Professional Documents
Culture Documents
Antiarrhythmics
Uploaded by
Cherry DuldulaoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antiarrhythmics
Uploaded by
Cherry DuldulaoCopyright:
Available Formats
J.
ONACRUZ,MD,MHPED,FPOGS
PHYSIOLOGY OF CARDIAC
CONTRACTION
ARRHYTHMIAS
ANTI-ARRHTYMIC DRUGS:
CLASSES I IV
OTHER ANTI-ARRHYTHMICS
ADENOSINE
DIGOXIN
Action Potential in SA Nodal Cells
ACTION POTENTIAL OF VENTRICULAR MYOCYTES
OUTSIDE CELL INSIDE CELL
Na+ Na+ Na+
Na+ Na+
Na+ Na+ Na+
Na+ Na+ Na+
Cell Membrane
Cell Membrane
OUTSIDE CELL INSIDE CELL
Na+
K+ K+ K+ K+
Cell Membrane
OUTSIDE CELL INSIDE CELL
Ca++
Ca++
Ca++
K+ K+ K+ K+
Ca++
K+ K+ K+ K+
Cell Membrane
OUTSIDE CELL INSIDE CELL
Increasing depolarization results from
gradual increase in permeability to sodium
Resting membrane potential is
restablished
SA Node- native pacemaker
AV Node- latent pacemaker
Bundle of His-latent pacemaker
Purkinje-latent pacemaker
1.Rate of spontaneous depolarization in
phase 4
2.Threshold potential
3.Resting membrane potential
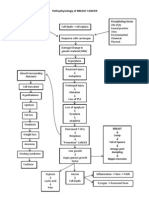
Impulse formation and/or
Impulse conduction
Altered automaticity (increased activity of
pacemakers)
Triggered Activity (EADs. DADs)
Physiologic
Pathologic
latent pacemakers takeover
escape, ectopic beats
direct tissue injury
Afterdepolarizations: occur when a normal
action potential triggers an EXTRA
depolarization
Simple block
Reentry or circus movement
Accessory Tracts
Bundle of Kent
1. Sodium channel blockade
2. Blockade of sympathetic autonomic
effects in the heart
3. Prolongation of effective refractory period
4. Calcium channel blockade
Ion channels can change into various
conformational states
Changes in membrane permeability to a
particular ion is mediated by
conformational changes in the channels
through which that ion passes
Antiarrhythmic agents often have
different affinities for different
conformational states of the ion
channel
Ectopic pacemakers
Depolarized tissues, ischemic tissues
Activated channels (phase 0) or
inactivated channels (phase 2)- use or
state dependent drug action
Reduction of phase 4 slope by blocking
sodium or calcium
Increase threshhold
Blockade of positive chronotropic action of
norepinephrine in the heart (beta blockers)
Slows conduction by:
1. steady state reduction of available
unblocked channels
2. prolongation of recovery time of
channels that are able to reach rested and
available state (increased refractory
period)
As dose of antiarrhythmics are increased,
they begin to suppress conduction in
normal polarized tissue of the heart
Therapeutic concentrations may also be
proarrhythmic in settings of fast heart
rates, acidosis, hyperkalemia, ischemia
SA NODAL EFFECTS:
decreases automaticity by increasing
threshold potential and decreasing slope
of phase 4 depolarization
Ventricular Myocyte effects:
decreases upstroke velocity (slope) of
phase 0, for some also prolongs
repolarization (increases ERP)
Generally decrease reentry and prevent
arrhythmia by:
1.decreasing conduction velocity
2.increasing the refractory period
Although all three subclasses have similar
effects on action potential in the SA node,
there are important differences in their
effects on ventricular action potential
Moderate sodium channel blockade
(Moderate reduction in slope of phase 0)
Prolongs repolarization in both SA node
and ventricles
Prolongs action potential duration
Increases Effective Refractory Period
duration
Weak sodium channel blockade (Small
reduction in phase 0 slope)
Shortens action potential duration in some
tissues of the heart
Decreases effective refractory period
Strong sodium blockade
Pronounced reduction in slope of phase 0
No effect on APD or ERP
Sodium Blockade
IC>IA>IB
ERP
IA-increase, IB-shortens, IC-no effect
Action Potential Duration (K+
repolarization current)
IA > IB IC-no effect
Slows phase 4 depolarization thereby
decreasing abnormal automaticity
Increases threshold for excitation in atrium
and ventricles- direct depressant actions
EXTRACARDIAC EFFECTS
ganglion blocking propertiesreduces
peripheral vascular resistance*
hypotension (esp.IV)
CARDIAC
excessive slowing of conduction
precipitation of new arrhythmias such
as torsades de pointes*
syncope
EXTRACARDIAC
lupus-like syndrome
nausea and diarrhea
rash
fever
hepatitis
agranulocytosis
WEAK ANTICHOLINERGIC EFFECTS
IV,IM, PO(good absorption)
NAPA metabolite- Class III activity*
Liver metabolism and renal excretion
Half life is 3-4 h (frequent dosaging)
Dose reduction in renal failure and heart
failure
Atrial and ventricular arrhythmias
Sustained ventricular arrhythmias with
acute MI (second choice)
CARDIAC EFFECTS
similar to procainamide
more cardiac antimuscarinic effects
than procainamide
Cardiac toxicities- excessive QT
interval prolongation, torsades de
pointes, excessive slowed conduction
EXTRACARDIAC EFFECTS
diarrhea, nausea, vomiting
cinchonism (headache, dizziness,
tinnitus)
thrombocytopenia
hepatitis
angioneurotic edema
fever
Rapid absorption after oral intake
Binds to albumin and alpha glycoprotein
Hepatic metabolism
Half life 6-8 hrs
Slow release formulations
Occasional: atrial flutter/fib
CARDIAC EFFECTS
similar to procainamide and quinidine
greater cardiac antimuscarinic effect than
quinidine*
CARDIAC TOXICITIES
similar to quinidine
precipitation of heart failure*
EXTRACARDIAC TOXICITIES
ATROPINE-LIKE EFFECTS-
urinary retention
dry mouth
blurred vision
constipation
glaucoma worsening
Oral
Reduced dose in renal failure
Ventricular arrhythmias
Low incidence of toxicity
Highly effective for arrhythmias in acute
MI
IV use only
CARDIAC EFFECTS
greater effects on purkinje and ventricular
cells than atrial
Selective depression of conduction in
depolarized and not in resting cells
CARDIAC
least cardiotoxic among class I
uncommon proarrhythmic effects
hypotension in large doses (heart failure
cases)*
EXTRACARDIAC
Neurologic*
paresthesia, tremor, nausea
lightheadedness, hearing disturbances
slurred speech, seizures
Extensive first pass hepatic metabolism*
Parenteral (infusion)
Half-life 1-2h (can be as short as 20 mins)
Higher concentration may be needed in
some cases of MI or other acute illness**
Doses are decreased in those with heart
failure, liver disease
Drug interaction:*
propranolol
cimetidine
(Renal disease has no effect)
DOC- tx for ventricular tachycardia and
prevention of ventricular fibrillation after
cardioversion in acute MI
Oral active congener of lidocaine
Adverse effects are dose-related and
frequently occur at therapeutic doses
(neurologic)*
Elimination half-life is 8-20 h*
Ventricular arrhythmias
Chronic pain conditions
Potent sodium and potassium blocker*
Does not prolong APD or QT interval
Well absorbed orally
Half-life- 20h
Hepatic metabolism, renal elimination
No antimuscarinic effects
TOXICITY:
severe arrhythmia exacerbation*
USE:
Supraventricular arrhythmias,PVCs
With weak beta blocking action
Structural similarity: propranolol
Spectrum of action: Quinidine
Liver metabolism
TOXICITY:
metallic taste
constipation
arrhythmia exacerbation
USE:
supraventricular arrhythmias
Potent sodium channel blocker
No APD prolongation
Many metabolites*
TOXICITY:
Dizziness
Nausea
Arrhythmia exacerbation
USE:
ventricular arrhythmias
Cardiac Effects: anti-arrhythmic
beta receptor blockade
direct membrane effects
Well tolerated but less effective than
sodium channel blockers*
Prevention of recurrent infarction and
sudden death in post-MI
Propranolol
Esmolol
Sotalol*
Drugs that prolong effective refractory
period via prolongation of action potential
Blocks K+ channel or enhance inward
currents of sodium
reverse-use dependence*
CARDIAC EFFECTS:
marked prolongation of the APD and QT
interval by blocking I
k
blocking effect occurs in all ranges of
heart rates*-the exception
broad range of actions- Class I-IV actions
CARDIAC EFFECTS
slows heart rate and AV node conduction
highly efficacious, low risk of torsades
even if QT is prolonged
EXTRACARDIAC EFFECTS
Peripheral vasodilatation*
USES
ventricular arrhythmias, tachycardia
supraventricular arrhythmias (atrial fib)
Accumulates in many tissues (heart, lung,
liver, skin, tears)
TOXICITY: CARDIAC
symptomatic bradycardia and heart block*
arrhythmia aggravation
TOXICITY:EXTRACARDIAC
dose-related pulmonary fibrosis
abnormal liver function tests and hepatitis
photodermatitis, gray blue discoloration of
exposed skin
asymptomatic corneal microdeposits
optic neuritis (rare)
anomalies in thyroid function*
KINETICS
bioavailability 35-65%
hepatic metab: desethylamiodarone*
elimination half-life
50% rapid component (3-10days)
50% slow (weeks)
*effects are maintained up to 3 months
after d/c
KINETICS
drug interaction
increase with cimetidine
decrease with rifampicin
increases levels of warfarin and digoxin
Direct antiarrhythmic effect and inhibitor of
neuronal catecholamine release
CARDIAC EFFECTS
lengthens ventricular* APD and ERP esp.
in ischemic tissues- reverses shortening
of APD due to ischemia
CARDIAC EFFECTS
initial positive inotropic effect*
EXTRACARDIAC EFFECTS
postural hypotension**
nausea and vomiting
KINETICS
available for IV use
USES (rare)
emergency- resuscitation from ventricular
fibrillation after failure of lidocaine and
cardioversion (amiodarone preferred)
Class 3 (APD prolongation) and Class 2
(beta blocker) actions
Racemic mixture:
*Beta blocking effect is in the l-isomer
APD prolongation in d- and l-isomers
KINETICS
100% bioavailability
excreted unchanged in the kidneys
half-life of 12 h
few direct drug interactions
CARDIAC TOXICITIES
torsades des pointes*
further depression of LV function**
USES
life threatening ventricular arrhythmias
maintaining sinus rhythm in atrial fib
supraventricular and ventricular
arrhythmias in pedia
Dose dependent blockade rapid
component of delayed rectifier potassium
current I
kr*
(esp. in hypokalemia)
Ability to block is independent on
stimulation frequency due to slow rate of
recovery from the blockade*
KINETICS
100% bioavailability
Drug interaction-
Verapamil*
Cimetidine**
80% excreted renally unchanged
20% excreted as inactive metabolites
dosage is based on creatinine clearance
Contraindication:
baseline QT interval of > 450ms,
intraventricular delay, bradycardia of <50
beats, hypokalemia
USE:
maintenance or restoration of normal
sinus rhythm in atrial fibrillation
Blockade of rapid component of delayed
rectifier potassium current and activation
of slow inward sodium current
KINETICS
rapid by hepatic metabolism
renal excretion
half-life 6 h
USES
acute conversion of atrial fibrillation and
flutter
CARDIAC TOXICITY
extreme prolongation of QT interval
torsades des pointes
Initially introduced for management of
angina pectoris
CARDIAC EFFECTS
blocks activated and inactivated L-type
calcium channels especially in rapidly
firing tissues, less completely polarized at
rest, those whose activation depends
more on calcium channels*
SA and AV NODES
CARDIAC EFFECTS
suppression of EAD and DAD
EXTRACARDIAC EFFECTS
Peripheral vasodilatation
TOXICITY: CARDIAC*
hypotension and ventricular fibrillation
when given for a misdiagnosed SVT**
negative inotropic effect
AV block
sinus arrest
TOXICITY: EXTRACARDIAC
constipation
lassitude
nervousness
peripheral edema
KINETICS
half life 7 h
extensive liver metabolism
20% bioavailability
USES
SVT (also adenosine)
reduction of ventricular rate in atrial fib or
flutter
Ventricular arrhythmias (occasional)
Similar to verapamil
Naturally occuring nucleoside
Half life 10 mins
Activates inward K+ rectifier current and
inhibits Ca current: marked
hyperpolarization and suppression of
calcium dependent action potentials
Bolus inhibits AV node conduction and
increases AV node refractory period*
DOC- prompt conversion of paroxysmal
SVT to sinus rhythm
Interactions
caffeine, theophylline
dipyridamole
TOXICITY:
flushing in 20%
shortness of breath, chest burning in 10%
brief AV block
atrial fibrillation
headache, hypotension, nausea, paresthesias
Effects on Na+/K+ ATPase, sodium
channels, calcium channels
USES:
Digitalis-induced arrhythmias in
hypomagnesemic patients
Torsades des pointes
Hypokalemia and hyperkalemia are both
arrhythmogenic
Therapeutic goal: normalization of
potassium gradients and pools in the body
You might also like
- Letter Request For A DAR CLEARANCEDocument6 pagesLetter Request For A DAR CLEARANCECherry DuldulaoNo ratings yet
- Dinosaur Color by Number WorksheetDocument1 pageDinosaur Color by Number WorksheetShelothaWinaDinarNo ratings yet
- Sample Special Power of Attorney Title WorkDocument1 pageSample Special Power of Attorney Title WorkCherry DuldulaoNo ratings yet
- Sample Acknowledgement Receipt Deed of SaleDocument1 pageSample Acknowledgement Receipt Deed of SaleCherry DuldulaoNo ratings yet
- Free Worksheets Spelling VocabularyDocument1 pageFree Worksheets Spelling VocabularyCherry DuldulaoNo ratings yet
- South Dakota Property Management Agreement PDFDocument2 pagesSouth Dakota Property Management Agreement PDFDrake MontgomeryNo ratings yet
- Sample Special Power of Attorney Title WorkDocument1 pageSample Special Power of Attorney Title WorkCherry DuldulaoNo ratings yet
- DAR Clearance Request for Land TransferDocument6 pagesDAR Clearance Request for Land TransferJhoana Parica Francisco80% (5)
- DAR Clearance Request for Land TransferDocument6 pagesDAR Clearance Request for Land TransferJhoana Parica Francisco80% (5)
- CMDF-AMO SPECS Presentation 2016Document47 pagesCMDF-AMO SPECS Presentation 2016Cherry DuldulaoNo ratings yet
- Sample Acknowledgement Receipt Deed of SaleDocument1 pageSample Acknowledgement Receipt Deed of SaleCherry DuldulaoNo ratings yet
- Free Phonics WorksheetsDocument1 pageFree Phonics WorksheetsRohit DangeNo ratings yet
- Letter Request For A DAR CLEARANCEDocument6 pagesLetter Request For A DAR CLEARANCECherry DuldulaoNo ratings yet
- Affidavit of Buyer TransfereeDocument2 pagesAffidavit of Buyer TransfereeJDNo ratings yet
- Bio Data Format For FreshersDocument1 pageBio Data Format For FreshersCherry DuldulaoNo ratings yet
- Bac 20211020001Document181 pagesBac 20211020001Cherry DuldulaoNo ratings yet
- CVC Words WorksheetDocument1 pageCVC Words WorksheetCherry Duldulao100% (1)
- Turnkey CMP Modality (For Developer)Document39 pagesTurnkey CMP Modality (For Developer)Cherry Duldulao50% (2)
- School Research PDFDocument1 pageSchool Research PDFjencyparkerNo ratings yet
- Cursive Handwriting WorksheetDocument1 pageCursive Handwriting WorksheetCherry DuldulaoNo ratings yet
- Five Senses WorksheetDocument1 pageFive Senses WorksheetCherry DuldulaoNo ratings yet
- Free Counting WorksheetDocument1 pageFree Counting WorksheetCherry DuldulaoNo ratings yet
- Dash Trace Handwriting WorksheetDocument1 pageDash Trace Handwriting WorksheetCherry DuldulaoNo ratings yet
- Blank Writing Practice WorksheetDocument1 pageBlank Writing Practice WorksheetCherry DuldulaoNo ratings yet
- Philippine Green Building Code SummaryDocument25 pagesPhilippine Green Building Code SummaryKrystal Precious Ann NabennegNo ratings yet
- Revised IRR BP220 2008Document75 pagesRevised IRR BP220 2008anyerieramranle100% (5)
- Revised IRR PD 957 2009Document66 pagesRevised IRR PD 957 2009Kaye ReguladoNo ratings yet
- Module 5 State of The Philippine Real Estate Articles 2020 2021Document11 pagesModule 5 State of The Philippine Real Estate Articles 2020 2021Cherry DuldulaoNo ratings yet
- DENR DAO 1996-37 On Environmental Impact System PDFDocument26 pagesDENR DAO 1996-37 On Environmental Impact System PDFAlvin ClariNo ratings yet
- Module 5 State of The Philippine Real Estate Articles 2020 2021Document11 pagesModule 5 State of The Philippine Real Estate Articles 2020 2021Cherry DuldulaoNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Engebretsen2011, INSULINA EN B BLOQDocument7 pagesEngebretsen2011, INSULINA EN B BLOQFabiola Delia Rosas AlarcónNo ratings yet
- Pathophysiology of BREAST CANCERDocument1 pagePathophysiology of BREAST CANCERAlinor Abubacar100% (6)
- Properties of Skeletal MuscleDocument21 pagesProperties of Skeletal Musclenirilib76% (17)
- HEMOLYTIC ANEMIAS AND ACUTE BLOOD LOSS: CAUSES, SIGNS, DIAGNOSIS AND TREATMENTDocument4 pagesHEMOLYTIC ANEMIAS AND ACUTE BLOOD LOSS: CAUSES, SIGNS, DIAGNOSIS AND TREATMENTAjay Pal NattNo ratings yet
- Medication AdministrationDocument88 pagesMedication AdministrationKBD100% (1)
- Mphil Bio-Chemistry ProjectDocument98 pagesMphil Bio-Chemistry ProjectBalaji Rao NNo ratings yet
- CNS: Anatomy, Cases of Trauma, Congenital, Infection, Degeneration & TumorsDocument29 pagesCNS: Anatomy, Cases of Trauma, Congenital, Infection, Degeneration & Tumorsamir hamzahNo ratings yet
- Interval Training For PerformanceDocument20 pagesInterval Training For PerformancePaulo Tsuneta100% (1)
- Cardiology Teaching PackageDocument13 pagesCardiology Teaching Packagesarah morleyNo ratings yet
- Nutrition Folio (Basal Metabolic Rate)Document15 pagesNutrition Folio (Basal Metabolic Rate)Nursakinah NajwahNo ratings yet
- Chapman System of ClassificationDocument6 pagesChapman System of Classificationvineetvishal73No ratings yet
- MSDS Garam MejaDocument5 pagesMSDS Garam MejaDesyrulaNo ratings yet
- NKC Fast Facts - Poop Chart - 5 2017 PDFDocument1 pageNKC Fast Facts - Poop Chart - 5 2017 PDFFaniaNo ratings yet
- Facts Ideas Learning IssuesDocument4 pagesFacts Ideas Learning IssuesGgg2046No ratings yet
- Pathophysiology of Clinical Benign Prostatic Hyperplasia: SciencedirectDocument6 pagesPathophysiology of Clinical Benign Prostatic Hyperplasia: SciencedirectMuhammad Fuad MahfudNo ratings yet
- Bag-Valve-Mask Ventilation (BVM)Document1 pageBag-Valve-Mask Ventilation (BVM)Aidan RajkumarNo ratings yet
- Types of Plant HormonesDocument6 pagesTypes of Plant HormonesKarren ReyesNo ratings yet
- Psychosomatic DisordersDocument79 pagesPsychosomatic DisordersMONIKANo ratings yet
- Naziya & JignaDocument44 pagesNaziya & Jignakishan100% (1)
- Test Bank For Anatomy and Physiology 10th Edition by PattonDocument32 pagesTest Bank For Anatomy and Physiology 10th Edition by PattonCassandraDuncanmcytd100% (34)
- Medico Legal Aspects of DeathDocument206 pagesMedico Legal Aspects of Deathrosana f.rodriguez83% (12)
- ADocument2 pagesAイ ロNo ratings yet
- Handheld Echocardiography: in DepthDocument11 pagesHandheld Echocardiography: in DepthDokter Annisa SppdNo ratings yet
- Cell Signaling Webquest: Part 1: Dropping SignalsDocument3 pagesCell Signaling Webquest: Part 1: Dropping Signalsa60ONo ratings yet
- Trimestral Exam First GradeDocument3 pagesTrimestral Exam First Gradeemmanuel espinozaNo ratings yet
- Unit 4 ObesityDocument40 pagesUnit 4 Obesityapi-306481199No ratings yet
- Seed Maturation Process Explained in DetailDocument22 pagesSeed Maturation Process Explained in DetailHitsugaya AbdullahNo ratings yet
- Indications For Initiation of DialysisDocument11 pagesIndications For Initiation of DialysisMilton BenevidesNo ratings yet
- Asthma Care Quick Reference - Diagnosing and Managing AsthmaDocument18 pagesAsthma Care Quick Reference - Diagnosing and Managing AsthmaMarizka Putri AftriaNo ratings yet
- Fundamental PositionsDocument35 pagesFundamental PositionsVinod Kumar50% (4)