Professional Documents
Culture Documents
Pedia 2.2b Dengue - Dra Bibera
Uploaded by
Dia Dimayuga0 ratings0% found this document useful (0 votes)
35 views10 pagesdengue
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentdengue
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
35 views10 pagesPedia 2.2b Dengue - Dra Bibera
Uploaded by
Dia Dimayugadengue
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 10
Page 1 of 10
Luka, Alrom, Dia, Iza, Dima, Joice PR: Dia
Dra. Bibera | August 1, 2014
PEDIATRICS II
2.2b DENGUE
2014-2015 1st
OUTLINE
I. Dengue
A. Dengue Fever
B. Vector
II. Risk Factors for Dengue Hemorrhagic Fever (DHF)
III. Hypothesis on the Pathgenesis of DHF
A. Homologous Antibodies
B. Heterologous Antibodies
C.
Clinical Case Definition for Dengue Hemorrhagic Fever
IV. Clinical Case Definition for Dengue Shock Syndrome
IV. Key and changing facs in Dengue
V. Updated Clinical Management Guidelines
A. Step 1: Overall Assessment
B. Step 2: Diagnosis, Assessment of Disease Phase and Severity
C. Management Disease Notification
VI. Management Decisions
A. Group A: Patients who may be sent Home
B. Group B: Patient who Should be Referred for Hospitalization
C. Group C: Patients with Severe Dengue who Require Emergency
treatment and Urgent Referral
VII. Summary
References:
PPT, Recording, Old Trans
Legend:
Italicized recording
bold emphasized by
2015 trans
A. DENGUE
Dengue is one disease entity with different clinical presentations
and often with unpredictable clinical evolution and outcome
Transmitted by Aedes aegypti mosquito
Figure 1. Areas at risk for Dengue
Approximately 2.5 billion people live in dengue endemic areas and
50 M infections occur annually
More than 75% live in southeast asia and western pacific regions
A. DENGUE VIRUS
Causes dengue and dengue hemorrhagic fever
Is an arbovirus
It is a flavivirus, from the family flaviviridae. Most of the
viruses from this family are arboviruses.
Transmitted by infected FEMALE mosquitoes
Has 4 serotypes (DEN 1,2,3,4)- Each serotype provides specific
lifetime immunity, and short term cross-term immunity which can
cause severe and fatal disease
DEN-1 and DEN-2: most common isolated serotypes in the
Philippines, but we have all 4 types.
Causes partial and transient protection against subsequent
infections by the other serotypes
If you have dengue now, you have protection from all other
types for the next 6 months. After 6 months, you are again
prone to have your next dengue episode.
Some genetic variants within each serotype appear to be more
virulent or have greater epidemic potential.
B. VECTOR
FEMALE Aedes aegypti
Other vectors: A. albopictus (gaining strength recently), A.
polysiensis, A. scutellaris
Dra. Bibera: Sadly, we have all other vectors, most commonly
A. albopictus. Aegypti is a very sociable mosquito.
The males are the weaker sex, because once they have mated
with the female mosquito, they die while the female
mosquito reigns and becomes the queen
Primarily a DAYTIME feeder
very sociable; lives around human habitation
Transmission sites: communities and schools
Common in urbanized municipalities
This is not true anymore, as it is already common even in the
rural areas
Lays eggs and produces larvae preferentially in artificial containers
Based on the study Entomological Survey in Selected Public
Hospitals in Metro Manila: Containers found positive for A.
aegypti larvae:
Flower vases in accounting office
Nursing office
Urology ward
Basin in OB ward
Plastic cups in hallway
Flight range: <25 meters in open, urban environment
Dispersal: 30-50 meters/day
Visits not more than 2-3 houses
Remains infective during lifetime
High humidity, longer mosquito survival
Average lifespan: 8-15 days
II. RISK FACTORS FOR DENGUE HEMORRHAGIC FEVER
(DHF)
Virus strain (genotype)
Epidemic potential: viremia level, infectivity
Virus Serotype
DHF risk is greatest for DEN-2, followed by DEN-3, DEN-4, and
DEN-1
Pre-existing Anti-Dengue Antibody (Understand this! This is the
basis for the PATHOGENESIS of DHF)
Previous infection
Maternal antibodies in infants
Higher risk in:
Secondary infections
Page 2 of 10
PEDIATRICS II 2.2b
In locations with two or more serotypes circulating
simultaneously at high levels (hyperendemic transmission)
III. HYPOTHESIS ON THE PATHOGENESIS OF DHF
A. HOMOLOGOUS ANTIBODIES (PART 1)
Persons who have experienced a dengue infection develop serum
antibodies that can neutralize the dengue virus of that same
(homologous) serotype
If DEN-1 virus enters the body, it forms a complex with the
neutralizing antibody and is consequently neutralized.
In the vicinity, NON-NEUTRALIZING ANTIBODY also develops
Figure 2. Homologous Antibodies form NON-INFECTIOUS Complexes
B. HETEROLOGOUS ANTIBODIES (PART 2)
In a subsequent infection, the pre-existing heterologous antibodies
form complexes with the new infecting virus serotype, but do not
neutralize the new virus
If DEN-2 virus enters the body, it forms a complex with the non-
neutralizing antibody. Consequently, the body cannot produce
specific antibodies for DEN-2, because it is already BOUND to a
non-neutralizing antibody.
Hence, the virus is not neutralized and is free to replicate
Figure 3. Heterologous Antibodies form INFECTIOUS Complexes
C. HETEROLOGOUS COMPLEX (PART 3)
Antibody-dependent enhancement is the process in which certain
strains of dengue virus, complexed with non-neutralizing
antibodies, can enter a greater proportion of cells of the
mononuclear lineage, thus increasing virus production
Figure 4. Heterologous Complexes Enter More Monocytes, Where Virus
Replicates
The heterologous complexes enter the monocytes where the virus can replicate
and trigger inflammatory cascade.
For a secondary infection, it becomes worse because there is a delay in the
production of antibodies.
D. PART 4
Infected monocytes release vasoactive mediators, resulting in
increased vascular permeability and hemorrhagic manifestations
that characterize DHF and DSS
HOST RISK FACTORS
Race
o Blacks less susceptible to shock
Nutritional Status
o Protein calorie malnutrition reduces risk to DHF/DSS (
Nimmanitya et al 1993)
o Malnutrition is protective since it suppresses cellular immune
response
o Children with malnutrition do not have an intact immune
system. Dengue likes healthy kids!
DENGUE CLINICAL SYNDROMES
A. Undifferentiated fever
B. Classic dengue fever
C. Dengue hemorrhagic fever
D. Dengue shock syndrome
A. UNDIFFERENTIATED FEVER
May be the most common manifestation of dengue
Prospective study found that 87% of students infected were either
asymptomatic or only mildly symptomatic
Other prospective studies including all age- groups also
demonstrate silent transmission
B. CLINICAL CHARACTERISTICS OF DENGUE FEVER
Fever
Headache
Muscle and joint pain
Nausea/vomiting
Rash
Hemorrhagic manifestations
C. HEMORRHAGIC MANIFESTATIONS OF DENGUE
Skin hemorrhages: (+) torniquet test, petechiae, purpura,
ecchymoses
Page 3 of 10
PEDIATRICS II 2.2b
Gingival bleeding
Nasal bleeding
Gastro-intestinal bleeding: hematemesis, melena, hematochezia
Hematuria
Increased menstrual flow
Figure 5. (+)Torniquet test not always synonymous to Dengue. It is seen in any
viral infection.
D. CLINICAL CASE DEFINITION FOR DENGUE HEMORRHAGIC
FEVER
MUST FULLFILL ALL 4 NECESSARY CRITERIA:
1. Fever, or recent history of acute fever (2-7 days)
2. Hemorrhagic manifestations
3. Low platelet count (100,000/mm3 or less)
4. Objective evidence of leaky capillaries:
Leaky capillaries is the main pathophysiology of dengue
hemorrhagic fever
Elevated hematocrit (20% or more over baseline); any
hematocrit > 40%; a drop in hct >20% following volume
replacement
Low albumin
Pleuralor other effusions because you have a lot of fluids
getting out of the BV into the 3rd space
Leaky capillaries Leakage of fluid because of capillary
permeability. This is the main pathophysiologic mechanism
that sets it apart from Dengue Fever thats why we don't look
at platelet count, we look at ELEVATED HCT because
fluid/plasma leaks out of the BV so you will have your elevated
Hct even in situations wherein you will have volume
replacement or even pushing a lot of IV fluids that Hct will go
up, then youre dealing with DHF.
Very difficult to diagnose DHF because you have to fulfill all 4
necessary criteria
FROM 2015B TRANS
CRITICAL STAGE OF DHF
End of febrile phase (1st 48 hours afebrile)
Onset of Shock is acute and occurs at the time of defervescence
Acute abdominal pain
Cold, clammy extremities, rapid and weak pulse
Narrow pulse pressure (<20mmHg)
Circumoral and peripheral cyanosis
Skin blotchy, mottled, purplish
Table 1. Grading of Dengue Hemorrhagic Fever. Grades III and IV are
considered to be Dengue Shock Syndrome
III. CLINICAL CASE DEFINITION FOR DENGUE SHOCK
SYNDROME
4 criteria for DHF + CIRCULATORY FAILURE manifested indirectly by all
of the following:
Rapid and weak pulse (Check the Dorsalis Pedis pulse since this will
be affected first)
Narrow pulse pressure ( 20 mmHg) OR hypotension for age (< 80
mmHg systolic < 5 yrs and 90 mmHg systolic > 5 yrs)
Narrow pulse pressure of 20 mmHg difference of systolic and
diastolic, so even if you have a normal systolic pressure,(e.g.
120/100) but has narrow pulse pressure, then thats a warning sign
of shock.
Cold, clammy skin and altered mental status
Frank shock is direct evidence of circulatory failure
FROM 2015 TRANS
A. CLINICAL COURSE OF DSS
Usually occurs between D3-D7 of illness
Critical period 24-48 hours
Adequate urine output and return of appetite-good
prognostic signs
Prolonged shock and metabolic acidosis-poor prognostic
signs (precipitate occurrence or enhance DIC->massive
bleeding)
If no treatment, dies within 12-24 hours after shock ensues
Recovery from shock is 2-3 days
Common findings in convalescence: sinus bradychardia and
arrhythmia
Characteristic confluent petecchial rash with small round
areas of normal skin
B. UNUSUAL MANIFESTATIONS OF DSS
CNS involvement
o Encephalitis
o Encephalopathy
Hepatic Involvement
o Jaundice
o Liver Failure with hepatic encephalopathy
o Increase liver enzymes
Page 4 of 10
PEDIATRICS II 2.2b
C. LABORATORY DIAGNOSIS
Thrombocytopenia
Hemoconcentration
Leukopenia
Lymphocytosis with 15-20% atypical lymphocytes 1-2 days
before defervescence
Hemostatic abnormalities:
o Prolonged PTT; decreased fibrinogen, decreased clotting
factors, increased fibrin split products
Other tests:
o Elevated liver enzymes
o Hyponatremia
o Increased BUN and creatinine
o Low Albumin
D. LABORATORY CONFIRMATION
Serologic examination
Hemagglutination Inhibition test
o Most widely used
o 4 fold or greater rise in inhibiting antibody titre in paired
sera
o Titre of 1:1280
Dengue ELISA
o Newer test
o Detection of specific IgM or IgG antibodies
o Requires only single blood samples
Dengue IgM capture (MAC-ELISA)
o Simple and rapid test
o Primary Infection: IgMAb positive: Day 5
o IgM antibody significantly higher in primary than in
o secondary dengue
Dengue NS1 test: Day 1-4
Virological confirmation:
o Isolation of dengue virus from serum or autopsy samples
Confirmation of all dengue virus by immunofluourescence
o Demonstration of dengue virus by PCR
o Sample preferably obtained 3-5 days after onset of fever
IV. KEY AND CHANGING FACTS IN DENGUE
Primarily an urban disease, now spreading to rural areas
worldwide
Co-circulation with multiple serotypes are common
Imported cases are common
DOH ON ALERT FOR TOUGHER DENGUE- CARRYING
MOSQUITO
A. TOUGHER AEDES
Behavior changes in Aedes cause for whole year round
activity.
o Reports about "evolved" breeds of mosquitoes that lay their
eggs even in polluted water in Peru.
o They can breed even in dirty environments like septic tanks.
Before: loves to breed only in artificial containers, now it
can breed anywhere. Also, it doesn't need rainfall
anymore for dengue. We can have dengue during
summer months, it only peaks during rainy season.
In the Philippines, there is a possibility that local
mosquitoes may have also evolved and are now breeding
even in areas without "clean" water.
B. NIGHT-BITING AEDES MOSQUITO
Philippine Association of Entomologists reported a study
conducted last year regarding Aedes albopictus:
o Daytime and night time feeder (biting time is extended from
6-8pm and 11pm to 1 am)
o Natural habitat is in the forested area of Mount Makiling.
SUGGESTED DENGUE CASE CLASSIFICATION AND LEVELS OF
SEVERITY (WHO 2009) (APPENDIX 1 and 2)
REVISED DENGUE CLASSIFICATION (DOH 2011) PHILIPPINIZED
VERSION
Added: flushed skin
Warning signs: decreased or no urine output with 6 hours
CLINICAL PROBLEMS ENCOUNTERED DURING THE DIFFERENT PHASES
OF DENGUE
Table 1. Phases of Dengue
1 Febrile
phase
a. Dehydration;
b. High fever may
cause neurological
disturbances and febrile
seizures in young
children
Fluid replacement is the
cornerstone of treatment
Encourage oral intake of
oral rehydration solution
(ORS), fruit juice and other
fluids containing electrolytes
and sugar to replace losses
from fever and vomiting
2 Critical
phase
Shock from plasma
leakage; Severe
hemorrhage; Organ
impairment
3 Recovery
phase
Hypervolaemia ( only in
excessive IVF therapy)
associated with
pulmonary edema or
CHF
Rehydrating oral fluids:
o Oral rehydration solution
o Fruit juice
o Rice water
Adequate oral fluid intake may be able to reduce the number of
hospitalizations
o In a hospital and health centre-based study in Nicaragua, fluid
intake during the 24 hours before being seen by a clinician
was statistically associated with decreased risk for
hospitalization of dengue fever patients .
o Similar results were obtained for children <15 years of age,
older adolescents, and adults in independent analyses.
CLINICAL QUESTION
A. In patients with DF/DHF who are NOT admitted, what oral
fluids are to be given? How much and how should it be given?
Page 5 of 10
PEDIATRICS II 2.2b
RECOMMENDATION #1:
Oral rehydration solution should be given as follows based on
weight, using the currently recommended ORS
Weight >3-10 kg 100 cc/kg
>10-20 kg 75
>20-30 kg 50-60
>30-60 kg 40-50
o Level of Evidence: Class 3 Grade A
RECOMMENDATION #2:
Sports drinks should NOT be used in children.
o Level of Evidence: Class 3 Grade A
B. What anti-pyretic is safe to give in a child with dengue fever?
Dengue Fever
o endemic in the country; occurs whole year round
o always part of the differential diagnosis of fever especially those
presenting with influenza-like illness
o Paracetamol is the recommended medicine for fever by WHO
o Aspirin, mefenamic acid, ibuprofen and other NSAIDs are NOT
recommended
Things to realize in giving medications for dengue
o The goal of treatment is NOT to increase the platelet count.
o Treatment should be geared towards decreasing plasma
leakage which is the main pathophysiology of dengue
V. UPDATED CLINICAL MANAGEMENT GUIDELINES-
ADMINISTRATIVE ORDER NO. 2012-0006
Stepwise Approach to Management of Dengue
A. STEP 1: OVERALL ASSESSMENT
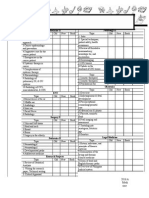
Table 2. Overall assessment: History and PE
Table 3. HEMODYNAMIC ASSESSMENT: CONTINUUM OF HEMODYNAMIC
CHANGES
Parameters
Stable
Circulation
Compensated
shock
Hypotensive
shock
Heart rate
Normal
heart rate
for age
Tachycardia Severe tachycardia with
bradycardia in late shock
Blood
pressure
Normal
blood
pressure for
age.
Normal pulse
pressure for
age.
Normal
systolic
pressure but
rising diastolic
pressure.
Narrowing
pulse.
Postural hypotension
Narrowed pulse pressure
(<20 mmHg).
Hypotension.
Unrecordable BP .
Respiratory
rate
Normal
respiratory
rate for age
Tachypnea Metabolic acidosis/
hyperpnea/ Kussmauls
breathing
Sensorium
Clear and
lucid
Clear and lucid Change of mental state
restless, combative
Capillary
refill time
Brisk (<2 sec) Prolonged (>2
sec)
Very prolonged, mottled
skin
Extermities Warm and
pink
extremities
Cool
peripheries
Cold, clammy extremities
Peripheral
pulse volume
Good volume Weak &
thready
Feeble or absent
Note: shock can be missed if you do not touch the patient
LABORATORY/INVESTIGATIONS:
Full Blood Count (FBC) should be done at the first visit.
Dengue diagnostic tests- viral culture isolation or PCR
*Investigation: A full blood count should be done at the first visit.
A hematocrit test in the early febrile phase establishes the
patients own baseline hematocrit.
Repeat FBC at least once daily. A decreasing white blood cell
count makes dengue very likely. A rapid decrease in platelet count
in parallel with a rising haematocrit compared to the baseline is
suggestive of progress to the plasma leakage/critical phase of the
disease. In the absence of the patients baseline, age-specific
population hematocrit levels could be used as a surrogate during
the critical phase.
Additional tests should be considered as indicated (and if
available). These should include tests of liver function, glucose,
serum electrolytes, urea and creatinine, bicarbonate or lactate,
cardiac enzymes, ECG and urine specific gravity
B. STEP 2: DIAGNOSIS, ASSESSMENT OF DISEASE PHASE AND
SEVERITY
DETERMINE:
Is this dengue?
Phase of dengue (febrile/critical/recovery)
Presence of Warning signs
Hydration and hemodynamic status
Does patient require admission?
C. STEP 3: MANAGEMENT DISEASE NOTIFICATION
In dengue-endemic countries, cases of suspected, probable and
confirmed dengue should be notified as soon as possible so that
appropriate public health measures can be initiated. Laboratory
confirmation is not necessary before notification, but should be
obtained.
The later the notification, the more difficult it is to prevent dengue
transmission.
HISTORY PHYSICAL EXAMINATION
Onset of fever/ illness
Oral intake
Assess for warning signs
Diarrhea
Seizures, impaired
consciousness, behavioral
changes
Urine output
Other relevant Hx: dengue in
family members/neighbors,
travel for dengue-endemic
areas,co-existing conditions,
jungle trekking/swimming,
recent unprotected sexual or
drug use behaviour
Mental state & GCS score
Hydration status
Hemodynamic status*
Tachypnea/ acidotic
breathing/ pleural effusion
Abdominal tenderness/
hepatomegaly/ ascites
Rash and bleeding
manifestations
Tourniquet test (repeat if
previously negative or if
there is no bleeding
manifestation)
Page 6 of 10
PEDIATRICS II 2.2b
VI. MANAGEMENT DECISIONS
A. GROUP A: Patients Who May Be Sent Home
Patients with all of the following:
1. Able to tolerate adequate volumes of oral fluids
2. Pass urine at least once every 6 hours
3. Do not have any of the warning signs, particularly
when fever subsides.
4. Stable hematocrit
Ambulatory patients should be monitored daily for disease
progression decreasing WBC, defervescence, warning signs until
out of the critical period
Advice to return immediately to the hospital if they develop any
of the warning signs.
Table 4. ACTION PLAN : GROUP A (Home Care)
ORS Reduced osmolarity ORS (245 mmol/L)
No sports drinks or fluids containing high
sugar/glucose
Plain water will cause electrolyte imbalance
Paracetamol Use appropriate dosages for children
Not more than 4g for adults
Do not give aspirin, ibuprofen or other NSAIDs
TSB
Antibiotics are not necessary
Dengue Home
Care Card &
Advice on when
to return to
hospital
Bed rest
Fluids
Fever management
Warning signs: bleeding, freq vomiting,
abdominal pain, drowsiness, mental confusion
or seizures, pale, cold or clammy hands and feet,
diff in breathing, dec or no urine output w/in 6
hrs
B. GROUP B: PATIENT WHO SHOULD BE REFERRED FOR
HOSPITALIZATION
Patients with any one of the following: Co-existing conditions that
may make dengue or its management more complicated, i.e.
pregnancy, infancy, old age, obesity, DM, renal failure, chronic
hemolytic diseases
Social circumstances, i.e. living alone, living far from ahealth
facility without reliable means of transport
Warning signs present
Figure 6. Dengue Without Warning Signs
FLUID MANAGEMENT FOR PATIENTS ADMITTED
WITHOUT WARNING SIGNS AND WITHOUT SHOCK
IVF(Isotonic solutions) : D5 LRS, D5 Acetated Ringers, D5 NSS/ D5
0.9 NaCl
Computation of Maintenance IVF
Periodic assessment needed for appropriate fluid adjustment
Monitor clinical parameters/hemodynamic status and correlate
with Hct
Decrease IVF anytime based on clinical assessment
Figure 7.
GROUP C: PATIENTS WITH SEVERE DENGUE WHO REQUIRE
EMERGENCY TREATMENT AND URGENT REFERRAL
Judicious IVF resuscitation is essential and usually sole intervention
required
Goals of fluid resuscitation:
o Improve central and peripheral circulation (decreasing
tachycardia, improving blood pressure, pulse volume, warm
and pink extremities, and capillary refill time <2 seconds)
o Improve end-organ perfusion i.e. stable conscious level
(more alert or less restless), urine output 0.5 ml/kg/hour,
decreasing metabolic acidosis.
What Personal Protection measures can be done?
Insect Repellents and duration of protection
Table 5.
Page 7 of 10
PEDIATRICS II 2.2b
VII. SUMMARY
Changes in the behavior of the vector caused changes in
epidemiology of dengue
Appropriate out-patient care including the proper use of Oral
rehydraton salt solution as initial fluid management may be life-
saving and Paracetamol remains to be the safest anti-pyretic of
choice in dengue
Fluid management and proper clinical evaluation remain to be
the cornerstone of treatment
Pop Quiz
1. A 10month old boy was brought to a clinic due to cough and fever
of 40C. Noted generalized hyper-pigmented rashes, which are starting
to desquamate. HR: 110; RR: 60. Whats the best thing to do?
(Measles)
a. Since at convalescent stage, advice mom to give anti-pyretics for
fever then increase oral fluid intake
b. Give Vit A, then send the patient home
c. Since complication like pneumonia is likely, admit to start antibiotics
2. The most common complication of rubella in adolescent girls is?
a. Thrombocytopenia
b. Arthritis
c. Encephalitis
d. Hepatitis
3. A 12 yo girl was brought to the clinic due to generalized pruritic
maculo-papular rashes with sore throat and mild headache. No
prodromal symptoms were noted. What PE finding will not be
associated with this girls condition?
a. Post auricular lymph nodes
b. Absence of kopliks spots
c. Confluent maculopapular rashes
d. Low grade fever
4. Which is true of mumps infection?
a. Parotitis occurs in 90% of cases
b. Orchitis is common in pre-pubertal male
c. Majority of infections are asymptomatic
d. CNS complications in 15%
5. Secondary bacterial super-infection of skin lesions in patients with
varicella is caused by this flesh eating bacteria
a. Staph epidermidis
b. Staph aures
c. Strep pyogenes
d. Strep pneumonia
6. A 15month old girl was brought to the clinic due to high-grade fever
of 4days duration. Fever started 3 days ago. Patient presented with
mild respiratory tract infection. Upon admission, patient was noted to
be irritable with maculo-papular rash on face and trunk. Temp was
37C. No other PE findings found. What is the most likely cause?
a. Erythema infectiosum
b. Coxsackie A16
c. HHV6
d. Influenza
7. True regarding the period of communicability of viral exanthems?
a. Varicella is most communicable when lesions are encrusted
b. Erythema infectiosum is most communicable during appearance of
maculo-papular rash on extremities
c. Measles is least communicable 4 days after onset of rash
d. Rubella is most communicable 4 days before onset of rash
8. A 5 yo girl suspected to have measles due to erythematous maculo-
papular rashes with koplik spots and conjunctivitis. What other
prodromal symptoms may be found?
a. Arthralgia
b. Post auricular adenopathy
c. Photophobia
d. Productive cough
9. True of post exposure prophylaxis of varicella
a. Acyclovir may be given in immunized patients 96 hours post
exposure
b. IVIG may be an alternative to VZIG and to be given 7-10days post
exposure
c. Varicella vaccine may be given within 7days post
d. VZIG must be administered within 96 h post exposure
10. The rashes seen in HFMD least affect this part of the body
a. Peri-oral
b. Buttock
c. Trunk
d. Soft palate.
11. The congenital heart disease as single defect of rubella is expected
at this time of infection
a. 4-8w
b. 9-12w
c. 12-16w
d. 18-24w
12. According to WHO treatment of choice of uncomplicated
chikungunya is:
a. Aspirin
b. Paracetamol
c. Steroids
d. NSAIDS
13. Which is not true regarding dengue virus?
a. All serotypes can cause severe and fatal disease
Page 8 of 10
PEDIATRICS II 2.2b
b. Life time immunity is provided by an infection from a specific
serotype
c. Some genetic variance appear to be more virulent than others
d. Dengue virus dont provide transient form of short term immunity
14. 7 yo male brought to ER due to fever of 4 days duration and
persistent abdominal pain with episodes of vomiting. Classify dengue
using the revised WHO classification.
a. Dengue without warning signs
b. Dengue with warning signs
c. Severe dengue with organ impairment
d. Severe dengue with plasma leakage
15. Using the WHO classification for DHF how would you classify the
patient in #15?
a. DHF I
b. DHF II
c. DHF III
d. DHF IV
16. Which is true of Aedes aegypti mosquito?
a. They are night and a daytime feeder
b. Breeds in any stagnant water
c. Mosquito survival may be shortened with humidity
e. High flying mosquito
17. The main pathophysiologic mechanism differentiating dengue
fever from dengue hemorrhagic fever is?
a. Antibody dependent enhancement
b. Anti body clotting factors
c. Severe plasma leakage
d. Cardiovascular collapse
18. Using the standard WHO classification the following criteria are
needed to diagnose DHF, except:
a. Increase in hematocrit despite fluid resuscitation
b. Platelet count of <150,000
c. Hemorrhagic manifestations
d. Fever of 2-7 days
19. Warning signs of dengue include the following, except:
a. Mucosal bleed
b. Persistent vomiting
c. High grade fever
d. Hepatomegaly
20. Which is true regarding the management of dengue?
a. Prophylactic transfusion with fresh frozen plasma is indicated for
platelet count of <50,000
b. Steroids may be given in severe dengue
c. Fluid management remain to be the cornerstone of treatment
regardless of severity
d. Ibuprofen may be given for tempereature at least 38 C
21. A 7 year old girl hospitalized because of 4 days fever and
thrombocytopenia 100,000 with one episode of epistaxis 3 days after
hospitalization on her second afebrile day she was noted to have puffy
eyelids with increased work of breathing, RR=40 per min, BP= 90/60,
there was decreased breath sounds noted bilaterally with abdominal
girth increase with note of ascites. Pulses were fair. Based on the
revised WHO criteria, this phase exemplifies severe dengue with?
a. Severe organ impairment
b. Severe plasma leakage
c. Severe hemorrhage
d. Severe cardiovascular collapse
Page 9 of 10
PEDIATRICS II 2.2b
APPENDIX
Appendix 1. New dengue classification
Page 10 of 10
PEDIATRICS II 2.2b
Appendix 2. Suggested Dengue Case Classification and Levels of Severity (WHO 2009)
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- 01 Jan IncompleteDocument123 pages01 Jan IncompleteDia DimayugaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- 1 MED II 6 - Systemic Therapy in Cancer PDFDocument14 pages1 MED II 6 - Systemic Therapy in Cancer PDFDia DimayugaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Pedia 2.1a Bacterial Infections - Dra CarlosDocument4 pagesPedia 2.1a Bacterial Infections - Dra CarlosDia DimayugaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Pharma NotesDocument6 pagesPharma NotesDia DimayugaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Day 1 April 27 SundayDocument1 pageDay 1 April 27 SundayDia DimayugaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- 1st LE Ophthalmology (2 Files Merged)Document16 pages1st LE Ophthalmology (2 Files Merged)Dia DimayugaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Pharmcheatsheets PDFDocument13 pagesPharmcheatsheets PDFDia DimayugaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- 1st LE MedicineDocument11 pages1st LE MedicineDia DimayugaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Autonomous Growth-Remote EffectsDocument4 pagesAutonomous Growth-Remote EffectsDia DimayugaNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- 5: Diarrhea and Constipation: MedicineDocument7 pages5: Diarrhea and Constipation: MedicineDia DimayugaNo ratings yet
- 1st LE ChecklistDocument2 pages1st LE ChecklistDia DimayugaNo ratings yet
- Glomerular DiseasesDocument7 pagesGlomerular DiseasesDia DimayugaNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- BallardScore ScoresheetDocument1 pageBallardScore ScoresheetIsabel BarradasNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- 5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDocument2 pages5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDia DimayugaNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- 5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDocument2 pages5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDia DimayugaNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- FYI InvitationDocument1 pageFYI InvitationDia DimayugaNo ratings yet
- 5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDocument2 pages5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDia DimayugaNo ratings yet
- A Young Lasallian Is US Environmental ScholarDocument1 pageA Young Lasallian Is US Environmental ScholarDia DimayugaNo ratings yet
- IM WW Case 2Document10 pagesIM WW Case 2Dia DimayugaNo ratings yet
- Nubel 1997 PCR Primers To Amplify 16S rRNA Genes From CyanobacteriaDocument6 pagesNubel 1997 PCR Primers To Amplify 16S rRNA Genes From CyanobacteriaHoballahNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Formal Laboratory ReportDocument2 pagesFormal Laboratory ReportDia DimayugaNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Activity 2Document3 pagesActivity 2Dia DimayugaNo ratings yet
- SharksDocument2 pagesSharksDia DimayugaNo ratings yet
- DEFINITION AND NATURE OF SOCIOLOGY IntroDocument2 pagesDEFINITION AND NATURE OF SOCIOLOGY IntroDia Dimayuga100% (3)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Chemical Bonds - Ionic or CovalentDocument4 pagesChemical Bonds - Ionic or CovalentDia DimayugaNo ratings yet
- Coronavirus Health News July 2020Document84 pagesCoronavirus Health News July 2020tuni santeNo ratings yet
- Patient A (Click On The Link To "Complete Patient A's Karyotype")Document2 pagesPatient A (Click On The Link To "Complete Patient A's Karyotype")ZzaiRraNo ratings yet
- Endocrine Gland Disorders and MetabolismDocument74 pagesEndocrine Gland Disorders and MetabolismRatnam hospitalNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Risk Assesment in Alcohol ConsumptionDocument21 pagesRisk Assesment in Alcohol ConsumptionDiya lizbeth joseNo ratings yet
- Unit 21 Authorised Assignment Brief For Learning Aim A and B Medical Physics Application Version 1 October 2016Document3 pagesUnit 21 Authorised Assignment Brief For Learning Aim A and B Medical Physics Application Version 1 October 2016isha yousafNo ratings yet
- Nursing Management of A Patient With Close FractureDocument15 pagesNursing Management of A Patient With Close FractureJoshuaYapNo ratings yet
- NCP Risk For Activity IntoleranceDocument4 pagesNCP Risk For Activity IntoleranceBAGUIO CATSNo ratings yet
- Bomba MedtronicDocument40 pagesBomba MedtronicrafaelplNo ratings yet
- Best definition stem cell quiz questionsDocument6 pagesBest definition stem cell quiz questionsChoe Yoek Soek0% (1)
- Valori Contract An. 2023 - Paraclinic - 20.09.2023Document21 pagesValori Contract An. 2023 - Paraclinic - 20.09.2023Matteo si Sofia vlog'sNo ratings yet
- Nines P Bautista, MD, MSDocument12 pagesNines P Bautista, MD, MSadnep1991No ratings yet
- Gabix Caps Leaflet PakistanDocument2 pagesGabix Caps Leaflet Pakistandalalala7662No ratings yet
- Postpartum BluesDocument17 pagesPostpartum BluesVeliani Putri anggrainiNo ratings yet
- Uterine Rupture and Cervical TearDocument16 pagesUterine Rupture and Cervical Tearsangita patil0% (1)
- Illegal Drugs and Its Ill EffectsDocument83 pagesIllegal Drugs and Its Ill EffectsJAIGLO LAYNONo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 9 Months Marathon Training Plan - OdtDocument6 pages9 Months Marathon Training Plan - OdtMichaelKahnertNo ratings yet
- The Relationship Between Internet Addiction and Mental Health ConDocument7 pagesThe Relationship Between Internet Addiction and Mental Health ConBrandusa TurlacNo ratings yet
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosis Pathophysiolog Y Planning Intervention Rationale EvaluationDocument1 pageNovilyn C. Pataray BSN - Ii: Assessment Diagnosis Pathophysiolog Y Planning Intervention Rationale EvaluationCharina Aubrey100% (3)
- DR Walsh Autism Ocd Pandas Depression MethylationDocument6 pagesDR Walsh Autism Ocd Pandas Depression MethylationAnupama PouloseNo ratings yet
- A CASE STUDY ON Chronic Renal FailureDocument2 pagesA CASE STUDY ON Chronic Renal FailureJake Yvan DizonNo ratings yet
- Pharmacy Formulary - Booklet - 2016Document178 pagesPharmacy Formulary - Booklet - 2016pcartercNo ratings yet
- IMCI Learning FeedbackDocument1 pageIMCI Learning Feedbackinah krizia lagueNo ratings yet
- MORPHINEDocument39 pagesMORPHINEShlok RathodNo ratings yet
- Drugs requiring loading dosesDocument1 pageDrugs requiring loading dosesandirio7486No ratings yet
- 4 - The Circulatory System - PPTDocument110 pages4 - The Circulatory System - PPTRinopro 555No ratings yet
- CETEBE Leafleat 165x235mm 4pagesDocument2 pagesCETEBE Leafleat 165x235mm 4pagestsveta.bozhinovaNo ratings yet
- Test Bank For Evidence Based Practice in Nursing Healthcare 4th EditionDocument36 pagesTest Bank For Evidence Based Practice in Nursing Healthcare 4th Editiontyphous.madrierdvfzai100% (47)
- Rheumatoid Arthritis Diagnosis and ManagementDocument53 pagesRheumatoid Arthritis Diagnosis and ManagementamereNo ratings yet
- I-3 Pediatric and Adolescent GynecologyDocument8 pagesI-3 Pediatric and Adolescent GynecologyuvioscribdNo ratings yet
- Integrins As Therapeutic TargetsDocument8 pagesIntegrins As Therapeutic TargetsAnonymous ceYk4p4No ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)