Professional Documents
Culture Documents
Immunopathology
Uploaded by
applesncore0 ratings0% found this document useful (0 votes)
80 views21 pagespath notes
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentpath notes
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
80 views21 pagesImmunopathology
Uploaded by
applesncorepath notes
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 21
IMMUNOPATHOLOGY
DR Dexter,MD FRC Path
Undercover Professor
Department of Pathology
St Georges University
Enabling objectives
Recapitulate the normal development of
hematopoiesis and steps involved in the mat-
uration of different varieties of T cells, B cells,
NK cells, mononuclear phagocytes, antigen
presenting cells and dendritic cells (from
Histology & Immunology Courses).
Recapitulate the mechanisms of functions and
interactions of these cells (from Immunology
Course).
Recapitulate the process of lymphocyte homing
recirculation (Immunology course)
Enabling objectives
Explain the concept of how MHC and clin-
ical tissue typing is achieved (Immunology
Course).
Explain how the major histocompatibility
complex (MHC) coordinates interactions
among immune cells (Immunology Course).
Explain how the common lab tests can
identify abnormalities of immune system
(Immunology Course)
OBJECTIVES FOR PATHOLOGY
COURSE
Differentiate the four varieties of hypersensitivity
based on mechanisms, pathologic changes,
clinical situations, lab data and outcomes.
Identify the main mechanism(s) in a
given clinical scenario of hypersensitivity.
Distinguish the 3 main types of transplant
rejection (hyper acute, acute and chronic)
based on mechanism, morphologic changes,
clinical features and outcomes using renal
transplant as a standard example.
OBJECTIVES
Recognize that deficiencies of complement and
defects in leukocyte functions including
chemotaxis, phagocytosis and lysosomal
activities also lead to immune deficiency and
produce specific patterns of infections.
Identify the infections that characterize AIDS and
the tissue responses in such patients (the viral
and immunological aspects of AIDS will be
covered in the Microbiology course).
OBJECTIVES
Explain the mechanism and clinical features
of Graft versus host reaction.
Distinguish the common immunodeficiency
states (listed) based on mechanisms, clinical
features, lab data and outcomes (Bruton x linked
agammaglobulinemia, selective IgA deficiency,
common variable immunodeficiency, Di George
Syndrome, Severe combined immunodeficiency,
Wiskott Aldrich Syndrome).
OBJECTIVES
Explain the pathogenesis and morphological and
clinical features of autoimmune diseases using
SLE as a classical example. Explain how the
antibody patterns can distinguish between SLE,
Rheumatoid arthritis, Sjogrens syndrome,
Progressive systemic sclerosis and mixed
connective disease.
Explain the meaning of organ specific
autoimmune disease citing examples of thyroid
and stomach
IMMUNITY
Immune system is a collection of organs,
tissues, cells & soluble factors
Immunity protects us against invasion by
foreign agents
BUT is TWO EDGED SWORD
Two main divisions INNATE (not antigen
specific) & ACQUIRED (antigen specific)
INNATE IMMUNITY
ACQUIRED IMMUNITY
PHYSICAL
BARRIERS
CELLULAR CHEMICAL
HUMORAL
CELLULAR
ANTIBODIES
(B CELLS)
CYTOKINES
(T CELLS)
Skin & mucus
membranes
PMNs, Macrophages,
Monocytes & Eosinophils
Enzymes, Acids
& Complement
THE LYMPHOID SYSTEM
Secondary lymphoid
organs
Lymph nodes
Spleen
Tonsils
Mucosa associated
Lymphoid tissue (MALT)
Primary lymphoid organs
Bone marrow
Thymus
ACQUIRED IMMUNITY
B CELLS
Antibodies
Neutralize
microbes
Activate
T CELLS
Directly lyse Produce cytokines
CAN RECOGNIZE
ANTIGENS & BIND
THEM
RECOGNIZE ONLY IF
Ag IS PROCESSED &
PRESENTED
(ROLE OF HLA)
Complement
Certain
Effector cells
(Macrophages,
Neutrophils)
ANTIGEN PRESENTING CELLS
Macrophages
Dendritic cells
B cells
Langerhans cells
Lysis
Phagocytosis
T LYMPHOCYTES
60-70% of the circulating lymphocytes
Each T cell recognizes specific cell bound
antigen by means of TCR ( T cell receptor)
TCR is heterodimer ( & chains)
Is linked to CD3 molecule complex
Along with either CD4 (60% of T cells) or
CD8 (30% of T cells) molecule
Normal CD4 to CD8 ratio is 2:1
T LYMPHOCYTES
CD4 can recognize antigen in context of
MHC II
CD8 binds to class I MHC molecules
MHC restriction
CD4 CELLS CD8 CELLS
All nucleated cells
(MHC I)
Usually process & present
antigens synthesized
in the cell ( e.g. viral proteins)
Endogenous antigens
Antigen presenting cells
(MHC II)
Usually process & present
exogenous antigens
TH 1 cells TH 2 cells
IL-2 & IFN -y IL-4 & IL-5
Delayed hypersensitivity
Macrophage activation
Aid synthesis of other
Antibodies esp. IgE
B LYMPHOCYTES
10-20% of the circulating lymphocytes
Immunoglobulin M is present on the
surface of all B lymphocytes
Is antigen binding component
In addition have complement receptors, Fc
receptors & CD 40
CD 40 binds the CD 40 ligand of T cells &
is essential for B cell maturation
EVALUATION OF IMMUNE
STATUS
Immunoglobulin levels by serum protein
electrophoresis ( gamma fraction)
For selective deficiencies quantitization of
isotopes
Measurement of specific antibody levels
e.g. Tetanus, Rabies, Rubella, Hepatitis B
Skin testing for DTH
Flow Cytometry CD4 / CD8 ratio
EVALUATION OF IMMUNE
STATUS
More specific tests include proliferation of
T cells in response to specific & non
specific stimuli
HYPERSENSITIVITY REACTIONS
DISORDERS OF
THE IMMUNE SYSTEM
AUTOIMMUNE
DISEASES
IMMUNODEFICIENCIES
HYPERSENSITIVITY
REACTIONS
HYPERSENSITIVITY REACTIONS
Reactions of antigen( Ag ) with an
antibody (Ab) or sensitized lymphocyte
which is harmful to the host
Three basic characteristics
Prior sensitization- sensitizing dose
Re exposure to the Ag- challenge dose
Additional exposures usually increase the
severity
Gell & Coombs Classification
(Based on mechanism)
Type I Immediate
IgE
Vasoactive amines
& spasmogenic
substances
Act on BV & SMCs
Asthma,hay
fever,hives
anaphylaxis
Type II Cytotoxic
IgG, IgM
Predispose cells to
lysis or
phagocytosis
AIHA,Grave
s disease,
Good
Pasture Syn.
Type III Immune
complex
IgG, IgM
Bind antigen &
activate
complement
SLE,RA,
Glomerulone
phritis
Type IV
Delayed
T cells
Sensitized T cells
cause tissue injury
Granulomato
us dis. (TB,
Sarcoidosis)
TYPE I HYPERSENSITIVITY
REACTION
is rapidly developing reaction (with in
minutes) of the combination of antigen &
antibody bound to mast cells or basophils.
IgE mediated
TH2 cells play a pivotal role
Can be systemic or localized
FIRST EXPOSURE TO ALLERGEN
Ag presented to TH2 cells by APC
IL-4
IL-3,IL-5 & GM-CSF
Attaches to Fc R
on mast cells
2
nd
EXPOSURE
Cross linking of IgE on
Surface of mast cells
IgE
Degranulation & de novo
Synthesis of mediators
(Contd).
Antigen
IgE
IgE Fc R
PRIMARY MEDIATORS SECONDARY MEDIATORS
1.HISTAMINE-smooth muscle
Contraction
Increased nasal & bonchial
Secretions
2.CHEMOTACTIC FACTORS
For PMNs & Eosinophils
3.ENZYMES
Proteases, acid hydrolases
4.PROTEOGLYCANS
Pack & store other
mediators
1.ARACHIDONIC ACID METABOLITES
Leukotriene B4 chemotactic
PGD2 bronchospasm
2.PLATELET AGGREGATING FACTOR
vascular permeablity, vasodilation
& release of histamine
3.CYTOKINES
TNF , IL-1,3,4,5
LOCALIZED ( ATOPY)
Genetically determined predisposition to
develop localized anaphylactoid reactions
to inhaled & ingested antigens
Patients have increased levels of IgE
Sites skin, nose,lungs,intestine
TYPE I HYPERSENSITIVITY
REACTION
Systemic -anaphylaxis
With I/V administration of antisera,
hormones, penicillin
With in minutes itching, hives & skin
erythema
Anaphylactic shock
If untreated fatal
TYPE II HYPERSENSITIVITY
REACTION
Antibodies against antigens present on
cell surface of cells or other tissue
components
In either case normal or altered surface
antigens
Three antibody dependent mechanisms
TYPE II HYPERSENSITIVITY
REACTION
Normal or altered cell surface
antigen
Binding of antibody
Activation of
complement
Recognized by
NK cells
Alter cell
function
Lysis Phagocytosis
Complement
dependent
Reactions
Antibody dependent
Cell mediated
Cytotoxicity (ADCC)
Antibody mediated
Cellular
Dysfunction
TYPE II
HYPER
SENSITIVITY
1.COMPLEMENT DEPENDENT
REACTIONS
IgG, IgM & Ag
on surface of the cell
Activate complement
MAC complex
Fixation of Ab or C3b
On cell surface
(opsonized)
Phagocytosis
COMPLEMENT DEPENDENT
REACTIONS
EXAMPLES
Transfusion reactions
Erythroblastosis fetalis
Autoimmune hemolytic anemia
Autoimmune thrombocytopenia
Good Pasture syndrome
Pemphigus vulgaris
2.ANTIBODY DEPENDENT CELL
CYTOTOXICITY ( ADCC)
Target cells coated with Ab
Killed by non sensitized cells
Have Fc receptors( Monocytes,
Macrophages, Neutrophils &
Natural killer cells)
Especially those targets which are
Quite large for phagocytosis
e.g. tumor cells, virus infected cells
3. ANTIBODY MEDIATED CELL
DYSFUNCTION
Antibodies can dysregulate function of
cells without cell injury
Myasthenia gravis-Antibodies against
acetylcholine receptors
Graves disease-Antibodies stimulate
follicular cells
TYPE III HYPERSENSITIVITY
REACTION
Incited by antigen antibody complexes
Further activate complement & produce
tissue damage
Immune complexes can form in circulation
(more common) or in situ
But produce disease only when localize in
some organ or tissue
Can be generalized (Deposited in many
organs) or localized (kidney, Joints)
TYPES OF ANTIGENS INVOLVED
EXOGENOUS
1.Infectious agents
Streptococci Glomerulonephritis
Hepatitis B Polyarteritis nodosa
Plasmodium Glomerulonephritis
2.Drugs, Chemicals
Foreign serum Serum sickness
Quinidine Hemolytic anemia
ENDOGENOUS
1.Nuclear antigens SLE
2.Immunoglobulins Rheumatoid
arthiritis
3.Tumor antigens Glomerulo-
nephritis
TYPE III HYPERSENSITIVITY
REACTION
Immune complex deposition
Complement activation
C3a & C5a
Anaphylactoid action Chemotactic action
Increased vascular
permeability
Neutrophils
Tissue injury Cytokines & other mediators
SYSTEMIC IMMUNE COMPLEX
MEDIATED DISEASE
1.FORMATION OF ANTIGEN ANTIBODY
COMPLEXES IN CIRCULATION
2.DEPOSITION OF IMMUNE COMPLEXES
IN VARIOUS TISSUES
3.SUBSEQUENT INFLAMMATORY REACTION
IN MANY SITES THROUGH OUT THE BODY
TYPE III HYPERSENSITIVITY
REACTION
Large complexes with antibody excess are
rapidly removed
Intermediate size or small ones are most
pathogenic
Favored sites are
Renal glomeruli
Joints
Skin
Heart
Serosal surfaces
Small blood vessels
ARTHUS REACTION
Is experimental model of vasculitis
Localized tissue injury by immune
complexes
In previously sensitized individual inject
local antigen
Circulating antibody & antigen diffuse
towards each other & form immune
complexes in walls of dermal vessels
ARTHUS REACTION
Leads to complement fixation and
recruitment of inflammatory cells (PMNs)
Takes 2-6 hrs for evidence of tissue injury
Fibrinoid necrosis in the walls of blood
vessels
TYPE III HYPERSENSITIVITY
REACTION
Diagnosis
Demonstration of immune complexes (e.g.
immunofluorescence, EM)
Detection of immune complexes by blood
assays
TYPE IV HYPERSENSITIVITY
REACTION
Also k. a. cell mediated hypersensitivity
Initiated by sensitized T cells
Includes
Classic delayed type hypersensitivity
(DTH) mediated by CD4 cells
Direct T cell mediated cytotoxicity
DELAYED TYPE
HYPERSENSITIVITY
First exposure to tubercle bacilli
By Antigen presenting cells (MHC II)
CD4 ( TH1 ) cells
Second exposure
Activation of memory cells
Blastic transformation & release of cytokines
DELAYED TYPE
HYPERSENSITIVITY
CYTOKINES
IL-12
Critical for DTH
Secreted by macrophages
Differentiation of T cells
IFN-y
Powerful stimulator
of macrophages
IL-2
Autocrine & paracrine
proliferation of T cells
TNF
Increases vascular permeability
Facilitate extravasation of
Lymphocytes & monocytes
DELAYED TYPE
HYPERSENSITIVITY
Examples
Contact dermatitis
Infections with
intracellular
pathogens
Transplant
rejection
Immunity in
neoplasia
T CELL MEDIATED
CYTOTOXICITY
Sensitized CD8 cells
Recognize antigens present in association
with MHC I (Virus infected cells)
Cause lysis by two mechanisms
Perforin granzyme dependent killing
Fas-Fas ligand dependent killing
TRANSPLANT REJECTION
Host recognizes graft as foreign
Role of both cellular & humoral immunity
Antigens responsible are those of MHC
HLA typing required
Also k. a. Host versus Graft immune
reaction
Three types-Hyperacute, Acute & Chronic
T CELL MEDIATED REACTIONS
Recipient's APCs process
& present the antigen
Antigens presented by the
APCs of the donor itself
CD4 cells CD8 cells
Activated
Cytokines
Increased vascular Recruitment of
Permeability inflammatory cells
Directly lyse the
grafted tissue
ANTIBODY MEDIATED
REACTIONS
ANTIBODIES
Preformed
Complement activation
Arthus type of recation
(hyperacute rejection)
Pts with multiple tranfusions,
previous transplants & multi-
parous females
Prevented by cross matching
Synthesis of antibodies. Can cause:
Complement dependent cytotoxicity
Antibody Dependent Cell mediated
Cytolysis ( ADCC)
Immune complex formation
Vessels main target
( Rejection vasculitis)
HYPERACUTE REJECTION
Immediate (Minutes to hours)
Sudden cessation of urine outflow
Flaccid & cyanotic kidney
M/E-Congestion
Thrombi in capillaries
Necrotizing vasculitis
Neutrophilic infiltration
Infarction & necrosis in severe cases
ACUTE REJECTION
Appear in days to months
Interplay of cellular & humoral immunity
In one patient one or the other mechanism
predominate
ACUTE REJECTION
Acute cellular rejection
Marked interstitial
MONONUCLEAR
infiltrate
Interstitial edema
Lymphocytic tubulitis
May damage endothelium
Responds well to immune-
suppression
Acute rejection vasculitis
Necrotizing vasculitis with
endothelial Cell damage
Thrombosis
Neutrophilic infiltration
Less severe cases marked
thickening of intima
May lead to atrophy & infarction
CHRONIC REJECTION
Progressive increase in serum creatinine
over 4-6 months
IRREVERSIBLE
Vascular changes
Interstitial fibrosis
Loss of renal parenchyma
Tubular atrophy
Abundant interstitial infiltrate of plasma
cells & eosinophils
Methods to increase graft survival
Good HLA matching
Immunosuppression
Blocking action of co-stimulatory
molecules
GRAFT VERSUS HOST DISEASE
Usually with transplant of hematopoietic
cells ( Bone marrow transplant)
Donor tissue is immunocompetent
Mediated by donor lymphocytes
Recipient is immunodepleted ( whole body
irradiation or chemotherapy)
Depletion of donor T cells eliminated the
risk
GRAFT VERSUS HOST DISEASE
Immunocompetent graft
Immunodepleted host
Histoincompatibility
Is type IV hypersensitivity reaction
ACUTE GVH DISEASE CHRONIC GVH DISEASE
> 100 days
Cutaneous injury with
destruction of skin appendages
Strictures in GIT
Cholestatic jaundice
Involution of thymus & depletion
of lymphocytes
Usually < 100 days
Mainly affects immune system
& epithelia of GIT, skin & liver
Rash , jaundice & diarrhea
IMMUNODEFICIENCY
DISEASES
IMMUNODEFICIENCY DISEASES
SECONDARY
PRIMARY
Defects in
B cell
T cell
Complement
Phagocytosis
More common
AIDS, PEM
X Linked Agammaglobulinemia Of
Bruton
Precursor B cells fail to differentiate in to
mature B cells
Mutation in cytoplasmic tyrosine kinase
No light chains
Heavy chains accumulate in cytoplasm
Affected male children present at age of 6-
8 months
Recurrent bacterial infections (lack of
opsonins)
X linked agammaglobulinemia of
Bruton
Persistent Giardia lamblia infection
T cell mediated immunity intact
Polio vaccine can cause paralysis
Markedly reduced B cells in circulation
Rudimentary germinal centers
Absence of plasma cells
Replacement therapy with
immunoglobulins
COMMON VARIABLE
IMMUNODEFICIENCY
Generally affects all classes of antibodies
Failure of differentiation into plasma cells
So near normal number of B cells
Clinical spectrum like Brutons
agammaglobulinemia except the following
Affects both sexes equally
Presents at later age
B cell areas are rather hyperplastic
COMMON VARIABLE
IMMUNODEFICIENCY
Recurrent herpes virus infections are
common
High frequency of autoimmune disorders &
lymphoid malignancies
50 fold increased risk of gastric carcinoma
ISOLATED IGA DEFICIENCY
Most common immunodeficiency
Can be familial or acquired
Defect in differentiation of IgA B
lymphocytes
Commonly asymptomatic
Recurrent gastrointestinal, respiratory &
urogenital infections
High risk of autoimmune disorders &
respiratory allergies
HYPER IGM SYNDROME
Abnormal T cells fail to induce B cells to
make isotypes other than IgM
70 % cases mutation in CD 40L (XLD)
Markedly increased levels of IgM
Absent or very low levels of IgA,IgE & IgG
Normal number of T & B cells
Recurrent pyogenic & opportunistic
infections (Pneumocystis carnii)
DI GEORGE SYNDROME
Defective development of 3
rd
& 4
th
pharyngeal pouches
Deletion in chromosome 22
But not a familial condition
Complete to partial absence of thymus
Congenital heart defects, tetany
DI GEORGE SYNDROME
Recognized early
Recurrent viral, fungal & protozoal
infections
Depletion of paracortical areas of lymph
nodes & periarteriolar sheaths of spleen
SEVERE COMBINED
IMMUNODEFICIENCY
Defect in both cellular & humoral immunity
More commonly in cellular which
secondarily affects humoral immunity
Can be X linked or autosomal recessive
In XLD signal transduction defect in
lymphoid precursors
They fail to be stimulated by cytokines
In AR adenine deaminase deficiency is
common cause
SEVERE COMBINED
IMMUNODEFICIENCY
Accumulation of toxic products which
damage immature T cells
Absence of T cells & agammaglobulinemia
Reduced volume of lymphoid tissue
Present before 6 months of age
Recurrent bacterial, viral, fungal &
protozoal infections
Bone marrow transplant & gene therapy
WISKOTT ALDRICH SYNDROME
THROMBO
CYTOPENIA
IMMUNO
DEFICIENCY
ECZEMA
WISKOTT ALDRICH SYNDROME
Progressive decline in number of T cells
with variable loss of humoral immunity
Pathogenesis not clear
X linked recessive
WAS gene encodes WASP protein
WASP in lymphoid cells &
megakaryocytes
WISKOTT ALDRICH SYNDROME
Recurrent infections with pneumococci,
H.influenzae & pneumocystis carinii
Thromocytopenia with small sized
platelets
Thrombocytopenia cured by splenectomy
Complicated by development of
autoimmune disorders & lymphomas
AIDS
Productive infection of T cells & hence
lysis
Profound defect of T cells
Early in disease course colonizes
lymphoid organs
Details of the virus & its immunological
repercussions- microbiology course
Pathology course-histopathology of
lesions, common infections & other related
pathologies
AIDS(T CELL ABNORMALITIES)
Direct infection of Thymus
Progenitor cells
Infection of T cells
Loss of CD4
precursors
Qualitative
defects
Quantitative
defects
Delayed and ed
TH1 response
Defects in intra-
Cellular signaling
Lysis Apoptosis
AIDS(B CELL ABNORMALITIES)
Paradoxical hypergammaglobulinemia
(multiple infections & polyclonal
stimulation)
But unable to mount response to a new
antigen
So disseminated bacterial infections are
common
Major immunological abnormalities
1) Lymphopenia & inversion of CD4/CD8
ratio
2) Decreased T cell function- Opportunistic
infections, decreased DTH & increased
susceptibility to neoplasms
3) Altered T cell function in vitro
4) Polyclonal B cell activation
5) Altered Monocyte / Macrophage function-
decreased chemotaxis & Phagocytosis,
decreased antigen presenting capacity
Pathological lesions
Associated with immune deficiency
repeated infections & opportunistic
infections (OI)
Neoplasms
Therapy related or iatrogenic
INFECTIONS IN AIDS PATIENT
Opportunistic infections responsible for
80% deaths in these patients
Unusual locations
Presence of large number of organisms
Poor inflammatory response
Disseminated
Simultaneous infections
INFECTIONS IN HIV
Many infections are common e.g. strep.,
H.influenzae, salmonella
But certain are included in AIDS defining
illnesses
Candidais of resp. tract, esophagus
Cryptosporidiosis, isosporiasis (> 1 month)
Extra pulmonary cryptococosis
Coccidioidomycosis- extrapulmonary
INFECTIONS IN HIV
CMV retinitis
Disseminated histoplasmosis
Mycobacterium avium intracellulare
Pneumocystis carnii
Toxoplasmosis brain
MALIGNANCIES IN AIDS
Kaposi sarcoma
Primary CNS lymphoma
NHL e.g. Burkitts lymphoma,
Immunoblastic lymphoma
AUTOIMMUNE DISEASES
AUTOIMMUNITY
Immune reaction against self antigens
Three criteria to label a disease as
autoimmune
Presence of autoimmune disorder
Not secondary to tissue damage
Absence of any other well defined cause
of the disease
Occurs loss of self tolerance
Bone marrow
Pro T cells
Self reactive clones
Deleted by apoptosis
Non self reactive
clones
Self reactive clones
But antigens not expressed
In thymus
Induction of immunity PERIPHERAL TOLERANCE
Repeated stimulation after
Encounter with self antigens
Many normal tissues lack
Co-stimulatory moleclues
Activation induced
Cell death
Clonal anergy
THYMUS
CENTRAL TOLERANCE
CLONAL DELETION
MECHANISM OF AUTOIMMUNE
DISEASES
No evidence for break down of central tolerance
AUTOIMMNE
DISEASES
Failure of peri-
pheral tolerance
Genetic factors
Microbes
GENETIC FACTORS
Familial clustering of many autoimmune
diseases e.g. SLE, AIHA, autoimmune
thyroiditis
Linkage of many autoimmune diseases
with HLA esp. class II
Induction of autoimmune response in HLA
B27 transgenic mice
MICROBIAL AGENTS
Share epitopes with self antigens
If associated with inflammation & necrosis
cause upregulation of co-stimulatory
molecules
Superantigens & microbial products
activate a large number of B & T cells
AUTOIMMUNE DISEASES
Can be organ specific or non organ
specific
Latter are more common
Organ specific ones are
Pernicious anemia (chronic gastritis)
Graves disease
Myasthenia gravis
Autoimmune hemolytic anemias
SYSTEMIC LUPUS
ERYTHEMATOSUS
Chronic , remitting & relapsing often febrile
illness characterized by injury to skin,
joints, kidneys & serosal membranes
F:M 9:1
Common in reproductive age group
Failure of self tolerance
Numerous autoantibodies against nuclear
& cytoplasmic components so not tissue
specific
Antinuclear Antibodies (ANA)
NUCLEOLAR
NON HISTONE
PROTEINS
PROTEINS
BOUND TO RNA
DNA HISTONES
Rim or
Peripheral Guldeep Uppal-SGUSOM
Immuno. Path
Speckled
Diffuse
Nucleolar
SYSTEMIC LUPUS
ERYTHEMATOSUS
But antibodies to ds DNA & Sm antigen
are diagnostic
SYSTEMIC LUPUS
ERYTHEMATOSUS
Whatever cause of antibody production
ultimately leads to tissue injury by immune
complex formation ( Type III reaction)
The antibodies can destroy red cells, white
cells & platelets ( Type II reaction)
ANTIPHOSPHOLIPID
ANTIBODIES
Seen in 40-50% patients
Against proteins complexed to
phospholipids
Can bind to cardiolipin Ag of treponema
(False positive)
Prolong coagulation time in vitro
BUT in vivo cause procoagulant
complications
ANTIPHOSPHOLIPID
ANTIBODIES
Recurrent abortions
Focal cerebral ischemia
Constitute Antiphospholipid antibody
syndrome
LE cell
Nuclei of damaged cells in
Tissues (Joints, pericardium)
Broken leukocytes in vitro
(Glass beads)
Exposed nuclei
ANA react
Homogenization & loss
Of chromatin pattern
Engulfed by phagocytes
HAEMATOXYLYN
BODY
LE CELL
In vivo
In vitro
MORPHOLOGY -KIDNEY
Normal L.M. but deposits on IF
Mesagioproliferative glomerulonephritis
Focal proliferative glomerulonephritis
Diffuse proliferative glomerulonephritis
Membranous glomerulonephritis
Ig & complement deposition in mesagium
If extensive subendothelial ( Wire loop
lesions)
SKIN
Malar or butterfly rash
Accentuates by sun light (photosensitive)
Non scarring
M/E-Vaculoar degeneration of basal
keratinocytes
Some times features of vasculitis
JOINTS
Non erosive synovitis
No deformities
Neutrophils & fibrin in synovial fluid
CVS-pericarditis
Libman Sacks endocarditis
1-3 mm vegetation on any valve & on
either surface of the valve
LIBMAN SACKS ENDOCARDITIS
CLINICAL FEATURES
Anemia
Arthritis
Skin rash
Fever, fatigue
Weight loss
Renal dysfunction
LABORATORY INVESTIGATIONS
Hematological work up
Routine urine
Renal function tests
Hypocomplementemia in active disease
LE cell phenomenon
ANAs
Anti ds DNA & Anti Sm (Diagnostic)
DRUG INDUCED SLE
Procainamide (most common),
Hydralazine, Isoniazid & D-pencillamine
Renal & CNS involvement uncommon
High frequency of anti histone antibodies
Remits with withdrawl of drug
RHEUMATOID ARTHRITIS
Chronic systemic inflammatory disorder
Mainly affects
Small joints
Skin, blood vessels, heart, lungs and
muscles
Symmetric bilateral involvement
RHEUMATOID ARTHRITIS
Non suppurative proliferative polyarthritis
Articular destruction & ankylosis
1% of worlds population
3-5 times more common in females
20-40 years ( more commonly)
Genetic
susceptibility
Arthritogenic
antigen
Inflammation of joints
New Igs act act as
antigens
(IgM against Fc of IgG)
Immune complexes
in synovium
Activated CD4 cells in
synovium
CYTOKINES
Proliferation of
Chondrocytes,
Fibroblasts
Destructive
enzymes
PANNUS
JOINT
DESTRUCTION
PATHOGENESIS
Systemic immune complexes
( e.g. vasculitis)
JOINT INJURY
CLINICAL FEATURES
Insidious onset
Malaise, fatigue, musculoskeletal pain
Small joints involved
Metacarpophalangeal, proximal
interphalangeal joints
Wrists, ankles, elbows, knees
Edematous, painful joints
Morning stiffness
CLINICAL FEATURES
RADIOLOGICALLY:
Joint effusions, juxtaarticular osteopenia
Narrowing of joint space
Loss of articular cartilage
Radial deviation of wrist
Ulnar deviation of fingers
Flexion extension deformities of fingers
(swan neck, boutonniere deformity)
MORPHOLOGY
Edematous, thickened and hyperplastic
synovium
Dense perivascular inflammatory infiltrate
(lymphocytes, plasma cells, macrophages)
Lymphoid follicles
Increased vascularity
Erosion of underlying cartilage by
PANNUS formation
MORPHOLOGY
PANNUS-is a fibrocellular mass of
synovium & synovial stroma consisting of
inflammatory cells and granulation tissue
which cause erosion of the underlying
cartilage
Subchondral cysts and osteoporosis
Neutrophils in synovial fluid
Ultimately fibrous & bony ankylosis
SKIN
Rheumatoid nodules
In 25% with severe disease
Ulnar aspect of forearm,occiput,
lumbosacral area
Less commonly viscera
Firm, non tender nodules in subcutaneous
Central fibrinoid necrosis surrounded by
epithelioid histiocytes, lymphocytes
BLOOD VESSELS
Vasculitic syndrome in severe cases
Catastrophic complication
Medium sized arteries
Vital organs
Does not affect kidneys
Peripheral neuropathy, ulcers & gangrene
DIAGNOSIS
Mainly clinical
Four of the following criteria
Morning stiffness, arthritis in three or more
joints, arthritis of hands joints, symmetric
arthritis, RA nodules, serum RA factor and
radiological changes
RA factor IgM agaist Fc portion of IgG
SJOGREN SYNDROME
Immune mediated destruction of
Lacrimal glands (Xeropthalmia)
Salivary glands (Xerostomia)
Can be primary or secondary
Secondary associated with other
autoimmune disorders (RA, SLE)
Dense lymphocytic infiltration & fibrosis of
the exocrine glands
SJOGREN SYNDROME
ANA in 50-80%
Specific antibodies are anti-SS-A &
anti SS-B (90%)
Lacrimal glands
Salivary glands
Others-Lining of GIT, Respiratory
tract & vagina
SALIVARY GLANDS
Perivascular & periductal infiltrate of
lymphocytes
Lymphoid follicles with germinal
centers
Later on fibrosis and hyalinization
Biopsy of lip is diagnostic
CLINICAL FEATURES
Difficulty in swallowing dry food
Inability to speak continuously
Burning sensation in mouth, eyes
Dry, erythematous & sticky oral mucosa
Enlargement of salivary glands ( parotid)
Blurring of vision
Sandy, gritty sensation in eyes
SYSTEMIC SCLEROSIS
Also k.a. Scleroderma
Characterized by fibrosis of
Skin
Blood vessels
GIT
Lungs
Heart
kidneys
SYSTEMIC SCLEROSIS
Diffuse scleroderma
Localized scleroderma-involvement limited
mainly to skin
Fibrosis because of abnormal activation
of immune system
Not a defect of fibroblasts!
SYSTEMIC SCLEROSIS
SKIN-diffuse sclerosis & atrophy of the
skin
Starts with fingers & extends proximally
Thinning of epidermis & loss of rete ridges
Edema, perivascular infiltrate
Abundant dermal collagen
Atrophy of dermal appendages
CLINICAL FEATURES
Peak incidence 50-60 years
More common in females (3:1)
Raynauds phenomenon
Skin changes
Dysphagia
Symmetric polyarthritis
MIXED CONNECTIVE TISSUE
DISEASE (MCTD)
Co-existence of features suggestive of
SLE, polymyositis, systemic sclerosis
So overlapping clinical features
Serologically antibodies to RNP particles
containing U1RNP
Extremely good response to steroids
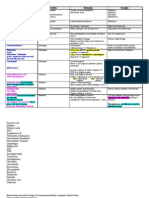
AUTOIMMUNE DISEASES
Disease Nature of Ag Autoantibody
SLE DNA
Sm (ribonuclear)
antidsDNA
Anti Sm
Scleroderma Topoisomerase Anti-scl-70
CREST Centromere Anti-centromere
Sjogrens Ribonulear
proteins
Anti-ss-A,ss-B
MCTD U1RNP Anti-U1RNP
You might also like
- DR - Gold Immunology NotesDocument11 pagesDR - Gold Immunology NotesAaron PhuaNo ratings yet
- Chapter 10 - Diseases of Infancy and ChildhoodDocument17 pagesChapter 10 - Diseases of Infancy and ChildhoodAgnieszka WisniewskaNo ratings yet
- Genetics-Exam 4 1Document5 pagesGenetics-Exam 4 1Farhan Ahmed100% (1)
- Biology Revision Notes Edexcel iGCSEDocument22 pagesBiology Revision Notes Edexcel iGCSEJoshua Jones100% (2)
- Soil Transmitted Helminth PDFDocument90 pagesSoil Transmitted Helminth PDFMinarni HoNo ratings yet
- Pathology B - Gastrointestinal Tract (Esguerra, 2015)Document18 pagesPathology B - Gastrointestinal Tract (Esguerra, 2015)Ars MoriendiNo ratings yet
- Hematology: Dr. I. Quirt Adriana Cipolletti, Jeremy Gilbert and Susy Hota, Chapter Editors Leora Horn, Associate EditorDocument42 pagesHematology: Dr. I. Quirt Adriana Cipolletti, Jeremy Gilbert and Susy Hota, Chapter Editors Leora Horn, Associate EditorRubyrose Tagum100% (1)
- Physiologic MonitoringDocument4 pagesPhysiologic MonitoringAimie DagaleaNo ratings yet
- Topic Outline: Elements of Parasitology (3P's) Types of Association of Living OrganismsDocument6 pagesTopic Outline: Elements of Parasitology (3P's) Types of Association of Living OrganismsJhunrick Corpuz TumpalanNo ratings yet
- CardiopathophysiologyDocument63 pagesCardiopathophysiologyapplesncoreNo ratings yet
- CardiopathophysiologyDocument63 pagesCardiopathophysiologyapplesncoreNo ratings yet
- Hematopoietic SystemDocument39 pagesHematopoietic SystemapplesncoreNo ratings yet
- Anti-Anemia and Hematopoietic Growth FactorsDocument8 pagesAnti-Anemia and Hematopoietic Growth FactorsIsabel CastilloNo ratings yet
- L6-PATHO-Neoplasia (Sept2821)Document12 pagesL6-PATHO-Neoplasia (Sept2821)Erald PaderangaNo ratings yet
- Chapter 11 Blood Vessels 8th Ed NotesDocument7 pagesChapter 11 Blood Vessels 8th Ed NotesKyle Christopher SiaNo ratings yet
- Hemodynamic DisordersDocument85 pagesHemodynamic DisordersTofik Mohammed100% (1)
- CELL OVERVIEW PREVENTION Notes 2015Document7 pagesCELL OVERVIEW PREVENTION Notes 2015Alexander LukashenkoNo ratings yet
- Oral Mucosal Drug Delivery and TherapyDocument289 pagesOral Mucosal Drug Delivery and TherapyАлександр ВолошанNo ratings yet
- Pathology - Lab: Pathology of The HeartDocument8 pagesPathology - Lab: Pathology of The HeartRazel PerezNo ratings yet
- CVS MCQDocument11 pagesCVS MCQمصطفى حسن هاديNo ratings yet
- Diseases of The Immune SystemDocument65 pagesDiseases of The Immune Systemanon_62816775No ratings yet
- Head and Neck McqsDocument3 pagesHead and Neck McqsRajitha DilhanNo ratings yet
- Cellular Injury, Adaptation and Cell DeathDocument8 pagesCellular Injury, Adaptation and Cell DeathJessica Febrina Wuisan100% (1)
- Parasitic AmoebaDocument23 pagesParasitic AmoebaJethrö MallariNo ratings yet
- Gram Positive Bacteria: Sporeforming Nonsporeforming Anaerobe AerobeDocument1 pageGram Positive Bacteria: Sporeforming Nonsporeforming Anaerobe Aerobemonica leeNo ratings yet
- CH 7 Genetic and Pediatric Diseases (P. 243-272, Nature of Genetic Abnormalities Contributing To Human DiseaseDocument16 pagesCH 7 Genetic and Pediatric Diseases (P. 243-272, Nature of Genetic Abnormalities Contributing To Human DiseaseJustine HungNo ratings yet
- Case Study (Preeclampsia)Document6 pagesCase Study (Preeclampsia)Jobelle AcenaNo ratings yet
- University of Santo Tomas: Faculty of Pharmacy - Department of Medical TechnologyDocument7 pagesUniversity of Santo Tomas: Faculty of Pharmacy - Department of Medical TechnologyWynlor AbarcaNo ratings yet
- Robinson Pathology Chapter 20 KidneyDocument11 pagesRobinson Pathology Chapter 20 KidneyElina Drits100% (1)
- HematologyDocument5 pagesHematologyIvy Jan OcateNo ratings yet
- Reversible Cell Injury and Adaptation (09.11.2017)Document25 pagesReversible Cell Injury and Adaptation (09.11.2017)ISRAELNo ratings yet
- 120-Nr-M.D. Degree Examination - June, 2008-Pathology-Paper-IDocument16 pages120-Nr-M.D. Degree Examination - June, 2008-Pathology-Paper-IdubaisrinivasuluNo ratings yet
- Pathology Cell InjuryDocument57 pagesPathology Cell InjuryMajd MustafaNo ratings yet
- Immunopathology Lec 4Document11 pagesImmunopathology Lec 4zaharNo ratings yet
- Activity Tabulation ParasitologyDocument18 pagesActivity Tabulation ParasitologyStephen YorNo ratings yet
- Necrosis and Degeneration - Copy)Document41 pagesNecrosis and Degeneration - Copy)Saubie Aslamiah100% (2)
- Answers To Virology MCQ Paper 2Document8 pagesAnswers To Virology MCQ Paper 2Idrissa ContehNo ratings yet
- General Pathology Saq Sample Exam eDocument7 pagesGeneral Pathology Saq Sample Exam eRIZ KHANNo ratings yet
- Abdominal Assessment: Sequence of ExamDocument7 pagesAbdominal Assessment: Sequence of ExamCristine SyNo ratings yet
- Pathology of InfectiousDocument39 pagesPathology of InfectiousDeEo OnoNo ratings yet
- Chronic Inflammation Non-Specific and GranulomatousDocument47 pagesChronic Inflammation Non-Specific and GranulomatousPradeepNo ratings yet
- 07 Pathological ClacificationDocument10 pages07 Pathological Clacificationraanja2No ratings yet
- The Complement SystemDocument4 pagesThe Complement SystemExamville.com100% (1)
- I. Cellular Adaptations:: Cellular Injury, Cell Adaptation & Cell Death 1. Hyperplasia 3. AtrophyDocument4 pagesI. Cellular Adaptations:: Cellular Injury, Cell Adaptation & Cell Death 1. Hyperplasia 3. AtrophyShuaib SiddiquiNo ratings yet
- HS202 Pathology ExamDocument6 pagesHS202 Pathology ExamJulio dR AltavasNo ratings yet
- C19 2 Hemopoiesis Eythropoiesis LeukopoiesisDocument11 pagesC19 2 Hemopoiesis Eythropoiesis Leukopoiesisnurul azisyah auraNo ratings yet
- Neoplasia I - RecordingDocument6 pagesNeoplasia I - RecordingIS99057No ratings yet
- Apoptosis PPT, Pathological AnatomyDocument15 pagesApoptosis PPT, Pathological AnatomyN J3 CNo ratings yet
- Mitosis: Labeled Diagram: Interphase: Gap 1 Phase (Growth), Synthesis Phase (Copy of DNA), Gap 2 Phase (OrganelleDocument7 pagesMitosis: Labeled Diagram: Interphase: Gap 1 Phase (Growth), Synthesis Phase (Copy of DNA), Gap 2 Phase (Organelleazzahra adeliaNo ratings yet
- General Pathology QuizDocument2 pagesGeneral Pathology QuizMatt DickoNo ratings yet
- Chapter 22 Bone and Joints (2nd Edition)Document23 pagesChapter 22 Bone and Joints (2nd Edition)Abhi KarmakarNo ratings yet
- PATHOLOGY Mendelian DisordersDocument8 pagesPATHOLOGY Mendelian DisordersAmna BaigNo ratings yet
- Class 9 Kasn FLSKF AlsgzsdgsdfhDocument20 pagesClass 9 Kasn FLSKF AlsgzsdgsdfhSiddhivinayak TidakeNo ratings yet
- Introduction To Pathology: Pathology Is The Study (Logos) of Disease (Pathos)Document44 pagesIntroduction To Pathology: Pathology Is The Study (Logos) of Disease (Pathos)53-Deepankar SutradharNo ratings yet
- CiullahemaDocument60 pagesCiullahemaMariel AbatayoNo ratings yet
- Cell Injury & AdaptationDocument22 pagesCell Injury & AdaptationUmam LoyalNo ratings yet
- Microbiology Key NotesDocument12 pagesMicrobiology Key NotesHarini Rajeev LaxminarayanNo ratings yet
- 2.medical HelminthologyDocument148 pages2.medical HelminthologyHanifatur Rohmah100% (2)
- Abdominal AbscessDocument3 pagesAbdominal AbscessIchalAzNo ratings yet
- Trans 1 - Cells As A Unit of Health and DiseaseDocument12 pagesTrans 1 - Cells As A Unit of Health and DiseaseCedrick BunaganNo ratings yet
- MAJOR HISTOCOMPATIBILITY COMPLEX Part 1'Document3 pagesMAJOR HISTOCOMPATIBILITY COMPLEX Part 1'Renzo SalasNo ratings yet
- Chapter 13 Neoplastic Proliferations of White CellsDocument16 pagesChapter 13 Neoplastic Proliferations of White CellsOmar100% (1)
- Immune Response ClassDocument55 pagesImmune Response ClassKoushali BanerjeeNo ratings yet
- Immune ToleranceDocument7 pagesImmune TolerancehamaadaNo ratings yet
- Pathology QuestionsDocument67 pagesPathology QuestionsRedentor MagdayaoNo ratings yet
- Microbiology - ParasitologyDocument34 pagesMicrobiology - ParasitologySasi DharanNo ratings yet
- TrematodesDocument5 pagesTrematodesdhaineyNo ratings yet
- 01 Pathology Paper IDocument12 pages01 Pathology Paper IMithun Abraham PrakashNo ratings yet
- 08 ImmunopathologyDocument118 pages08 ImmunopathologySteven Mark MananguNo ratings yet
- Gastrointestinal Tract (Partial Edit)Document47 pagesGastrointestinal Tract (Partial Edit)applesncoreNo ratings yet
- Renal Pathology: Kidney and The Urinary Collecting SystemDocument37 pagesRenal Pathology: Kidney and The Urinary Collecting Systemapplesncore100% (1)
- Pediatric PathologyDocument27 pagesPediatric PathologyapplesncoreNo ratings yet
- Cardiovascular + Clinical ScenariosDocument36 pagesCardiovascular + Clinical ScenariosapplesncoreNo ratings yet
- Fluid and Hemodynamic DisordersDocument19 pagesFluid and Hemodynamic DisordersapplesncoreNo ratings yet
- Pathology of The Lung Objectives: Define and Use in Proper Context The Following TermsDocument45 pagesPathology of The Lung Objectives: Define and Use in Proper Context The Following TermsapplesncoreNo ratings yet
- Pathology of Infections Objectives: ©bharti B-Pathologyof infections-SGUSOM 2Document25 pagesPathology of Infections Objectives: ©bharti B-Pathologyof infections-SGUSOM 2applesncoreNo ratings yet
- Gluteraldehyde, Peracetic Acid Alcohol, Iodophors QAC (Quarternary Ammonium Compounds)Document3 pagesGluteraldehyde, Peracetic Acid Alcohol, Iodophors QAC (Quarternary Ammonium Compounds)applesncoreNo ratings yet
- Neoplasia Path NotesDocument13 pagesNeoplasia Path NotesapplesncoreNo ratings yet
- Cerebrospinal Fluid Flow - Anatomy and Functions - KenhubDocument8 pagesCerebrospinal Fluid Flow - Anatomy and Functions - KenhubSajal SahaNo ratings yet
- Biology Project: C XIBDocument18 pagesBiology Project: C XIBPranjal SharmaNo ratings yet
- Lesson 1: The Curriculum Guide ObjectivesDocument48 pagesLesson 1: The Curriculum Guide ObjectivesGodwin Jerome ReyesNo ratings yet
- Health Assessment Semi Finals NotesDocument43 pagesHealth Assessment Semi Finals NotesDazell VarronNo ratings yet
- Anatomy Physio ExamDocument2 pagesAnatomy Physio ExamJecxter BedañaNo ratings yet
- MCQ Exemplar - Cell StructureDocument6 pagesMCQ Exemplar - Cell StructurenitikaNo ratings yet
- Female Reproductive AnatomyDocument34 pagesFemale Reproductive AnatomyAswin Dwi PrayudiNo ratings yet
- 4M GeneticsDocument12 pages4M GeneticsAubrey Justine GaleonNo ratings yet
- Science6 ST1 Q2Document2 pagesScience6 ST1 Q2Joseph PederisoNo ratings yet
- Self-Assessment Questions Chapter 14 ImmunityDocument9 pagesSelf-Assessment Questions Chapter 14 ImmunityShahd MohamedNo ratings yet
- Nervous Tissue System-92618Document151 pagesNervous Tissue System-92618gokulkrishnayadhavNo ratings yet
- Gastric Neuroendocrine TumorsDocument17 pagesGastric Neuroendocrine TumorsNelsonLopezNo ratings yet
- Template New Report Akreta Update EropaDocument1 pageTemplate New Report Akreta Update EropaAyu Dyah PrimaningrumNo ratings yet
- AQA Biology GCSE Combined B4 Practice AnswersDocument1 pageAQA Biology GCSE Combined B4 Practice AnswersMahebul MazidNo ratings yet
- Endocrine System Worksheet AnswersDocument3 pagesEndocrine System Worksheet AnswersmariaNo ratings yet
- Bio Ms Sally Part 1Document2 pagesBio Ms Sally Part 1romaehab201912No ratings yet
- Physical & Chemical InjuriesDocument201 pagesPhysical & Chemical Injurieslifeinanutshell0000No ratings yet
- Human Anatomy 5th Edition Saladin Test BankDocument47 pagesHuman Anatomy 5th Edition Saladin Test Bankbevisnhan89cq0m100% (30)
- Cell ModificationDocument1 pageCell ModificationAPZELIA ANGEL DURUINNo ratings yet
- E Operations Manual Intl 0940Document62 pagesE Operations Manual Intl 0940mona miaNo ratings yet
- Anterior Triangle of NeckDocument13 pagesAnterior Triangle of NeckÑäd ÉèmNo ratings yet
- L 051 04Document4 pagesL 051 04Dzuhri Elrich AsakuraNo ratings yet
- Janat00041 0262bDocument2 pagesJanat00041 0262bFranky YehNo ratings yet