Professional Documents
Culture Documents
Arterial Compression of Nerve Is The Primary Cause of Trigeminal Neuralgia
Uploaded by
Tejo Pramono0 ratings0% found this document useful (0 votes)
14 views6 pagesArterial compression of nerve is the primary cause of trigeminal neuralgia. Decompression of veins need not be a priority when performing microvascular dissection.
Original Description:
Original Title
10072_2013_Article_1518
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentArterial compression of nerve is the primary cause of trigeminal neuralgia. Decompression of veins need not be a priority when performing microvascular dissection.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
14 views6 pagesArterial Compression of Nerve Is The Primary Cause of Trigeminal Neuralgia
Uploaded by
Tejo PramonoArterial compression of nerve is the primary cause of trigeminal neuralgia. Decompression of veins need not be a priority when performing microvascular dissection.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
ORI GI NAL ARTI CLE
Arterial compression of nerve is the primary cause of trigeminal
neuralgia
Guo-qiang Chen
Xiao-song Wang
Lin Wang
Jia-ping Zheng
Received: 11 April 2013 / Accepted: 7 August 2013 / Published online: 21 August 2013
The Author(s) 2013. This article is published with open access at Springerlink.com
Abstract Whether arterial or venous compression or
arachnoid adhesions are primarily responsible for com-
pression of the trigeminal nerve in patients with trigeminal
neuralgia is unclear. The aim of this study was to determine
the causes of trigeminal nerve compression in patients with
trigeminal neuralgia. The surgical ndings in patients with
trigeminal neuralgia who were treated by micro vascular
decompression were compared to those in patients with
hemifacial spasm without any signs or symptoms of tri-
geminal neuralgia who were treated with microvascular
decompression. The study included 99 patients with tri-
geminal neuralgia (median age, 57 years) and 101 patients
with hemifacial spasm (median age, 47 years). There were
signicant differences between the groups in the relation-
ship of artery to nerve (p \0.001) and the presence of
arachnoid adhesions (p \0.001) but no signicant differ-
ence in relationship of vein to nerve. After adjustment for
age, gender, and other factors, patients with vein com-
pression of nerve or with artery compression of nerve were
more likely to have trigeminal neuralgia (OR = 5.21 and
42.54, p = 0.026 and p \0.001, respectively). Patients
with arachnoid adhesions were less likely to have trigem-
inal neuralgia (OR = 0.15, p = 0.038). Arterial compres-
sion of the trigeminal nerve is the primary cause of
trigeminal neuralgia and therefore, decompression of veins
need not be a priority when performing microvascular
dissection in patients with trigeminal neuralgia.
Keywords Demyelination Hemifacial spasm
Microsurgical decompression Nerve compression
Trigeminal neuralgia
Introduction
Trigeminal neuralgia is characterized by severe facial pain
in the distribution of the trigeminal nerve that is paroxys-
mal, provokable, unilateral, and not accompanied by sen-
sory loss [1, 2]. The pain typically lasts only seconds, but is
described as excruciating, and is triggered by sensory
stimuli that can include chewing, yawning, and speaking
[3]. The pain is episodic and pain-free intervals can range
from day to years. The incidence of trigeminal neuralgia is
reported to be approximately 4 per 100,000 population and
gradually increases with age; the condition is rare before
40 years of age and the average age of onset is 60 years
[25].
Though the condition has been well-studied, there is still
debate regarding the pathophysiology. Most experts agree
that the etiology is segmental demyelination of trigeminal
sensory nerves in the nerve root or brainstem, and the
demyelination is due to chronic compression of the nerve
root where it exits from the pons [3, 6, 7]. Compression can
be due to vascular abnormalities such as an aneurysm or
arteriovenous malformation [8], and demyelination due to
multiple sclerosis has been described [6]. Most theories,
however, consider compression from an artery and/or vein
(e.g., superior cerebellar) as the trigeminal nerve exits the
pons as the cause [3, 5, 9]. Though vascular compression is
the most widely accepted theory, other theories such as
bioresonance have been examined [10].
Medical treatment for trigeminal neuralgia primarily
consist of anticonvulsants [11]. Carbamazepine is the
G. Chen X. Wang (&) L. Wang J. Zheng
Department of Neurosurgery, Yuquan Hospital of Tsinghua
University, 5 Shijing Shan Road, Shi Jing Shan District,
Beijing 100049, China
e-mail: waxiso@126.com
1 3
Neurol Sci (2014) 35:6166
DOI 10.1007/s10072-013-1518-2
rst-line treatment, and other that are used include phe-
nytoin, oxcarbazepine and lamotrigine. Other medications
that can be tried include gabapentin and baclofen. When
medical treatment is ineffective, or a patient cannot tolerate
the side effects, the primary surgical treatment is micro-
vascular decompression.
Microvascular decompression is performed based on the
hypothesis that compression of the trigeminal nerve is
responsible for the demyelination and pain [1215]. The
procedure is performed via a retrosigmoid posterior fossa
craniotomy, and the root of the trigeminal nerve is explored
for signs of compression, which are then relieved by
microdissection and moving the vessel causing the com-
pression. The most common vessels identied as causing
compression are the superior cerebellar artery and anterior
inferior cerebellar artery [1215]. However, there is debate
regarding the cause of compression which is focused on
arterial compression, venous compression, or compression
secondary to adhesions [1216].
Thus, the purpose of this study was to determine the
causes of trigeminal nerve compression in patients with
trigeminal neuralgia undergoing microsurgical decompres-
sion, and compare the results with examination of the tri-
geminal nerve in patients without symptoms of trigeminal
neuralgia undergoing microdissection for hemifacial spasm.
Patients and methods
This prospective, case-controlled study included 99
patients with trigeminal neuralgia who were cured by
microscopic decompression surgery at Yuquan Hospital of
Tsinghua University from November 2008 to April 2010,
and 101 patients with hemifacial spasm without any signs
or symptoms of trigeminal neuralgia who were treated with
microsurgical decompression in the same period and
served as the control group. Patients with hemifacial spasm
who were undergoing microdissection were chosen for the
control group because the trigeminal nerve would be visi-
ble and could be examined during the course of surgery. No
patient in the study had both trigeminal neuralgia and
hemifacial spasm. This study was approved by the Insti-
tutional Review Board of the hospital, and all patients
provided written informed consent.
All trigeminal neuralgia patients had failed or were
unable to tolerate medical therapy, and some had under-
gone prior surgical procedures including gasserian gan-
glion block, nerve avulsion, retrogasserian rhizotomy,
peripheral nerve block, and gamma knife surgery. Preop-
erative visual analogue scale (VAS) pain scores with 0
indicating no pain and 10 indicating the worst pain imag-
inable were obtained for trigeminal neuralgia patients.
Microvascular dissection was performed in a standard
manner [17]. Intraoperative ndings recorded included the
presence of compression and the vessel(s) causing the
compression and the presence of adhesions. The relation-
ship between the vessel and the nerve was categorized as
either none, close to nerve, contact, or compression. All
patients were followed up in the outpatient clinic.
Patients with hemifacial spasm also received standard
microvascular dissection [18], and the trigeminal nerve was
examined but not operated on. Observations of the tri-
geminal nerve were the same as those done for trigeminal
neuralgia patients.
Statistical analysis
Categorical data were presented as number with percentage
and compared using Fishers exact test. Continuous data
were presented as median with inter-quartile range (range
from 25th to 75th percentiles) and compared using the
MannWhitney test. Logistic regression model analysis
was performed to nd the independent impact factors of
trigeminal neuralgia. Data were analyzed with using SPSS
15.0 statistics software (SPSS Inc., Chicago, IL, US), and a
p \0.05 was considered statistically signicant.
Results
A total of 99 patients (47 males and 52 females; median
age: 57 years) with trigeminal neuralgia were included in
the analysis. The course of trigeminal neuralgia ranged
from 1 month to 30 years (median: 5 years). Eighty-ve
patients were treated with carbamazepine. The control
group consisted of 101 patients (32 males and 69 females;
median age: 47 years) with hemifacial spasm.
The characteristics of the patients in each disease group
are summarized in Table 1. The patients with trigeminal
neuralgia were signicantly older than the patients with
hemifacial spasm (median age: 57 vs. 47 years, p \0.001);
70.7 % of the patients with trigeminal neuralgia were over
50 years old compared with only 41.6 % of the patients
with hemifacial spasm (p \0.001). More males were
included in the trigeminal neuralgia group than in the
hemifacial spasm group (47.5 vs. 31.7 %, p = 0.03).
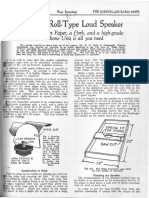
Representative images of artery compression, vein
compression, and arachnoid adhesions are shown in Fig. 1.
The relative position of an artery and the trigeminal nerve
was signicantly associated with trigeminal neuralgia
(p \0.001) (Table 1). Among the 200 patients, 76 had an
artery compressing the trigeminal nerve, and 68 of these
patients had trigeminal neuralgia (68.7 %), whereas only 8
had hemifacial spasm (7.9 %). Among 37 patients noted to
have arterial contact with the trigeminal nerve, 12 had
trigeminal neuralgia (12.1 %) and 25 had hemifacial spasm
62 Neurol Sci (2014) 35:6166
1 3
(24.8 %). Of 12 patients noted to have the artery close to
but not touching the trigeminal nerve, only 2 had trigem-
inal neuralgia, whereas 10 had hemifacial spasm. Lastly, 21
patients were found to have arachnoid adhesions, and of
these, 18 had hemifacial spasm while only 3 had trigeminal
neuralgia (17.8 vs. 3.0 %, p \0.001) (Table 1). There was
no signicant difference between the disease groups in the
frequency of a vein compressing, being in contact, or being
close to the nerve (Table 1).
The results of logistic regression analysis are shown in
Table 2. After adjustment for age, gender, and other
factors, patients with a vein compressing the nerve were
more likely to have trigeminal neuralgia (OR = 5.21,
p = 0.026) as were patients with a vein in contact with the
Table 1 Summary for the patients characteristics by disease groups
Trigeminal
neuralgia
(n = 99)
Hemifacial
spasm (n = 101)
p value
Age (year) 57.0 (49.0, 64.0) 47.0 (40.0, 57.0) \0.001*
Age group
B30 2 (2.0 %) 3 (3.0 %) \0.001*
[30B50 27 (27.3 %) 56 (55.4 %)
[50B70 59 (59.6 %) 39 (38.6 %)
[70 11 (11.1 %) 3 (3.0 %)
Gender
Female 52 (52.5 %) 69 (68.3 %) 0.030*
Male 47 (47.5 %) 32 (31.7 %)
Vein
None 59 (59.6 %) 68 (67.3 %) 0.268
Close to nerve 5 (5.1 %) 9 (8.9 %)
Contact 21 (21.2 %) 13 (12.9 %)
Compression 14 (14.1 %) 11 (10.9 %)
Artery
None 17 (17.2 %) 58 (57.4 %) \0.001*
Close to nerve 2 (2.0 %) 10 (9.9 %)
Contact 12 (12.1 %) 25 (24.8 %)
Compression 68 (68.7 %) 8 (7.9 %)
Arachnoid adhesions
Yes 3 (3.0 %) 18 (17.8 %) \0.001*
No 96 (97.0 %) 83 (82.2 %)
Course of the
disease (year)
5.0 (2.0, 12.0) NA
VAS 7.0 (7.0, 9.0) NA
* Indicates a signicant difference between disease groups
Fig. 1 Representative intraoperative images of a artery compression
and vein close, b vein compression, and c arachnoid adhesions
Neurol Sci (2014) 35:6166 63
1 3
nerve (OR = 4.22, p = 0.008). Patients with an artery
compressing the nerve were more likely to have trigeminal
neuralgia (OR = 42.54, p \0.001). In addition, patients
with arachnoid adhesions were less likely to have trigem-
inal neuralgia (OR = 0.15, p = 0.038).
Lesions were frequently found at the maxillary branch,
and most of them involved one nerve. All trigeminal
neuralgia patients were followed up for a minimum of
2 years. Patients report no improvement in their symptoms
had been excluded from this study.So all of these 99
patients in analysis were cured after surgery.
Discussion
The ndings of this study indicate that compression of the
trigeminal nerve by an artery is most often the cause of
trigeminal neuralgia rather than compression of the nerve
by a vein. These results indicate that in patients with
arterial compression, complete decompression is required
and removal of adhesions are also necessary, but no
treatment of the vein is needed. This study is unique in that
the control group consisted of patients without symptoms
of trigeminal neuralgia in whom the trigeminal nerve could
still be examined. Prior studies used cadavers as the control
group which may have affected the ndings. During
microvascular decompression in patients with hemifacial
spasm, the arachnoid above the auditory nerve is opened
and the trigeminal nerve can be observed.
Much of the theoretical evidence for the treatment of
trigeminal neuralgia with microvascular dissection is from
cadaveric anatomic studies [19]. However, anatomic
changes noted in cadavers do not necessarily reect ana-
tomic variations seen intraoperatively. Few animal models
have been developed to study compression of the trigem-
inal nerve root [20]. Advances in imaging techniques have
allowed for detailed examination of neurovascular struc-
tures and studies in patients with trigeminal neuralgia have
demonstrated contact between vessels and the trigeminal
nerve [2124]. The majority of the evidence for vascular
compression of the trigeminal nerve as the cause of tri-
geminal neuralgia is from studies examining outcomes
after microsurgical decompression [1215, 17].
Zhang et al. [15] recently reported the results of 154
consecutive patients with trigeminal neuralgia who under-
went microvascular decompression, and the initial and
5-year pain-free rates were 84 and 72 %, respectively.
Obvious vessel compression observed during surgery was
signicantly associated with long-term pain relief
(OR = 3.2). Sekula et al. [12] reported that 31 of 36
patients (86 %) with a mean age of 73 years had excellent
outcomes after microvascular decompression for trigeminal
neuralgia. Tucer et al. [13] reported good outcomes in 37
patients who received microvascular decompression for
trigeminal neuralgia, and found that the only factors
affecting prognosis of the surgery were intraoperative
detection of compression and signs of compression on
preoperative magnetic resonance imaging (MRI) and MR
Table 2 Summary for the
impact factors of trigeminal
neuralgia
* Indicates a signicant
association to trigeminal
neuralgia
Crude OR (95 % CI) p value Adjusted OR (95 % CI) p value
Age (year) 1.06 (1.03, 1.08) \0.001* 1.07 (1.03, 1.11) 0.001*
Gender
Male 1.95 (1.10, 3.47) 0.023* 1.37 (0.60, 3.08) 0.453
Female Reference Reference
Vein
None Reference Reference
Close to nerve 0.64 (0.20, 2.02) 0.446 2.69 (0.61, 12.00) 0.193
Contact 1.86 (0.86, 4.04) 0.116 4.22 (1.46, 12.22) 0.008*
Compression 1.47 (0.62, 3.48) 0.384 5.21 (1.22, 22.15) 0.026*
Artery
None Reference Reference
Close to nerve 0.68 (0.14, 3.42) 0.642 0.87 (0.13, 5.73) 0.883
Contact 1.64 (0.68, 3.93) 0.269 1.69 (0.56, 5.12) 0.351
Compression 29.00 (11.67, 72.08) \0.001* 42.54 (13.39, 135.19) \0.001*
Arachnoid adhesions
Yes 0.14 (0.04, 0.51) 0.003* 0.15 (0.03, 0.90) 0.038*
No Reference Reference
64 Neurol Sci (2014) 35:6166
1 3
angiography (MRA) studies. Oesman and Mooij [14] also
reported good results of microvascular decompression, and
that immediate resolution of symptoms postoperatively
was the most important predictor of long-term relief of
pain. Despite the encouraging results of individual studies,
a recent Cochrane systematic review by Zakrzewska and
Coakham [25] found that although microvascular decom-
pression is likely the most effective therapy in correctly
diagnosed patients, high-quality prospective studies are
lacking.
Vein compression is frequently found during surgery in
patients with trigeminal neuralgia, but in many cases the
site of vein compression is not consistent with the area of
pain, and decompression of the vein by moving the vessel
of ligation with electrocoagulation does not resolve the
symptoms or only transient improvement is observed. Few
studies, have reported trigeminal neuralgia due to venous
compression alone [16]. During microvascular dissection,
manipulation of the veins is associated with a risk of
rupture and ligation of the veins may result in the
obstruction of venous return in the brainstem and cere-
bellum, or possible congestive cerebral infarction. Our
nding that trigeminal neuralgia was not associated with
venous compression indicates that there might be no
requirement for special treatment of the veins, which may
reduce the risk for venous injury and venous return
obstruction. Since most arteries are tortuous, and their
stiffness increases with age, this increasing stiffness can
result in compression of the root of the trigeminal nerve,
leading to demyelination and subsequent trigeminal neu-
ralgia. On the contrary, veins do not bear high blood
pressure, their walls are thin, and their location is rela-
tively xed, and thus, veins tend not to become stiff and/or
tortuous with age and are therefore not likely to cause
compression of the nerve.
Conclusions
The ndings of this study indicate that compression of the
trigeminal nerve from veins was not a cause of trigeminal
neuralgia. These results indicate that while in patients with
arterial compression of nerve, complete decompression is
required and removal of adhesions is also necessary,
treatment of the vein may not need to be a priority when
performing microvascular dissection.
Conict of interest None.
Open Access This article is distributed under the terms of the
Creative Commons Attribution License which permits any use, dis-
tribution, and reproduction in any medium, provided the original
author(s) and the source are credited.
References
1. Tronnier VM, Rasche D, Hamer J, Kienle AL, Kunze S et al
(2001) Treatment of idiopathic trigeminal neuralgia: compariso-
nof long-term outcome after radiofrequency rhizotomy and
microvascular decompression. Neurosurgery 48:12611268
2. Kabatas S, Albayrak SB, Cansever T, Hepgul KT et al (2009)
Microvascular decompression as a surgical managementfor tri-
geminal neuralgia: a critical review of the literature. Neurol India
57:134138
3. Love S, Coakham HB (2001) Trigeminal neuralgia: pathology
and pathogenesis. Brain 124:23472360
4. Bennetto L, Patel NK, Fuller G (2007) Trigeminal neuralgia and
its management. BMJ 334:201205
5. Nurmikko TJ, Eldridge PR et al (2001) Trigeminal neuralgia
pathophysiology, diagnosis and current treatment. Br J Anaesth
87:117132
6. Dhople AA, Adams JR, Maggio WW, Naqvi SA, Regine WF,
Kwok Y et al (2009) Long-term outcomes of Gamma Knife
radiosurgery for classic trigeminal neuralgia: implications of
treatment and critical review of the literature. J Neurosurg
111:351358
7. Krafft RM (2008) Trigeminal neuralgia. Am Fam Physician
2008(77):12911296
8. Dandy WE (1934) Concerning the cause of trigeminal neuralgia.
Am J Surg 1934(24):447455
9. Lunsford LD, Apfelbaum RI et al (1985) Choice of surgical
therapeutic modalities for treatment of trigeminalneuralgia. Clin
Neurosurg 32:319333
10. Jia DZ, Li G et al (2010) Bioresonance hypothesis: a new
mechanism on the pathogenesis of trigeminal neuralgia. Med
Hypotheses 74:505507
11. Larsen A, Piepgras D, Chyatte D, Rizzolo D et al (2011) Tri-
geminal neuralgia: diagnosis and medical and surgical manage-
ment. JAAPA 24:2025
12. Sekula RF Jr, Frederickson AM, Jannetta PJ, Quigley MR, Aziz
KM, Arnone GD et al (2011) Microvascular decompression for
elderly patients with trigeminal neuralgia: a prospective study
and systematic review with meta-analysis. J Neurosurg
114:172179
13. Tucer B, Ekici MA, Demirel S, Basarslan SK, Koc RK, Guclu B
et al (2012) Microvascular decompression for primary trigeminal
neuralgia: short-term follow-up results and prognostic factors.
J Korean Neurosurg Soc 52:4247
14. Oesman C, Mooij JJ et al (2011) Long-term follow-up of
microvascular decompression for trigeminal neuralgia. Skull
Base 21:313322
15. Zhang H, Lei D, You C, Mao BY, Wu B, Fang Y (2012) The
long-term outcome predictors of pure microvascular decom-
pression for primary trigeminal neuralgia. World Neurosurg 2012
Jan 26. [Epub ahead of print]
16. Hong W, Zheng X, Wu Z, Li X, Wang X, Li Y, Zhang W, Zhong
J, Hua X, Li S et al (2011) Clinical features and surgical treat-
ment of trigeminal neuralgia caused solely by venous compres-
sion. Acta Neurochir (Wien) 153:10371042
17. Tomasello F, Alafaci C, Angileri FF, Calisto A, Salpietro FM
et al (2008) Clinical presentation of trigeminal neuralgia and the
rationale of microvascular decompression. Neurol Sci 29(Suppl
1):S191S195
18. Hyun SJ, Kong DS, Park K(2010) Microvascular decompression for
treating hemifacial spasm: lessons learned from a prospective study
of 1,174 operations. Neurosurg Rev 33:325334 discussion 334
19. Guclu B, Sindou M, Meyronet D, Streichenberger N, Simon E,
Mertens P et al (2011) Cranial nerve vascular compression
Neurol Sci (2014) 35:6166 65
1 3
syndromes of the trigeminal, facial and vago-glossopharyngeal
nerves: comparative anatomical study of the central myelin por-
tion and transitional zone; correlations with incidences of corre-
sponding hyperactive dysfunctional syndromes. Acta Neurochir
(Wien) 153:23652375
20. Luo DS, Zhang T, Zuo CX, Zuo ZF, Li H, Wu SX, Wang W, Li
YQ et al (2012) An animal model for trigeminal neuralgia by
compression of the trigeminal nerve root. Pain Physician
15:187196
21. Zhou Q, Liu ZL, Qu CC, Ni SL, Xue F, Zeng QS et al (2012)
Preoperative demonstration of neurovascular relationship in tri-
geminal neuralgia by using 3D FIESTA sequence. Magn Reson
Imaging 30:666671
22. Leal PR, Roch JA, Hermier M, Souza MA, Cristino-Filho G,
Sindou M et al (2011) Structural abnormalities of the trigem-
inal root revealed by diffusion tensor imaging in patients with
trigeminal neuralgia caused by neurovascular compression: a
prospective, double-blind, controlled study. Pain 152:2357
2364
23. Leal PR, Hermier M, Froment JC, Souza MA, Cristino-Filho G,
Sindou M et al (2010) Preoperative demonstration of the neuro-
vascular compression characteristics with special emphasis on the
degree of compression, using high-resolution magnetic resonance
imaging: a prospective study, with comparison to surgical nd-
ings, in 100 consecutive patients who underwent microvascular
decompression for trigeminal neuralgia. Acta Neurochir (Wien)
152:817825
24. Kakizawa Y, Seguchi T, Kodama K, Ogiwara T, Sasaki T, Goto
T, Hongo K et al (2008) Anatomical study of the trigeminal and
facial cranial nerves with the aid of 3.0-tesla magnetic resonance
imaging. J Neurosurg 108:483490
25. Zakrzewska JM, Coakham HB (2012) Microvascular decom-
pression for trigeminal neuralgia: update. Curr Opin Neurol
25:296301
66 Neurol Sci (2014) 35:6166
1 3
You might also like
- Intralipid infusion for Myelin Sheath Repair in Multiple Sclerosis and Trigeminal Neuralgia?From EverandIntralipid infusion for Myelin Sheath Repair in Multiple Sclerosis and Trigeminal Neuralgia?No ratings yet
- Trigeminal Nerve Pain: A Guide to Clinical ManagementFrom EverandTrigeminal Nerve Pain: A Guide to Clinical ManagementAlaa Abd-ElsayedNo ratings yet
- Xia 2014Document5 pagesXia 2014Akmal Niam FirdausiNo ratings yet
- Englot2011 PDFDocument6 pagesEnglot2011 PDFGaby JimenezNo ratings yet
- Neurosurg Focus Article PE13Document15 pagesNeurosurg Focus Article PE13Bunga AlifatulNo ratings yet
- 2009 8 Focus09158Document5 pages2009 8 Focus09158ninostranoNo ratings yet
- Long-Term Outcomes After Surgical Treatment of Pediatric Neurogenic Thoracic Outlet SyndromeDocument11 pagesLong-Term Outcomes After Surgical Treatment of Pediatric Neurogenic Thoracic Outlet Syndromewalter fire 0057No ratings yet
- Allam Anthony K Trigeminal NeuralgiaDocument15 pagesAllam Anthony K Trigeminal NeuralgiaAnonymous tG35SYROzENo ratings yet
- TMP E094Document7 pagesTMP E094FrontiersNo ratings yet
- (19330693 - Journal of Neurosurgery) Evaluation of Surgical Treatment For Neuropathic Pain From Neuroma in Patients With Injured Peripheral NervesDocument6 pages(19330693 - Journal of Neurosurgery) Evaluation of Surgical Treatment For Neuropathic Pain From Neuroma in Patients With Injured Peripheral NervesGeorgios StathisNo ratings yet
- Trigeminal Neuralgia. Diagnosis and Treatment. Allam AK, Sharma H, Larkin MB, Viswanathan ADocument15 pagesTrigeminal Neuralgia. Diagnosis and Treatment. Allam AK, Sharma H, Larkin MB, Viswanathan ANana ShkodinaNo ratings yet
- Journal NeuroDocument6 pagesJournal NeuroBetari DhiraNo ratings yet
- Hydrocephalus and Trigeminal Neuralgia: Exploring The Association and Management OptionsDocument5 pagesHydrocephalus and Trigeminal Neuralgia: Exploring The Association and Management Optionsakhmad ridhaniNo ratings yet
- Trigeminal NeuralgiaDocument6 pagesTrigeminal NeuralgiamimirkuNo ratings yet
- Controversies in The Neurosurgical Management of Cerebellar Hemorrhage and InfarctionDocument10 pagesControversies in The Neurosurgical Management of Cerebellar Hemorrhage and InfarctionThiago SouzaNo ratings yet
- Microvascular Decompression As A Surgical Management For Trigeminal Neuralgia: Long-Term Follow-Up and Review of The LiteratureDocument8 pagesMicrovascular Decompression As A Surgical Management For Trigeminal Neuralgia: Long-Term Follow-Up and Review of The LiteratureAkmal Niam FirdausiNo ratings yet
- P ('t':'3', 'I':'669304988') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document6 pagesP ('t':'3', 'I':'669304988') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ferry PrawiraNo ratings yet
- Trigeminal NeuralgiaDocument3 pagesTrigeminal NeuralgiaPao JeyNo ratings yet
- Jurnal Cts 2Document10 pagesJurnal Cts 2Muhammad Hanafi QNo ratings yet
- Tratamiento Quirúrgico Efectivo de Las Malformaciones Cavernosas Cerebrales - Un Estudio Multicéntrico de 79 Pacientes PediátricosDocument4 pagesTratamiento Quirúrgico Efectivo de Las Malformaciones Cavernosas Cerebrales - Un Estudio Multicéntrico de 79 Pacientes PediátricosGonzalo Leonidas Rojas DelgadoNo ratings yet
- Advances in Diagnosis, Classification, Pathophysiology and Mannagement of Trigeminal Neuralgia PDFDocument13 pagesAdvances in Diagnosis, Classification, Pathophysiology and Mannagement of Trigeminal Neuralgia PDFSergio A SalgadoNo ratings yet
- Acc 61 - Supp2 96Document7 pagesAcc 61 - Supp2 96intermediosamberesNo ratings yet
- Alça VascularDocument10 pagesAlça Vascularceciliatigre10No ratings yet
- PIIS1526590013009358Document8 pagesPIIS1526590013009358intermediosamberesNo ratings yet
- Clinical Neurology and Neurosurgery: SciencedirectDocument7 pagesClinical Neurology and Neurosurgery: SciencedirectMella WarizkaNo ratings yet
- Management of Trigeminal Neuralgia. A Comparison of Two TechniquesDocument20 pagesManagement of Trigeminal Neuralgia. A Comparison of Two TechniquesAbhikNo ratings yet
- Nerve Entrapment - UpdateDocument17 pagesNerve Entrapment - UpdatealobrienNo ratings yet
- Management of NeuralgiaDocument2 pagesManagement of NeuralgiaNeivashini MaDhavanNo ratings yet
- Idiopatic SyringomyeliaDocument9 pagesIdiopatic SyringomyeliaIrenaNo ratings yet
- Pathophysiology, Causes, and Differential Diagnosis: Multiple SclerosisDocument4 pagesPathophysiology, Causes, and Differential Diagnosis: Multiple SclerosisjaideepbaggaNo ratings yet
- Rodriguez2005-Cognitive Dysfunction After Total Knee Arthroplasty - Effects of Intraoperative Cerebral Embolization and Postoperative ComplicationsDocument9 pagesRodriguez2005-Cognitive Dysfunction After Total Knee Arthroplasty - Effects of Intraoperative Cerebral Embolization and Postoperative ComplicationsSyahpikal SahanaNo ratings yet
- Peripheralneuromodulation Fortreatmentofchronic MigraineheadacheDocument4 pagesPeripheralneuromodulation Fortreatmentofchronic MigraineheadacheCorin Boice TelloNo ratings yet
- Occipital Nerve Blockade in Chronic ClusterDocument9 pagesOccipital Nerve Blockade in Chronic ClusterToni DNo ratings yet
- (10920684 - Neurosurgical Focus) Neurogenic Thoracic Outlet Syndrome - Current Diagnostic Criteria and Advances in MRI DiagnosticsDocument5 pages(10920684 - Neurosurgical Focus) Neurogenic Thoracic Outlet Syndrome - Current Diagnostic Criteria and Advances in MRI DiagnosticsGeorgios StathisNo ratings yet
- 2008 Trigeminal NeuralgiaDocument6 pages2008 Trigeminal NeuralgiaApril Rose Airoso - AramburoNo ratings yet
- In-Hospital Stroke Recurrence and Stroke After Transient Ischemic AttackDocument15 pagesIn-Hospital Stroke Recurrence and Stroke After Transient Ischemic AttackferrevNo ratings yet
- Mechanical Thrombectomy in Stroke: MedicineDocument8 pagesMechanical Thrombectomy in Stroke: MedicineSebastian RiveroNo ratings yet
- Thrombolysis With Alteplase 3 To 4.5 Hours After Acute Ischemic StrokeDocument13 pagesThrombolysis With Alteplase 3 To 4.5 Hours After Acute Ischemic StrokeParvathy R NairNo ratings yet
- Endovascular Treatment of Intracranial Aneurysms: Initial Experience in A Low-Volume CenterDocument5 pagesEndovascular Treatment of Intracranial Aneurysms: Initial Experience in A Low-Volume CenterAswin ChristantoNo ratings yet
- NeuralRegenRes114559-8526593 234105Document2 pagesNeuralRegenRes114559-8526593 234105JouleAlSBNo ratings yet
- The Neurology of Eclampsia: Some Observations: Views and ReviewsDocument8 pagesThe Neurology of Eclampsia: Some Observations: Views and ReviewsFajar Rudy QimindraNo ratings yet
- Trigeminal Neuralgia PDFDocument4 pagesTrigeminal Neuralgia PDFCHenyLeeNo ratings yet
- Nejmoa 2310392Document11 pagesNejmoa 2310392ENRIQUEFREDNo ratings yet
- Chest Wall, Pneumothorax, and Hemothorax: Brain DeathDocument5 pagesChest Wall, Pneumothorax, and Hemothorax: Brain DeathMelly SyafridaNo ratings yet
- SaudiMedJ 36 1363Document4 pagesSaudiMedJ 36 1363Lý TưởngNo ratings yet
- Characterization of The Spectrum of Hemodynamic Profiles in Trauma Patients With Acute Neurogenic ShockDocument5 pagesCharacterization of The Spectrum of Hemodynamic Profiles in Trauma Patients With Acute Neurogenic Shockzefri suhendarNo ratings yet
- 2017 Article 1793Document5 pages2017 Article 1793annisaNo ratings yet
- Kakizawa 2008Document8 pagesKakizawa 2008Vasantha RajanNo ratings yet
- ASRA GuidelinesDocument26 pagesASRA GuidelinesAzam DanishNo ratings yet
- Ekim, H. y Tuncer, M. (2009) - Manejo de Lesiones Traumáticas de La Arteria Braquial Informe de 49 PacientesDocument5 pagesEkim, H. y Tuncer, M. (2009) - Manejo de Lesiones Traumáticas de La Arteria Braquial Informe de 49 PacientesEdgar Geovanny Cardenas FigueroaNo ratings yet
- Cervical InjuryDocument9 pagesCervical Injurypmahi8854No ratings yet
- Estenosis Traqueal ComplejaDocument8 pagesEstenosis Traqueal ComplejaFabiolaNo ratings yet
- Wilhour-Nahas2018 Article The NeuralgiasDocument8 pagesWilhour-Nahas2018 Article The NeuralgiasCamilo Benavides BurbanoNo ratings yet
- J JCRC 2013 11 018Document5 pagesJ JCRC 2013 11 018Andres Rojas JerezNo ratings yet
- Surveillance IchDocument6 pagesSurveillance IchGabriel Septiana CitraNo ratings yet
- Yang 2014Document4 pagesYang 2014Akmal Niam FirdausiNo ratings yet
- Hemorragia Intracerebral No TraumaticaDocument3 pagesHemorragia Intracerebral No TraumaticaSara CNo ratings yet
- Journal ReadingDocument53 pagesJournal ReadingRhadezahara PatrisaNo ratings yet
- Carotid Endarterectomy: Experience in 8743 Cases.Document13 pagesCarotid Endarterectomy: Experience in 8743 Cases.Alexandre Campos Moraes AmatoNo ratings yet
- Consult Labelling Cough Cold 091022 ReviewDocument27 pagesConsult Labelling Cough Cold 091022 ReviewTejo PramonoNo ratings yet
- 2010 Article 198Document6 pages2010 Article 198Tejo PramonoNo ratings yet
- Vesikel Trafik - KBK RahmanDocument14 pagesVesikel Trafik - KBK RahmanTejo PramonoNo ratings yet
- 0030207Document6 pages0030207Tejo PramonoNo ratings yet
- Pain in Trigeminal Neuralgia: Neurophysiology and Measurement: A Comprehensive ReviewDocument6 pagesPain in Trigeminal Neuralgia: Neurophysiology and Measurement: A Comprehensive ReviewTejo PramonoNo ratings yet
- Resis MalariaDocument22 pagesResis MalariaTejo PramonoNo ratings yet
- HMT RM65 Radial DrillDocument2 pagesHMT RM65 Radial Drillsomnath213No ratings yet
- Lc420euf Sda1 LGDocument41 pagesLc420euf Sda1 LGjavierNo ratings yet
- LPG GasDocument39 pagesLPG Gasv prasanthNo ratings yet
- Ecotopia Remixed II-FormattedDocument54 pagesEcotopia Remixed II-FormattedthisisdarrenNo ratings yet
- Michelle LeBaron, Venashri - Pillay) Conflict AcrosDocument241 pagesMichelle LeBaron, Venashri - Pillay) Conflict AcrosBader100% (2)
- 40 RT-flex Control-System Rev01Document68 pages40 RT-flex Control-System Rev01Mayvon Botelho100% (2)
- Simple Roll-Type: A Loud SpeakerDocument1 pageSimple Roll-Type: A Loud SpeakerEudes SilvaNo ratings yet
- Latihan To: Nilai: 7.4 Benar: 37 Salah: 13Document17 pagesLatihan To: Nilai: 7.4 Benar: 37 Salah: 13glensNo ratings yet
- Motor CAT C13 AcertDocument3 pagesMotor CAT C13 AcertJosé Gonzalez100% (4)
- How To Eat WellDocument68 pagesHow To Eat WelleledidiNo ratings yet
- Tabel Gsi, RMR, RmiDocument4 pagesTabel Gsi, RMR, RmiPup BooNo ratings yet
- Generalized Anxiety DisorderDocument24 pagesGeneralized Anxiety DisorderEula Angelica OcoNo ratings yet
- Arts6,4, Week2, Module 2V4Document24 pagesArts6,4, Week2, Module 2V4Loreen Pearl MarlaNo ratings yet
- ST 36Document4 pagesST 36ray72roNo ratings yet
- Guidelines For The Management of Brain InjuryDocument26 pagesGuidelines For The Management of Brain InjuryfathaNo ratings yet
- Aircraft Design Course PhillStocking 4.2Document48 pagesAircraft Design Course PhillStocking 4.2ugurugur1982No ratings yet
- Paranoia XP - Gamemaster Screen Booklet - Mandatory Fun Enforcement PackDocument24 pagesParanoia XP - Gamemaster Screen Booklet - Mandatory Fun Enforcement PackStBash100% (3)
- Academic Reading: All Answers Must Be Written On The Answer SheetDocument21 pagesAcademic Reading: All Answers Must Be Written On The Answer SheetLemon MahamudNo ratings yet
- Chennai To Vishakhapatnam El6Vvd: Indigo 6E-6835Document3 pagesChennai To Vishakhapatnam El6Vvd: Indigo 6E-6835VENKATESH POONDRUNo ratings yet
- ZhentarimDocument4 pagesZhentarimLeonartNo ratings yet
- Book BindingDocument14 pagesBook Bindingpesticu100% (2)
- Statistics and Probability Module 3Document3 pagesStatistics and Probability Module 3Eftychia LeegleeNo ratings yet
- All Pop SongsDocument53 pagesAll Pop SongsMadeleneQuiogueNo ratings yet
- Rac Question PaperDocument84 pagesRac Question PaperibrahimNo ratings yet
- Index PDFDocument159 pagesIndex PDFHüseyin IşlakNo ratings yet
- MiscanthusDocument27 pagesMiscanthusJacob GuerraNo ratings yet
- Sheet Metal Manufacturing Companies NoidaDocument9 pagesSheet Metal Manufacturing Companies NoidaAmanda HoldenNo ratings yet
- Tesla Magazine Vol4Document48 pagesTesla Magazine Vol4jonathan100% (1)
- Bhagwati School Strap Report AnalysisDocument60 pagesBhagwati School Strap Report AnalysisReverse Minded100% (1)