Professional Documents
Culture Documents
For Asthma and COPD
Uploaded by
Howell Yap0 ratings0% found this document useful (0 votes)
16 views14 pageshaha
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documenthaha
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
16 views14 pagesFor Asthma and COPD
Uploaded by
Howell Yaphaha
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 14
1
Drugs Used for the
Management of Asthma
Jason X.-J. Yuan, M.D., Ph.D.
Professor of Medicine and Pharmacology
University of Illinois at Chicago
Institute for Personalized Respiratory Medicine
Department of Medicine
(Section of Pulmonary, Critical Care, Sleep and Allergy )
Department of Pharmacology
Center for Cardiovascular Research
Katzung BG, Masters SB, Trevor AJ
Basic & Clinical
Pharmacology 11e
Chapter 20: Drugs Used in Asthma
(Homer A. Boushey and Bertram G. Katzung)
Reference
Leaning Objectives
Definition and basic pathology of asthma
Various cell types and mediators in the
pathogenesis of asthma
Rationale for the use of -agonist therapy
(bronchodilation) and its side effects
Therapeutic actions of cromolyn (inhibiting
mast cell degranulation), corticosteroids
(anti-inflammation), and theophylline
(bronchodilation and anti-inflammation)
2
Definition of Asthma
(What is Asthma?)
Physiologically characterized a) by
increased responsiveness of the trachea
and bronchi to various stimuli and b) by
widespread narrowing of the airways
Pathologically featured by airway
smooth muscle contraction, mucosal
thickening from edema and cellular
infiltration, an inspissation in the airway
lumen of abnormally thick, viscid plugs
of mucus
Definition of Asthma
Asthma is a chronic inflammatory
disease of the airways
Hyper-responsiveness
Airway contraction (bronchospasm)
Inflammation
Airway/bronchial remodeling
(thickening)
Asthma Therapy
Short-term Relievers:
Bronchodilators
-adrenoceptor agonists (e.g., isoproterenol)
Antimuscarinic agents (e.g., theophylline)
Long-term Controllers:
Anti-inflammatory Agents
Inhaled corticosteroid
Leukotriene antagonists
Inhibitors of mast cell degranulation (e.g.,
cromolyn or nedocromil)
3
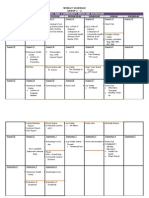
Schematic Diagram of the
Deposition of Inhaled Drugs
Delivery by inhalation results in the greatest local effect on airway smooth muscle
with the least systemic toxicity.
Aerosol deposition depends on particle size, breathing pattern, airway geometry.
Even with particles in the optimal size range of 2-5 m, 80-90% of the total dose of
aerosol is deposited in the mouth or pharynx.
Metered-dose inhaler (MDI)
Pathogenesis of Asthma
(Immunological Model)
1) IgE antibodies bound to mast cells in airway
mucosa
2) On reexposure to antigens, antigen-antibody
interaction on the surface of master cells
triggers release/synthesis of mediators (e.g.,
histamine, tryptase, leukotrienes, and PGs)
3) Mediators (also including cytokines,
interleukins) cause bronchial contraction
(smooth muscle), vascular leakage, cellular
infiltration, mucus hyper-secretion
4) Inflammatory response
Conceptual Model for the
Immunopathogenesis of Asthma
1
2
3
4
Allergen causes synthesis of
IgE which binds to mast cells;
Allergen activates T-cells
On reexposure to allergens,
antigen-antibody interaction
causes release of mediators
Bronchoconstriction, vascular
leakage, cellular infiltration
Cytokines activate eosinophils/
neutrophils releasing ECP/MBP
proteases, PAF, and cause
late reaction
1
2
3
4
3
4
Hyperresponsiveness
Bronchospasm can be elicited by:
Allergens (hypersensitivity to)
Non-antigenic stimuli (e.g., distilled water,
exercise, cold air, sulfur dioxide, and rapid
ventilation) (nonspecific bronchial
hyperreactivity )
Bronchial hyperreactivity is quantitated by
measuring the fall in FEV
1
(forced expiratory
volume in 1 s) provoked by inhaling aerosolized
histamine or methacholine (serially increasing
concentration)
Mechanisms of Bronchial
Hyperreactivity
1) Inflammation of airway mucosa
2) Increased ozone exposure, allergen inhalation,
& viral infection (causing airway inflammation)
3) Increased inflammatory cells (eosinophils,
neutrophils, lymphocytes and macrophages)
and increased products from these cells
(causing airway smooth muscle contraction)
4) Sensitization of sensory nerves (afferent and
efferent vagal nerves) in the airways
5) Cellular mechanisms in airway smooth muscle
cells and epithelial cells
Asthmatic Bronchospasm
Caused by a combination of:
Increased release/synthesis of contractile
mediators (mainly from master cells and
inflammatory cells)
Enhanced responsiveness of airway smooth
muscle to these mediators
Afferent and efferent vagal nerves (e.g., cholinergic
motor fibers innervate M
3
receptors on the smooth
muscle)
Airway smooth muscle cells
Airway epithelial cells
5
Mechanisms of Inhaled
Irritant-mediated Bronchial
Constriction
1
CNS
Inhaled irritants can cause
bronchoconstriction by:
(1) Triggering release of chemical
mediators from response cells (e.g.,
mast cells, eosinophils, neutrophils)
(2) Stimulating afferent receptors to
initiate reflex bronchoconstriction
(via acetylcholine, ACh) or to release
tachykinins (e.g., substance P) that
directly stimulate smooth muscle
contraction
2
1
ACh
Asthmatic Bronchospasm
Treated by drugs that:
Reduce the amount of IgE bound to mast cells (anti-
IgE antibody)
Prevent mast cell degranulation (cromolyn, -
agonists, calcium channel blockers)
Block the action of released mediators (anti-
histamine, leukotriene receptor blockers)
Inhibit the effect of acetylcholine (ACh) released
from vagal motor nerves (muscarinic antagonists)
Directly relax airway smooth muscle (theophylline,
-agonists)
Basic Pharmacology of Agents
for Treatment of Asthma
The drugs mostly used for
management of asthma are:
-Adrenoceptor agonists
Used as short-term relievers or
bronchodilators
Inhaled corticosteroids
Used as long-term controllers or anti-
inflammatory agents
6
Basic Pharmacology of Agents
for Treatment of Asthma
Symathomimetic Agents (-adrenoceptor agonists)
Epinephrine, isoproterenol, salmeterol, formoterol
Corticosteroids
Beclomethasone, flunisolide, fluticasone, triamcinolone
Methylxanthine Drugs
Theophylline, theobromine, caffeine
Antimuscarinic Agents
Ipratropium, atropine
Cromolyn and Nedocromil (inhibitors of mast cell degranulation)
Leukotriene Inhibitors
Zileuton, montelukast, zafirlukast
Other Drugs in the Treatment of Asthma:
Anti-IgE monoclonal antibodies (omalizumab), calcium channel
blockers (nifedipine, verapamil), Nitric oxide donors (sodium
nitroprusside)
Basic Pharmacology
(Sympathomimetic Agents)
Adrenergic Receptors (adrenoceptors):
-receptors (1, 2)
-receptors
1, heart muscle (causing increased heart
rate/contractility); kidney (causing renin
release)
2, airway smooth muscle (causing
bronchodilation); GI smooth muscle, cardiac
muscle, skeletal muscle, vascular smooth muscle
3, adipose tissue (causing lipolysis, increasing
fatty acids in the blood)
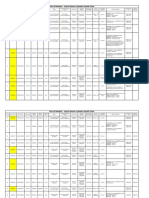
Bronchodilation is Promoted
by Increased cAMP
Bronchodilation
Bronchoconstriction
cAMP
Theophylline
Theophylline
Muscarinic
antagonists
-agonists
Acetylcholine Adenosine
Bronchial tone
+
_
Activate or
increase
Inhibit or
decrease
AC, adenylyl cyclase
7
Basic Pharmacology
(Sympathomimetic Agents)
Mechanisms of Action
Activation of -adrenergic receptor
1 and 2 receptors
G protein-coupled receptor
Stimulation of adenylyl cyclase (AC)
Ten known ACs (AC1-AC10)
AC1, AC3 and AC8 are activated by Ca
2+
/CaM
AC5 and AC6 are inhibited by Ca
2+
/CaM
Increase in the formation of cAMP
Relaxation of airway smooth muscle
Molecular Action of
2
-
agonists to Induce Airway
Smooth Muscle Relaxation
Basic Pharmacology
(Sympathomimetic Agents)
Non-selective -Adrenoceptor
Agonists (
1
and
2
)
Epinephrine
Injected subcutaneously or inhaled as a
microaerosol, rapid action (15 min)
Ingredient in non-prescription inhalants
Ephedrine
Oral intake, long-lasting action, obvious central
effects (used less frequently now)
Isoproterenol
Inhaled as a microaerosol, rapid action (5 min)
8
Basic Pharmacology
(Sympathomimetic Agents)
Selective
2
-Adrenoceptor Agonists (most
widely used -agonists for the treatment of asthma)
Terbutaline, Metaproterenol, Albuterol,
Pirbuterol, Levalbuterol, Bitolterol
Inhalation from a metered-dose inhaler
Bronchodilation is maximal by 30 min and
persists for 3-4 hrs
Salmeterol, Formoterol
Long-acting
2
agonists (12 hrs or more)
High lipid solubility (into smooth muscle cells)
Interact with inhaled corticosteroids to improve
asthma control
Basic Pharmacology
(-adrenoceptor Agonists)
Administration
Inhalation (by aerosol)
Available orally and for injection
Side Effects
Muscle tremor
Tachycardia and palpitations
Increased free fatty acid, glucose, lactate
V/Q mismatch due to pulmonary
vasodilation
Basic Pharmacology
(Corticosteroids)
Mechanism of Action
Anti-inflammatory effect mediated by
inhibiting production of inflammatory
cytokines
Inhibition of the lymphocytic, eosinophic airway
mucosal inflammation of asthmatic airways
Reduce bronchial reactivity
Reduce the frequency of asthma
exacerbations if taken regularly
No relaxant effect on airway smooth muscle
Potentiate the effect of -agonists
9
Basic Pharmacology
(Corticosteroids)
Administration
Inhaled (aerosol treatment is the most
effective way to decrease the systemic
adverse effects, e.g., lipid-soluble
beclomethasone, budesonide, flunisolide,
fluticasone, triamcinolone)
Oral and parenteral (e.g., intravenous
infusion) use is reserved for patients who
require urgent treatment (nonresponders
to bronchodilators)
Clinical Pharmacology
(Corticosteroids)
Side Effects
Dysphonia
Oropharyngeal candidiasis (an opportunistic
mucosal infection caused by the fungus )
Both can be reduced by mouth rinsing with water
after inhalation
vocal cords
Effect of Corticosteroids on
Inflammatory and Structural
Cells in the Airway
1) Anti-inflammation
2) Reducing bronchial reactivity
10
Cellular Mechanism of anti-
inflammatory Action of
Corticosteroids in Asthma
GR, glucocorticoid
receptor
Basic Pharmacology
(Methylxanthine Drugs)
Major methylxanthines
Theophylline
1,3-dimethylxanthine
Aminophylline (a theophylline-ethylenediamine
complex)
Dyphylline (a synthetic analog of theophylline)
Theobromine
3,7-dimethylxanthine
Caffeine
1,3,7-trimethylxanthine
Inexpensive and can be taken orally
Basic Pharmacology
(Methylxanthine Drugs)
Mechanisms of Action
Bronchodilation
Inhibition of phosphodiesterases (PDEs; e.g.
PDE4), which results in an increased level of
cAMP (and cGMP) causing airway smooth muscle
relaxation
Inhibition of adenosine receptor on the surface
membrane (adenosine causes airway smooth
muscle contraction and provokes histamine
release from master cells)
Anti-inflammation
Inhibition of antigen-induced release of
histamine from lung tissue
11
Theophylline Affects Multiple
Cell Types in the Airway
Mechanisms of Theophylline-
mediated Bronchodilation
Bronchodilation
Bronchoconstriction
cAMP
Theophylline
Theophylline
Muscarinic
antagonists
-agonists
Acetylcholine Adenosine
Bronchial tone
+
_
Activate or
increase
Inhibit or
decrease
cGMP
AC GC
PDE4 PDE5 Theophylline
AMP/GMP
ATP/GTP
PDE, phosphodiesterase
Basic Pharmacology
(Antimuscarinic Agents)
Mechanism of Action
Inhibits the effect of acetylcholine (ACh) at
muscarinic (M) receptors
Block airway smooth muscle contraction
Decrease mucus secretion by blocking vagal
activity
Major Antimuscarinic Agents
Atropine
Ipratropium bromide (a selective quaternary
ammonium derivative of atropine)
Tiotropium (for COPD)
12
Antimuscarinic Agent-
mediated Bronchodilation
1
CNS
Atropine and Ipratropium
blocks bronchoconstriction
induced by vagal activity
ACh
Basic Pharmacology
(Cromolyn & Nedocromil)
Mechanism of Action
Blockade of chloride channels and calcium
channels in mast cells (and airway smooth
muscle cells), and inhibition of cellular activation
Inhibition of mast cell degranulation (inhibiting
inflammatory response to allergens, exercise,
cold air. Inhibition of eosinophils/neutrophils to
release inflammatory mediators
Inhibition of bronchial responsiveness (with
long-term treatment)
No bronchodilator or antihistamine activity
Basic Pharmacology
(Leukotriene Inhibitors)
Mechanism of Action
Leukotriene causes bronchoconstriction,
increased bronchial reactivity, mucosal edema,
and mucus hypersecretion
Inhibition of 5-lipoxygenase on arachidonic acid
leads to decreased synthesis of leukotriene
(zileuton)
Blockade of leukotriene D
4
receptors leads to
decreased action of leukotriene (zafirlukast,
montelukast)
Both inhibitors (used orally) decrease airway
responses to allergens and exercise
13
Effects of Leukotrienes on the
Airways and Their Inhibition by
Anti-leukotriene Drugs
LTC4 Receptor
Blockers
LT Synthesis
Inhibitors
Basic Pharmacology
(Other Drugs)
Anti-IgE Monoclonal Antibodies
Omalizumab (anti-IgE Mab)
Calcium channel blockers
Nifedipine, verapamil
Nitric Oxide Donors
Sodium nitroprusside (SNP)
Possible Future Therapies
Monoclonal antibody against to cytokines (e.g.,
IL-4/-5/-8), antagonists of cell adhesion
molecules, protease inhibitors, etc.
Leaning Objectives
Definition and basic pathology of asthma
Various cell types and mediators in the
pathogenesis of asthma
Rationale for the use of -agonist therapy
(bronchodilation) and its side effects
Therapeutic actions of cromolyn (inhibiting
mast cell degranulation), corticosteroids
(anti-inflammation), and theophylline
(bronchodilation and anti-inflammation)
14
Questions
Jason Yuan
312-355-5911 (office phone)
jxyuan@uic.edu (email)
COMRB 3131
You might also like
- Opd Meds Jgej PDFDocument4 pagesOpd Meds Jgej PDFKaty SanchezNo ratings yet
- Management of Febrile SeizuresDocument13 pagesManagement of Febrile SeizuresfitriohpNo ratings yet
- PrayerDocument1 pagePrayerHowell YapNo ratings yet
- For PrintingDocument1 pageFor PrintingHowell YapNo ratings yet
- (FCM3) G7-8. ProjectPlanning - maternalReproductiveHealthDocument11 pages(FCM3) G7-8. ProjectPlanning - maternalReproductiveHealthHowell YapNo ratings yet
- Compiled Case Study-LenovoDocument24 pagesCompiled Case Study-LenovoHowell Yap100% (2)
- CPG Pcap 2012 PDFDocument54 pagesCPG Pcap 2012 PDFroshmae67% (3)
- Opd Meds Jgej PDFDocument4 pagesOpd Meds Jgej PDFKaty SanchezNo ratings yet
- Therapeutic IndexDocument8 pagesTherapeutic IndexHowell YapNo ratings yet
- FM Rotation Weekly Schedule Group C-2Document2 pagesFM Rotation Weekly Schedule Group C-2Howell YapNo ratings yet
- CPG Management of Dengue Infection in Adults (Revised 2nd Edition)Document68 pagesCPG Management of Dengue Infection in Adults (Revised 2nd Edition)umiraihana1No ratings yet
- DDX OsteochondromaDocument2 pagesDDX OsteochondromaHowell YapNo ratings yet
- Febrile Seizure GuidelineDocument1 pageFebrile Seizure GuidelinesmileyginaaNo ratings yet
- 8356Document8 pages8356Howell YapNo ratings yet
- FINAL Outcome Community Grand ProjectDocument4 pagesFINAL Outcome Community Grand ProjectHowell YapNo ratings yet
- W10 Water, Vitamins & MineralsDocument37 pagesW10 Water, Vitamins & MineralsHowell YapNo ratings yet
- Local AnestheticsDocument3 pagesLocal Anestheticsravi98195No ratings yet
- LUCAS vs TUAÑO CaseDocument2 pagesLUCAS vs TUAÑO CaseHowell YapNo ratings yet
- NDocument1 pageNHowell YapNo ratings yet
- 3b Ctc#05 Malaria 06.27.14edited2Document28 pages3b Ctc#05 Malaria 06.27.14edited2Howell YapNo ratings yet
- Henoch SCH NleinDocument42 pagesHenoch SCH NleinHowell YapNo ratings yet
- NDocument6 pagesNHowell YapNo ratings yet
- FCDocument1 pageFCHowell YapNo ratings yet
- GitDocument5 pagesGitHowell YapNo ratings yet
- To DoDocument1 pageTo DoHowell YapNo ratings yet
- UntitledDocument1 pageUntitledHowell YapNo ratings yet
- Community Immersion Program FormatDocument2 pagesCommunity Immersion Program FormatHowell YapNo ratings yet
- Overview of Carbohydrate Metabolism PathwaysDocument3 pagesOverview of Carbohydrate Metabolism PathwaysHowell YapNo ratings yet
- AnthraxDocument3 pagesAnthraxHowell YapNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Resume Template & Cover Letter Bu YoDocument4 pagesResume Template & Cover Letter Bu YoRifqi MuttaqinNo ratings yet
- Iq TestDocument9 pagesIq TestAbu-Abdullah SameerNo ratings yet
- PROF ED 10-ACTIVITY #1 (Chapter 1)Document4 pagesPROF ED 10-ACTIVITY #1 (Chapter 1)Nizelle Arevalo100% (1)
- Survey Course OverviewDocument3 pagesSurvey Course OverviewAnil MarsaniNo ratings yet
- Prenatal and Post Natal Growth of MandibleDocument5 pagesPrenatal and Post Natal Growth of MandiblehabeebNo ratings yet
- Built - in BeamsDocument23 pagesBuilt - in BeamsMalingha SamuelNo ratings yet
- Liebert PSP: Quick-Start Guide - 500VA/650VA, 230VDocument2 pagesLiebert PSP: Quick-Start Guide - 500VA/650VA, 230VsinoNo ratings yet
- M8-2 - Train The Estimation ModelDocument10 pagesM8-2 - Train The Estimation ModelJuan MolinaNo ratings yet
- Circular Flow of Process 4 Stages Powerpoint Slides TemplatesDocument9 pagesCircular Flow of Process 4 Stages Powerpoint Slides TemplatesAryan JainNo ratings yet
- ABP - IO Implementing - Domain - Driven - DesignDocument109 pagesABP - IO Implementing - Domain - Driven - DesignddoruNo ratings yet
- GLF550 Normal ChecklistDocument5 pagesGLF550 Normal ChecklistPetar RadovićNo ratings yet
- Origins and Rise of the Elite Janissary CorpsDocument11 pagesOrigins and Rise of the Elite Janissary CorpsScottie GreenNo ratings yet
- Pre Job Hazard Analysis (PJHADocument2 pagesPre Job Hazard Analysis (PJHAjumaliNo ratings yet
- #### # ## E232 0010 Qba - 0Document9 pages#### # ## E232 0010 Qba - 0MARCONo ratings yet
- Marshal HMA Mixture Design ExampleDocument2 pagesMarshal HMA Mixture Design ExampleTewodros TadesseNo ratings yet
- Accomplishment Report 2021-2022Document45 pagesAccomplishment Report 2021-2022Emmanuel Ivan GarganeraNo ratings yet
- Write UpDocument5 pagesWrite Upmourad baNo ratings yet
- FR Post-10Document25 pagesFR Post-10kulich545No ratings yet
- Assignment 2 - Weather DerivativeDocument8 pagesAssignment 2 - Weather DerivativeBrow SimonNo ratings yet
- Maverick Brochure SMLDocument16 pagesMaverick Brochure SMLmalaoui44No ratings yet
- Radio Frequency Transmitter Type 1: System OperationDocument2 pagesRadio Frequency Transmitter Type 1: System OperationAnonymous qjoKrp0oNo ratings yet
- Java development user guide eclipse tutorialDocument322 pagesJava development user guide eclipse tutorialVivek ParmarNo ratings yet
- Conv VersationDocument4 pagesConv VersationCharmane Barte-MatalaNo ratings yet
- Lecture Ready 01 With Keys and TapescriptsDocument157 pagesLecture Ready 01 With Keys and TapescriptsBảo Châu VươngNo ratings yet
- RUJUKANDocument3 pagesRUJUKANMaryTibanNo ratings yet
- Biagioli Did Galileo Copy The TelescopeDocument28 pagesBiagioli Did Galileo Copy The TelescopeGregory HooNo ratings yet
- CMC Ready ReckonerxlsxDocument3 pagesCMC Ready ReckonerxlsxShalaniNo ratings yet
- Non Circumvention Non Disclosure Agreement (TERENCE) SGDocument7 pagesNon Circumvention Non Disclosure Agreement (TERENCE) SGLin ChrisNo ratings yet
- Rohit Patil Black BookDocument19 pagesRohit Patil Black BookNaresh KhutikarNo ratings yet
- 621F Ap4405ccgbDocument8 pages621F Ap4405ccgbAlwinNo ratings yet