Professional Documents
Culture Documents
Double-Blind Randomized Study Comparing Brand-Name and Generic Phenytoin Monotherapy
Uploaded by
Sergio Guadalupe Dévora Ramírez0 ratings0% found this document useful (0 votes)
24 views7 pagesArticulo de investigacion
Original Title
Articulo 01
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentArticulo de investigacion
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
24 views7 pagesDouble-Blind Randomized Study Comparing Brand-Name and Generic Phenytoin Monotherapy
Uploaded by
Sergio Guadalupe Dévora RamírezArticulo de investigacion
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 7
Epilepsia, 33(2):359-365, 1992
Raven Press, Ltd., New York
0 International League Against Epilepsy
Double-Blind Randomized Study Comparing Brand-Name
and Generic Phenytoin Monotherapy
Mohamad Mikati, Nancy Bassett, and Steven Schachter
Department of Neurology, Childrens Hospital, Harvard Medical School, Boston, Massachusetts, U. S. A
Summary: Ten patients with well-controlled seizures re-
ceiving chronic phenytoin (PHT) monotherapy for sei-
zure prophylaxis completed a randomized double-blind
crossover study comparing brand-name and generic PHT.
Each patient received the same dose of each preparation
for 3 months during which trough PHT concentrations
and adverse effects were monitored. The average predose
steady-state total PHT concentration was 11.9 ? 4.9 pg/
ml during brand-name therapy and 14.2 % 8.2 pg/ml dur-
ing generic therapy. The average predose steady-state
free PHT concentrations were 0.93 2 0.47 pg/ml (brand
name) and 1.14 ? 0.64 pg/ml (generic), respectively (p <
0.005). The potency (capsule content) values for the lots
used in the study were 99.2% for the brand-name and
104.6% for generic. Because of the nonlinear Michaelis-
Menten kinetics of PHT, a 5.4% difference in potency
could account for the observed differences in plasma con-
centrations. When compared with brand-name PHT ther-
apy, the generic drug was associated with an increase in
serum concentration. This increase was consistent with
the reported difference in capsule content between the
generic and brand-name lots used in this study. Key
Words: Anticonvulsants-Phenytoin-Nonlinear phar-
macokinetics-Therapeutic equivalency-Capsules-
Generic drugs.
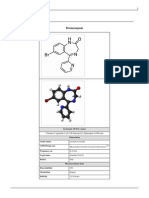
Phenytoin (PHT) is a useful first-line antiepileptic
drug (AED) for the treatment of partial and gener-
alized seizures. PHT manifests dose-dependent ki-
netics. At low plasma PHT concentrations, elimi-
nation half-life is 16-24 h. At therapeutic concen-
trations, PHT disappears at a slower rate, with a
half-life of up to 42 h. After i.v. infusions of 15-18
mg/kg (which generally produce therapeutic levels),
PHT half-life varies from 10 to 160 h. A patient
manifesting a half-life of 160 h (-1 week) is not
expected to achieve steady-state before five half-
lives, or 5 weeks, after onset of therapy (Wood-
bury, 1989).
There are numerous reports of therapeutically in-
equivalent PHT products. In many cases these
products have resulted in alterations in serum con-
centrations with or without associated clinical prob-
lems (Balla, 1968; Rail, 1968; Tyrer et al., 1970;
Melikian et al., 1977; Sawchuk et al., 1982a,b;
Rosenbaum, 1988). To avoid such complications
the U.S. Food and Drug Administration has devel-
Received June 1990; revision accepted February 1991.
Address correspondence and reprint requests to Dr. M. Mikati
at Childrens Hospital, Division of Clinical Neurophysiology,
300 Longwood Avenue, Boston, Massachusetts 021 15, U.S.A.
oped criteria that allow for only minimal differences
in bioavailability for products that are passed as
bioequivalent. In addition, United States Pharma-
copeia (USP) criteria allow for some variation (93-
107%) in capsule content (potency). Because of the
nonlinear kinetics manifested by PHT, small differ-
ences in the amount absorbed could theoretically
result in larger changes in serum concentrations in
patients who have changed from one PHT prepara-
tion to another. The role that variation in capsule
content may play in generic substitution of PHT
during chronic monotherapy for seizures has not
been studied.
A double-blind crossover study comparing the se-
rum concentrations and the adverse effects in pa-
tients during long-term monotherapy with generic
and brand-name PHT has not been performed.
The goal of this study was to investigate these
issues in patients receiving chronic PHT monother-
aPY *
MATERIALS AND METHODS
Study design
This was a 6-month double-blind randomized
crossover study comparing two extended-release
PHT preparations: a generic one (Phenytex) and the
3.59
360 M. MIKATI ET AL.
brand-name product (Dilantin). Phenytex is a ge-
neric PHT preparation that until recently was con-
sidered as bioequivalent to Dilantin. Each patient
was randomly assigned to one preparation, and af-
ter 3 months changed to the same dose of the alter-
native preparation. The protocol received Institu-
tional Review Board approval.
Test medications
Generic and brand-name 100-mg PHT capsules
were used. Each was enclosed in a number-zero
identically looking opaque gelatin capsule that com-
pletely obscured the preparation. The research
pharmacist dispensed a 1-month supply. The num-
ber of pills dispensed and returned was verified and
recorded at each visit by the research nurse and the
pharmacist. A separate sealed bottle with an emer-
gency supply was given at each visit and returned
on the subsequent visit.
Patients
Thirteen patients (seven male, six female) were
randomized and received at least one PHT prepa-
ration. All fulfilled the following criteria: (a) Adults
(ages 18-60 years) who were receiving PHT mono-
therapy for seizure prophylaxis. All had suffered
from prior seizures except one, who was receiving
PHT prophylaxis after intracranial surgery. All
other patients had had either partial or generalized
seizures necessitating PHT monotherapy as judged
by their referring physicians. All had had an EEG
within the 2 years preceding enrollment in the
study. None was receiving any other chronic med-
ication except for one postmenopausal woman who
was receiving a chronic constant dose of Premarin
(1.25 mg/day). This was maintained at the same
dose throughout the study. (b) Patients judged to
have poor compliance were excluded. None of the
patients had significant cardiovascular, gastrointes-
tinal, hematologic, hepatic, renal, or psychiatric
disease or alcohol or drug abuse. Patients judged to
be unreliable in reporting the necessary informa-
tion, side effects, or seizures were not enrolled. Pa-
tients with significant abnormalities in liver function
or blood count were also not enrolled. If a patient
developed any potentially interfering condition (like
infections requiring antibiotic therapy during the
study) enrollment was terminated.
Procedures
At the screening visit the patients inclusion and
exclusion criteria were reviewed, and the patient
was informed about the study. In many cases sev-
eral screening visits were conducted to establish the
reliability and compliance of the patient. At the first
study visit, the patient signed an informed consent,
the history was reviewed, and full physical and neu-
rological examinations were done. At that time the
patient was randomized to treatment with either
brand-name or generic PHT therapy. The random-
ization code was kept by the research pharmacist
(with 24-h coverage), and was not available to the
investigators or to the patients. During this first
visit seizure frequency and adverse effects were re-
viewed and recorded. Blood studies, including he-
matology, liver function, and free and total PHT
concentrations were obtained. The patient was dis-
pensed a months supply of the study medication in
a double-blind fashion. Patients were instructed to
take the medication always at exactly the specified
time throughout the study (every 12 h for some pa-
tients and every 24 h for others). Patients also al-
ways recorded the exact time (hour and minute) of
their intake of the last PHT dose received before a
scheduled visit. All visits were scheduled at the
same time of the day. PHT concentrations were al-
ways drawn within l h of intake of the next dose.
Patients were seen monthly and were telephoned
frequently in between (as needed) to ensure com-
pliance. At each visit compliance was verified by
pill count, careful interviews, and reviewing seizure
frequency and adverse effect diaries. During the
study patients kept daily records of seizure fre-
quency and of any potential adverse effects they
may have developed. The number, severity, dura-
tion, and type of seizures and adverse effects were
reviewed and verified during each monthly visit,
and evidence for neurotoxicity was examined by
the following tests: finger-nose-finger, heel-knee-
shin, gait, tandem gait, Romberg, and nystagmus.
Free and total plasma PHT levels were obtained at
each visit, and PHT was dispensed in the same fash-
ion as at the initial visit. On the fourth visit (end of
month 3), the patient was changed to the same dose
of the alternative preparation. Blood studies were
repeated during the fourth visit and during the last
visit at the conclusion of the study. Complete phys-
ical and neurological examinations were also re-
peated during the last visit.
Total PHT assay methodology (enzyme-multi-
plied immunoassay technique) coefficient of varia-
tion was <lo%, while that of free PHT [high-
performance liquid chromatography (HPLC) ul-
trafiltration] was 68%.
RESULTS
Serum concentrations
The average daily PHT dose was 4.58 mg/kg
(range, 2.86-5.35 mglkg). Ten of our patients com-
Epi l epsi a, Vol. 33, No. 2, 1992
GENERIC SUBSTITUTION OF PHENYTOIN 361
pleted both arms of the study (generic and brand-
name). The other three could not complete the
study because of adverse experiences necessitating
introduction of new AEDs and/or change in therapy
(Table 1). None of these adverse experiences could
be attributed to changes in PHT concentrations (see
Table 1 for details).
Because the mean total and free PHT levels are
not normally distributed and because the t test as-
sumes normal distribution, we also performed the
Wilcoxon signed rank test. This test is based on the
ordinal scale of measurement and does not assume
normal distribution of the data. The results showed
agreement between analyses performed by the t test
and the Wilcoxon signed rank test.
Because serum concentrations can be altered by
changes in body weight, the level/dose ratio was
used as our primary parameter of analysis (Table 2).
Only very minimal changes in weight were ob-
served during this study.
level/dose ratio =
average predose steady-state concentration
dose
The dose was the total daily dose (in mg/kg/day).
The average predose steady-state concentration
(p,g/ml) was the average trough concentration of
months 2 and 3 (for one preparation) and of months
5 and 6 (for the other preparation). Months 1 and 4
concentrations were excluded because steady-state
levels may not have been achieved at that time (see
introductory statement). The only exception was
patient 10, who could not receive the same dose of
generic PHT because of development of symptoms
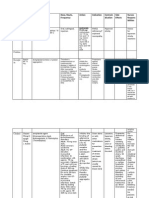
TABLE 1. Patients who could not complete 6 months
of the study because of an adverse experience
Adverse
Patient Month Preparation experience
11 1 Brand namea,' Worse seizures
1 1 1 Generic"," Worse seizures
12 4 Generic'," Worse seizures
13 4.5 Brand name Allergic rash
a Worsening of seizure control could not be attributed to a
change in phenytoin (PHT) levels (see below).
' The trough PHT concentration was 6 Fg/ml in baseline. It
was 8. 3 p.g/rnl during month 1 when the patient suddenly devel-
oped poor (complex partial) seizure control.
Patient 11 was reenrolled after the dose was increased and
after stabilizing with excellent seizure control for 2.5 months.
Trough PHT level was 9 p.g/ml at the time of worsening of sei-
zures.
Trough PHT concentrations were remarkably stable at 6, 6 ,
6 , 6 , 6 , p.g/ml at baseline, months 1, 2, 3, and 4, respectively. The
increased seizure frequency was thus thought to be independent
of the PHT preparation.
of toxicity with high serum concentrations 2 weeks
after being changed to generic therapy. Thus this
patient's PHT concentration, obtained after 2
weeks of generic therapy, was used as an approxi-
mation of steady-state concentration. This concen-
tration probably underestimated steady-state con-
centration and biased the analysis toward not find-
ing a difference between the two preparations.
The average predose free PHT concentration dur-
ing brand-name therapy was 0.93 k 0.48 pg/ml, and
during generic therapy 1.14 ? 0.64 p,g/ml. Each of
the nine patients showed a higher average free PHT
Concentration during generic therapy (Table 2). The
difference was statistically significant (two-sided
paired t test, p <0.01; Wilcoxon rank sum test, p <
0.005).
The average predose total PHT concentration
during brand-name therapy was 11.9 ? 4.9 pglml,
and during generic 14.2 2 8.2 pg/ml. The difference
approached but did not achieve statistical signifi-
cance (0.05 <p <0.1 for two-sided paired t test and
Wilcoxon rank sum test).
Adverse experiences
The most common adverse experiences observed
in the 10 patients completing both arms of the study
included headaches, gastrointestinal upset, fatigue,
dizziness, and lethargy. With one exception, these
experiences were mild, transient, tolerable, and in
most cases the relationship to PHT therapy was not
definite. The incidence of each of these adverse ex-
periences was not statistically different between the
two preparations (McNemar test, p >0.25). One
patient (lo), a 27-year-old woman, developed intol-
erable adverse effects after changing from brand-
name to generic therapy. During the first phase of
the study this patient received 300 mg of brand-
name PHT per day, which she tolerated very well
despite an average predose steady-state concentra-
tion of 20.5 pg/ml. Twelve days after changing to
the generic preparation (same daily dose), she noted
the gradual onset of difficulty in concentration,
headaches, ataxia, diplopia, and progressive som-
nolence. Thirty-six hours later, her symptoms were
more severe and her serum PHT concentration was
30.2 pg/ml. PHT was stopped. Two days later PHT
concentration dropped to 25.9 p,g/ml and symptoms
gradually subsided. Three days later 200 mglday ge-
neric preparation was started. Subsequent PHT se-
rum concentrations were 8.0, 7.0, and 7.0 p,g/ml at
months 4, 5 , and 6 of the study.
The results of the laboratory tests during therapy
with each preparation are summarized in Table 3.
There were no statistically significant differences
Epilepsia, Vol. 33, No. 2 , 1992
362 M. MI KATI ET AL.
TABLE 2. Phenytoin ( PHT) serum concentration to dose rati osU
Total Free
Change Dilantin Generic Change Dilantin Generic
1 1.45 1.84 0.39 0.127 0.151 0.024
2 4.22 4.82 0.60 0.343 0.408 0.065
3 1.69 I .91 0.22 0.125 0.139 0.014
4 3.43 4.36 0.93 0.284 0.388 0.104
5 1.53 2.01 0.48 0.117 0.139 0.022
6 3.56 4.98 1.42 0.465 0.572 0.107
7 2.56 2.08 - 0.48 0.185 0.244 0.059
8 1.99 1.65 - 0.34 0.140 0.158 0.018
9 1.41 1.24 - 0.17 0.102 0.116 0.014
10300 3.79 5.75 1.96 (0.370) NA -
1020Ob
- (1.96) - - (0.122) -
Mean 2.56 3.06 0.501 0.210 0.257 0.0474
SD 1.09 1.70 0.773 0.127 0.161 0.0379
The numbers in parentheses were not used in calculating the mean and SD values.
NA, not available.
Concentration to dose ratio =Concentration (pg/ml)/Dose (mg/kg/day).
Patient 10 was initially started with 300 mg/day of brand-name PHT (300). Upon being changed to generic PHT the patient developed
toxic concentrations and the dose had to be decreased to 200 mg/day (200).
between the laboratory values with either prepara-
tion (paired t test, p >0.05).
Seizure frequency
Daily seizure records were kept by all patients.
Most of the patients were very well controlled, and
eight of ten completing both arms of the study were
seizure-free. Thus, the number of patients and their
low seizure frequency do not allow for any mean-
ingful comparison of efficacy.
DISCUSSION
Interpretation of the data
We observed a statistically significant difference
in the free PHT concentration between the two
preparations. The average predose free steady-state
PHT concentration was 22.6% higher during ge-
neric than during brand-name therapy (0.93 vs. 1.14
kg/ml). The difference between the total PHT con-
centrations approached but did not achieve statisti-
cal significance. The average predose steady-state
TABLE 3. Blood studies
Dilantin Generic
Hgb (gm/dl) 14.3 f 1.5 14.2 f 1.2
WBC (103/mm3) 7.9 f 3.0 7.2 % 2.5
Bilirubin (mg/dl) 0.2 ? 0.08 0.24 f 0.05
SGOT (U/L) 21 f 14 25 f 9
Alkaline phosphatase (U/L) 100 f 87 115 f 80
SGPT (U/L) 34 f 22 34 f 21
GGT (U/L) 88 f 71 112 f 73
Hgb, hemoglobin; WBC, white blood cells; SGOT, serum glu-
tamic oxaloacetic transaminase; SGPT, serum glutamic pyruvic
transaminase; GGT, gamma-glutamyl transpeptidase.
PHT total concentration was 19.3% higher during
generic than during brand-name therapy (1 1.9 vs.
14.2 pg/ml).
There are four possible explanations for our find-
ings: (a) There is increased bioavailability and/or
capsule content of generic as compared to brand-
name PHT and the number of patients studied was
large enough to detect differences in the free levels
but not in the total levels. (b) There is less protein
binding of PHT during generic therapy. (c) There is
a decrease in PHT clearance during generic ther-
apy. (d) There is a systematic confounding variable
affecting PHT levels obtained under each prepara-
tion (e.g., more intake of medication during the ge-
neric phase of the study).
We favor the first explanation because: (a) there
were no differences between albumin and protein
levels with either preparation; (b) it is biologically
impossible for a change in clearance or protein
binding to result from a change in preparation; (c)
our study was double-blind and randomized; and (d)
there are multiple factors biasing our data toward
not detecting differences that may actually exist.
These factors appear to have affected the total con-
centration more than the free concentration (see be-
low).
Factors in our study that make it more difficult to
detect real differences between the two prepara-
tions include: (a) Interindividual variability in drug
clearance. (b) Day-to-day variability in PHT assays.
This variability was higher for the total PHT assay
than for the free fraction assay (610 vs. =3%). (c)
Interpatient variability of protein binding and albu-
min concentrations. (d) Steady-state concentrations
Epi l epsi a, Vol. 33, No. 2, 1992
GENERIC SUBSTITUTION OF PHENYTOIN 363
were probably not achieved by the one patient (10)
who manifested the largest increase in concentra-
tion upon changing from brand-name to generic
PHT. Thus in this patient the concentration used for
generic PHT was an underestimate of the real
steady-state concentration. (e) A relatively small
number of patients.
These factors result in underestimating the mag-
nitude of the observed concentration increases dur-
ing generic PHT therapy and/or in increasing the
standard deviation of the data. This is particularly
true for the total PHT concentrations, where the
standard deviatiodmean ratio is 0.773/0.501 =1.54
(Table 2). This ratio for free PHT concentrations
was 0.0379/0.0474 or 0.80 (Table 2). Power calcula-
tions (Zar, 1984) show that, given the standard de-
viation of our data, -20 patients are needed to de-
tect a mean increase of 20% in total PHT concen-
tration (a = 0.05, p =0.1). To detect a 20%
increase in free PHT concentration (a =0.05, p =
0.1) only nine patients are needed. Having studied
10 patients, we were thus able to detect statistically
significant differences in the free levels, but the
number of our patients was not sufficient to detect
differences that probably also existed in the total
concentrations.
Potency (capsule content) analyses were per-
formed using an HPLC technique with ultraviolet
light detection based on the USP XXII procedures.
The potency of the brand-name lot was 99.21% ?
1.47, and that of the generic preparation was
104.63% +3.72. Because of the nonlinear Michae-
lis-Menten PHT pharmacokinetics, a difference of
5.4% in the amount absorbed can account for a 20%
difference in serum concentrations (see calculations
below).
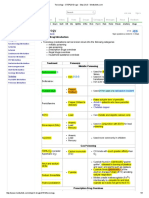
By using the published adult mean K, and V,
values (Browne et al., 1985) and the mean steady-
state concentrations achieved on each preparation
in the group of patients we studied, the observed
relative genericbrand-name dosing rate ratio can be
calculated using the following formula (Shargel and
Yu, 1985):
V", * c2
_ - R2 Km+c2
R1 vnl. c2
KIn +c1
-
where R, is the dosing rate with generic PHT; C, is
the steady-state concentration with generic PHT
(14.2 pg/ml); V, (the maximum rate of metabolism
of PHT) =487 mg/day (Browne et al., 1985); K,
(the plasma concentrations at which the metabolic
rate is one-half the maximum) =4.3 pg/ml (Browne
et al., 1985); R, is the dosing rate with brand-name
PHT; and C, is the steady-state concentration with
brand-name PHT (1 I .9 pgfml).
This formula gives an observed R,/R, ratio of
1.046. This is remarkably similar to the predicted
R,/R, value of 1.04610.992 =1.054. Thus, the most
likely explanation for our findings is the presence of
differences in capsule content between the two
preparations studied.
We must point out the limitations of our method-
ology. There was variability in the assays of free
and total PHT Concentrations. Although we took
extra care to achieve and check for compliance with
repeated pill counts and careful records, these out-
patient methods do not ensure complete compliance
(Pullar et al., 1989; Rudd et al., 1989). Hence, in any
one of our patients, including the one who devel-
oped toxic concentrations, we cannot absolutely
rule out an undetected confounding variable, for ex-
ample, an unrecognized change in compliance.
Confounding variables, however, would not ac-
count for statistically significant differences unless
those variables were systematically associated with
one preparation (Osorio and Reed, 1988). This pos-
sibility can be eliminated because our study was
double-blind and randomized.
Review of the literature and significance of
the study
Differences in serum concentrations and/or pa-
tient response upon nonequivalent preparation sub-
stitution have been reported for carbamazepine
(Koch and Allen, 1987; Sachdeo, 1987), valproate
(MacDonald, 1987), and PHT (Balla, 1968; Eadie et
al., 1968; Tyrer et al., 1970). The FDA criteria for
bioequivalence (Federal Register 1977) allow for a
+20% difference in bioavailability between generic
and brand-name products. In addition, USP criteria
specify that capsule content should be within +7%
(93-107%) of the stated content (100 mg in the case
of the studied PHT capsules). Thus, certain differ-
ences (albeit small) are allowable in products that
are considered bioequivalent. Such differences may
be particularly important in medications that mani-
fest nonlinear kinetics, particularly in patients who
happen to be on the nonlinear portions of their
dose-concentration curves.
Studies to establish bioequivalence are per-
formed on healthy volunteers, and thus may not
account for the full pharmacologic and therapeutic
impact of generic substitution. Physicians consider-
ing generic substitution should consider several fac-
tors: (a) the risk that such a substitution could result
Epilepsiu, Vol. 33, No. 2, 1992
364 M. MIKATI ET AL.
in a change in serum concentration; (b) the risk that
such a change, if it occurs, may lead to significant
adverse effects or loss of efficacy; (c) the cost of
generic versus brand-name therapy; (d) the cost of
blood tests necessary to ensure that the new con-
centrations are adequate; (e) the cost of time and
effort spent in adjusting the dose (if needed); (0 the
risk that patients may receive different generics
each time they refill the prescription; (8) the effect
generic substitution may have on patient compli-
ance; and (h) patient motivation and interest in re-
ceiving a generic preparation.
Our study was designed to address several of
these issues. Its advantages were as follows: (a) The
protocol was double-blind and randomized. (b) We
took extra care to control potential confounding
variables. We believe that the fact we were able to
demonstrate statistically significant differences
while studying a relatively small number of patients
is due, at least in part, to a favorable degree of
control of confounding variables. (c) Our findings
have direct relevance to daily clinical practice be-
cause we studied patients receiving chronic mono-
therapy. (d) When adverse effects or changes in sei-
zure frequency occurred they were managed ac-
cording to guidelines based on standard clinical
practice. (e) We followed patients for 3 months with
each preparation and excluded the concentrations
from months one and four to exclude a sequence
effect.
We conclude that generic substitution of PHT can
be associated with increases in PHT serum concen-
trations. In our experience, these increases were
asymptomatic in nine of ten patients, but were as-
sociated with intolerable dose-dependent adverse
effects in the tenth. Such increases may be even
more important if there is increased interlot vari-
ability in capsule content of generic preparations or
if there is increased intergeneric variability as com-
pared to the interlot variability of the brand-name
product. Prior studies have emphasized the role of
differences in bioavailability in producing differ-
ences in serum concentrations between brand-name
and generic preparations. The potential role of cap-
sule content (potency) has been largely ignored.
Out study indicates that variability in capsule con-
tent may be an important factor to be considered
during generic substitution of medications that, like
PHT, manifest nonlinear pharmacokinetics.
Acknowledgment: We thank Dr. Douglas R. Flanagan
for performing capsule content analyses, Dr. David Grun-
blatt for his advice, and Ms. Tracey Thomas for technical
assistance.
REFERENCES
Balla J . Dilantin overdosage. Med J Aust 1968;2:480-1.
Browne TR, Evans J E, Szabo GK, Evans BA, Greenblatt DJ ,
Schumacher GE. Studies with stable isotopes. I: Changes in
phenytoin pharmacokinetics and biotransformation during
monotherapy . J Clin Pharmacol 1985;25:43-50.
Eadie MJ , Sutherland J M, Tyrer J H. Dilantin overdosage. Med
J Aust 1968;2:515.
Department of Health, Education and Welfare, Food and Drug
Administration. Certain anticonvulsants. Proposed bioequiv-
alence requirements. [21CFR Part 320.1 Federal Register
I977 ;42: 39675-9.
Koch G, Allen J P. Untoward effects of generic carbamazepine
therapy. Arch Neurol 1987;44:578-9.
MacDonald J T. Breakthrough seizures following substitution of
Depakene (Abbott) with a generic. Neurology 1987;37: 1885.
Melikian AP, Straughn AB, Slywka GWA, Whyatt PL, Meyer
MC. Bioavailability of 1 1 phenytoin products. J Pharmaco-
kinet Biopharm 1977;5: 133-46.
Osorio I, Reed RC. Breakthrough seizures with generic carbam-
azepine: uncertainty of absorption or patient bias? A case
report. Ep ilep s ia 1988;29: 67 1-2.
Pullar T, Kumar S, Tindall H, Feely M. Time to stop counting
the tablets? Clin Pharmacol Ther 1989;46: 163-8.
Rail L. Dilantin overdosage. Med J Aust 1968;2:339.
Rosenbaum DH, Tuchman L, Moro MA, French J A, Rowan AJ .
Comparative bioavailability of a generic phenytoin and dilan-
tin. Epilepsia 1988;29:671.
Rudd P, Byyny RL, Zachary V, et al. The natural history of
medication compliance in a drug trial: limitations of pill
counts. Clin Pharmacol Ther 1989;46: 169-76.
Sachdeo RC, Chokroverty S, Belendiuk G. Risk of switching
from brand name to generic drugs in seizure disorder. Epi-
lepsia 1987;28:581.
Sawchuk RJ , Pepin SM, Leppik IE, Gumnit RJ . Rapid and slow
release of phenytoin in epileptic patients at steady state: com-
parative plasma levels and toxicity. J Pharmacokinet Bio-
pharrn 1982~; 10:365-82.
Sawchuk RJ , Pepin SM, Leppik IE, Gumnit RJ . Rapid and slow
release of phenytoin in epileptic patients at steady state:
amount of relative bioavailability utilizing Michaelis-Menten
parameters. J Pharmacokinet Biopharm 19826;30:383-91.
Shargel L, Yu A. Applied biopharmaceutics and pharmacokinet-
ics. 2nd ed. Norwalk, CT: Appleton-Century Crofts, 1985.
Tyrer JH, Eadie MJ , Sutherland J M, Hooper WD. Outbreak of
anticonvulsant intoxication in an Australian city. Br Med J
1970;2:27 1-3.
Woodbury DM. Phenytoin: absorption, distribution and excre-
tion. In: Levy RH, Dreifuss FE, Mattson RH, Meldrum BS,
Penry J K, eds. Antiepileptic Drugs. 3rd ed. New York:
Raven Press, 1989.
Zar J H. Biostatistical analysis. 2nd ed. Englewood Cliffs, NJ :
Prentice-Hall, 1984.
RfSUME
Dix patients prksentant des crises bien contr6lCes sous mono-
thtrapie chronique par phtnytoine (PHT) ont ttt i nch dans une
Ctude croisCe rendomizke en double-aveugle, comparant une
PHT de marque et une PHT gkntrique. Chaque patient a r ey la
m&me dose de chaque prtparation pendant 3 mois, avec surveil-
lance des taux sanguins de PHT et relev6 des effets collatCraux.
La concentration totale de PHT 1Ctat dtquilibre avant la prise
du medicament Ctait de 11.9 f 4.9 mg/ml pendant le traitement
par PHT de marque, contre 14.2 2 8.2 mg/ml par traitement gC-
nCrique. La concentration moyenne a ICtat dkquilibre de PHT
libre avant prise du mkdicament, Ctait de 0.93 f 0.47 mg/ml
(PHT de marque) contre 1.14 f 0.64 mg/ml (gCnCrique) (p <
0.005). La puissance (contenu de la capsule) pour les les lots
utilisCs dans les ttudes, ttait de 99.2% pour le mtdicament de
Epilepsia, Vol. 33, No. 2, 1992
GENERIC SUBSTITUTION OF PHENYTOIN 365
marque contre 104.6% pour le generique. En raison de la cine-
tique non lineaire de la PHT, une difference 5.4% pourrait ex-
pliquer les differences observCes dans les concentrations plas-
matiques. Par comparaison au produit de marque, la PHT gC-
nerique a Bte associB B une augmentation des taux sanguins.
Cette augmentation a CtC cohtrente avec la difftrence des con-
tenus des comprimts constatte entre le mtdicament de marque
et le gkntrique utilisCs dans cette Ctude.
(P. Genton, Marseille)
RESUMEN
Diez enfermos con ataques bien controlados con Fenitoina
(PHT) cronica en forma de monoterapia, para la profilaxis de
ataques, completaron un estudio cruzado, randomizado y doble
ciego comparando la marca comercial y el nombre gentrico de la
PHT. Cada paciente recibio la misma dosis de cada preparacih
durante 3 meses en 10s cuales se monotorizaron las concentra-
ciones de PHT y 10s efectos adversos. Las concentraciones pro-
medio pre-dosis, en estado estable, de fenitoina fueron de
11.9 f 4.9 microgramos/ml durante la terapia con el nombre
comercial (marca) y 14.2 f 8.2 microgramos/ml durante el tra-
tamiento con el preparado genkrico. El promedio pre-dosis de las
concentraciones de PHT en estado estable libre fueron de
0.93 * 0.47 microgramos/ml (nombre comercial o marca) y
1.14 +- 0.64 microgramos/ml (preparado generico) respectiva-
mente (P <0.005). Los valores de potencia (contenido de la
cApsula) para 10s lotes usados en este estudio fueron 99.2% para
el preparado con marca y 104.6% para el genCrico. Seglin la
cinetica no linear de Michaelis-Menten de la PHT, se piensa que
un 5.4% de diferencia en la potencia podria ser la causa de las
diferencias observadas en las concentraciones plasmaticas.
Cuando se compara con el nombre comercial, la terapia con
fenitoina genkrica se asocia a un incremento en las concentra-
ciones stricas. Este incremento estaba de acuerdo con ladife-
rencia del contenido en la cilpsula entre 10s lotes de preparado
gentrico y de marca, usados en este estudio.
(A. Portera-Sanchez, Madrid)
ZUSAMMENFASSUNG
Bei 10 Patienten mit gut eingestellten Anfallen unter chroni-
scher Phenytoin (PHT) Monotherapie wurde eine randomisierte
Doppelblind crossover Studie zum Vergleich einer Reinsubstanz
und einse Firmenpraparates gemacht. J eder Patient erhielt die
gleiche Dosis jeder Praparation fur die Dauer von 3 Monaten,
wobei PHT-Konzentrationen und Nebenwirkungen registriert
wurden. Die mittlere gesamte Gleichgewichtskonzentration von
PHT vor Einnahme betrug 11.9 * 4.9 pg/rnl bei dem Firmenpra-
parat und 14.2 f 8.2 kg/ml bei der reinen Substanz. Die mittlere
freie Gleichgewichts-PHT-Konzentration betrug 0.93 f 0.47 pg/
ml (Firmenpraparat) und 1.14 f 0.64 pg/ml (Reinsubstanz) je-
weils vor Gabe (p <0.005). Die Potenzwerte (Kapselinhalt) fur
die Einheiten bei der Studie betrugen 99.2% fur das Fabrikat und
104.6% fur die Reinsubstanz. Wegen der nicht-linearen Michae-
lis-Menten Kinetik von Phenytoin kann eine 5.4% Differenz der
Potenz fur die beobachteten Unterschihede in den Plasma-
konzentrationen verantwortlich sein. Im Vergleich zu der Fir-
menzubereitung war die Reinsubstanz-Therapie mit einem An-
stieg der Serumkonzentrationen assoziiert. Dieser Anstieg war
konsistent mit den berichteten Unterschieden im Kapselinhalt
zwischen Reinsubstanz und Firmenpraparat bei dieser Untersu-
chung.
(C. K. Benninger, Heidelberg)
Epilepsia, Vol. 33, No. 2, 1992
You might also like
- Effect of Methadone Dose Contingencies ON Urinalysis Test Results of Polydrug-Abusing Methadone-Maintenance PatientsDocument8 pagesEffect of Methadone Dose Contingencies ON Urinalysis Test Results of Polydrug-Abusing Methadone-Maintenance PatientsWao wamolaNo ratings yet
- Multiple Versus Single Antipsychotic Agents For Hospitalized Psychiatric Patients: Case-Control Study of Risks Versus BenefitsDocument7 pagesMultiple Versus Single Antipsychotic Agents For Hospitalized Psychiatric Patients: Case-Control Study of Risks Versus BenefitsPutri KeyshaNo ratings yet
- Use of Methadone For Opioid Weaning in Children: Prescribing Practices and TrendsDocument8 pagesUse of Methadone For Opioid Weaning in Children: Prescribing Practices and TrendsJessica VillanuevaNo ratings yet
- Jurding AulDocument5 pagesJurding AulRizky AuliaNo ratings yet
- Short-Term and Long-Term Evaluation of Selective Serotonin Reuptake Inhibitors in The Treatment of Panic Disorder: Fluoxetine Vs CitalopramDocument6 pagesShort-Term and Long-Term Evaluation of Selective Serotonin Reuptake Inhibitors in The Treatment of Panic Disorder: Fluoxetine Vs CitalopramBakhita MaryamNo ratings yet
- Boghossian Et Al-2017-Cochrane Database of Systematic ReviewsDocument4 pagesBoghossian Et Al-2017-Cochrane Database of Systematic ReviewsrisdalNo ratings yet
- Efficacy and Safety of Paliperidone Palmitate Eca ADocument14 pagesEfficacy and Safety of Paliperidone Palmitate Eca AMaria Fernanda AbrahamNo ratings yet
- Rubio Valera2013Document10 pagesRubio Valera2013Marcus Fábio leite AndradeNo ratings yet
- Multiple Versus Single Antipsychotic Agents For Hospitalized Psychiatric Patients: Case-Control Study of Risks Versus BenefitsDocument7 pagesMultiple Versus Single Antipsychotic Agents For Hospitalized Psychiatric Patients: Case-Control Study of Risks Versus BenefitsPutri KeyshaNo ratings yet
- Approach by Health Professionals To The Side Effects of Antihypertensive Therapy: Strategies For Improvement of AdherenceDocument10 pagesApproach by Health Professionals To The Side Effects of Antihypertensive Therapy: Strategies For Improvement of AdherenceSabrina JonesNo ratings yet
- Topiramato y TouretteDocument5 pagesTopiramato y TouretteilonaskorinNo ratings yet
- Herrmann WM, Stephan K. Int Psychogeriatr. 1992 4 (1) :25-44.Document20 pagesHerrmann WM, Stephan K. Int Psychogeriatr. 1992 4 (1) :25-44.Ангелина СкоморохинаNo ratings yet
- Repetition Following Amelioration in Homoeopathy A Randomized Placebo Controlled Pilot StudyDocument7 pagesRepetition Following Amelioration in Homoeopathy A Randomized Placebo Controlled Pilot StudyHomoeopathic PulseNo ratings yet
- Proposal SalmaDocument4 pagesProposal Salmaبشير حيدرNo ratings yet
- Jurnal DMDocument19 pagesJurnal DMCcNo ratings yet
- Comparative Bioavailability Study of Phenytoin inDocument4 pagesComparative Bioavailability Study of Phenytoin inHuydiNo ratings yet
- Jurnalnantipsychotic PDFDocument9 pagesJurnalnantipsychotic PDFamiaslimNo ratings yet
- Histopathology of Preclinical Toxicity Studies: Interpretation and Relevance in Drug Safety EvaluationFrom EverandHistopathology of Preclinical Toxicity Studies: Interpretation and Relevance in Drug Safety EvaluationNo ratings yet
- Journal ClubDocument63 pagesJournal Clubdrkadiyala2No ratings yet
- Inappropriate Use of Proton Pump Inhibitors in Elderly Patients Discharged From Acute Care HospitalsDocument6 pagesInappropriate Use of Proton Pump Inhibitors in Elderly Patients Discharged From Acute Care HospitalsFitriNo ratings yet
- Literature ReviewDocument53 pagesLiterature ReviewJEMY JOSENo ratings yet
- Soap2 PDFDocument13 pagesSoap2 PDFframc3sca2911No ratings yet
- Interventions in Nursing HomesDocument18 pagesInterventions in Nursing Homesvictory818No ratings yet
- Role of Aprepitant in Chemotherapy Induced Nausea and VomitingDocument13 pagesRole of Aprepitant in Chemotherapy Induced Nausea and Vomitinganon_602767910No ratings yet
- Drug Utilization Review (DUR) Meeting May 8, 2013 Members PresentDocument8 pagesDrug Utilization Review (DUR) Meeting May 8, 2013 Members PresentNana BernabeuNo ratings yet
- Sachmechi 2007Document5 pagesSachmechi 2007Susana RocheNo ratings yet
- Olanzapine For The Prevention of Chemotherapy-Induced Nausea and VomitingDocument9 pagesOlanzapine For The Prevention of Chemotherapy-Induced Nausea and VomitingAdina NeagoeNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Betahistine Dihydrochloride in The Treatment of Peripheral Vestibular VertigoDocument6 pagesBetahistine Dihydrochloride in The Treatment of Peripheral Vestibular VertigoRidho HidayatullohNo ratings yet
- Omeprazole-Mg 20.6 MG Is Superior To Lansoprazole 15 MG For Control of Gastric Acid: A Comparison of Over-The-Counter Doses of Proton Pump InhibitorsDocument6 pagesOmeprazole-Mg 20.6 MG Is Superior To Lansoprazole 15 MG For Control of Gastric Acid: A Comparison of Over-The-Counter Doses of Proton Pump InhibitorsrahmaNo ratings yet
- Proton-Pump Inhibitors Therapy and Blood Pressure ControlDocument6 pagesProton-Pump Inhibitors Therapy and Blood Pressure ControlTeky WidyariniNo ratings yet
- PJMS 34 959Document5 pagesPJMS 34 959Husni FaridNo ratings yet
- CATIE Schizophrenia Trial Results ImpactDocument14 pagesCATIE Schizophrenia Trial Results ImpactNim RodNo ratings yet
- 2014 Lee (TOFA Vs MTX)Document10 pages2014 Lee (TOFA Vs MTX)Marcel JinihNo ratings yet
- Fluoxetine TreatmentDocument6 pagesFluoxetine TreatmentDoyin AwodeleNo ratings yet
- New Topics in phaRMcology (97-2003)Document18 pagesNew Topics in phaRMcology (97-2003)api-3761895No ratings yet
- Placebo-Controlled Trial of Tofacitinib Monotherapy in RA Agust 2012Document13 pagesPlacebo-Controlled Trial of Tofacitinib Monotherapy in RA Agust 2012Idhul AR FitraNo ratings yet
- Case Based Clinical Pearls - A Schizophrenic Case StudyDocument5 pagesCase Based Clinical Pearls - A Schizophrenic Case StudyTeofel John Alvizo PantaleonNo ratings yet
- A Textbook of Clinical Pharmacology and Therapeutics PDFDocument6 pagesA Textbook of Clinical Pharmacology and Therapeutics PDFMovie Box MoviesNo ratings yet
- 07 Dosage RegimenDocument44 pages07 Dosage Regimenzetttttttttt100% (3)
- Mother NejmDocument12 pagesMother NejmIzara Maité Mondragón MorenoNo ratings yet
- Tofacitinib For Psoriatic Arthritis in Patients With An Inadequate Response To TNF InhibitorsDocument12 pagesTofacitinib For Psoriatic Arthritis in Patients With An Inadequate Response To TNF InhibitorsPutri YunandaNo ratings yet
- Acetatode Medroxiprogesterona PDFDocument5 pagesAcetatode Medroxiprogesterona PDFG Chewie CervantesNo ratings yet
- 24-Hour Efficacy and Safety of Triple-Combination Therapy With Olmesartan, Amlodipine, and Hydrochlorothiazide: The TRINITY Ambulatory Blood Pressure SubstudyDocument8 pages24-Hour Efficacy and Safety of Triple-Combination Therapy With Olmesartan, Amlodipine, and Hydrochlorothiazide: The TRINITY Ambulatory Blood Pressure SubstudyRaissa Andi SoekrisnoNo ratings yet
- Appi Ajp 2018 17111282Document14 pagesAppi Ajp 2018 17111282Alan AlvídrezNo ratings yet
- Out Come StudyDocument12 pagesOut Come StudyjaraNo ratings yet
- 12 - 2015 - LT Safety and Efficacy of Imatinib in PAH - IMPRES (10) 70Document10 pages12 - 2015 - LT Safety and Efficacy of Imatinib in PAH - IMPRES (10) 70edward the iiiNo ratings yet
- Meta-Analysis: 4CLPH - Group 9Document36 pagesMeta-Analysis: 4CLPH - Group 9Marlon Mallillin IIINo ratings yet
- 8400-Article Text-50016-1-10-20090108Document5 pages8400-Article Text-50016-1-10-20090108Dammi LauNo ratings yet
- PG15Document44 pagesPG15Nabila ChakourNo ratings yet
- RelapseDocument10 pagesRelapseEmil Eduardo Julio RamosNo ratings yet
- Hyperprolactinemia and Galactorrhea Induced by Serotonin and Norepinephrine Reuptake Inhibiting AntidepressantsDocument10 pagesHyperprolactinemia and Galactorrhea Induced by Serotonin and Norepinephrine Reuptake Inhibiting AntidepressantsSteven KatuukNo ratings yet
- Evaluation of A Pharmaceutical Care Program For Hypertensive Patients in Rural PortugalDocument7 pagesEvaluation of A Pharmaceutical Care Program For Hypertensive Patients in Rural PortugalNOorulain HyderNo ratings yet
- Original Papers: Prolonged Thiopentone Infusion For Neurosurgical Emergencies: Usefulness of Therapeutic Drug MonitoringDocument10 pagesOriginal Papers: Prolonged Thiopentone Infusion For Neurosurgical Emergencies: Usefulness of Therapeutic Drug MonitoringMohammedNo ratings yet
- Prescribing Pattern of Antihypertensive Drugs in A Tertiary Care Hospital in Jammu-A Descriptive StudyDocument4 pagesPrescribing Pattern of Antihypertensive Drugs in A Tertiary Care Hospital in Jammu-A Descriptive StudyMahantesh NyayakarNo ratings yet
- Pharmacokinetics, PharmacodynamicsDocument18 pagesPharmacokinetics, PharmacodynamicspinkbutterNo ratings yet
- Características de Las Interacciones Farmacológicas en Una Unidad de Cuidados Intensivos de PediatríaDocument8 pagesCaracterísticas de Las Interacciones Farmacológicas en Una Unidad de Cuidados Intensivos de PediatríaJohn AlexNo ratings yet
- PK ProblemsDocument18 pagesPK ProblemsJosephine Valsa JoseNo ratings yet
- Shirure Et AlDocument7 pagesShirure Et AleditorijmrhsNo ratings yet
- (1479683X - European Journal of Endocrinology) A Comparison Between Spironolactone and Spironolactone Plus Finasteride in The Treatment of HirsutismDocument4 pages(1479683X - European Journal of Endocrinology) A Comparison Between Spironolactone and Spironolactone Plus Finasteride in The Treatment of HirsutismSoheil SssNo ratings yet
- Chemistry H3 Notes The Synthesis of ParacetamolDocument15 pagesChemistry H3 Notes The Synthesis of ParacetamolSimon KohNo ratings yet
- Managing dental patients with cardiovascular diseasesDocument54 pagesManaging dental patients with cardiovascular diseasesSafiraMaulidaNo ratings yet
- DrugsDocument10 pagesDrugsRebecca JolieNo ratings yet
- The Truth About CrackDocument24 pagesThe Truth About Crackofficialdfw100% (1)
- Mycophenolate Information For Parents/CarersDocument12 pagesMycophenolate Information For Parents/CarersDavid LopezNo ratings yet
- Drugs For Gastrointestinal Tract DisordersDocument32 pagesDrugs For Gastrointestinal Tract DisordersPam LalaNo ratings yet
- Module 2Document30 pagesModule 2mannanNo ratings yet
- Case04.Epilepsy-Tonic ClonicDocument38 pagesCase04.Epilepsy-Tonic Clonicshivani7448No ratings yet
- Professional Adjustment and Nursing JurisprudenceDocument8 pagesProfessional Adjustment and Nursing JurisprudenceLheidaniel MMM.No ratings yet
- Multiple SclerosisDocument21 pagesMultiple Sclerosisjhodane100% (1)
- FN-SSB 119Document5 pagesFN-SSB 119LunaPolidoNo ratings yet
- Dispensing, Incompatibilities, ADR PDFDocument19 pagesDispensing, Incompatibilities, ADR PDFKate Evangelista100% (1)
- Myasthenia GravisDocument39 pagesMyasthenia GravisDelyn Gamutan Millan100% (1)
- Amino Acid Therapy ChartDocument2 pagesAmino Acid Therapy Chartahill140100% (12)
- Bio Availability and Bioequivalane-LastDocument13 pagesBio Availability and Bioequivalane-LastAhmedothman62100% (1)
- BromazepamDocument6 pagesBromazepamMariusNeicuNo ratings yet
- Pharmaceutical Dosage Forms PDFDocument20 pagesPharmaceutical Dosage Forms PDFdavenNo ratings yet
- State Director Letter - Joint ACF CMS and SAMHSA On Psychotropic Drug Use in Foster CareDocument7 pagesState Director Letter - Joint ACF CMS and SAMHSA On Psychotropic Drug Use in Foster CareBeverly TranNo ratings yet
- Drugs and Their ClassificationDocument23 pagesDrugs and Their Classificationkalkigarg0% (2)
- Toxicology - MedbulletsDocument5 pagesToxicology - MedbulletsindyaholicNo ratings yet
- Patient Write-Up Example 2Document6 pagesPatient Write-Up Example 2Meliara101No ratings yet
- Drugs Pregnancy CategoryDocument14 pagesDrugs Pregnancy CategoryDevi RachmawatiNo ratings yet
- Loyalty CardDocument42 pagesLoyalty CardAnonymous 5RdFcggNo ratings yet
- Assignment - Anti Viral DrugsDocument5 pagesAssignment - Anti Viral DrugsmziabdNo ratings yet
- SpironolaktoneDocument2 pagesSpironolaktoneReza Ervanda ZilmiNo ratings yet
- RopDocument364 pagesRopIeie MawonNo ratings yet
- Medcorps Patient FormDocument7 pagesMedcorps Patient Formapi-3609449100% (1)
- Pharmaceutical Industry in BangladeshDocument3 pagesPharmaceutical Industry in BangladeshWalidur Rahman MridulNo ratings yet
- OTC drug database with active ingredientsDocument7,389 pagesOTC drug database with active ingredientsserifblackNo ratings yet
- DyspepsiaDocument228 pagesDyspepsiaamal.fathullah100% (1)