Professional Documents
Culture Documents
Edited To Include Report 1
Uploaded by
allanrnmanaloto0 ratings0% found this document useful (0 votes)
28 views16 pagesMAN
Original Title
Edited to Include Report 1
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentMAN
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
28 views16 pagesEdited To Include Report 1
Uploaded by
allanrnmanalotoMAN
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 16
1
NURSING CARE OF THE HIGH RISK
PRENATAL CLIENT
HIGH RISK
Is one in which a concurrent disorder, pregnancy related complication, or
external factor jeopardizes the health of the woman, the fetus or both.
Poverty
Lack of support people circumstances that
Poor coping mechanisms causes women to be
Genetic inheritance high- risk
Past history of pregnancy complications
Should be seen more frequently for prenatal care
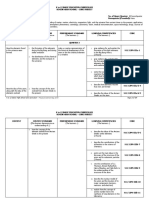
A. IDENTIFYING CLIENTS AT RISK
1. ASSESSMENT OF RISK FACTORS
Factors Effects
Demographic factors
1. Age (<16 or >35 years)
2. Poverty
3. Mulitiparity ( >4 pregnancies)
Less than 18: increased risk for LBW and
preterm labor, PIH, anemia,CS for CPD.
More than 35 years: increased risk of
chromosomal abnormalities, PIH
Associate with LBW, preterm infants
Hemorrhage, CS and fetal loss
Personal social factors/lifestyle
1. Weight
2. Height ( <5 feet)
3. Smoking
4. Alcohol/illegal drug use
<100 lbs: associated with LBW
>200 lbs: PIH, LGA infants, difficult labor, CS
due to CPD
Increased risk for CS due to CPD
LBW, preterm birth
Congenital anomalies, fetal withdrawal
syndrome, fetal alcohol syndrome
Obstetric factors
1. Birth of previous infant with weight
>8.5 lbs
Increased risk for CS, birth injury, maternal
gestational diabetes and neonatal
hypoglycemia
2
2. Previous stillbirth
3. Rh sensitization
4. Cervical insufficiency
5. Multiple gestations
Increased risk of maternal psychological
distress
Increased risk for fetal anemia,
eryhroblastosis and kernicterus
Associated with delivery of previable fetus
Associated with nutritional anemia,
preeclampsia, preterm labor, malpresentation,
CS, postpartum hemorrhage
Existing medical conditions
1. DM
2. Hypothyroidism
3. Cardiac disease
4. Renal disease
5. Concurrent infection
6. Seizure disorders
7. Liver disease
Increased risk of PIH. CS, LGA, SGA ,
neonatal hypoglycemia, fetal or neonatal
death, congenital anomalies
Increased risk of spontaneous abortion,
congenital anomalies, congenital
hypothyroidism
Increased risk of fetal or neonatal death
Watch out for signs of worsening heart disease
such as edema, crackles, activity intolerance,
SOB , irregular heart rate.
Associated with maternal renal failure,
preterm delivery, intrauterine growth
retardation
Severe fetal effects if maternal disease occurs
in the first trimester
Increased risk for spontaneous abortion and
congenital anomalies
Increased risk of fetal malformation, increased
incidence of cerebral palsy, seizure disorder
and mental retardation in offspring
Preterm and stillbirths
Environmental agents Impair fertility, interfere with normal placental
function and may be toxic to the fetus leading
to fetal death
B. FACTORS THAT CATEGORIZES A PREGNANCY AS HIGH RISK
Psychological Social Physical
Prepregnancy History of drug
dependence (
including alcohol)
History of
intimate partner
abuse
Occupation
involving handling
of toxic,
substances (
including
radiation and
anesthesia gases)
Visual or hearing
challenges
Pelvic inadequacy
or misshape
Uterine
incompetency,
3
Surat , NCM 102 lec
History of mental
illness
History of poor
coping
mechanisms
Cognitively
challenged
Survivor of
childhood sexual
abuse
Environmental
contaminants at
home
Isolated
Lower economic
level
Poor access to
transportation for
care
High altitude
Highly mobile
lifestyle
Poor housing
Lack of support
people
position or
structure
Secondary major
illness ( heart
disease, diabetes
mellitus, kidney
disease,
hypertension.
Chronic infection
such as
tuberculosis,
hemopoietic or
blood disorder,
malignancy)
Poor gynecologic
or obstetric
history
History of
previous poor
pregnancy
outcome (
miscarriage,
stillbirth,
intrauterine fetal
death)
History of child
with congenital
anomalies
Obesity ( BMI >30)
Underweight (
BMI <18.5)
Pelvic
inflammatory
disease
History of
inherited disorder
Small stature
Potential of blood
incompatibility
Younger than age
18 years or older
than 35 years
Cigarette smoker
Substance abuser
Pregnancy Loss of support
person
Illness of a family
member
Decrease in self
esteem
Drug abuse (
including alcohol
and cigarette
Refusal of or
neglected prenatal
care
Exposure to
environmental
teratogens
Disruptive family
incident
Conception less
Subject to trauma
Fluid or
electrolyte
imbalance
Intake of
teratogen such as
a drug
Multiple gestation
A bleeding
4
Surat , NCM 102 lec
smoking)
Poor acceptance
of pregnancy
than 1 year after
last pregnancy
disruption
Poor placental
formation or
position
Gestational
diabetes
Nutritional
deficiency of iron,
folic acid, or
protein
Poor weight gain
Pregnancy-
induced
hypertension
Infection
Amniotic fluid
abnormality
Postmaturity
Labor and birth Severely
frightened by
labor and birth
experience
Inability to
participate
because of
anesthesia
Separation of
infant at birth
Lack of separation
for labor
Birth of infant
who is
disappointing in
some way ( such
as sex,
appearance, or
congenital
anomalies)
Illness in newborn
Lack of support
person
Inadequate home
for infant care
Unplanned
cesarean birth
Lack of access to
continued health
care
Lack of access to
emergency
personnel or
equipment
Hemorrhage
Infection
Fluid and
electrolyte
imbalance
C. MEDICAL CONDITIONS AFFECTING PREGNANCY OUTCOMES ( PRE-
GESTATIONAL CONDITIONS)
1. Assessment of a woman with CARDIAC DISEASE:
Thorough health history---to document her prepregnancy cardiac status
Ask her level of exercise performance
5
Surat , NCM 102 lec
Ask if she has cough or edema
Instruct the woman to report coughing during pregnancy---bec pulmonary
edema from heart failure may first manifest itself as a simple cough.
Normal edema of pregnancy involves only the feet and ankles
Edema of pregnancy induced hypertension usually begins after week 20.
Sign of heart failure:
o Edema
o Irregular pulse
o Rapid or difficult respirations
o Chest pain on exertion
Making comparison assessment for nail bed ( should be <5 seconds)
Jugular venous distention
Assess liver size ( heart dss involves right sided heart failure)- difficult to
assess, since the uterus presses the liver upward under the ribs and difficult to
palpate.
Echocardiography
Chest radiograph----- abdomen is covered with lead apron during exposure
ECG------ less accurate because ty
tHe enlarge uterus presses upward on the diaphragm and displaces the heart
Four categories of heart disease:
1. Class 1 and II can expect to experience a normal pregnancy and birth.
2. Class III can complete a pregnancy by maintaining almost complete bed
rest.
3. Class IV are poor candidates for pregnancy because they are in cardiac
failure even at rest and when they are not pregnant.
- Advised to avoid pregnancy.
HEPARIN drug of choice for early pregnancy . Anticoagulant
- No teratogenic effect
- Does not cross the placenta and the fetus
SODIUM WARFARIN (COUMADIN) can be used after week 12 but a woman will returned to
heparin therapy during the last month of pregnancy======for the fetus not to develop a
coagulation disorder at birth.
Fetal assessment
Cardiac failure affect fetal growth
o Maternal blood pressure becomes insufficient to provide an adequate supply of
blood and nutrients to the placenta.
o Low birth weight
o acidotic fetal environment
o Preterm labor
o Immaturity
o Infant may not respond to labor ( late decelerations)
6
Surat , NCM 102 lec
Note: When cardiac output is not enough to meet systemic body demands---peripheral
vasoconstriction occurs because the uterus is a peripheral organ that causes the
uterine/placental constriction.
Interventions:
1. Promote healthy nutrition
Must gain weight but not so much weight ( burden to her heart)
2. Take iron supplements to prevent anemia
3. Educate regarding medication
Digoxin= administered to a woman during pregnancy to slow the Fetal heart if fetal
tachycardia is present
Adenosine beta blockers and angiotensin convertine enzyme ( ACE) inhibitors
= to reduce hypertension, safe during pregnancy
Nitroglycerin= a compound often prescribed for angina, safe
A valid exception to the rule No medicine during pregnancy
4. Educate regarding the avoidance of infection
Caution a woman with heart disease to avoid visiting or being visited by people
with infection
Interventions during labor and birth
1. Monitpr FHR and uterine comntractions in all women with heart dss
2. Assess BP, pulse and RR frequently
A rapid increasing PR ( >100 beats/min) is an indication that a heart is pumping
ineffectively and has increased its rate in an effort to compensate.
Advise the woman to assume a side lying position to reduce the possibility of
supine hypertension syndrome
If she has pulmonary edema= have her chest and head elevated ( semi-fowlers ) to
ease the work of breathing.
Fatigue is a symptom of heart decompression
3. Oxygen administration
4. Swan ganz catheter- to monitor the heart function
5. Epidural anesthesia
If epidural anesthesia is used, low forcep or vacuum extractor can be used for birth
6. Should not push with contractions
Interventions during postpartum
1. Decreased activity
2. Anticoagulant and digoxin therapy
3. Antiembolic stockings and ambulation may be needed to increase venous return from
the legs
4. If prophylactic antibiotics had not been started prior to birth, they will be started
immediately after birth to discourage subacute bacterial endocarditis
5. Close inspection of the baby
Acrocyanosis normal in newborn
6. Oxytocin (pitocin) for uterine involution, used with caution=tend to increase BP
7
Surat , NCM 102 lec
7. Kegel exercise for perineal strengthening but NOT postpartum exercises to improve
abdominal tone.wait for the dr or midvives order.
8. Stool softener
As a rule, woman with heart disease can brestfeed without difficulty
RHEUMATIC ENDOCARDITIS/RHEUMATIC HEART DISEASE
Is an acue, recurrent inflammatory disease that causes damage to the heart as a
sequel to group.
A beta hemolytic streptococcal infection, particularly the valves, resulting in valve
leakage ( insufficiency) and or obstruction ( narrowing or stenosis).
There are associated compensatory changes in the size of the hearts chambers and
the thickness of chamber walls.
Pathophysiology and etiology
Rheumatic fever is a sequel to group A streptococcal infection that occur in
about 3% of untreated infections. It is a preventable disease through the
detection and adequate treatment of streptococcal pharyngitis.
Connective tissue of the heart, blood vessels, joints and subcutaneous tissues
can be affected.
Lesions in connective tissue are known as aschoff bodies which are localized
areas of tissue necrosis is surrounded by immune cells.
Heart valves are affected, resulting in valve leakage and narrowing
Compensatory changes in the chamber sizes and thickness of chamber walls
occur.
Heart involvement ( carditis) also includes pericarditis, myocarditis and
endocarditis.
Myocarditis inflammatory process involving the myocardium
Pericarditis inflammation of the pericardium, the membranous sac enveloping
the heart
Clinical manifestations
1. Symptoms of streptococcal pharyngitis may precede rheumatic symptoms
a. Sudden onset of sore throat, throat reddened with exudate
b. Swollen, tender lymph nodes at angle of jaw
c. Headache and fever 101 -104 F ( 38.9 -40C)
d. Abdominal pain ( children)
e. Some cases of streptococcal throat infection are relatively asymptomatic
2. Warm and swollen joints ( polyarthritis)
3. Chorea ( irregular jerky, involuntary, unpredictable muscular movements)
4. Erythema marginatum (transient meshlike mascular rash on trunk an dextremities in
about 10% of patients)
5. Subcutaneous nodules ( hard, painless nodules over extensor surfaces of extremities )
6. Fever
8
Surat , NCM 102 lec
7. Prolonged PR interval demonstrated by ECG
8. Heart murmurs, pleural and pericardial rubs
Diagnostic evaluation
1. Throat culture to determine presence of streptococcal organisms
2. Sedimentation rate, WBC count and differential, and CRP increased during acute
phase of infection
3. Elevated antistreptolysin O ( ASO) titer
4. ECG prolonged PR interval or heart block
Management
1. Antimicrobial therapy- penicillin is the drug of choice
a. Note that missed doses of antibiotics due to the patients unavailability while off of
the unit for diagnostic tests are given after return to the unit.
b. Missed antibiotic doses may have irreversible deleterious consequences.
c. Notify heath acre provider if doses will be missed to make sure that appropriate
alternative measure are taken.
2. Rest to maintain optimal cardiac function
3. Salicylates or NSAIDS to control fever and pain
4. Prevention of recurrent episodes through long term penicillin therapy for 5 years after
initial attack in most adults, periodic prophylaxis throughout life if valvular damage.
Complications
1. Valvular heart disease
2. Cardiomyopathy
3. Heart failure
Nursing Assessment
1. Ask patient about symptoms of fever or throat or joint pain.
2. Ask patient about chest pain, dyspnea, fatigue
3. Observe for skin lesions or rash on trunk and extremities.
4. Palpate for firm, nontender movable nodules near tendons or joints.
5. Auscultate heart sounds for murmurs and rubs
Nursing Diagnosis
1. Hyperthermia related to disease process.
2. Decreased cardiac output relate to decreases cardiac contractility
3. Activity intolerance related to joint pain and easy fatigability.
Nursing Interventions
Reducing Fever
1. Administer penicillin therapy as prescribed to eradicate hemolytic streptococcus ; an
alternative drug may be prescribed if patients is allergic to penicillin or sensitivity
testing and desensitization may be done.
2. Give salicylates/NSAIDS as prescribes to suppress rheumatic activity by controlling
toxic manifestations. To reduce fever and to relieve joint pain.
3. Assess for effectiveness of drug therapy
a. Take and record temperature every 3 hours.
b. Evaluate patients comfort level every 3 hours.
9
Surat , NCM 102 lec
Maintaining adequate cardiac output
1. Assess for signs and symptoms of acute rheumatic carditis.
a. Be alert to patients complaint of chest pain, palpitations, and or precordial
tightness
b. Monitor for tachycardia ( usually persistent when patient sleeps) or bradycardia.
c. Be alert to development of second degree heart block or wenckebachs disease (
acute rheumatic carditis causes PR interval prolongation).
2. Auscultate heart sounds every 4 hours.
a. Document presence of murmur or pericardial friction rub.
b. Document extra heart sounds ( S3 gallop, S4 gallop).
3. Monitor for development of chronic rheumatic endocarditis, which may include valvular
disease and heart failure.
Maintaining Activity
1. Maintain bed rest for duration of fever or if signs of active carditis are present.
2. Provide ROM exercise program.
3. Provide diversuonal activities that prevents exertion.
4. Discuss needs for tutorial services with parents to help child keep up with school work.
Patient education and health maintenance
1. Counsel patient to maintain good nutrition.
2. Counsel patient on hygienic practices.
a. Discuss proper hand washing, disposal of tissues, laundering of handkerchiefs (
decrease risk of exposure to microbes)
b. Discuss the importance of using patients own toothbrush, soap and washcloths
when living in group situations.
3. Counsel patient on importance of receiving adequate rest.
4. Instruct patient to seek treatment immediately should sore throat occur.
5. Support patients in long-term antibiotic therapy to prevent relapse ( 5 years for most
adults)
6. Instruct patient with valvular disease to use prophylactic penicillin therapy before
certain procedures and surgery.
7. Explore with patient his ability to pay for medical treatment. If appropriate, contact
social services for patient.
2. DIABETES MELLITUS
Is an endocrine d/o in which the pancreas cannot produce adequate insulin to
regulate body glucose levels.
NOT a good candidate for oral contraceptive
because progesterone interferes with insulin activity and therefore increases
blood glucose levels
estrogen has the potential increasing lipid and cholesterol levels and blood
coagulation
NOT a candidate for using IUD
Associated with higher rates of Pelvic inflammatory disease
Have problems fighting infections
Subcutaneous implanted or IM injections of progestin may be good choice
10
Surat , NCM 102 lec
Clinical Presentation
Polyuria
Polydypsia
Polyphagia
Weight loss
Frequent UTI
Large fetus
3 Classification of Diabetes Mellitus
Type Description
Type 1 Formerly known as insulin dependent
diabetes mellitus
A state characterized by the destruction
of the beta cells in the pancreas that
usually leads to absolute insulin
deficiency.
A. immune mediated diabetes mellitus
resulys from autoimmune destruction
of the beta cells.
B. Idiopathic type I refers to forms that
has no cause
Type 2 Formerly known as non-insulin
dependent diabetes mellitus.
A state that usually arises because of
insulin resistance combined with a
relative deficiency in the production of
insulin
Gestational diabetes
Risk factors:
Obesity
Age over 25 years
Hx of large babies (10 lb or more)
Hx of unexplained fetal or perinatal
loss
Hx of congenital anomalies in
previous pregnancies
Hx of polycystic ovary syndrome
Family hx of diabetes ( one close
relative or two distant ones)
Member of a population with a high
risk for diabetes
A condition of abnormal glucose
metabolism that arises during
pregnancy. ( 24
th
-28
th
weeks)
Impaired glucose homeostasis A state between normal and
diabetes in which the body is no
longer using and or secreting insulin
properly.
A. impaired fasting glucose- a state
when fasting plasma glucose is at least
110 but under 126mg/dl
B. impaired glucose tolerance- a state
11
Surat , NCM 102 lec
when the results of the oral glucose
tolerance test are at least 140 but
under 200 mg/dl in the 2 hour sample.
Complications
Maternal Fetal
PIH Macrosomia
Infection ( cardiasis) Congenital anomalies
Polyhydramnios ( higher urine production
caused by hyperglycemia
Stillbirths
Spontaneous abortion
TEST
1. 50 g oral glucose challenge test
To confirm diabetes = fasting plasma glucose of 126 mg/dl or above or a
nonfasting plasma glucose of 200 mg/dl or above = with diabetes
After the oral 50 g glucose load- a venous sample is taken for glucose
determination 60 minutes later.
Done during the first prenatal visit and repeat at 24-28 weeks AOG
2. If negative: use 100g Glucose Tolerance test at 32-34 weeks
If the serum glucose level at 1 hour is more than 140 mg/dl, the woman is
scheduled for a 100 g , 3 hour fasting glucose tolerance test.
If 2 of the 4 blood samples collected for this test are abnormal or the fasting
value is above 95 mg/dl diabetes is present
Oral glucose challenge test values (fasting plasma glucose values) for pregnancy
Test type Pregnant glucose level
(mg/dl) by carpenter
and coustan
Fasting 95
1 hour 180
2 hours 155
3 hours 140
Following a 100 g glucose load. Rate is abnormal if two values are exc
Nursing care and management:
1. Complete patient database and document test results during pregnancy.
2. Educate both the patient and her family
Assess patients understanding of her condition and ite effects on daily life
Discuss and demonstrate self administration of insulin
Demonstrate self monitoring of blood glucose level before meals and at bedtime.
Stress the importance of recording
blood glucose levels
insulin dose
dietary intake
periods of exercise
periods of hypoglycemia
kind and amount of treatment
12
Surat , NCM 102 lec
urine test results daily
3. Explain importance of continued evaluation even during the postpartum period (
monitor glucose levels every 4-6 hours for 24 hours, administer insulin subcutaneously
when needed) and even when blood glucose levels are normal.
4. Arrange for patients consultation with a dietician
Diet: 20% CHON, 40-50% CHO, 30% fats
5. Encourage regular exercise ( 3-4x /week, duration of 15-30 minutes, HR maintains
between 130-160 bpm)
6. Attend to patients emotional and psychological needs and provide assurance.
7. Ensure patients preparation for intensive and regular intrapartun assessment:
Fetal monitoring
Intravenous glucose
Insulin and oxytocin infusion
Evaluation for diabetic hetoacidosis
IVF replacement
Invasive maternal cardiac monitoring
8. Identify and refer the patient and her family to possible support groups and resources
9. Advise contraception in diabetic women
10. Monitor BP and lipid levels
11. Woman who is type 1 0r 2 should meet with her obstetrician before she becomes
pregnant.
12. Use home test kit to determine if she is pregnant to know it at earliest time.
13. Glycosylated hemoglobin is used to detect the degree of hyperglycemia
Glucose circulates in the blood, binds to a portion of hemoglobin in the blood.
Measuring glycosylated hemoglobin is advantageous because it reflects the
average blood glucose levels over the past 4-6 weeks ( the time the RBC were
picking up glucose)
14. Ophthalmic examination is done during pregnancy
15. Urine culture may be done each trimester to detect asymptomatic UTI as the increased
glucose concentration in urine leads to increased infection.
Therapeutic management
1. Insulin
Regular = short acting insulin ( Lispro or insulin aspart)
2/3 given in the morning
1/3- evening
Self administered 30 minutes before breakfast in aratio 2:1 ( intermediate to
regular)
Again before dinner: ratio 1:1
Human insulin is recommended bec it has lesser antibody response than beef or
pork insulins.
2. Blood glucose monitoring
To determine if hypoglycemia or hyperglycemia exists
Signs and symptoms of hypoglycemis and hyperglycemia
Hypoglycemia= common in the 2
nd
and 3
rd
months
Hyperglycemia= common in the 6
th
months
Sweating
Pallor, cold, clammy skin
Disorientation, irritability
headache
Fatigue
Flushed, hot skin
Dry mouth, excessive thirst
Frequent urination
13
Surat , NCM 102 lec
hunger
blurred vision
nervousness
weakness, fatigue
shallow breathing, but normal PR
urine negative for glucose and ketones
blood glucose level <60 mg/dl
Rapid, deep breathing, fruity breath
odor
Depressed reflexes
Drowsiness, headache
3. ANEMIA
Normally: blood volume expands during pregnancy ( pseudo anemia)
True anemia
1
st
and 3
rd
trimester: hemoglobin concentration is less than 11g/dl (
hematocrit <33%)
2
nd
trimester: hemoglobin is less than 10.5g/dl (hematocrit <32%)
a. Iron deficiency anemia
A microcytic ( small red blood cell), hypochromic ( less hemoglobin than the
average red cell) anemia because when an inadequate supply of iron is
ingested, iron is unavailable for incorporation into red blood cells.
Most common anemia of pregnancy
Hemoglobin level is below 12 mg/dl
Hematocrit <33%
Low serum iron level confirms iron deficiency anemia
Increased iron binding capacity
Causes:
o Diet low in iron
o Heavy menstrual flow
o Unwise weight reduction programs
o Pregnant less than 2 years
o Low socio economic levels
Made available to the body by absorption from the duodenum
into the bloodstream after it is ingested.
In the blood stream------transferrin----for transport to the
liver, spleen and bone marrow------------and incorporated into
hemoglobin or stored as ferritin.
Effects:
o LBW
o Preterm birth
o Pica ( food craving) like ice or starch
Management:
1. Women should take prenatal vitamins
Iron supplement of 60 mg
2. Diet high in iron and vitamins * green leafy vegetables, meat, legumes , fruit)
3. Therapeutic levels of medications * 120-200 mg elements iron/day)in the form of
Ferrous sulfate or ferrous gluconate
Iron is best absorbed from an acid medium
Side effects:
o Constipation
14
Surat , NCM 102 lec
o Gastric irritation
Mgt: increase roughage diet
Always take the pills with food
If iron deficiency anemia is severe and a woman has difficulty with oral iron therapy, IM or
IV iron dextran can be prescribed.
b. Folic acid deficiency anemia
Folic acid/ folacin- B vitamins= necessary for the normal formation of red
blood cells in the mother.
Associated with preventing neural tube defects in the fetus.
High- risk:
Occurs most in multiple pregnancies bec of increased fetal demand
Women with secondary hemolytic illness---there is rapid destruction
and production of new red blood cells
Women taking hydantoin an anticonvulsant agent that interferes
with folate absorption
Women taking oral contraceptives
Women who had gastric bypass for morbid obesity
Megaloblastic anemia enlarged red blood cells
Anemia common in this type
The mean corpuscular volume will ne elevated in contrast to the
lowered level seen with iron deficeiency
Take several weeks to develop
Apparent during 2
nd
trimester
A contributory factor in early miscarriage or premature separation of
the placenta.
Occur in the 1
st
few weeks of fetal development
Advised the woman to begin 400 microgram folic acid daily
Eat folacin food (green leafy vegetables, oranges, dried beans.
During pregnancy
Folic acid requirement increases to 600 microgram daily
c. Sickle cell anemia
An inherited hemolytic anemia caused by abnormal aminmo acid in the beta
chain of hemoglobin.
If an abnormal amino acid replaces the amino acid valine, sickle hemoglobin
(HbS) results
If it is substituted for the amino acid lysine, nonsickling hemoglobin ( HbC)
results.
An individual is heterozygous ( has only one gene in which the abnormal
substitution has occurred) has the sickle cell trait ( HbAS)
If the person in homozygous ( has 2 genes in which the substitution has
occurred) sickle cell disease results. ( HbSS)
Majority of the red blood cells are irregular or sickle shaped------cannot carry
as much hemoglobin as a normally shaped red cells do.
oxygen
bld becomes viscid ( dehydrated) cells clump
hemolysis blood flow to organs vessel blockage
decrease # of RBC severe anemia
15
Surat , NCM 102 lec
Effects of homozygous disease:
1. Prematurity
2. Miscarriage
3. Perinatal mortality
4. Increased incidence of asymptomatic bacteriuria resulting in increase incidence of
pyelonephritis.
Sickle cell anemia is a threat to life if vital blood vessels such as those to the liver, kidneys,
heart, lungs or brain become blocked.
In pregnancy, blockage to the placental circulation can directly compromise the fetus,
causing low birth weight and possibly fetal death.
Assessment:
1. Monitor hemoglobin level
2. Clean catch urine sample
Since they are susceptible to bacteriuria
3. Monitor diet throughout pregnancy
4. Fluid intake carefully monitored
Should consume at least 8 glasses of fluids daily
If nauseated ----decrease fluid intake, dehydration then sickle cell crisis occurs.
5. Assess for presence of varicosities during prenatal visits
Due to uterine pressure during pregnancy/pooling of blood in leg veins
Pooling and pressure can lead to red blood cell destruction
Standing for long time causes this pressure
6. Encourage woman to elevate legs while sitting
7. Sims position to encourage venous return from the lower extremities
8. Monitor fetal health by
a. UTZ at 16-24 weeks to assess for intrauterine growth restriction
b. NST by weekly beginning at 30 weeks
c. Blood flow velocity to measure blood flow to the uterus and placenta
If reduced ------ intrauterine growth restriction
Therapeutic Management:
1. Periodic exchange transfusion throughout pregnancy----to replace sickled cells with non
sickled cells
2. O2 administration
3. Increase fluid volume
Hypotonic (0.45 saline)---to keep plasma tension low because of the
difficulty of a woman concentrating urine to remove large amounts of
fluids.
As a rule women with sickle cell anemia are not given iron supplement during
pregnancy
Sickle cells cannot incorporate with iron same manner as non sickled cell
cell can, so excessive iron buildup may result
4. Hospitalization
If with fever to rule out the development of sickle cell crisis
With infection and hemolysis
16
Surat , NCM 102 lec
If a woman has the disease and her partner has the trait----50% child born with the
dss, and all of their child will have the disease.
Symptoms of sickle cell disease do not become apparent until an infants fetal
hemoglobin converts to a largely adult pattern ( in 3 -6 months).
Fetal hgb= 2 alpha 2 gamma chains
Adult hgb = 2 alpha 2 beta chains
Bec sickle cell trait is carried on the beta chain, symptoms will be manifested until this
chain appears.
5. Electrophoresis of RBC---obtained thru percutaneous umbilical blood
sampling/amniocentesis----can reveal the presence of the disease.
NB have 15% adult hgb at birth-----so electrophoresis at birth can reveal if the
dss is present.
6. HIV
Risk factors:
Multiple sexual partners of the individual or sexual partner
Bisexual partners
Intravenous drug used by the individuals or sexual partner
Assessment:
a. Reproductive tract irritation
b. Mild flu symptoms
c. Seroconversion- in which a woman converts from having no HIV antibodies in her blood
serum ( HIV serum negative) to having antibodies against HIV ) HIV serum positive
Happens 6 weeks to 1 year after exposure
d. Weight loss
e. fatigue
higher risk of developing toxoplasmosis and cytomegalovirus infections
HIV positive woman may invade the cerebrospinal fluid and cause extreme
neurologic involvement.
f. Tuberculis
ELISA or Western blot analysis
Zidovudine ( ZVD)- administerd to the woman beginning with the 14
th
week of pregnancy
And newborns receives antiviral therapy beginning with birth. And a follow- up of 6weeks .
Therapeutic Mgt:
1. Advised not to be pregnant
2. Trimethoprin with sulfamethoxazole (bactrim)- with pneumonia
Teratogenic in early pregnancy
Sulfamethoxazole ( gantanol)- may lead to increase bilirubin levels in newborn if
administered late in pregnancy
3. Chemotheraphy for those with Kaposis sarcoma- contraindicated during early
pregnancy bec of potential for fetal injury but can be used later in pregnancy to halt the
malignant growth.
4. Cs delivery
Effects:
Low birth weight
Preterm birth
You might also like
- Introduction To High Risk PregnancyDocument13 pagesIntroduction To High Risk PregnancyMabes100% (1)
- High-Risk Pregnancy Factors & CareDocument19 pagesHigh-Risk Pregnancy Factors & CareRoger Jr PumarenNo ratings yet
- Prematurity to Postmaturity: Nursing Care for Preterm and Post-Term NewbornsDocument38 pagesPrematurity to Postmaturity: Nursing Care for Preterm and Post-Term NewbornsJessy Arcaina BañagaNo ratings yet
- High-Risk Pregnancy: The Internet Journal of Gynecology and ObstetricsDocument16 pagesHigh-Risk Pregnancy: The Internet Journal of Gynecology and ObstetricsWidelmark FarrelNo ratings yet
- Heart Disease To STDDocument7 pagesHeart Disease To STDCURT JAZTYN PASCUALNo ratings yet
- HRPGDDocument16 pagesHRPGDyuastikapsNo ratings yet
- The Internet Journal of Gynecology and ObstetricsDocument8 pagesThe Internet Journal of Gynecology and Obstetricsrett_ttaNo ratings yet
- Gestational Hypertension: Maternal Health Care-ClinicalDocument10 pagesGestational Hypertension: Maternal Health Care-ClinicalIbrahim W. HassanNo ratings yet
- Hand Out For Pregnant Client NCM 109Document8 pagesHand Out For Pregnant Client NCM 109Allaine Royce LibrandoNo ratings yet
- Abc Ob 2010Document351 pagesAbc Ob 2010anjilozanoNo ratings yet
- Nursing Care of The High Risk Pregnancy ClientDocument7 pagesNursing Care of The High Risk Pregnancy ClientJoash Karlo De GuzmanNo ratings yet
- Case Study CP 104Document22 pagesCase Study CP 104Mor Shi DA BalutintikNo ratings yet
- 1 Maternal High Risk Intro Pregestational ConditionsDocument90 pages1 Maternal High Risk Intro Pregestational ConditionsKaren Joy Jacinto Ello100% (2)
- 109 Pregestational Nov2019Document68 pages109 Pregestational Nov2019Sean kevinNo ratings yet
- High Risk Pregnancy NewDocument16 pagesHigh Risk Pregnancy NewSurya SasidharanNo ratings yet
- NCM 109 Care of at RiskDocument38 pagesNCM 109 Care of at RiskMia Fe Cuaya LorenzoNo ratings yet
- S1 5 OB Lec Nursing Care of The Pregnant Client Pre Gestational ConditionDocument132 pagesS1 5 OB Lec Nursing Care of The Pregnant Client Pre Gestational ConditionJustine Ingrid O. FernandezNo ratings yet
- Health Education For Record BookDocument24 pagesHealth Education For Record BookRoselineTiggaNo ratings yet
- Cardiovascular Disorders in PregnancyDocument55 pagesCardiovascular Disorders in PregnancyRyrey Abraham PacamanaNo ratings yet
- Assesment of Women in LabourDocument103 pagesAssesment of Women in Labourmikegrace02No ratings yet
- Identifying Risk Factors in PregnancyDocument3 pagesIdentifying Risk Factors in PregnancyKenneth NovenoNo ratings yet
- High Risk NewbornDocument127 pagesHigh Risk NewbornLeigh Angelika Dela CruzNo ratings yet
- High Blood Pressure: Gestational DiabetesDocument2 pagesHigh Blood Pressure: Gestational DiabetesKarlo ReyesNo ratings yet
- High Risk Preg 2020Document23 pagesHigh Risk Preg 2020ghyramirezNo ratings yet
- Fetal Issues: Table 25.16Document3 pagesFetal Issues: Table 25.16CristinaNo ratings yet
- Pregnancy Induced Hypertension (Pih) Nursing Management: EfinitionDocument3 pagesPregnancy Induced Hypertension (Pih) Nursing Management: Efinitiongebremeskel tikueNo ratings yet
- Maternal Risk Factors and Fetal AssessmentDocument88 pagesMaternal Risk Factors and Fetal AssessmentLeofe CorregidorNo ratings yet
- Risk factors for high-risk pregnanciesDocument3 pagesRisk factors for high-risk pregnanciesWindySeptianiIshakNo ratings yet
- Complications of Pregnancy Are The Symptoms and Problems That AreDocument6 pagesComplications of Pregnancy Are The Symptoms and Problems That Arekikai18No ratings yet
- Case Pres Except PATHO at PADocument99 pagesCase Pres Except PATHO at PAHanwell Keith SantosNo ratings yet
- Preeclampsia and High Blood Pressure During Pregnancy-ACOGDocument6 pagesPreeclampsia and High Blood Pressure During Pregnancy-ACOGrenaNo ratings yet
- Perinatal Medicine GuideDocument7 pagesPerinatal Medicine GuideMerna MahrousNo ratings yet
- High Risk PregnancyDocument14 pagesHigh Risk Pregnancymarlynperez867173No ratings yet
- StillbirthDocument4 pagesStillbirthTubagus Siswadi WijaksanaNo ratings yet
- Factors That Can Lead to a High-Risk PregnancyDocument6 pagesFactors That Can Lead to a High-Risk PregnancyRajalakshmiNo ratings yet
- Nursing Care for High-Risk Pregnancies Due to Pre-Existing ConditionsDocument31 pagesNursing Care for High-Risk Pregnancies Due to Pre-Existing Conditionsallanrnmanaloto100% (2)
- Assessment of High-Risk PregnancyDocument23 pagesAssessment of High-Risk PregnancyNiña Ricci MtflcoNo ratings yet
- Importance of Prenatal CareDocument12 pagesImportance of Prenatal CarePinkymekala HasanparthyNo ratings yet
- Pregnancy Induced HypertensionDocument4 pagesPregnancy Induced HypertensionMjhay SalvadorNo ratings yet
- Term PaperDocument85 pagesTerm PaperAbhilash PaulNo ratings yet
- High - Risk PregnancyDocument110 pagesHigh - Risk PregnancyAndre DityaNo ratings yet
- NCM - Pregancy Induced HypertensionDocument5 pagesNCM - Pregancy Induced HypertensionZam PamateNo ratings yet
- Pediatric Paper RevisiDocument31 pagesPediatric Paper RevisiEksa BintariNo ratings yet
- Nursing Care OF A Family Experiencing A Pregnancy From A Preexisting OR Newly Acquired IllnessDocument55 pagesNursing Care OF A Family Experiencing A Pregnancy From A Preexisting OR Newly Acquired IllnessJohn Van Dave TaturoNo ratings yet
- C Are The Symptoms and Problems That Are Associated With: J J J JDocument8 pagesC Are The Symptoms and Problems That Are Associated With: J J J JCelestine De CastroNo ratings yet
- Elderly PrimiDocument7 pagesElderly PrimiAnnapurna Dangeti67% (3)
- PIHDocument4 pagesPIHAngelica Floreza DullasNo ratings yet
- Intro To High Risk PregnancyDocument10 pagesIntro To High Risk PregnancyKenneth Jake Quinagon TayabanNo ratings yet
- Pre EclampsiaDocument6 pagesPre EclampsiaDannyca Kyle BahallaNo ratings yet
- High Risk Prenatal ClientDocument81 pagesHigh Risk Prenatal ClientestimojervsNo ratings yet
- Cardiac, DM, Substance Abuse LECDocument65 pagesCardiac, DM, Substance Abuse LECFarmisa MannanNo ratings yet
- Alh 2220 Preeclampsia Research PaperDocument9 pagesAlh 2220 Preeclampsia Research Paperapi-431367905No ratings yet
- Disorders of Maturation MD 3Document34 pagesDisorders of Maturation MD 3wizborrlyzo006No ratings yet
- High Risk Pregnancy HB TranxDocument11 pagesHigh Risk Pregnancy HB TranxangeliquepastranaNo ratings yet
- Medical and Surgical Complicating PregnancyDocument70 pagesMedical and Surgical Complicating PregnancyGunaNo ratings yet
- Preeclampsia Case StudyDocument9 pagesPreeclampsia Case StudyVanet100% (2)
- High Risk Infant-1Document5 pagesHigh Risk Infant-1MauZungNo ratings yet
- Portfolio On M104 Clinical Management and High Risk PregnanciesDocument31 pagesPortfolio On M104 Clinical Management and High Risk PregnanciesKIMBERLY JANE OTAGAN DALAGANNo ratings yet
- Pre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Are You Fertile?: Guides on Healthy Lifestyles that Increases Fertility Chances in Men and WomenFrom EverandAre You Fertile?: Guides on Healthy Lifestyles that Increases Fertility Chances in Men and WomenNo ratings yet
- Learning Continuity Plan SY 2020 - 2021Document5 pagesLearning Continuity Plan SY 2020 - 2021allanrnmanalotoNo ratings yet
- DRR1112 IIc D 32Document5 pagesDRR1112 IIc D 32allanrnmanalotoNo ratings yet
- DRR11/12-Ic-8. Explain The Meaning of VulnerabilityDocument6 pagesDRR11/12-Ic-8. Explain The Meaning of VulnerabilityallanrnmanalotoNo ratings yet
- Department of Education Region III: I. ObjectivesDocument3 pagesDepartment of Education Region III: I. ObjectivesallanrnmanalotoNo ratings yet
- Science Learner Module-130708064905-Php Appilcation01 :)Document350 pagesScience Learner Module-130708064905-Php Appilcation01 :)William Bryle Pertos75% (4)
- DRR11 12 Ia B 6Document3 pagesDRR11 12 Ia B 6allanrnmanalotoNo ratings yet
- 1 - Page Modified Daily Lesson Log For Senior High SchoolDocument4 pages1 - Page Modified Daily Lesson Log For Senior High Schoolallanrnmanaloto100% (1)
- DRR11 12 Ic D 34Document3 pagesDRR11 12 Ic D 34allanrnmanalotoNo ratings yet
- How Does An Event Become A Disaster? 2. When Does An Event Become A Disaster?Document3 pagesHow Does An Event Become A Disaster? 2. When Does An Event Become A Disaster?allanrnmanalotoNo ratings yet
- DRRRM LC 9Document3 pagesDRRRM LC 9allanrnmanalotoNo ratings yet
- DRRR 11 12 Ic 7Document3 pagesDRRR 11 12 Ic 7ben leeNo ratings yet
- DLP DRR LC 24Document3 pagesDLP DRR LC 24allanrnmanaloto100% (1)
- STEM - Gen Chem 1 and 2 CG PDFDocument18 pagesSTEM - Gen Chem 1 and 2 CG PDFChelie Trangia50% (2)
- Stem - Physics 2 CGDocument15 pagesStem - Physics 2 CGVictoria Mabini100% (7)
- NBNBNB, BHJHJGFJFKGDocument293 pagesNBNBNB, BHJHJGFJFKGYvi100% (2)
- Lesson Guide in Earth and Life Science I. ObjectivesDocument3 pagesLesson Guide in Earth and Life Science I. ObjectivesallanrnmanalotoNo ratings yet
- Science 8 Teachers GuideDocument230 pagesScience 8 Teachers GuideMichelle Gonzales Caliuag86% (141)
- SHS Core - Physical Science CG - 0Document17 pagesSHS Core - Physical Science CG - 0Loo DrBrad67% (3)
- S11ES IIc 28Document5 pagesS11ES IIc 28allanrnmanalotoNo ratings yet
- Learn Earth Science essentialsDocument6 pagesLearn Earth Science essentialsJake Arman PrincipeNo ratings yet
- STEM - Biology 2 CG - With Tagged Sci EquipmentDocument4 pagesSTEM - Biology 2 CG - With Tagged Sci EquipmentVictoria MabiniNo ratings yet
- Stem - Physics 1 CGDocument13 pagesStem - Physics 1 CGVictoria MabiniNo ratings yet
- STEM - Biology 1 CG - With Tagged Sci Equipment PDFDocument8 pagesSTEM - Biology 1 CG - With Tagged Sci Equipment PDFKOUJI N. MARQUEZNo ratings yet
- S11ES IIa 23Document5 pagesS11ES IIa 23allanrnmanalotoNo ratings yet
- Science G8 (LM Front)Document8 pagesScience G8 (LM Front)xdmhundz999No ratings yet
- S11ES II J 41Document4 pagesS11ES II J 41allanrnmanalotoNo ratings yet
- Lesson Guide in Earth and Life Science I. ObjectivesDocument5 pagesLesson Guide in Earth and Life Science I. ObjectivesallanrnmanalotoNo ratings yet
- S11ES IIi 40Document3 pagesS11ES IIi 40allanrnmanaloto50% (2)
- Lesson Guide in Earth and Life Science I. ObjectivesDocument2 pagesLesson Guide in Earth and Life Science I. ObjectivesallanrnmanalotoNo ratings yet
- S11ES IIh I 39Document2 pagesS11ES IIh I 39allanrnmanaloto50% (2)
- Controlling Rabies-One Humane SolutionDocument16 pagesControlling Rabies-One Humane SolutionTatiana Vieira de LimaNo ratings yet
- Lung Link: Improved Artificial Lung ConduitsDocument1 pageLung Link: Improved Artificial Lung ConduitsAwadhNo ratings yet
- Dentist-Patient Communication-A Maior Factor in Treatment PrognosisDocument3 pagesDentist-Patient Communication-A Maior Factor in Treatment Prognosis'Montserrat Orozco GutierrezNo ratings yet
- Drugs and Cosmetics ActDocument29 pagesDrugs and Cosmetics ActRanvidsNo ratings yet
- Differin (Adapalene) Gel, 0.1%: ® For The Treatment of AcneDocument143 pagesDifferin (Adapalene) Gel, 0.1%: ® For The Treatment of AcnePaulNo ratings yet
- Dermatology Questions and Clinchers PDFDocument10 pagesDermatology Questions and Clinchers PDFSahar nazNo ratings yet
- MCPS COVID-19 Simplified Decision Making ModelDocument2 pagesMCPS COVID-19 Simplified Decision Making ModelNBC MontanaNo ratings yet
- Perkembangan Epidemiologi2Document64 pagesPerkembangan Epidemiologi2Mangun AngkatNo ratings yet
- Management of Deep Caries 1st PartDocument45 pagesManagement of Deep Caries 1st PartLames Ali Sayed Ahmed AttiaNo ratings yet
- Management of Myelofibrosis: Alessandro M. VannucchiDocument9 pagesManagement of Myelofibrosis: Alessandro M. VannucchifrnksusNo ratings yet
- GMDSS Exam Schedule For Year 2023Document5 pagesGMDSS Exam Schedule For Year 2023Nilesh KumarNo ratings yet
- The US FDA and Probiotics Regulatory CategorizationDocument4 pagesThe US FDA and Probiotics Regulatory CategorizationBambangNo ratings yet
- Five Year PlanDocument104 pagesFive Year PlanJyoti EkkaNo ratings yet
- Choosing Blood Cultures Wisely - Choosing WiselyDocument4 pagesChoosing Blood Cultures Wisely - Choosing WiselyAlberto Mata VargasNo ratings yet
- Ecc0018 0202Document7 pagesEcc0018 0202Mari PetrelliNo ratings yet
- Gestational DiabetesDocument37 pagesGestational DiabetesSathish Kumar ANo ratings yet
- Jurnal Infeksi Saluran PencernaanDocument22 pagesJurnal Infeksi Saluran PencernaanDini Okta PutriNo ratings yet
- Essential NB Care Checklist 2020 3Document2 pagesEssential NB Care Checklist 2020 3karenbescaserNo ratings yet
- Clinical Case Presentation on Peptic Ulcer DiseaseDocument44 pagesClinical Case Presentation on Peptic Ulcer DiseaseRUSSELL CILOTNo ratings yet
- Monthlyshot December 1Document10 pagesMonthlyshot December 1api-308247685No ratings yet
- Written Assignment: Reflective WritingDocument9 pagesWritten Assignment: Reflective WritingNur Aziemah Mohd Zamri100% (1)
- Lab Medical International Vol.28.6-7Document68 pagesLab Medical International Vol.28.6-7Iguodala OwieNo ratings yet
- Learning Plan Medsurg Clinical RotationDocument7 pagesLearning Plan Medsurg Clinical Rotationapi-275795160100% (2)
- ENEMA ChecklistDocument2 pagesENEMA ChecklistJessoliver GalvezNo ratings yet
- Intern Journal reading-MRI-osteomyelitis-OOOE-2008Document6 pagesIntern Journal reading-MRI-osteomyelitis-OOOE-2008yuni madjidNo ratings yet
- The LATCH Scoring SystemDocument7 pagesThe LATCH Scoring SystemAndini PramonoNo ratings yet
- The Developing Occlusion ofDocument6 pagesThe Developing Occlusion ofAlistair KohNo ratings yet
- Severe Burns in Australian and New Zealand Adults: Epidemiology and Burn Centre CareDocument6 pagesSevere Burns in Australian and New Zealand Adults: Epidemiology and Burn Centre CareE.sundara BharathiNo ratings yet
- Understanding Clinical Trials - PDDocument7 pagesUnderstanding Clinical Trials - PDCristina SalcianuNo ratings yet
- Warning Signs of Various DiseasesDocument44 pagesWarning Signs of Various DiseasesamsabavanNo ratings yet