease. Green-
top Guideline No. 36. London: RCOG; 2003.
41. Harding JE, Pang J, Knight DB, Liggins GC. Do antenatal
corticosteroids help in the setting of preterm rupture of
membranes. Am J Obstet Gynecol 2001;184:1319.
42. Royal College of Obstetricians and Gynaecologists. Antenatal
Corticosteroids to Prevent Respiratory Distress Syndrome.
Green-top Guideline No.7. London: RCOG; 2004.
43. How HY, Cook CR, Cook VD, Miles DE, Spinnato JA. Preterm
premature rupture of membranes: aggressive tocolysis versus
expectant management. J Matern Fetal Med 1998;7:812.
44. Levy D, Warsof SL. Oral ritodrine and preterm premature
rupture of membranes. Obstet Gynecol 1985;66:62133.
45. Dunlop PDM, Crowley PA, Lamont RF, Hawkins DF. Preterm
ruptured membranes, no contractions. J Obstet Gynecol.
1986;7:926.
46. Jazayeri A, Jazayeri MK, Sutkin G. Tocolysis does not improve
neonatal outcome in patients with preterm rupture of
membranes. Am J Perinatol. 2003;20:18993.
47. Christensen KK, Ingemarsson I, Leiderman T, Solum H,
Svenningsen N. Effect of ritodrine on labour after premature
rupture of the membranes. Obstet Gynecol 1980;55:18790.
48. Weiner CP, Renk K, Klugman M. The therapeutic efficacy and
costeffectiveness of aggressive tocolysis for premature labor
associated with premature rupture of the membranes. Am J
Obstet Gynecol 1988;159:21622.
49. Garite TJ, Keegan KA, Freeman RK, Nageotte MP. A randomised
trial of ritodrine tocolysis versus expectant management in
patients with premature rupture of membranes at 25 to 30
weeks of gestation. Am J Obstet Gynecol 1987;157:38893.
50. Royal College of Obstetricians and Gynaecologists. Tocolytic
Drugs for Women in Preterm Labour. Green-top Guideline No.
1b. London:RCOG; 2002.
51. Hofmeyr GJ. Amnioinfusion for preterm rupture of membranes.
Cochrane Database Syst Rev 2000;(2):CD000942.
52. Nageotte MP, Freeman RK, Garite TJ, Dorchester W. Prophylactic
intrapartum amnioinfusion in patients with preterm premature
rupture of membranes. Am J Obstet Gynecol 1985;153:55762.
53. Tranquilli AL, Giannubilo SR, Bezzeccheri V, Scagnoli C.
Transabdominal amnioinfusion in preterm premature rupture
of membranes: a randomised controlled trial. BJOG
2005;112:75963.
54. Ogunyemi D, Thompson W. A case controlled study of serial
transabdominal amnioinfusions in the management of second
trimester oligohydramnios due to premature rupture of
membranes. Eur J Obstet Gynceol Reprod Biol 2002;102:16772.
55. De Santis M, Scavvo M, Noia G, Masini L, Piersigilli F, Romagnoli
C, Caruso A. Transaabdominal amnioinfusion treatment of
severe oligohydramnios in preterm premature rupture of
membranes at less than 26 gestational weeks. Fetal Diagn Ther
2003;18:41217.
56. Roberts D. Amnio infusion in preterm premature rupture of
membranes (AMIPROM) study. Liverpool Womens Hospital
NHS Trust. ISRCTN 81932589.
57. Quintero RA, Morales WJ, Allen M, Bornick PW, Arroyo J, Le Parc
G. Treatment of iatrogenic previable premature rupture of
membranes with intra-amniotic infection of platelets and
cryoprecipitate (amniopatch): preliminary experience. Am J
Obstet Gynecol 1999;181:7449.
58. Sciscione AC, Manley JS, Pollock M, Maas B, Shlossman PA, Mulla
W, et al. Intracervical fibrin sealants: a potential treatment for
early preterm premature rupture of the membranes. Am J
Obstet Gynecol. 2001;184:36873.
59. Young BK, Roque H, Abdelhak YF, Poiolek D, Demopulos R,
Lockwood CJ. Minimally invasive endoscopy in the treatment
of preterm premature rupture of membranes by application of
fibrin sealant. J Perinat Med 2000;28:32630.
60. Naef RW 3rd, Allbert JR, Ross EL, Weber M, Martin RW, Morriso
JC. Premature rupture of membranes at 34 to 37 weeks
gestation: aggressive versus conservative management. Am J
Obstet Gynecol 1998;178:12630.
61. Lieman JM, Brumfield CG, Carlo W, Ramsey PS. Preterm
premature rupture of membranes: is there an optimal
gestational age for delivery. Obstet Gynecol 2005;105:1217.
62. Mercer BM, Crocker RN, Boe NM, Sibai BM. Induction versus
expectant management in premature rupture of the
membranes with mature amniotic fluid at 32 to 36 weeks: a
randomized trial. Am J Obstet Gynecol. 1993;169:77582.
63. Cox SM, Leveno KJ. Intentional delivery versus expectant
management with preterm ruptured membranes at 3034
weeks gestation. Obstet Gynecol 1995;86:8759.
64. Neerhof MG, Cravello C, Haney EI, Silver RK. Timing of labor
induction after premature rrupture of membranes between 32
and 36 weeks gestation. Am J Obstet Gynecol 1999;180:34952.
65. Lacaze-Masmonteil T, Chari R. Safety and Efficacy of Intentional
Delivery in Women with Preterm and Prelabour Rupture of the
Membranes. University of Alberta, USA. NCT00259519.
66. Morris J. A randomised controlled trial of immediate delivery
versus expectant care in women with ruptured membranes
close to term. Australian National Health and Medical Research
Council. 2005. Royal North Shore Hospital, Australia, ISRCTN
44485060.
RCOG Guideline No. 44 10 of 11
Grades of recommendations
Requires at least one randomised
controlled trial as part of a body of
literature of overall good quality and
consistency addressing the specific
recommendation. (Evidence levels Ia, Ib)
Requires the availability of well controlled
clinical studies but no randomised clinical
trials on the topic of recommendations.
(Evidence levels IIa, IIb, III)
Requires evidence obtained from expert
committee reports or opinions and/or
clinical experiences of respected
authorities. Indicates an absence of directly
applicable clinical studies of good quality.
(Evidence level IV)
Good practice point
Recommended best practice based on the
clinical experience of the guideline
development group.
Classification of evidence levels
Ia Evidence obtained from meta-analysis of
randomised controlled trials.
Ib Evidence obtained from at least one
randomised controlled trial.
IIa Evidence obtained from at least one
well-designed controlled study without
randomisation.
IIb Evidence obtained from at least one
other type of well-designed quasi-
experimental study.
III Evidence obtained from well-designed
non-experimental descriptive studies,
such as comparative studies, correlation
studies and case studies.
IV Evidence obtained from expert
committee reports or opinions and/or
clinical experience of respected
authorities.
C
B
A
APPENDIX
Clinical guidelines are: systematically developed statements which assist clinicians and patients in
making decisions about appropriate treatment for specific conditions. Each guideline is systematically
developed using a standardised methodology. Exact details of this process can be found in Clinical
Governance Advice No. 1: Guidance for the Development of RCOG Green-top Guidelines (available on
the RCOG website at www.rcog.org.uk/clingov1). These recommendations are not intended to dictate
an exclusive course of management or treatment. They must be evaluated with reference to individual
patient needs, resources and limitations unique to the institution and variations in local populations. It is
hoped that this process of local ownership will help to incorporate these guidelines into routine
practice. Attention is drawn to areas of clinical uncertainty where further research may be indicated.
The evidence used in this guideline was graded using the scheme below and the recommendations
formulated in a similar fashion with a standardised grading scheme.
11 of 11
RCOG Guideline No. 44
This guideline was produced on behalf of the Guidelines and Audit Committee of the Royal College of Obstetricians
and Gynaecologists by:
Mr SGM Carroll FRCOG, Dublin, Ireland
and peer reviewed by:
British Association of Perinatal Medicine; Dr PJ Danielian FRCOG, Aberdeen; Professor D Edwards, Professor of
Paediatrics, Hammersmith Hospital, London; Mr DI Fraser MRCOG, Norfolk; Ms J Grant, Pharmacist, Princess Royal
Maternity Hospital, Glasgow; Mr A Gouveia, Obstetrician and Gynaecologist, Maternidade de Julio Dinis, Portugal;
Ms S Kenyon, Senior Research Fellow, Leicester Royal Infirmary, Leicester; Mr KT Moriarty MRCOG, London;
Mr J Morris, Professor Obstetrics and Gynaecology and Maternal Fetal Medicine Specialist, University of Sydney, Sydney;
RCOG Consumers Forum; Dr Roberts MRCOG, Liverpool; Royal College of Midwives; Dr NC Smith FRCOG, Aberdeen;
Professor DJ Taylor FRCOG, Leicester; Mr J Wyatt, Professor of Neonatal Paediatrics, University College London
Medical School, The Rayne Institute, London.
The Guidelines and Audit Committee lead peer reviewers were:
Professor DJ Murphy MRCOG, Dublin, Ireland; Mr SA Walkinshaw FRCOG, Liverpool; and Dr RG Hughes FRCOG, Edinburgh.
The final version is the responsibility of the Guidelines and Audit Committee of the RCOG.
DISCLAIMER
The Royal College of Obstetricians and Gynaecologists produces guidelines as an educational aid to good clinical
practice. They present recognised methods and techniques of clinical practice, based on published evidence, for
consideration by obstetricians and gynaecologists and other relevant health professionals. The ultimate judgement
regarding a particular clinical procedure or treatment plan must be made by the doctor or other attendant in the light
of clinical data presented by the patient and the diagnostic and treatment options available.
This means that RCOG Guidelines are unlike protocols or guidelines issued by employers, as they are not intended to
be prescriptive directions defining a single course of management. Departure from the local prescriptive protocols or
guidelines should be fully documented in the patients case notes at the time the relevant decision is taken.
Valid until November 2009
unless otherwise indicated
You might also like
- Guide to Pediatric Urology and Surgery in Clinical PracticeFrom EverandGuide to Pediatric Urology and Surgery in Clinical PracticeNo ratings yet
- Preterm Prelabour Rupture of MembranesDocument12 pagesPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanNo ratings yet
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsFrom EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsNo ratings yet
- Manage PPROM to Lower Infection RiskDocument6 pagesManage PPROM to Lower Infection RiskResi Lystianto PutraNo ratings yet
- Premature Rupture of Membrane ReadingDocument4 pagesPremature Rupture of Membrane ReadingAdrienne Nicole AlforteNo ratings yet
- Rcog PpromDocument7 pagesRcog PpromDevi SyamNo ratings yet
- Labor Induction in The Patient With Preterm Premature Rupture of MembranesDocument6 pagesLabor Induction in The Patient With Preterm Premature Rupture of MembranesYudhi AuliaNo ratings yet
- Premature Rupture of Membranes at Term GuideDocument12 pagesPremature Rupture of Membranes at Term GuideCitra YuliasariNo ratings yet
- 2 Comparison of Maternal CRP With WBC Count in Predicting Intra Amniotic Infection in Premature Rupture of MembranesDocument4 pages2 Comparison of Maternal CRP With WBC Count in Predicting Intra Amniotic Infection in Premature Rupture of MembranesDeomicah SolanoNo ratings yet
- PromDocument15 pagesPromEstefan Johannes VillaranNo ratings yet
- PROM Management and OutcomesDocument6 pagesPROM Management and OutcomesRayhan AlatasNo ratings yet
- Obgyn Ob PRPM Pt1 13Document6 pagesObgyn Ob PRPM Pt1 13SalmonteNo ratings yet
- PROM Dilemmas: Choosing A Strategy, Knowing When To Call It QuitsDocument8 pagesPROM Dilemmas: Choosing A Strategy, Knowing When To Call It QuitsRohmantuah_Tra_1826No ratings yet
- 10-Manejo de RPMDocument11 pages10-Manejo de RPMMelissa Garcia SandovalNo ratings yet
- Antepartum HaemorrhageDocument23 pagesAntepartum HaemorrhageSutanti Lara DewiNo ratings yet
- 37004-Article Text-130842-2-10-20180629Document5 pages37004-Article Text-130842-2-10-20180629nishita biswasNo ratings yet
- Pregnancy Complication: Department of Gynaecology and ObstetricsDocument40 pagesPregnancy Complication: Department of Gynaecology and ObstetricssanjivdasNo ratings yet
- Obstetrics 2Document7 pagesObstetrics 2Tommy FebriantoNo ratings yet
- Antepartum Hemorrhage PDFDocument23 pagesAntepartum Hemorrhage PDFfrizkapfNo ratings yet
- Premature Rupture of Membranes: Diagnosis and ManagementDocument17 pagesPremature Rupture of Membranes: Diagnosis and ManagementFahmi Sulistyo HutomoNo ratings yet
- Pi Is 0020729213005055Document4 pagesPi Is 0020729213005055Winna Eka PNo ratings yet
- Scopus (29) Many2017Document7 pagesScopus (29) Many2017ika puspitaNo ratings yet
- Journal Pone 0105882Document7 pagesJournal Pone 0105882Ayu Wedhani SpcNo ratings yet
- Prom Preterm and PosttermDocument127 pagesProm Preterm and PosttermgibreilNo ratings yet
- Fetal Inflamatory Response SyndromeDocument9 pagesFetal Inflamatory Response SyndromeAnonymous mvNUtwidNo ratings yet
- Fetal screening in the second trimesterDocument3 pagesFetal screening in the second trimesterYwagar Ywagar100% (1)
- 61 Goepfert2004Document7 pages61 Goepfert2004angela_karenina_1No ratings yet
- Preterm: Intrauterine Infection and LaborDocument9 pagesPreterm: Intrauterine Infection and LaborabcdeNo ratings yet
- Premature Rupture of MembranesDocument8 pagesPremature Rupture of Membraneshadi_abdNo ratings yet
- Meconium PpromDocument7 pagesMeconium Ppromkutra3000No ratings yet
- Outcome of Neonates Born To Mothers With Premature Rupture of MembranesDocument5 pagesOutcome of Neonates Born To Mothers With Premature Rupture of MembranesDevi SilalahiNo ratings yet
- Premature Rupture of MembranesDocument9 pagesPremature Rupture of MembranesYessica MelianyNo ratings yet
- 77754571Document7 pages77754571stephaniedianNo ratings yet
- Dip 2013Document17 pagesDip 2013mariajuliabechepecheNo ratings yet
- Acta Obstet Gynecol Scand - 2011 - MARIA PATERNOSTER - Cervical phIGFBP 1 in The Evaluation of The Risk of Preterm deDocument5 pagesActa Obstet Gynecol Scand - 2011 - MARIA PATERNOSTER - Cervical phIGFBP 1 in The Evaluation of The Risk of Preterm dePriscilla GeraldineNo ratings yet
- Management Outcome of Premature Rupture of Membranes in A Tertiary Health Facility in South Western NigeriaDocument7 pagesManagement Outcome of Premature Rupture of Membranes in A Tertiary Health Facility in South Western NigeriaSulis SipinNo ratings yet
- JurnalDocument7 pagesJurnalAlifiya Changmin CassiopeiaNo ratings yet
- Frequency, Causes and Outcome of PolyhydramniosDocument4 pagesFrequency, Causes and Outcome of PolyhydramniosMina LelymanNo ratings yet
- TOG Evolution in Screening For Down SyndromeDocument7 pagesTOG Evolution in Screening For Down SyndromeMarNo ratings yet
- BJOG 2014 GBS Và PROMDocument10 pagesBJOG 2014 GBS Và PROMHòa HồNo ratings yet
- Sepsis Neonatal 2012 PeiatricsDocument12 pagesSepsis Neonatal 2012 PeiatricsWalter LojaNo ratings yet
- Predictive value of maternal s erum β-hCG concentration in the ruptured tubal ectopic pregnancyDocument7 pagesPredictive value of maternal s erum β-hCG concentration in the ruptured tubal ectopic pregnancyyayayaNo ratings yet
- OligohidramnionDocument9 pagesOligohidramnionRizki R. WahidahNo ratings yet
- Aafp Pprom PDFDocument6 pagesAafp Pprom PDFGerry SanjayaNo ratings yet
- Study On Preterm Pre Mature Rupture of Membrane With Special Reference To Maternal and Its Fetal OutcomeDocument7 pagesStudy On Preterm Pre Mature Rupture of Membrane With Special Reference To Maternal and Its Fetal OutcomeBEREKETNo ratings yet
- Etiologi Diagnosis PPROM-dikonversiDocument46 pagesEtiologi Diagnosis PPROM-dikonversiDokumen BiasaNo ratings yet
- BJOG - 2019 - Thomson - Care of Women Presenting With Suspected Preterm Prelabour Rupture of Membranes From 24 0 Weeks ofDocument15 pagesBJOG - 2019 - Thomson - Care of Women Presenting With Suspected Preterm Prelabour Rupture of Membranes From 24 0 Weeks ofdindacNo ratings yet
- Malaria in Pregnancy A Literature Review JournalDocument4 pagesMalaria in Pregnancy A Literature Review Journalc5p0cd99100% (1)
- Sepsis Management of Neonates With Suspected or Proven Early-Onset BacterialDocument12 pagesSepsis Management of Neonates With Suspected or Proven Early-Onset BacterialAldo CancellaraNo ratings yet
- (Journal of Perinatal Medicine) Management of Prelabour Rupture of Membranes (PROM) at TermDocument3 pages(Journal of Perinatal Medicine) Management of Prelabour Rupture of Membranes (PROM) at TermSofri m.tahirNo ratings yet
- Alteration of The Amniotic Fluid and Neonatal Outcome 2004Document5 pagesAlteration of The Amniotic Fluid and Neonatal Outcome 2004Sergio CuervoNo ratings yet
- Aggressive Intervention of Previable Preterm Premature Rupture of MembranesDocument8 pagesAggressive Intervention of Previable Preterm Premature Rupture of MembranesVanessa Riaño GodoyNo ratings yet
- Congenital Toxoplasmosis TXDocument6 pagesCongenital Toxoplasmosis TXHervi LaksariNo ratings yet
- AsdasfasfvDocument7 pagesAsdasfasfvPulseWangminNo ratings yet
- O@g Maternal and Fetal Mesures ContentDocument22 pagesO@g Maternal and Fetal Mesures Contentjeya maniNo ratings yet
- Bedah JurnalDocument5 pagesBedah JurnalMastura AjaNo ratings yet
- Genetic Counselling and Prenatal ScreeningDocument8 pagesGenetic Counselling and Prenatal ScreeningFarheen khanNo ratings yet
- Managing Placenta Accreta: Medical vs Surgical OptionsDocument9 pagesManaging Placenta Accreta: Medical vs Surgical OptionsAslesa Wangpathi PagehgiriNo ratings yet
- Meconium-Stained Amniotic Fluid: A Risk Factor For Postpartum HemorrhageDocument5 pagesMeconium-Stained Amniotic Fluid: A Risk Factor For Postpartum HemorrhagelaniNo ratings yet
- Delirium in The ElderlyDocument8 pagesDelirium in The Elderlyloko_knvbNo ratings yet
- 4.4.7.5 APEC PROM Guidelines 11-13-13 PDFDocument7 pages4.4.7.5 APEC PROM Guidelines 11-13-13 PDFAnnisa Rizki Ratih PratiwiNo ratings yet
- Obstetrics 4Document9 pagesObstetrics 4Darrel Allan MandiasNo ratings yet
- Aip Chap16 PromDocument6 pagesAip Chap16 PromRida MfNo ratings yet
- J Neurol Neurosurg Psychiatry 2004 Burns 362 7Document7 pagesJ Neurol Neurosurg Psychiatry 2004 Burns 362 7Paty DiazNo ratings yet
- Jurnal HipospadiaDocument13 pagesJurnal HipospadiaIndra PudlianNo ratings yet
- Gui 294 CPG1307 EDocument11 pagesGui 294 CPG1307 ERida MfNo ratings yet
- Histopathology and ImmunopathologyDocument2 pagesHistopathology and ImmunopathologyRida MfNo ratings yet
- Tuition FeeDocument2 pagesTuition FeeRida MfNo ratings yet
- Jurnal HipospadiaDocument13 pagesJurnal HipospadiaIndra PudlianNo ratings yet
- Akademos Cme 203 Afc0fa9eDocument16 pagesAkademos Cme 203 Afc0fa9eRida MfNo ratings yet
- OPENMINDDocument17 pagesOPENMINDRida MfNo ratings yet
- J 1742-6723 2011 01455 X PDFDocument12 pagesJ 1742-6723 2011 01455 X PDFRida MfNo ratings yet
- Depsite 1Document61 pagesDepsite 1Rida MfNo ratings yet
- A Woman Brought Her Husband To The Emergency Room With Weakness of His Right FaceDocument1 pageA Woman Brought Her Husband To The Emergency Room With Weakness of His Right FaceRida MfNo ratings yet
- Aa 11Document5 pagesAa 11Eriekafebriayana RNo ratings yet
- Ascorbic Acid Drug StudyDocument1 pageAscorbic Acid Drug Studyahmad ryan100% (1)
- NCP DrainageDocument3 pagesNCP DrainageRuby GuarinNo ratings yet
- ENDOCHAT 162 Uriel JOE 2016 PDFDocument9 pagesENDOCHAT 162 Uriel JOE 2016 PDFMaria Camila Sarmiento100% (1)
- COVID-19 Case Investigation Form InsightsDocument1 pageCOVID-19 Case Investigation Form InsightsAlpha BatteryNo ratings yet
- Psychiatric Social WorkDocument4 pagesPsychiatric Social WorkBora Deepak PrinceNo ratings yet
- FREE NLE REVIEW Fundies and OthersDocument40 pagesFREE NLE REVIEW Fundies and OthersAngel Lopez100% (1)
- Introduction: What Is Hiv and Aids?Document6 pagesIntroduction: What Is Hiv and Aids?Hasib AhmedNo ratings yet
- EBPM Dalam Audit Operasional BPJS KesehatanDocument8 pagesEBPM Dalam Audit Operasional BPJS KesehatanluciaNo ratings yet
- Post Operative Care of PatientsDocument37 pagesPost Operative Care of Patientsapi-370869850% (2)
- EEReview PDFDocument7 pagesEEReview PDFragavendharNo ratings yet
- Dwi Warna Aju FatmawatiDocument4 pagesDwi Warna Aju FatmawatiAnonymous FiiSmGgNo ratings yet
- Fina Violita Christi-PaperDocument5 pagesFina Violita Christi-PaperFina ViolitaNo ratings yet
- CCJC BodinDocument2 pagesCCJC Bodinapi-495663503No ratings yet
- Maternal Fetal AttachmentDocument14 pagesMaternal Fetal AttachmentNida Tsaura SNo ratings yet
- Pathology Situational EthicsDocument28 pagesPathology Situational Ethicsmohitsingla_86No ratings yet
- Assignment On Unconciousness: Subject:-Advanced Nursing PracticeDocument15 pagesAssignment On Unconciousness: Subject:-Advanced Nursing PracticeShaells JoshiNo ratings yet
- SDCEP Periodontal Disease Guidance in BriefDocument19 pagesSDCEP Periodontal Disease Guidance in BriefLupu AndreeaNo ratings yet
- FNCP Inadquate Nutrition IntakeDocument3 pagesFNCP Inadquate Nutrition Intakekat_leon_250% (2)
- CPD Nursing Care PlanDocument2 pagesCPD Nursing Care PlanFaye Dianne Damian-BuenafeNo ratings yet
- Clinical Assessment and Examination in OrthopedicsDocument196 pagesClinical Assessment and Examination in OrthopedicsMom of twoNo ratings yet
- Shalu Bathla - Chronic PeriodontitisDocument6 pagesShalu Bathla - Chronic PeriodontitisFerdinan PasaribuNo ratings yet
- Study On Empowering Youth and Adults To Overcome Mental Health Hardships Using A Web ApplicationDocument6 pagesStudy On Empowering Youth and Adults To Overcome Mental Health Hardships Using A Web ApplicationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Pain Related To Perineal Suture NCPDocument3 pagesPain Related To Perineal Suture NCPDharylle CariñoNo ratings yet
- New Drug Application HardDocument37 pagesNew Drug Application HardGANESH KUMAR JELLA100% (1)
- B36 Group 6 Community Engagement ProposalDocument5 pagesB36 Group 6 Community Engagement ProposalLenard SusanoNo ratings yet
- Nurani Kaeda - Part 1Document5 pagesNurani Kaeda - Part 1farah_nishuNo ratings yet
- Module 1-Week 1-4 - Diet and HealthDocument31 pagesModule 1-Week 1-4 - Diet and HealthAsteria RafalloNo ratings yet
- KaileyDocument7 pagesKaileyapi-470964508No ratings yet
- Chlorhexidine's Effect on Fibroblast AttachmentDocument5 pagesChlorhexidine's Effect on Fibroblast AttachmentAna Maria Montoya GomezNo ratings yet
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Breaking the Habit of Being YourselfFrom EverandBreaking the Habit of Being YourselfRating: 4.5 out of 5 stars4.5/5 (1455)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- How to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipFrom EverandHow to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipRating: 4.5 out of 5 stars4.5/5 (1135)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- Deep Sleep Meditation: Fall Asleep Instantly with Powerful Guided Meditations, Hypnosis, and Affirmations. Overcome Anxiety, Depression, Insomnia, Stress, and Relax Your Mind!From EverandDeep Sleep Meditation: Fall Asleep Instantly with Powerful Guided Meditations, Hypnosis, and Affirmations. Overcome Anxiety, Depression, Insomnia, Stress, and Relax Your Mind!Rating: 4.5 out of 5 stars4.5/5 (10)
- Deep Sleep Hypnosis: Guided Meditation For Sleep & HealingFrom EverandDeep Sleep Hypnosis: Guided Meditation For Sleep & HealingRating: 4.5 out of 5 stars4.5/5 (103)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)