Professional Documents
Culture Documents
Drug Study
Uploaded by
Alyssa Marie0 ratings0% found this document useful (0 votes)
1K views7 pagesTramadol is used in the management of moderate to moderately severe pain. The maximum dose is 400 mg / day. Tramadol may increase central nervous system and respiratory depression.
Original Description:
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentTramadol is used in the management of moderate to moderately severe pain. The maximum dose is 400 mg / day. Tramadol may increase central nervous system and respiratory depression.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
1K views7 pagesDrug Study
Uploaded by
Alyssa MarieTramadol is used in the management of moderate to moderately severe pain. The maximum dose is 400 mg / day. Tramadol may increase central nervous system and respiratory depression.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 7
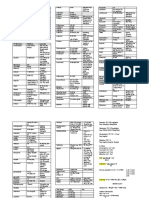
Drug Study
Tramadol
Indication Tramadol is used in the management of
moderate to moderately severe pain.
Extended release tablets are used for
moderate to moderately severechronic pain in
adults who require continuous treatment for an
extended period.
Dosing The recommended dose of tramadol is 50-100
mg (immediate release tablets) every 4-6
hours as needed for pain. The maximum dose
is 400 mg/day. To improve tolerance patients
should be started at 25 mg/day, and doses
may be increased by 25 mg every 3 days to
reach 100 mg/day (25 mg 4 times daily).
Thereafter, doses can be increased by 50 mg
every 3 days to reach 200 mg day (50 mg 4
times daily). Tramadol may be taken with or
without food.
Recommended dose for extended release
tablets is 100 mg daily which may be
increased by 100 mg every 5 days but not to
exceed 300 mg /day. Extended release tablets
should be swallowed whole and not crushed or
chewed.
Drug Interactions Carbamazepine reduces the effect of tramadol
by increasing its inactivation in the
body. Quinidine (Quinaglute, Quinidex)
reduces the inactivation of tramadol, thereby
increasing the concentration of tramadol by
50%-60%. Combining tramadol with
monoamine oxidase inhibitors (for example,
Parnate) or selective serotonin inhibitors
[(SSRIs, for example, fluoxetine (Prozac)] may
result in severe side effects such
as seizures or a condition called serotonin
syndrome.
Tramadol may increase central nervous
system and respiratory depression when
combined with alcohol, anesthetics, narcotics,
tranquilizers or sedative hypnotics.
Side Effects Tramadol is generally well tolerated, and side
effects are usually transient. Commonly
reported side effects
include nausea, constipation,
dizziness,headache, drowsiness,
and vomiting. Less commonly reported side
effects include itching, sweating, dry
mouth, diarrhea, rash, visual disturbances,
and vertigo. Some patients who received
tramadol have reported seizures. Abrupt
withdrawal of tramadol may result in anxiety,
sweating, insomnia, rigors, pain,
nausea, diarrhea, tremors, and hallucinations.
Ketorolac
Indication Ketorolac is used for short-term management
(up to 5 days) of moderately severe acute pain
that otherwise would require narcotics. It most
often is used after surgery.
Dosing Treatment should be started with ketorolac
injection. Tablets are used only if treatment is
continued after patients begin to eat and drink.
The total duration of therapy should not
exceed 5 days because of the potential for
gastrointestinal bleeding and other side
effects. The recommended adult intravenous
single dose is 15 to 60 mg. Multiple
intravenous doses of 15 or 30 mg every 6
hours, not to exceed 60 or 120 mg a day, also
may be used. Following intravenous therapy,
the recommended dose is one or two tablets
initially followed by 1 tablet every 4-6 hours,
not to exceed 40 mg daily. The smaller dose is
used for patients with poor kidney function or
those older than 65 years
Drug Interactions Probenecid (Benemid) should not be
combined with ketorolac because it reduces
the elimination of ketorolac by the kidneys.
This may lead to increased levels of ketorolac
in the body and increased side effects from
ketorolac.
Ketorolac may increase the blood levels
of lithium (Eskalith) by reducing the elimination
of lithium by the kidneys. Increased levels of
lithium may lead to lithium toxicity.
Concomitant use of ketorolac and angiotensin
converting enzyme (ACE) inhibitors may
reduce the function of the kidneys.
Individuals taking oral blood thinners or
anticoagulants [for
example, warfarin(Coumadin) should avoid
ketorolac because ketorolac also thins the
blood, and excessive blood thinning may lead
to bleeding.
Side Effects Common side effects from ketorolac
include rash, ringing in the
ears,headaches, dizziness,
drowsiness, abdominal
pain, nausea, diarrhea, constipation,heartburn,
and fluid retention. NSAIDs reduce the ability
of blood to clot and therefore increase
bleeding after an injury. Ketorolac may cause
ulcers and bleeding in the stomach and
intestines, particularly with use for more than
five days. Sometimes, stomach ulceration and
intestinal bleeding can occur without any
abdominal pain. Black tarry stools, weakness,
and dizziness upon standing may be the only
signs of the bleeding. NSAIDs reduce the flow
of blood to the kidneys and impair function of
the kidneys. The impairment is most likely to
occur in patients with preexisting impairment
of kidney function or congestive heart failure,
and use of NSAIDs in these patients should be
done cautiously. Liver failure has also been
associated with ketorolac. People who are
allergic to aspirin and other NSAIDs should not
use ketorolac. Individuals withasthma or nasal
polyps are more likely to experience allergic
reactions to NSAIDs.
Ampicillin + Sulbactam
Indication This medication contains ampicillin, an
antibiotic used to treat a wide variety of
bacterial infections. Sulbactam makes the
ampicillin more effective.
Dosing The usual oral dose range for most infections
is 250 to 500 mg 4 times daily for 7-14 days.
When used to treat gonorrhea, a single 3.5
gram dose (seven 500 mg capsules) is
administered with probenecid (Benemid). The
probenecid slows down the elimination of
ampicillin so that ampicillin remains in the
body longer. Food in the stomach reduces
how much and how quickly ampicillin is
absorbed. Therefore, ampicillin should be
taken either 1 hour prior to or 2 hours following
a meal for maximal absorption; however, for
persons who experience nausea or stomach
distress after taking ampicillin, it may be taken
with meals.
Drug Interactions Tell your doctor of all the medications you take
(prescription and nonprescription) especially
of: probenecid, tetracyclines, allopurinol. This
drug may interfere with the effectiveness
of birth control pills. Discuss using other
methods of birth control with your doctor. This
medication can affect the results of some
diabetic urine testing products (cupric sulfate-
type). Consult your doctor or pharmacist for
recommendations. Do not start or stop any
medicine without doctor or pharmacist
approval.
Side Effects This medication may cause stomach
upset, diarrhea, nausea,headache, itching and
fatigue during the first few days as your body
adjusts to the medication. If these symptoms
persist or become severe, inform your doctor.
Notify your doctor immediately if an allergic
reaction occurs while taking this medication.
Symptoms include: skin rash, itching, difficulty
breathing, hives, chest pain, facial swelling. If
you notice other effects not listed above,
contact your doctor or pharmacist.
Ibuprofen
Indication Ibuprofen is used for the treatment of mild to
moderate pain, inflammation and fever caused by
many and diverse diseases.
Dosing For minor aches, mild to moderate pain, menstrual
cramps, and fever, the usual adult dose is 200 or
400 mg every 4 to 6 hours.
Arthritis is treated with 300 to 800 mg 3 or 4 times
daily.
When under the care of a physician, the maximum
dose of ibuprofen is 3.2 g daily. Otherwise, the
maximum dose is 1.2 g daily. Individuals should
not use ibuprofen for more than 10 days for the
treatment of pain or more than 3 days for the
treatment of a fever unless directed by a
physician.
Children 6 months to 12 years of age usually are
given 5-10 mg/kg of ibuprofen every 6-8 hours for
the treatment of fever and pain. The maximum
dose is 40 mg/kg daily.
Juvenile arthritis is treated with 20 to 40
mg/kg/day in 3-4 divided doses.
Ibuprofen should be taken with meals to prevent
stomach upset.
Drug Interactions Ibuprofen is associated with several suspected or
probable interactions that can affect the action of
other drugs. Ibuprofen may increase the blood
levels of lithium (Eskalith) by reducing the
excretion of lithium by the kidneys. Increased
levels of lithium may lead to lithium toxicity.
Ibuprofen may reduce the blood pressure-lowering
effects of drugs that are given to reduce blood
pressure. This may occur because prostaglandins
play a role in the regulation of blood pressure.
When ibuprofen is used in combination with
aminoglycosides [for
example, gentamicin (Garamycin)] the blood
levels of the aminoglycoside may increase,
presumably because the elimination of
aminoglycosides from the body is reduced. This
may lead to aminoglycoside-related side effects.
Individuals taking oral blood thinners or
anticoagulants [for example,warfarin (Coumadin)]
should avoid ibuprofen because ibuprofen also
thins the blood, and excessive blood thinning may
lead to bleeding.
Side Effects The most common side effects from ibuprofen
are rash, ringing in the ears, headaches,
dizziness, drowsiness, abdominal
pain, nausea, diarrhea,constipation and heartburn.
NSAIDs reduce the ability of blood to clot and
therefore increase bleeding after an injury.
Ibuprofen may cause ulceration of the stomach or
intestine, and the ulcers may bleed. Sometimes,
ulceration can occur without abdominal pain, and
black, tarry stools, weakness, and dizziness upon
standing (orthostatic hypotension) due to bleeding
may be the only signs of an ulcer. NSAIDs reduce
the flow of blood to the kidneys and impair
function of the kidneys. The impairment is most
likely to occur in patients who already have
impaired function of the kidney or congestive heart
failure, and use of NSAIDs in these patients
should be cautious. People who are allergic to
other NSAIDs, including aspirin, should not use
ibuprofen. Individuals with asthmaare more likely
to experience allergic reactions to ibuprofen and
other NSAIDs. Fluid retention (edema), blood
clots, heart attacks, hypertension and heart
failure have also been associated with the use of
NSAIDs.
Ranitidine
Indication Ranitidine blocks the action of histamine on
stomach cells, and reduces stomach acid
production. Ranitidine is useful in promoting
healing of stomach and duodenal ulcers, and
in reducing ulcer pain. Ranitidine has been
effective in preventing ulcer recurrence when
given in low doses for prolonged periods of
time. In doses higher than that used in ulcer
treatment, ranitidine has been helpful in
treating heartburn and in healing ulcer and
inflammation of the esophagus resulting from
acid reflux (reflux esophagitis).
Dosing May be taken with or without food. Since
ranitidine is excreted by the kidney and
metabolized by the liver, dosages of ranitidine
need to be lowered in patients with
significantly abnormal liver or kidney function.
Drug Interactions Antacids may decrease the absorption of
ranitidine. Safety of ranitidine in children has
not been established. Ranitidine is not habit
forming. Ranitidine can interfere with the
metabolism of alcohol. Patients taking
ranitidine who drink alcohol may have elevated
blood alcohol levels.
Side Effects Minor side effects
include constipation, diarrhea, fatigue,
headache, insomnia, muscle pain, nausea,
and vomiting. Major side effects are rare; they
include: agitation, anemia,
confusion, depression, easy bruising or
bleeding, hallucinations, hair loss, irregular
heartbeat, rash, visual changes, and yellowing
of the skin or eyes.
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Flash Notes Billie-GeneticsDocument29 pagesFlash Notes Billie-GeneticsschxzerrydawnNo ratings yet
- Antibiotic Sensitivity ChartDocument1 pageAntibiotic Sensitivity ChartFerdinand von HebraNo ratings yet
- What Is An Adenovirus InfectionDocument3 pagesWhat Is An Adenovirus InfectionMihaela BajenaruNo ratings yet
- Pedia NotesDocument3 pagesPedia NotesNikki DiocampoNo ratings yet
- Arellano, Ma. Frances Therese D. BSN Ii-A Drug/S Generic/Brand Name Uses Adverse Effect Drug Interaction Nursing ResponsibilitiesDocument6 pagesArellano, Ma. Frances Therese D. BSN Ii-A Drug/S Generic/Brand Name Uses Adverse Effect Drug Interaction Nursing ResponsibilitiesTherese ArellanoNo ratings yet
- Difference Between GERD and PUDDocument7 pagesDifference Between GERD and PUDOla Adel ShabeebNo ratings yet
- Treatment of GoutDocument21 pagesTreatment of GoutAlbertoBeltránRojasNo ratings yet
- Case Study: BronchiectasisDocument5 pagesCase Study: BronchiectasisHanna Mae HernandezNo ratings yet
- GEFITINIBDocument3 pagesGEFITINIBErza GenatrikaNo ratings yet
- Thyroid in PregnancyDocument40 pagesThyroid in PregnancyGPFanNo ratings yet
- Board Ujian NeuroDocument2 pagesBoard Ujian NeuroTrisna RizkiNo ratings yet
- Common Sexually Transmitted Diseases: STD 101 For CliniciansDocument68 pagesCommon Sexually Transmitted Diseases: STD 101 For CliniciansAnonymous h2EnKyDbNo ratings yet
- Latihan Soal UKMPPD Kedokteran VignetteDocument152 pagesLatihan Soal UKMPPD Kedokteran Vignetteelizabeth tanNo ratings yet
- Ascorbic Acid Drug StudyDocument1 pageAscorbic Acid Drug StudyWenalyn Grace Abella Llavan67% (3)
- Azithromycin Drug Monograph 18may2020Document141 pagesAzithromycin Drug Monograph 18may2020OKE channelNo ratings yet
- Laporan Stock Opname Seluruh Outlet Validasi 2 2020-04-01 00:00:00.0Document86 pagesLaporan Stock Opname Seluruh Outlet Validasi 2 2020-04-01 00:00:00.0Kimia ByPass TabananNo ratings yet
- Pid (Pelvic Inflammatory Disease)Document13 pagesPid (Pelvic Inflammatory Disease)Anandila MaulinaNo ratings yet
- Vaccination Reaction in Dog, A DR - Jibachha Sah PresentationDocument13 pagesVaccination Reaction in Dog, A DR - Jibachha Sah PresentationJibachha ShahNo ratings yet
- CefepimeDocument2 pagesCefepimeshendae cosmianoNo ratings yet
- Management of Infection Guidance For Primary Care in IrelandDocument29 pagesManagement of Infection Guidance For Primary Care in IrelandLouise GleesonNo ratings yet
- No Nama Obat Ven Sediaan Harga SatuanjumlahDocument2 pagesNo Nama Obat Ven Sediaan Harga SatuanjumlahCINDYAH ANASTASIA CLARITANo ratings yet
- CKD TakeCare Kidney'sDocument2 pagesCKD TakeCare Kidney'stimtimNo ratings yet
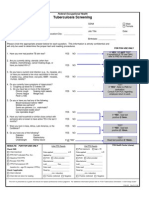
- FOH-25 Tuberculosis Screening (M.25)Document1 pageFOH-25 Tuberculosis Screening (M.25)Maria CabañasNo ratings yet
- Pediatric GERDDocument51 pagesPediatric GERDPatNo ratings yet
- Product Guide 2015Document269 pagesProduct Guide 2015Joy loboNo ratings yet
- MastitisDocument2 pagesMastitisJuviely PremacioNo ratings yet
- PiptazDocument2 pagesPiptazZyrah Ziska Zafra100% (1)
- Butamirate CitrateDocument2 pagesButamirate CitratenisircNo ratings yet
- Common Disorders of The PancreasDocument2 pagesCommon Disorders of The PancreasEli AyaseNo ratings yet
- Dr. Limdawati FK Ukm / Rsi 2012Document45 pagesDr. Limdawati FK Ukm / Rsi 2012Limdawati KweeNo ratings yet